Abstract
Objectives
Most U.S. hospitals lack primary percutaneous coronary intervention (PCI) capabilities to treat patients with ST-elevation myocardial infarction (STEMI) necessitating transfer to PCI-capable centers. Transferred patients rarely meet the 120-minute benchmark for timely reperfusion and referring EDs are a major source of preventable delays. We sought to use more granular data at transferring EDs to describe the variability in length of stay at referring EDs.
Methods
We retrospectively analyzed a secondary dataset used for quality improvement for patients with STEMI transferred to a single PCI center between 2008 and 2012. We conducted a descriptive analysis of the total time spent at each referring ED (door-in-door-out [DIDO] interval), time periods that comprised DIDO (door-to-EKG, EKG-to-PCI activation, and PCI activation-to-exit), and the relationship of each period with overall time to reperfusion (medical contact-to-balloon [MCTB] interval).
Results
We identified 41 EDs that transferred 620 patients between 2008 and 2012. Median MCTB was 135 minutes (IQR 114,172). Median overall ED DIDO was 74 minutes (IQR 56,103) and was comprised of: door-to-EKG 5 minutes (IQR 2,11), EKG-to-PCI activation 18 minutes (IQR 7,37), and PCI activation-to-exit 44 minutes (IQR 34,56). DIDO accounted for the largest proportion (60%) of overall MCTB and had the largest variability (coefficient of variability=1.37) of these intervals.
Conclusions
In this cohort of transferring EDs, we found high variability and substantial delays after EKG performance for patients with STEMI. Factors influencing ED decision-making and transportation coordination following PCI activation are a potential target for intervention to improve the timeliness of reperfusion in patients with STEMI.
INTRODUCTION
Timely reperfusion of ischemic myocardium is an important predictor of clinical outcomes for patients with ST-elevation myocardial infarction (STEMI).1 The preferred reperfusion strategy is primary percutaneous coronary intervention (PCI),2 yet, the majority of U.S. healthcare facilities lack primary PCI capabilities necessitating inter-facility transfer.3 Unlike patients with STEMI who directly present to a facility with PCI capabilities, transferred patients rarely achieve timely reperfusion due to delays in the transfer process.
Two process measures quantify the timeliness of care for patients with STEMI. Door-in-door-out (DIDO) measures the length of stay at a transferring ED. Maximum time goals are between 30 and 45 minutes but neither was officially recommended in the latest STEMI guidelines.2 Medical-contact-to-balloon (MCTB) measures the time from original contact at the transferring ED through myocardial reperfusion at the PCI center. The goal is for 90% of patients to achieve reperfusion within 120 minutes of first medical contact.2 While similar to the door-to-balloon process measure which applies to direct presenters and has a 90 minute goal, MCTB only applies to transferred patients with STEMI.2
Most patients presenting directly to primary PCI facilities meet the 90 minute door-to-balloon goal for timely reperfusion.4 However, patients with STEMI requiring transfer, up to 45% in some regions,5,6 meet reperfusion goals for approximately 10% of transfers.7,8 Compared with direct presenters, transferred patients experience significantly longer MCTB times and may benefit from targeted process improvement interventions designed to reduce delays to primary PCI.9
The ED plays a central role in the timely care of patients with STEMI. Transferred patients who spent ≤ 30 minutes at a transferring ED (ie, DIDO) had a lower in-hospital mortality rate.10 Most preventable delays occur at referring EDs (64%) rather than during transportation (13%) or the receiving PCI centers (16%).11 The 30 minute DIDO goal is only met for approximately 11% of transferred patients with STEMI.10,12 Prioritizing process improvement efforts to reduce DIDO requires detailed measurements of the process steps at transferring EDs. However, collecting high quality process data across multiple organizations can be challenging further limiting analysis and process improvement efforts.
Large datasets (eg, ACTION Registry® and the Center for Medicare and Medicaid Service's [CMS] Hospital Compare) collect limited process data on inter-facility STEMI transfers. Detailed process timestamps enable the ability to pinpoint where and when delays occur and to better explain why delays occur in the transfer process. The ACTION Registry® records only three timestamps of process steps at referring EDs: patient arrival, electrocardiogram (EKG) performed, and exit. As a result, only two time intervals (ie, door-to-EKG and EKG-to-exit) can be calculated to describe the referring ED length of stay. One of the activities and its associated interval, door-to-EKG, was already targeted by national process improvement efforts, and is also part of the latest STEMI guidelines.2,13 Efforts to quickly perform an EKG have improved the door-to-EKG interval and now represents a minor fraction of overall DIDO. The remaining time interval available in ACTION®, EKG-to-exit, represents a large time period that encompasses multiple processes including PCI center activation, patient preparation for transfer, transportation coordination, and exit from the referring ED.
