Abstract
Background
Bone tumor resections for limb salvage have become the standard treatment. Recently, intercalary tumor resection with epiphyseal sparing has been used as an alternative in patients with osteosarcoma. The procedure maintains normal joint function and obviates some complications associated with osteoarticular allografts or endoprostheses; however, long-term studies analyzing oncologic outcomes are scarce, and to our knowledge, the concern that a higher local recurrence rate may be an issue has not been addressed.
Questions/purposes
We wanted to assess (1) the overall survival in patients treated with this surgical technique; (2) the percentage of local recurrence and limb survival, specifically the incidence of recurrence in the remaining epiphysis; (3) the frequency of orthopaedic complications, and, (4) the functional outcomes in patients who have undergone intercalary tumor resection.
Methods
We analyzed all 35 patients with osteosarcomas about the knee (distal femur and proximal tibia) treated at our center between 1991 and 2008 who had resection preserving the epiphysis and reconstruction with intercalary allografts. Minimum followup was 5 years, unless death occurred earlier (mean, 9 years; range, 1–16 years), and no patients were lost to followup. During the study period, our indications for this approach included patients without metastases, with clinical and imaging response to neoadjuvant chemotherapy, that a residual epiphysis of at least 1 cm thickness could be available after a surgical margin width in bone of 10 mm was planned, and 16% of patients (35 of 223) meeting these indications were treated using this approach. Using a chart review, we ascertained overall survival of patients, oncologic complications such as local recurrence and tumor progression, limb survival, and orthopaedic complications including infection, fracture, and nonunion. Survival rates were estimated using the Kaplan-Meier method. Patient function was evaluated using the Musculoskeletal Tumor Society (MSTS)-93 scoring system.
Results
Overall survival rate of the patients was 86% (95% CI, 73%–99%) at 5 and 10 years. Five patients died of disease. No patient had a local recurrence in the remaining bony epiphysis, but three patients (9%; 95% CI, 0%–19%) had local recurrence in the soft tissue. The limb survival rate was 97% (95% CI, 89%–100%) at 5 and 10 years. Complications treated with additional surgical procedures were recorded for 19 patients (54%), including three local recurrences, two infections, 11 fractures, and three nonunions. In 10 of these 19 patients, the allograft was removed. Only five of the total 35 study patients (14%) lost the originally preserved epiphysis owing to complications. The mean functional score was 26 points (range, 10–30 points, with a higher score representing a better result) at final followup.
Conclusions
Although the recurrence rate was high in this series, the small sample size means that even one or two fewer recurrences might have resulted in a much more favorable percentage. Because of this, future, larger studies will need to determine whether this is a safe approach, and perhaps should compare epiphyseal preservation with other possible approaches, including endoprosthetic reconstruction and/or osteoarticular allografts.
Level of Evidence
Level IV, therapeutic study.
Introduction
Currently, patients with high-grade osteosarcoma treated with the combination of chemotherapy and tumor resection with adequate margins may have a survival rate greater than 70% after 5 years [3, 8]. The most common tumor resection technique used for a metaphyseal osteosarcoma of the distal femur or proximal tibia is the intraarticular resection of the distal part of the femur, proximal part of the tibia, or both [11, 23]. However, intercalary tumor resection, with preservation of the epiphysis and knee, is an alternative in patients without tumor involvement of the distal part of the femur or the proximal part of the tibia [1, 5, 7, 14, 24, 26]. The technique is possible in selected patients owing to advances in preoperative imaging [9, 10, 18–22], which allows the surgeon to determine tumor margins and plan tumor resection that preserve a patient’s uninvolved epiphysis.
Some short-term results have been reported [15, 16, 25], but long-term studies analyzing oncologic outcomes are scarce [27]. Although we previously found that reconstructive complications that require second operations are to be expected [16], we suggested that approximately one of six metaphyseal osteosarcomas around the knee could be treated with appropriate oncologic margins and preservation of the epiphysis of the affected bone; however, evaluation of these patients with longer followup has not been reported.
We therefore sought to determine whether this type of resection allows acceptable limb function without increasing the risk of local recurrence or death in patients with osteosarcoma of the knee followed for 5 or more years. To address this issue, we asked the following questions: what is (1) the overall survival in patients treated with this surgical technique; (2) the percentage of local recurrence and limb survival, specifically, the incidence of recurrence in the remaining epiphysis; (3) the frequency of orthopaedic complications; and (4) the functional outcomes in patients who have undergone intercalary tumor resection.
Patients and Methods
We reviewed 223 patients with high-grade osteosarcomas of the knee treated from March 1991 to March 2008 at our institution. We included in this study all patients treated with proximal tibia or distal femur epiphyseal preservation after tumor resection, and who had reconstruction with an intercalary allograft. We excluded patients treated with resection of the entire distal femur or proximal tibia or patients who had a previous inappropriate operation owing to misdiagnosis. This left 35 patients available for our study (Table 1). During the study period, our indications for this approach included patients without metastases, with clinical and imaging response to neoadjuvant chemotherapy, that a residual epiphysis of at least 1 cm thickness could be available after a surgical margin width in bone of 10 mm was planned, and 16% of patients (35 of 223) meeting these indications were treated using this approach.
Table 1.
Demographic data of the patients
| Patient | Age (years) | Sex | Bone | Open growth plate | Tumor necrosis (percent) | Followup (months) | Epiphysis preservation | Complication | MSTS | Normal knee function | Use of external support |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 18 | F | T | No | ≥ 90 | 276 | Yes | No | 27 | Yes | No |
| 2 | 24 | M | T | No | ≥ 90 | 123 | No | Infection | 10 | No | Yes |
| 3 | 9 | F | F | Yes | ≥ 90 | 184 | Yes | Fracture | 27 | No | No |
| 4 | 16 | M | F | No | ≥ 90 | 189 | Yes | Fracture | 20 | No | No |
| 5 | 18 | F | F | No | ≥ 90 | 26 | Yes | No | NA | NA | NA |
| 6 | 40 | F | F | No | ≥ 90 | 174 | Yes | Fracture | 29 | Yes | No |
| 7 | 21 | M | F | No | ≥ 90 | 156 | No | Fracture | 20 | No | Yes |
| 8 | 17 | F | F | No | ≥ 90 | 166 | Yes | No | 29 | Yes | No |
| 9 | 14 | F | T | No | ≥ 90 | 162 | Yes | Fracture | 29 | Yes | No |
| 10 | 18 | M | T | No | ≥ 90 | 161 | Yes | Fracture | 25 | Yes | No |
| 11 | 15 | F | T | No | ≥ 90 | 147 | Yes | LR | 30 | Yes | No |
| 12 | 13 | F | T | Yes | ≥ 90 | 134 | Yes | Fracture | 29 | Yes | No |
| 13 | 17 | F | F | No | ≥ 90 | 153 | Yes | No | 28 | Yes | No |
| 14 | 18 | F | F | No | ≥ 90 | 129 | No | Fracture | 22 | No | No |
| 15 | 11 | F | F | Yes | ≥ 90 | 132 | Yes | No | 30 | Yes | No |
| 16 | 50 | F | F | No | < 90 | 59 | No | LR | NA | NA | NA |
| 17 | 16 | M | T | No | ≥ 90 | 132 | Yes | Nonunion | 30 | Yes | No |
| 18 | 16 | M | T | No | < 90 | 129 | Yes | No | 29 | Yes | No |
| 19 | 16 | M | F | No | ≥ 90 | 134 | Yes | Fracture | 30 | Yes | No |
| 20 | 22 | M | F | No | ≥ 90 | 113 | Yes | Nonunion | 25 | No | No |
| 21 | 12 | M | F | Yes | ≥ 90 | 121 | Yes | Fracture | 27 | No | No |
| 22 | 21 | M | F | No | < 90 | 23 | Yes | No | NA | NA | NA |
| 23 | 9 | M | F | Yes | ≥ 90 | 21 | Yes | LR | NA | NA | NA |
| 24 | 15 | F | F | No | < 90 | 92 | Yes | No | 30 | Yes | No |
| 25 | 6 | M | F | Yes | < 90 | 87 | Yes | No | 28 | No | No |
| 26 | 8 | F | F | Yes | ≥ 90 | 88 | Yes | No | 27 | No | No |
| 27 | 17 | M | T | No | ≥ 90 | 85 | Yes | Infection | 29 | Yes | No |
| 28 | 8 | M | F | Yes | ≥ 90 | 79 | Yes | Nonunion | 25 | No | No |
| 29 | 37 | F | F | No | ≥ 90 | 85 | Yes | No | 30 | Yes | No |
| 30 | 5 | M | F | Yes | ≥ 90 | 81 | Yes | Fracture | 28 | No | No |
| 31 | 19 | M | F | No | < 90 | 76 | Yes | No | 27 | Yes | No |
| 32 | 13 | F | F | No | ≥ 90 | 62 | Yes | No | 28 | Yes | No |
| 33 | 10 | M | F | Yes | ≥ 90 | 60 | Yes | No | 28 | No | No |
| 34 | 13 | M | F | No | ≥ 90 | 60 | Yes | No | 28 | Yes | No |
| 35 | 2 | M | F | Yes | ≥ 90 | 34 | Yes | No | NA | NA | NA |
T = tibia; F = femur; LR = local recurrence; MSTS = Musculoskeletal Tumor Society functional score; NA = not available.