The Centers for Medicare and Medicaid Services Hospital Compare database provides even less detail than the ACTION Registry®. Hospital Compare reports OP-3B, Median Time to Transfer to Another Facility for Acute Coronary Intervention, a measure equivalent to DIDO. No additional timestamps are available about referring ED length of stay. Therefore, these two datasets provide little detail to adequately describe the processes that occur at referring EDs.
Further dissection of the processes after the performance of an EKG in patients with STEMI may enhance our understanding of this time period, better identify potential sources of delays and prioritize process improvement efforts. To conduct such an analysis, we used an existing quality improvement hospital dataset tracking patients with STEMI transferred to Vanderbilt University Medical Center (VUMC) for primary PCI. We then discuss implications for evaluating referring ED performance and intervening to improve it.
METHODS
Study Design and Population
We used an existing cohort of patients with STEMI who were transferred to a single primary PCI center (VUMC), for our analyses. Originally developed in 2007 as part of an ongoing quality improvement initiative, the STEMI Transfer database began data collection in the fourth quarter of 2007. We received separate IRB approval from the Vanderbilt University Institutional Review Board for this study.
Even if patients with STEMI bypassed the ED, the transfer database includes all patients with STEMI who were transferred to VUMC for primary PCI. For the present analysis, we included only patients with STEMI transferred between January 1, 2008 and December 31, 2012. We excluded patients who received fibrinolytics which are recommended when the anticipated delay to primary PCI is ≥ 120 minutes.2 We excluded “scene STEMI” patients transported directly to VUMC from the field bypassing a referring ED. Finally, we excluded patients who did not have complete referring ED time interval data (ie, DIDO).
Data Collection
Documents providing details and timing of care prior to and at VUMC are regularly collected and scanned into the VUMC electronic health record (EHR). A clinical study nurse then uses the VUMC EHR to complete a data dictionary and case report form with REDCap™ (Research Electronic Data Capture),14 a secure browser-based metadata-driven electronic data capture tool. If data were not available, the clinical study nurse attempted to collect records from the referring facilities and transporting agencies. Operational data included: emergency medical services (EMS), referring hospital, cardiac catheterization laboratory and transportation interval timestamps. Clinical data included presenting symptoms, demographics, past medical history, procedures, in-hospital outcomes, originating facility and distance (using Google Maps) to VUMC.
Data Analysis
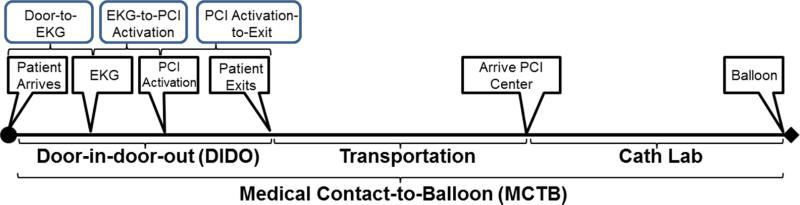
For the present study, data were provided as a de-identified dataset. Time intervals were pre-calculated as the difference between two timestamps in order to remove protected health information. We deconstructed DIDO according to the following time intervals for care at the referring ED: door-to-EKG, EKG-to-PCI activation, and PCI activation-to-exit as seen in Figure 1. Each time interval was calculated using the following approach. The door-to-EKG interval was calculated as the maximum of the door-to-EKG interval or zero. Values were set to zero if the door-to-EKG interval was negative suggesting that the EKG was performed prior to arrival at the ED. The EKG-to-PCI activation interval was calculated as the door-to-PCI activation minus the calculated door-to-EKG interval. Finally, the PCI activation-to-exit interval was calculated as the overall ED LOS (ie, DIDO) minus the door-to-PCI activation interval. We did not perform imputation for missing transportation and Cath Lab values.
Figure 1.
A timeline of the time period from initial medical contact through myocardial reperfusion including timestamps at the referring ED and resulting intervals.
We used an established zone classification system to distinguish facilities by distance.15 Zone 1 facilities are < 60 miles from the PCI center and zone 2 facilities are between 60 miles and 210 miles from the PCI center. We also quantified the number of STEMIs transferred by facilities for each year.
To evaluate whether transferred patient demographics and timeliness changed during the study period, we calculated and compared patient populations and timeliness performance using Kruskal-Wallis (for continuous variables) and Pearson's chi-square tests (for categorical variables). Significance was set a priori at 0.05. For the seven time intervals, we corrected for multiple comparisons using the Bonferroni method with a revised significance level of 0.007 (0.05/7). Next, to quantify differences in referring ED timeliness, analyses included both numeric and graphical methods to detail the distribution of DIDO component intervals and total time. Quartiles, means, and standard deviation were calculated to describe the distributions. Histograms and box-plots were used to graphically compare the distribution of component time periods to identify those with greater variability, and those intervals accounting for a larger proportion of overall ED DIDO. To quantify variability we calculated the coefficient of variation for time intervals.16 We stratified our analyses by time (year), and distance (zone). To evaluate the effect of missing transportation and Cath Lab values on our results, we performed a sensitivity analysis where only patients with complete data for every possible timestamp were included. Finally, rank-based Spearman correlation coefficients were calculated between patient-level factors (age, gender, body mass index [BMI] and race) and time intervals. Statistical analyses were conducted using R 2.14.1.
RESULTS
Characteristics of Study Subjects and Setting
Between 2008 and 2012, we identified 620 patients with STEMI from 41 facilities who were transferred from a referring ED to VUMC for primary PCI. Table 1 describes the patients and facilities. The distribution of patients transferred by facility is represented in Figure 2. A flow chart of patients meeting inclusion/exclusion criteria can be seen in Figure 3. Patients had a median age of 59.3 (IQR 50.4, 69.0). Of the 620 patients, 21% were female, 45% were white, 31% had private insurance and 25% had government insurance (ie, Medicare or Medicaid). The majority of our study population (69%) presented to facilities in zone 1 (< 60 miles), and most of the study population (71%) was transported to the PCI center by helicopter.
Table 1.
Characteristics of transferred STEMI patients and facilities transferring patients.
| Patient characteristics (N=620) | |
|---|---|
| Age, median (IQR), y | 59.3 (50.4,69.0) |
| Sex (% Female) | 21.3 |
| Race (% White) | 45.0 |
| Insurance | |
| Medicare (%) | 20.8 |
| Medicaid (%) | 5.0 |
| Private (%) | 31.5 |
| Self Pay (%) | |
| Presentation by Year | |
| 2008 (%) | 14.8 |
| 2009 (%) | 23.4 |
| 2010 (%) | 23.2 |
| 2011 (%) | 19.7 |
| 2012 (%) | 18.9 |
| Time Intervals, median (IQR), minutes | |
| MCTB | 135 (114,172) |
| DIDO | 74 (56,103) |
| Door-to-EKG | 5 (2,11) |
| EKG-to-PCI Activation | 18 (7,37) |
| PCI Activation-to-Exit | 44 (34,56) |
| Transportation | 31 (22,42) |
| Cath Lab | 30 (23,37) |
| Initial presentation to Zone 1 hospital (%) | 64.1 |
| Helicopter Transportation to PCI Center (%) | 71.4 |
| Facility Characteristics (N=41) | |
|---|---|
| Overall STEMIs transferred by ED, median (IQR) | 6 (2,22) |
| Distance from PCI, median (IQR), miles | 47.2 (33.8,64.7) |
Note: DIDO, door-in-door-out; EKG, electrocardiogram; IQR, inter-quartile range; MCTB, Medical Contact-to-Balloon; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
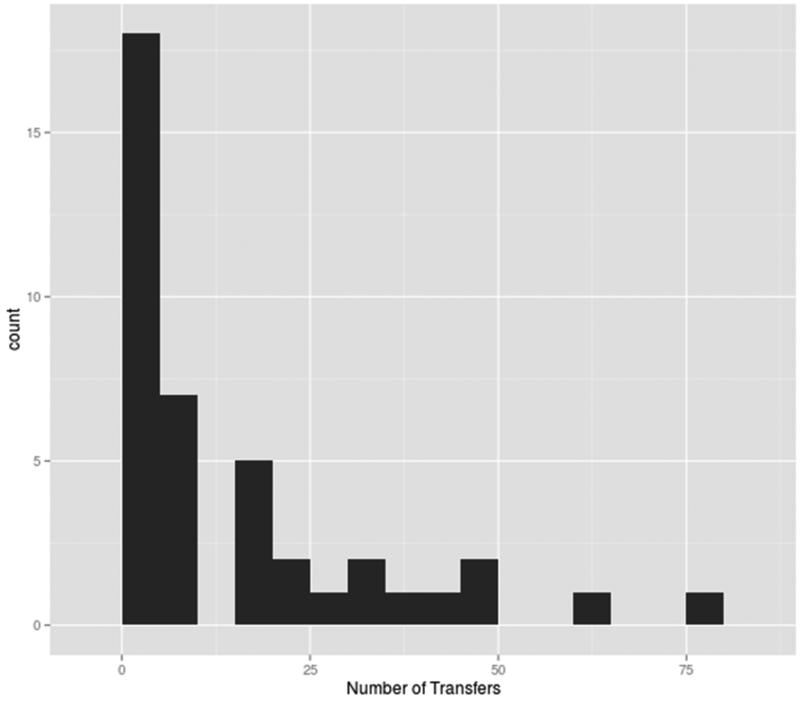
Figure 2.