Nine tumors were located in the tibia and 26 were in the femur. There were 16 females and 19 males, with a mean age of 17 years (range, 2–50 years).The growth plate was open in 11 patients (seven patients were younger than 10 years) and we did not attempt to preserve it in these patients. Patients with limb length discrepancy were treated by distraction osteogenesis procedures if needed at skeletal maturity. A minimum followup of 5 years was required for inclusion, unless death from tumor progression occurred earlier. The duration of followup was calculated from the date of the resection to the date that the patient was last seen (for asymptomatic patients) or the date of death or amputation (for limb-survival analysis). The average followup was 9 years (range, 1–23 years, again allowing for inclusion of patient data from those who died before the 5-year minimum followup). No patient was lost to followup.
All patients were treated with neoadjuvant chemotherapy. Three patients were treated with a combination of cisplatinum (100 mg/m2, Weeks 0, 6, and 14), ifosfamide (3 g/m2 for 2 days, Weeks 3, 11, and 17), and doxorubicin (25 mg/m2 for 3 days, Weeks 3, 6, 11, 14, and 17) [4]. Surgical treatment was in the ninth week of the protocol. The remaining 32 patients were treated with a combination of ifosfamide (1.8 g/m2 for 5 days, Weeks 0, 5, and10), Adriamycin (25 mg/m2 for 3 days, Weeks 0, 5, and10), and high-dose methotrexate (12 g/m2, Weeks 3, 4, 8, 9, 13, and 14) [4]. Surgical treatment occurred during the 15th week of the protocol.
Preoperatively, we evaluated all patients with MRI. Images were acquired with a 1.5-T Magnetom Vision unit (Siemens, Erlangen, Germany) at the time of the diagnosis and at the end of each chemotherapy regimen. The image acquisition protocol was made as reported previously [16]. The extent of epiphyseal involvement was calculated with coronal, sagittal, and axial images defining the edge of the tumor as the point in which marrow signal intensity changed from normal to abnormal. Patients were evaluated according to the following criteria: (1) the assessment of tumor response or progression as assessed by MRI; (2) the age of the patient and potential for skeletal growth; (3) the distance between the articular joint cartilage and the tumor as assessed by MRI of 2 cm or more, to obtain a bone width margin of 10 mm and a remaining residual epiphysis of 1 cm (Fig. 1); and (4) a sufficient amount of epiphysis preserved to allow fixation of the osteotomy junction [16]. Tumors with evidence of clinical response, such as pain and mass reduction, and evidence of necrosis and reduction of soft tissue mass on MR images during chemotherapy were considered for this procedure. In all patients, operative treatment consisted of resection of the tumor and insertion of an allograft segment tailored to fit the bone defect using a technique previously described [17]. After the operations, the histologic margins were negative in all patients. All patients had a margin width in bone of at least 10 mm. Although all patients showed clinical response and response on MR images to preoperative chemotherapy, 29 had tumor necrosis of 90% or greater (Table 1) and six had necrosis less than 90%.
Fig. 1.
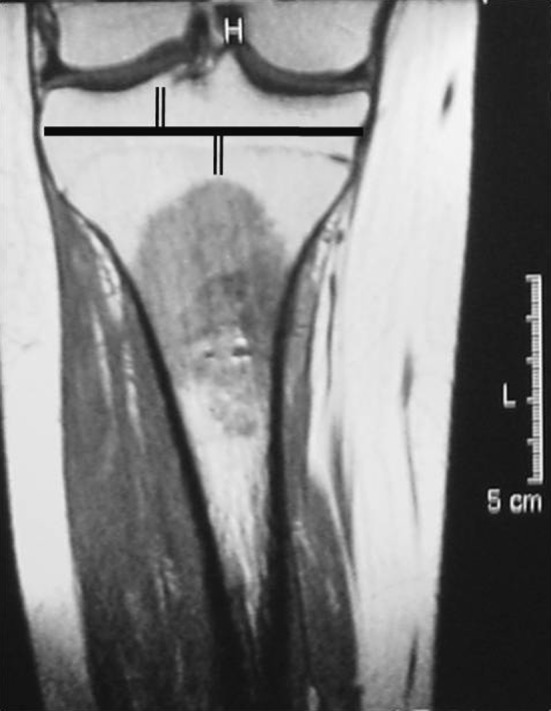
A coronal MR image of the right proximal tibia shows how the transepiphyseal osteotomy was planned in a patient with an osteosarcoma. The horizontal black line shows the planned osteotomy in the epiphysis, there are two 1-cm vertical black lines on either side of the osteotomy (the proximal line shows the remaining proximal tibia, and the distal one shows the 1 cm margin planned to be obtained).
Patients’ overall survival and limb survival were estimated using the Kaplan–Meier method [13]. Oncologic complications, such as local recurrence and tumor progression, were evaluated. We analyzed limb survival, the number of secondary amputations, and the number of patients in whom the preserved epiphysis eventually was maintained. We used SPSS 17.0 for Windows (SPSS, Inc, Chicago, IL, USA) for statistical analyses.
Functional evaluation of the patients was performed using the revised 30-point functional classification system established by the International Society of Limb Salvage and the Musculoskeletal Tumor Society (MSTS) [6]. The functional score measured six parameters: pain, function, emotional acceptance, use of walking supports, walking ability, and gait. Each parameter is given a value ranging from 0 to 5, according to specific criteria. The individual scores are added together to obtain an overall functional score, with a maximum of 30 points, which then is expressed as a percentage of normal, with 30 points being defined as normal function. A score of 23 points or greater is considered an excellent functional result, 15 to 22 points is a good result, 8 to 14 points is a fair result, and less than 8 points is a poor result [6].
Results
The overall Kaplan-Meier survival for our study population was 86% at 5 years and 10 years (95% CI, 73%–99%) (Fig. 2). At the final followup, 30 patients continued to be disease-free and five had died of disease (three with ≥ 90% tumor necrosis and two with < 90% tumor necrosis).
Fig. 2.
A graph shows a Kaplan-Meier curve for survival of the study patients. The overall survival rate for patients was 86% at 5 years and 10 years (95% CI, 73%–99%).
Three patients (9%; 95% CI, 0%–19%) had a soft tissue local recurrence (two with ≥ 90% tumor necrosis and one with < 90% tumor necrosis) (Table 1) and two of them died of pulmonary metastases. Of the three patients with local recurrences, one was treated with amputation because of contact with neurovascular structures and died of disease 30 months from discovery of the recurrence. The remaining two patients were treated with resection of the local soft tissue recurrence. One patient is alive without detectable disease at 120 months after resection of the recurrence and the other died 11 months after resection. Of these three patients, one had had a previous pathologic fracture at the time of the original diagnosis. No patient had a local recurrence in the preserved epiphysis. The Kaplan-Meier limb survival was 97% at 5 years and 10 years (95% CI, 89%–100%). In total, five patients lost the originally saved epiphysis owing to fracture (three patients), amputation (one patient), or infection (one patient).
Of the 35 patients in the study, 16 (46%; 95% CI, 22%–70%) achieved healing without orthopaedic or oncologic complications. A second surgical procedure was performed in 19 patients, three to treat oncologic complications (three local recurrences) and 16 to treat orthopaedic complications, including 11 fractures, three diaphyseal nonunions, and two deep infections. In nine (26%) patients, the allograft was removed because of orthopaedic complications (seven fractures and two infections). Kaplan-Meier allograft survival was 73% at 5 years (95% CI, 58%–88%) and 68% at 10 years (95% CI, 50%–86%) (Fig. 3). In seven of the 11 fractures, the allografts were removed and treated with a new reconstruction. All were localized in the femur and four were treated with another intercalary graft to preserve the original epiphysis. The remaining three fractures were treated with distal femur endoprostheses (two patients) or an osteoarticular allograft (one patient), sacrificing the originally preserved epiphysis. Four of the 11fractures were nondisplaced; three were tibial fractures and one was located in the femur. All were treated with a new osteosynthesis using autogenous bone graft. In all three diaphyseal nonunions, one operation in which the internal fixation was replaced and autogenous graft was added to the site resulted in union at the host-donor junction in a mean of 4 months. Two patients had acute deep infections, which were treated with removal of the allograft and implantation of a temporary antibiotic-impregnated cement spacer. After infection control one patient finally was treated with a new intercalary allograft (Fig. 4) and the other had reconstruction with a proximal tibia allograft-prosthesis composite, losing the originally saved epiphysis.