The distribution of the number of STEMI transfers by referring ED to Vanderbilt University Medical Center between 2008 and 2012.
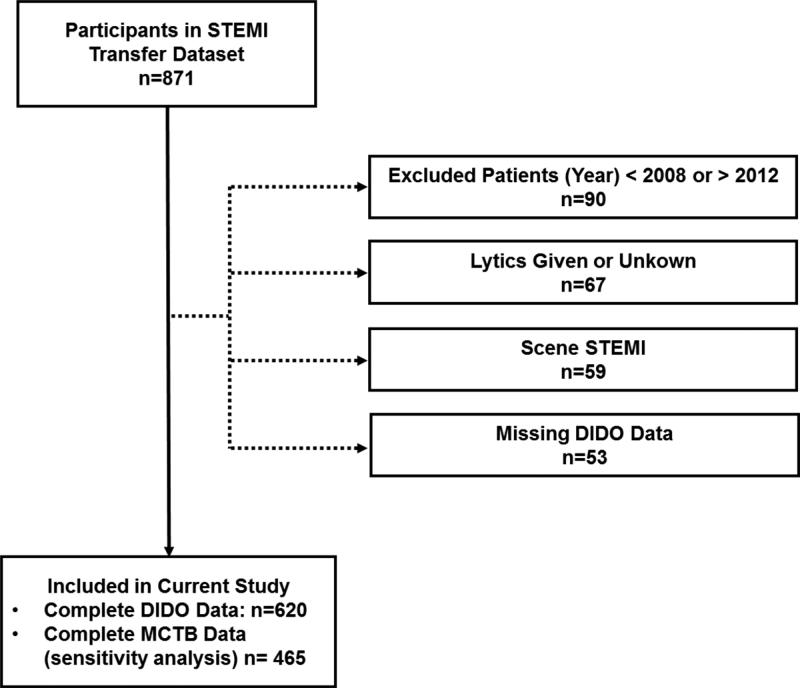
Figure 3.
Flow chart of patients who met inclusion/exclusion criteria for the study population.
Note: Some cases may have been excluded for more than one reason.
Transferred patients arrived from a median distance of 47 miles (IQR 38, 64) in 2008, 47 miles (IQR 32, 65) in 2010, and 53 miles (IQR 38, 73) in 2012 (p<0.001). There was no difference across years in the proportion of patients transported by helicopter with 75% in 2008, 66% in 2010, and 80% in 2012 (p=0.1).
For patients with transfer distance recorded in the dataset (n=594, Appendix Table 1), fewer patients with STEMI presented to zone 2 (31.1%), were more likely to be white in zone 2 compared to zone 1 (56.2% vs. 40.1%; p< 0.001), but were otherwise not different in age (p=0.1) or gender (p=0.2). Zone 2 patients were more likely to have private insurance (40.5% vs. 27.4%, p=0.001) and Medicare (25.9% vs. 18.8%; p=0.05) but were no different in the proportion of patients with Medicaid (p=0.8), as compared with zone 1. Zone 2 patients were more likely to be transferred by helicopter (86.5%) compared with zone 1 (64.1%; p<0.001).