Fig. 3.
The graph shows a Kaplan-Meier curve for survival of allografts. The overall survival rate for the 35 allografts was 73% at 5 years (95% CI, 58%–88%) and 68% at10 years (95% CI, 50%–86%).
Fig. 4A–C.
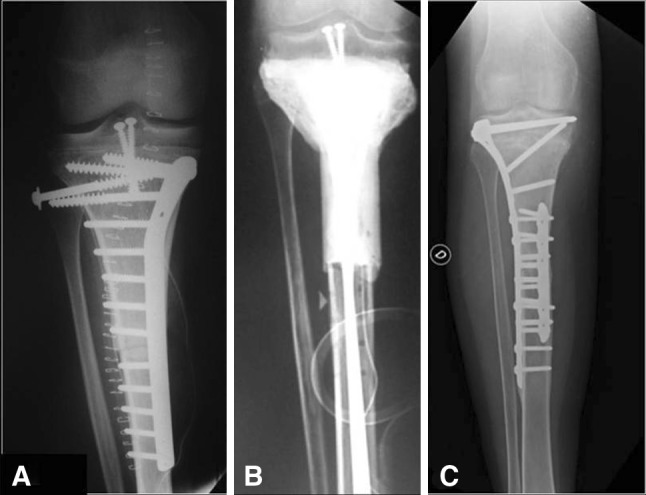
A 17-year old male patient had an osteosarcoma of the right proximal tibia. He underwent reconstruction with an intercalary tibia allograft after transepiphyseal resection of a metadiaphyseal osteosarcoma. (A) An AP radiograph of the right proximal tibia obtained immediately after resection of the tumor and reconstruction with an allograft shows fixation of the allograft to the host bone with a medial buttress proximal plate and two screws in the remaining epiphysis. (B) An AP radiograph of the right proximal tibia 1 year after reconstruction shows a temporary antibiotic-impregnated cement spacer that replaced the original allograft owing to a deep infection. (C) Seven years postoperatively, the patient’s AP radiograph of the right tibia is shown. The patient underwent reconstruction with a second allograft with a new lateral long plate (proximal tibia locking compression plate) that covers both osteotomies and addition of a short medial plate in the distal osteotomy.
The 30 patients available for functional evaluation had a mean functional score of 26 points (range, 10–30 points) (Table 1). Two patients needed some kind of support to walk, whereas the other 28 were able to walk unaided. Eighteen patients achieved normal knee flexion and extension. The 26 patients who had the epiphysis preserved had a mean functional score of 28 points.
Discussion
Tumor resection surgery with preservation of the epiphysis in patients with metaphyseal osteosarcoma is a technique that has been attempted in recent years. This is likely attributable to better imaging technologies and more experience with limb-preservation techniques. However, there is a paucity of literature regarding the long-term oncologic and orthopaedic results of this approach [24]. We therefore sought to evaluate (1) the overall survival in patients treated with this surgical technique; (2) the percentage of local recurrence and limb survival, specifically, the incidence of recurrence in the remaining epiphysis; (3) the frequency of orthopaedic complications; and (4) the functional outcomes in patients treated with this approach.
We acknowledge some limitations to our study. It was a retrospective study with a small number of patients. Given the relative rarity of the disease and the unique surgical treatment for each individual, it would be difficult to obtain a larger series at one center, however, to our knowledge, ours is one of the largest studies for this type of bone tumor resection and it presents long-term oncologic and orthopaedic outcomes. Another limitation is that we did not analyze patients who met reasonable indications for an epiphyseal-sparing approach but were treated with other approaches (prostheses or osteoarticular grafts) because of the lack of evidence of clinical or MRI response, or both, to compare survival or local recurrence.
Overall survival in our series was 86%. This survival rate is higher compared with other series of patients with high-grade osteosarcomas [3, 8], however, for this type of surgical resection, patients were carefully selected. One of the main indications for this method is clinical and imaging response of the patient to neoadjuvant chemotherapy. Conversely, if a patient did not respond during neodjuvant chemotherapy, this type of resection would be contraindicated. However, although we selected these patients with clinical and imaging parameters, six were not good responders, but the margins obtained were free of tumor and no other surgical approach was performed. Andreou et al. [2] reported that patients participating in a study fared significantly better (p < 0.0001) than those who were only registered and followed prospectively. This could be the cause of the higher patient survival in our series because although six patients were histologically poor responders, they could have other favorable characteristics such as small tumor size, adequate biopsy, or absence of soft tissue infiltration.