Main Results
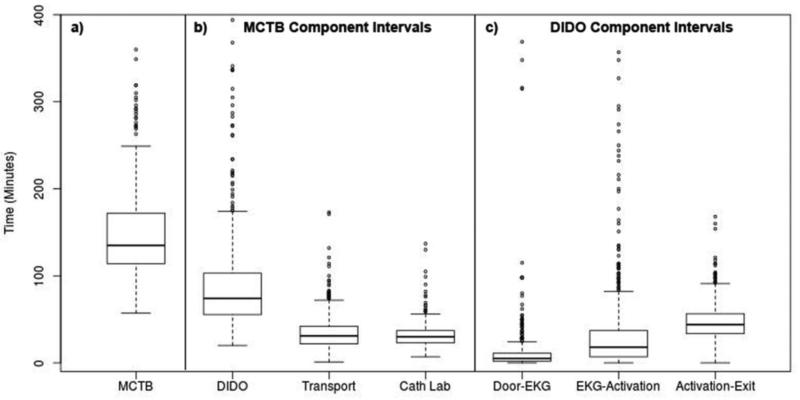
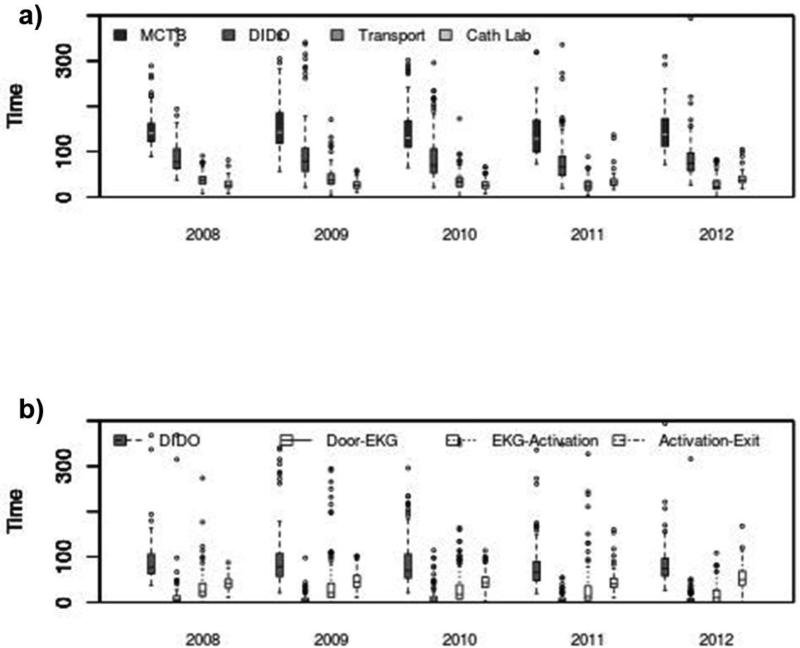
Both overall and year-to-year performance of referring EDs is reported in Table 2 and is further depicted in Figure 4. Median overall MCTB (Figure 4a) was 135 minutes (IQR 114, 172). Among the time intervals that constitute MCTB (Figure 4b), the median overall DIDO was 74 minutes (IQR 56,103), the median overall transportation time between the referring ED and PCI center was 31 minutes (IQR 22, 42), and the median Cath Lab time (ie, overall time spent at the PCI center until reperfusion) was 30 minutes (IQR 23, 37). Using means, DIDO comprised the largest proportion (60.0%) of MCTB compared with the transportation interval (21.1%) and Cath Lab interval (18.9%). DIDO also had the largest variability among the three MCTB intervals with a coefficient of variation of 1.37 compared with 0.71 and 0.44 for the transportation and Cath Lab time intervals, respectively. Within the intervals that comprise DIDO at the referring EDs (Figure 4c), the median door-to-EKG time interval was 5 minutes (IQR 2, 11), the median EKG-to-PCI activation time interval was 18 minutes (IQR 7, 37), and the median PCI activation-to-exit interval was 44 minutes (IQR 34, 56). Using means, the door-to-EKG interval was 16.0% of DIDO, EKG-to-PCI activation was 36.6% of DIDO and the PCI activation-to-exit interval was the largest with 47.5% of overall DIDO.
Table 2.
Time intervals by year. Times are medians with interquartile ranges reported in minutes.
| Time Interval, min (IQR)* | 2008 (N=92) | 2009 (N=145) | 2010 (N=144) | 2011 (N=122) | 2012 (N=117) | p value** |
|---|---|---|---|---|---|---|
| MCTB | 140 (123,162) | 143 (118,186) | 130 (110,168) | 128 (100,169) | 138 (112,172) | 0.04 |
| DIDO | 77 (64,106) | 79 (57,108) | 70 (54,106) | 66 (48,90) | 75 (58,97) | 0.04 |
| Door-to-EKG | 6 (3,14) | 5 (2, 9) | 6 (2,12) | 4 (2,9) | 5 (2,8) | 0.03 |
| EKG-to-PCI Activation | 24 (14,42) | 21 (11,42) | 17 (8,39) | 13 (5,35) | 10 (1,27) | <0.001 |
| PCI Activation-to-Exit | 42 (32,51) | 45 (34,59) | 43 (33,55) | 41 (33,53) | 50 (38,69) | 0.001 |
| Transportation | 38 (29,46) | 37 (29,51) | 34 (23,43) | 24 (16,35) | 23 (18,36) | <0.001 |
| Cath Lab | 25 (21,34) | 26 (20,33) | 26 (20,33) | 32 (27,39) | 37 (32,46) | <0.001 |
Note1: DIDO, door-in-door-out; EKG, electrocardiogram; IQR, interquartile range; MCTB, Medical Contact-to-Balloon; PCI, percutaneous coronary intervention.
Note 2: Sample size available by interval to calculate duration: MCTB (465), DIDO (620), EKG-to-PCI Activation (620), PCI Activation-to-Exit (620), Transportation (619), Cath Lab (465).
p value following multiple comparisons is 0.007
Figure 4.
Box whisker plot of time intervals, in minutes, for patients transferred for primary PCI. a) shows overall medical contact-to-balloon (MCTB) and b) MCTB component intervals; c) shows component intervals that constitute DIDO times at the referring EDs. The boxes represent the interquartile range (IQR); the dark bar within the boxes represents the median value. The whiskers represent 1.5 times the IQR from the box. Outliers are values beyond the whiskers and are shown as circles (o). Outliers ≥400 minutes were trimmed for better visualization.
When evaluating time intervals during the five-year study period, several patterns emerge (Table 2, and Figure 5). Following correction for multiple comparisons with an adjusted level of significance of 0.007, MCTB (p=0.04), DIDO (p=0.04), and the door-to-EKG (p=0.03) intervals were not different across the study period. However, the median EKG-to-PCI activation interval did change across the study period with a median of 24 minutes in 2008 (IQR 14, 42), 17 minutes in 2010 (IQR 8, 39) and 10 minutes (IQR 1, 27) in 2012 (p<0.001). In addition, the median PCI activation-to-exit in 2008 of 42 minutes (IQR 32, 51), 43 minutes in 2010 (IQR 33, 55) and 50 minutes (IQR 38, 69) in 2012 (p=0.001) and the median transportation time of 38 minutes (IQR 29,46) in 2008, 34 minutes in 2010 (IQR 23, 43), and 23 minutes (IQR 18,36) in 2012 (p<0.001) all changed across the study period. Finally, the median Cath Lab time changed from 25 minutes (IQR 21, 34) in 2008, 26 minutes in 2010 (IQR 20, 33), and to 37 minutes (IQR 32, 46) in 2012 (p<0.001).
Figure 5.
Intervals for referring ED performance by year for a) medical contact to balloon (MCTB), door-in-door-out (DIDO) at the referring ED, transportation to the PCI center, and time spent at the PCI center prior to reperfusion; b) intervals that comprise referring ED performance.
When analyzed with respect to zone (Appendix Table 1), using the adjusted significance level of 0.007, median MCTB was longer in zone 2 compared with zone 1 (156 [IQR 131, 200] vs. 124 minutes [IQR 105, 155], p<0.001). In zone 2, the median DIDO was longer (81 [IQR 61, 109] vs. 69 minutes, [IQR 53, 95] p<0.001), the median PCI activation-to-exit interval was longer (49 [IQR 40, 64] vs. 40 minutes [IQR 30, 53], p< 0.001) and the median transportation interval was longer (42 [IQR 36, 51] vs. 26 minutes [IQR 19, 35], p<0.001). However, the door-to-EKG (p=0.02), EKG-to-PCI activation (p=0.08) and the Cath Lab interval (p=0.02) durations were no different for patients transferred from zone 2 facilities.
A sensitivity analysis of this dataset including only subjects with complete data for every timestamp (n=465) confirmed the findings using complete DIDO timestamp data. Last, we did not identify any significant correlations between patient factors (age, gender, race and BMI) with time intervals (Appendix Table 2).
DISCUSSION
Our investigation makes the novel contribution that the EKG-to-PCI activation and PCI activation-to-exit intervals at referring EDs exhibited high variability across the five-year study period. These two intervals encompass multiple tasks including: STEMI diagnosis, activation of the cardiac catheterization laboratory, coordination with EMS and the PCI center, and departure from the ED. While the EKG-to-PCI activation interval is shorter, it has more variability than the PCI activation-to-exit interval. Although distinct from each other, both intervals represent potential intervention targets to improve the timeliness of transfer for patients with STEMI.
Several factors may contribute to the high variability seen in the EKG-to-PCI activation interval. Shortly before our study period began, studies and guidelines formally recognized the critical role of the ED and emergency physicians in rapid myocardial reperfusion. Empowerment of the ED and its physicians to activate the cardiac catheterization laboratory was recommended as a strategy to improve reperfusion timeliness.13,17 Activating the cardiac catheterization laboratory applies to both transferred and non-transferred patients since they share similar processes. Implementing these recommendations combined with a delay in diffusion of knowledge may contribute to the variability seen in the EKG-to-PCI activation interval during the five-year study period.18 In addition, the degree to which the included hospitals empower their EDs and emergency physicians may also affect the variability we identified.