In our series, we observed three (9%) local recurrences. Only one patient was treated with amputation for a local recurrence, giving us a limb-survival rate of 97%, a percentage of limb salvage similar to those of other published series [5, 16]. Two other local recurrences were treated with an oncologic resection with limb preservation. All recurrences were in soft tissue, and none was in the remaining original epiphysis. Although the recurrence rate was high in our series, the small sample size means that even one or two fewer recurrences might have resulted in a much more favorable percentage. Canadell et al. [5] performed transepiphyseal resection in 12 high-grade osteosarcomas and had one local recurrence in their series. Our incidence of local recurrences is similar to that observed in other patients with osteosarcomas treated with limb-sparing surgery with other techniques [2, 5, 8, 12, 14]. Ferrari et al. [8] reported 18 local recurrences (8%) in 230 patients who had conservative surgery. Although there is no consensus regarding what constitutes an appropriate margin for resection of an osteosarcoma with a good response to chemotherapy, in our series, leaving a margin of at least 1 cm, we observed no local recurrences in the remaining bony epiphysis. Andreou et al. [2] reported that limb-sparing procedures were associated with a higher local recurrence rate (7.5%), with no difference in disease-specific survival (p = 0.118). They also found that surgical margin width in bone did not correlate with the local recurrence rate, either in the group as a whole (p = 0.126) or in subgroup analyses of limb-sparing procedures only (p = 0.692), margin width of 10 mm or less only (p = 0.223), 20 mm or less only (p = 0.379), or when comparing a width of 10 mm or less with a width of 11 to 20 mm. Jeon et al. [12] analyzed 35 local recurrences in 445 osteosarcomas (7.8%), and reported no relation between the adequacy of soft tissue margin and local recurrences in a corresponding area. They observed local recurrence located away from the initial tumor or in patients who had whole muscle compartment resections. They suggested that in the soft tissues, poor responders might have different local tumor spread mechanisms from those of good responders. Recurrence could be more dependent on vascular or lymphatic pathways rather than by direct infiltration of the muscle compartment.
Sixteen of our patients (46%) had orthopaedic complications related to the reconstruction. The main complication was fracture of the allograft in 11 patients (31%). Yu et al. [27] analyzed five patients with preservation of the epiphysis after resection of high-grade osteosarcomas with a minimum followup of 5 years, and they described three fractures (66%) in their series. Weitao et al. [25] analyzed 15 patients with epiphysis-preserving operations for treatment of lower-limb malignant bone tumors, with a minimum followup of 2 years who had reconstruction with an intercalary allograft. They observed 13 patients with delayed union (87%), two with resorption of the graft (13%), and one with infection (7%). We had only three patients with nonunion (9%), but our infection rate was similar to their reported rate (6%; two of 35 patients).
Allograft survival was 73% with a mean functional score of 26 for our patients. Normal knee flexion and extension was achieved by 18 patients and 28 patients were able to walk unaided after surgery. These results are comparable with those of previous studies of reconstruction of bone defects if the epiphysis is preserved [7, 23–27]. Yu et al. [27] evaluated five patients in whom the epiphysis was preserved after resection of osteosarcoma of the distal femur; their patients were followed for more than 5 years. The mean functional score in their series was 25.6 points. Weitao et al. [25] analyzed 15 patients with epiphysis-preserving operations for treatment of lower-limb malignant bone tumors. Normal knee flexion and extension were achieved by 14 patients and all were able to walk unaided 24 months after surgery. Yao et al. [26] evaluated six patients with distal femur osteosarcoma who underwent epiphysis-preserving operations. The final functional MSTS score for their patients was 27.20 ± 1.92.
Preservation of the epiphysis is a reasonable alternative in selected patients with a metaphyseal osteosarcoma located at the knee, with adequate long-term survival. The advantages of this technique are preservation of a normal joint in a young patient, the possibility of avoiding joint complications seen with osteoarticular grafts (need for conversion to TKA at some point, joint instability) and endoprostheses (loosening, revisions). However, the recurrence rate was high in our series with a selected group of patients. Crucial factors in selecting patients for this technique are the ability to obtain adequate margins and good response to neoadjuvant chemotherapy. It is possible that poor responders have different local tumor spread mechanisms from those of good responders. Although we selected patients with clinical and imaging parameters, a small number of the patients were good responders, and might have been better served with another surgical approach. Future studies with more patients are needed to determine whether this is a safe approach, and perhaps should compare epiphyseal preservation with other possible approaches, including endoprosthetic reconstruction and/or osteoarticular allografts.