The next time interval, PCI activation-to-exit, includes processes that occur following the activation of the PCI center. Unlike the preceding interval, the time after PCI center activation differs between facilities with and without PCI capabilities. The time after PCI center activation for transferred patients involves coordination of care among the referring ED, the transporting EMS agency and the receiving PCI center. If not already present, the transferring EMS agencies must dispatch, and subsequently arrive at the referring ED. Further complicating this process is the physical distance between the referring ED and the PCI center. Facilities in zone 2 (ie, 60 to 210 miles from PCI center) had a 10 minute longer PCI activation-to-exit interval representing the entire difference in DIDO between the two zones. This difference may be explained by the longer distance from the PCI center and the increased use of helicopters. The use of helicopters for transport of patients with STEMI is associated with increased delays in inter-facility transfer for primary PCI.19-21 While helicopters can travel faster, deployment time including both start-up and shut down of helicopters, may outweigh the faster travel time.
The variability and delays following PCI activation may also be affected by the substantial investment needed to coordinate patient care with EMS, a complex, yet necessary activity among high performing health systems.22 Delays associated with EMS deployment time may affect the reliability and time to response at transferring EDs. The substantial differences in the structure and performance of EMS systems of STEMI care in the U.S. may also inhibit optimal performance.23 Given the variability and magnitude of duration, the time after PCI activation likely represents the largest opportunity for process improvement.
While the interval after PCI activation may be the largest in magnitude, the physical distance between two facilities is fixed. Therefore, interventions that enhance the efficiency and coordination of the transferring ED and transporting EMS agencies are needed. Multiple strategies hold promise. For example, activating EMS transportation prior to PCI center activation,24 using the 911 system to transfer patients,25 using operations research tools to enhance the operational flexibility of the ED,26,27 enhancing regionalization efforts to reduce EMS response times,28,29 standardizing the initial interaction with EMS (eg, patient staying on the stretcher),24 enhancing hospital-EMS relationships,22 and appropriate use of ground-based (rather than helicopter) EMS.19,20
Reducing variability at referring EDs may also be complicated by fewer STEMIs being seen in U.S. EDs. A study using the National Emergency Department Sample found that STEMI is decreasing in U.S. EDs.30 How this affects timeliness performance as emergency providers see fewer STEMIs is unknown. However, less experience may result in more variability and subsequently more delays at referring EDs. In addition, fewer STEMIs in U.S. EDs may also affect an ED's decision to transfer a patient with STEMI. As providers are less experienced in handling such patients, they may be more inclined to transfer to specialized centers of care further affecting their proficiency in handling the transfer process.
In summary, among patients transferred to a single PCI center for STEMI care, there was high variation and lengthy time durations within the referring community hospitals’ EDs both following the performance of an EKG prior to PCI activation and following PCI activation until ED exit. These results suggest that ED decision-making and coordination of transportation following PCI activation are potential targets for improving care. The identification and sharing of current best practices, utilization of quality improvement methods and additional studies to better understand causal factors for delays and the effectiveness of interventions to minimize delays should be pursued.
LIMITATIONS
Our results must be considered in light of several limitations. The current study was a secondary analysis on a dataset that was established for the primary purpose of quality improvement on inter-facility STEMI transfer timeliness. Consequently, although the analysis explores timeliness of transfers and generates hypotheses about the variability and duration of time intervals at referring EDs, the data has shortcomings when used for research on the timing of processes at referring EDs. Confirmation of our findings is needed using rigorous prospective data collection on timing of events and the patient, provider, and ED- and patient-level (eg, case-mix) factors contributing to patient care, transfer decisions along with clinical outcomes for these patients.
In addition, only the time duration and not the actual timestamps were available in this dataset. The use of time durations might interfere with accurate calculation of specific time intervals. For example, 12 negative values ranged from -8 to -1 were observed for door-to-EKG time interval. This might be explained as a result of the EKG being performed by EMS before the patient arrival. Since the EKG-to-PCI activation interval was not provided and had to be calculated as door-to-PCI activation (provided in the secondary data) minus door-to-EKG, negative values of door-to-EKG time interval were set to zero during data cleaning. However, the effect of this operation on the accuracy of specific time interval is minimal due to the sample size, the magnitude of negative values and the lack of change in our results when we conducted a sensitivity analysis using complete timestamp data for all process.