Footnotes
One of the authors certifies that he (LA-T), or a member of his or her immediate family, has or may receive payments or benefits, during the study period, an amount in excess of USD $10,000 from a commercial entity (Stryker Americas, Miramar, FL, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Amitani A, Yamazaki T, Sonoda J, Tanaka M, Hirata H, Katoh K, Uchida A. Preservation of the knee joint in limb salvage of osteosarcoma in the proximal tibia: a case report. Int Orthop. 1998;22:330–334. doi: 10.1007/s002640050272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andreou D, Bielack SS, Carrle D, Kevric M, Kotz R, Winkelmann W, Jundt G, Werner M, Fehlberg S, Kager L, Kühne T, Lang S, Dominkus M, Exner GU, Hardes J, Hillmann A, Ewerbeck V, Heise U, Reichardt P, Tunn PU. The influence of tumor- and treatment-related factors on the development of local recurrence in osteosarcoma after adequate surgery: an analysis of 1355 patients treated on neoadjuvant Cooperative Osteosarcoma Study Group protocols. Ann Oncol. 2011;22:1228–1235. doi: 10.1093/annonc/mdq589. [DOI] [PubMed] [Google Scholar]
- 3.Anninga JK, Gelderblom H, Fiocco M, Kroep JR, Taminiau AH, Hogendoorn PC, Egeler RM. Chemotherapeutic adjuvant treatment for osteosarcoma: where do we stand? Eur J Cancer. 2011;47:2431–2445. doi: 10.1016/j.ejca.2011.05.030. [DOI] [PubMed] [Google Scholar]
- 4.Ayerza MA, Farfalli GL, Aponte-Tinao L, Muscolo DL. Does increased rate of limb-sparing surgery affect survival in osteosarcoma? Clin Orthop Relat Res. 2010;468:2854–2859. doi: 10.1007/s11999-010-1423-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Canadell J, Forriol F, Cara JA. Removal of metaphyseal bone tumours with preservation of the epiphysis: physeal distraction before excision. J Bone Joint Surg Br. 1994;76:127–132. [PubMed] [Google Scholar]
- 6.Enneking WF, Dunham W, Gebhardt MC, Malawer M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246. [PubMed] [Google Scholar]
- 7.Fang B, Yi C, Zhang H, Zhang Q, Li Y, Wei Q, He W, Zeng Z. [Combined epiphyseal preservation and autograft bone transfer in treatment of children osteosarcoma][in Chinese] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2013;27:45–49. [PubMed] [Google Scholar]
- 8.Ferrari S, Ruggieri P, Cefalo G, Tamburini A, Capanna R, Fagioli F, Comandone A, Bertulli R, Bisogno G, Palmerini E, Alberghini M, Parafioriti A, Linari A, Picci P, Bacci G. Neoadjuvant chemotherapy with methotrexate, cisplatin, and doxorubicin with or without ifosfamide in nonmetastatic osteosarcoma of the extremity: an Italian sarcoma group trial ISG/OS-1. J Clin Oncol. 2012;30:2112–2118. doi: 10.1200/JCO.2011.38.4420. [DOI] [PubMed] [Google Scholar]
- 9.Han G, Wang Y, Bi WZ, Wang DJ, Lu SB, Zhang L, Zhao B. Magnetic resonance imaging is appropriate for determining the osteotomy plane for appendicular osteosarcoma after neoadjuvant chemotherapy. Med Oncol. 2012;29:1347–1353. doi: 10.1007/s12032-011-9861-8. [DOI] [PubMed] [Google Scholar]
- 10.Hoffer FA, Nikanorov AY, Reddick WE, Bodner SM, Xiong X, Jones-Wallace D, Gronemeyer SA, Rao BN, Kauffman WM, Laor T. Accuracy of MR imaging for detecting epiphyseal extension of osteosarcoma. Pediatr Radiol. 2000;30:289–298. doi: 10.1007/s002470050743. [DOI] [PubMed] [Google Scholar]
- 11.Jaffe N, Puri A, Gelderblom H. Osteosarcoma: evolution of treatment paradigms. Sarcoma. 2013;2013:203531. doi: 10.1155/2013/203531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeon DG, Song WS, Kong CB, Cho WH, Cho SH, Lee JD, Lee SY. Role of surgical margin on local recurrence in high risk extremity osteosarcoma: a case-controlled study. Clin Orthop Surg. 2013;5:216–224. doi: 10.4055/cios.2013.5.3.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 14.Kumta SM, Chow TC, Griffith J, Li CK, Kew J, Leung PC. Classifying the location of osteosarcoma with reference to the epiphyseal plate helps determine the optimal skeletal resection in limb salvage procedure. Arch Orthop Trauma Surg. 1999;119:327–331. doi: 10.1007/s004020050420. [DOI] [PubMed] [Google Scholar]
- 15.Manfrini M, Gasbarrini A, Malaguti C, Ceruso M, Innocenti M, Bini S, Capanna R, Campanacci M. Intraepiphyseal resection of the proximal tibia and its impact on lower limb growth. Clin Orthop Relat Res. 1999;358:111–119. doi: 10.1097/00003086-199901000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Muscolo DL, Ayerza MA, Aponte-Tinao LA, Ranalletta M. Partial epiphyseal preservation and intercalary allograft reconstruction in high-grade metaphyseal osteosarcoma of the knee. J Bone Joint Surg Am. 2004;86:2686–2693. doi: 10.2106/00004623-200412000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Muscolo DL, Ayerza MA, Aponte-Tinao LA, Ranalletta M. Partial epiphyseal preservation and intercalary allograft reconstruction in high-grade metaphyseal osteosarcoma of the knee. J Bone Joint Surg Am. 2005;87(suppl 1):226–236. doi: 10.2106/JBJS.E.00253. [DOI] [PubMed] [Google Scholar]
- 18.Norton KI, Hermann G, Abdelwahab IF, Klein MJ, Granowetter LF, Rabinowitz JG. Epiphyseal involvement in osteosarcoma. Radiology. 1991;180:813–816. doi: 10.1148/radiology.180.3.1871299. [DOI] [PubMed] [Google Scholar]
- 19.O’Flanagan SJ, Stack JP, McCee HM, Dervan P, Hurson B. Imaging of intramedullary tumor spread in osteosarcoma: a comparison of techniques. J Bone Joint Surg Br. 1991;73:998–1001. doi: 10.1302/0301-620X.73B6.1955451. [DOI] [PubMed] [Google Scholar]
- 20.Onikul E, Fletcher BD, Parham DM, Chen G. Accuracy of MR imaging for estimating intraosseous extent of osteosarcoma. AJR Am J Roentgenol. 1996;167:1211–1215. doi: 10.2214/ajr.167.5.8911182. [DOI] [PubMed] [Google Scholar]
- 21.Saifuddin A. The accuracy of imaging in the local staging of appendicular osteosarcoma. Skeletal Radiol. 2002;31:191–201. doi: 10.1007/s00256-001-0471-y. [DOI] [PubMed] [Google Scholar]
- 22.San Julian M, Aquerreta JD, Benito A, Cañadell J. Indications for epiphyseal preservation in metaphyseal malignant bone tumors of children: relationship between image methods and histological findings. J Pediatr Orthop. 1999;19:543–548. doi: 10.1097/01241398-199907000-00025. [DOI] [PubMed] [Google Scholar]
- 23.Thompson RC, Jr, Cheng EY, Clohisy DR, Perentesis J, Manivel C, Le CT. Results of treatment for metastatic osteosarcoma with neoadjuvant chemotherapy and surgery. Clin Orthop Relat Res. 2002;397:240–247. doi: 10.1097/00003086-200204000-00028. [DOI] [PubMed] [Google Scholar]
- 24.Tsuchiya H, Abdel-Wanis ME, Sakurakichi K, Yamashiro T, Tomita K. Osteosarcoma around the knee: intraepiphyseal excision and biological reconstruction with distraction osteogenesis. J Bone Joint Surg Br. 2002;84:1162–1166. doi: 10.1302/0301-620X.84B8.13330. [DOI] [PubMed] [Google Scholar]
- 25.Weitao Y, Qiqing C, Songtao G, Jiaqiang W. Epiphysis preserving operations for the treatment of lower limb malignant bone tumors. Eur J Surg Oncol. 2012;38:1165–1170. doi: 10.1016/j.ejso.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 26.Yao W1, Cai Q, Gao S, Wang J, Zhang P, Wang X. [Epiphysis preserving by physeal distraction for treatment of femur osteosarcoma in children][in Chinese]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2013;27:423–427. [PubMed]
- 27.Yu XC, Xu M, Xu SF, Song RX. Long-term outcomes of epiphyseal preservation and reconstruction with inactivated bone for distal femoral osteosarcoma of children. Orthop Surg. 2012;4:21–27. doi: 10.1111/j.1757-7861.2011.00167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]