Last, our study involved only a single PCI center limiting the generalizability of our findings. Other settings may have a distinct patient population, processes that differ by PCI center, may use helicopter transportation to a different degree, or may have a different relationship with their referring EDs. However, our study included a broad group of referring EDs and our results are consistent with national findings of inter-facility transfer delays for PCI. Thus, we are encouraged that our findings are indicative of national trends on the timeliness performance of inter-facility transfers for patients with STEMI. Considering the original purpose of this study was to explore the use of more granular operational data, future studies will need to be conducted in other settings to examine the representativeness of our findings.
CONCLUSIONS
In a single catchment area, the time after PCI activation at referring EDs was a substantial source of variability and delay in transfer of patients with STEMI. More granularity in the time after PCI center activation refines our understanding of when delays occur during the STEMI transfer process and may represent an opportunity to measure and to understand how facilities differ in their performance during this time. Additional studies are needed to identify why these delays occur and the effectiveness of interventions to minimize delays.
Acknowledgments
Disclosures: The project described was supported by Award Number K12 HL109019 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
The project publication described was supported by CTSA award No. UL1TR000445 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Appendix
Appendix Table 1.
Patient and Facility Demographics by Zone from PCI Center.
| Patient Characteristics | ||||||
|---|---|---|---|---|---|---|
| <60 Miles N=409 | ≥60 Miles N=185 | p value | ||||
| Age, median (IQR), y | 59 (50,68) | 61 (51,70) | 0.1 | |||
| Sex (% Female) | 19.6 | 24.3 | 0.2 | |||
| Race (% White) | 40.1 | 56.2 | <0.001 | |||
| Insurance (%) | ||||||
| Medicare | 18.8 | 25.9 | 0.05 | |||
| Medicaid | 4.89 | 5.4 | 0.8 | |||
| Private | 27.4 | 40.5 | 0.001 | |||
| Self Pay | 9.53 | 10.3 | 0.8 | |||
| Helicopter Transportation (%) | 64.1 | 86.5 | <0.001 | |||
| Time Intervals, median (IQR), minutes* | ||||||
| MCTB | 124 (105,155) | 156 (131,200) | <0.001 | |||
| DIDO | 69 (53, 95) | 81 (61,109) | <0.001 | |||
| Door-to-EKG | 5 (2,12) | 5 (2,9) | 0.1 | |||
| EKG-to-PCI Activation | 16 (6,36) | 19 (9,36) | 0.08 | |||
| PCI Activation-to-Exit | 40 (30, 53) | 49 (40,64) | <0.001 | |||
| Transportation | 26 (19,35) | 42 (36,51) | <0.001 | |||
| Cath Lab | 29 (22,36) | 32 (24,39) | 0.02 | |||
| Facility Characteristics | ||||||
| Distance from PCI, median (IQR), miles | 45 (32,53) | 79 (68,90) | <0.001 | |||
Note: DIDO, door-in-door-out; EKG, electrocardiogram; IQR, inter-quartile range; MCTB, Medical Contact-to-Balloon; PCI, percutaneous coronary intervention.
Sample size available by interval to calculate duration: MCTB (465), DIDO (620), EKG-to-PCI Activation (620), PCI Activation-to-Exit (620), Transportation (619), Cath Lab (465).
Appendix Table 2.
Correlation matrix for time intervals and patient factors at the patient level. Values in the upper right (dark gray) represent correlations. Values in the lower left (light gray) are p values.
| Variable | MCTB | DIDO | Transport | Cath Lab | Door-to-EKG | EKG-to-Activation | Activation-to-Exit | Number of Transfers | Gender | Age | White | BMI |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MCTB | 1 | 0.90 | 0.41 | 0.37 | 0.25 | 0.58 | 0.53 | −0.32 | −0.15 | 0.08 | −0.11 | 0.09 |
| DIDO | <0.001 | 1 | 0.16 | 0.21 | 0.37 | 0.61 | 0.57 | −0.21 | −0.15 | 0.00 | −0.04 | 0.03 |
| Transport | <0.001 | <0.001 | 1 | −0.18 | −0.02 | 0.18 | 0.13 | −0.38 | −0.13 | 0.14 | −0.06 | −0.06 |
| Cath Lab | <0.001 | <0.001 | <0.001 | 1 | 0.06 | 0.08 | 0.18 | −0.06 | −0.03 | 0.10 | −0.16 | 0.03 |
| Door-to-EKG | <0.001 | <0.001 | 0.58 | 0.20 | 1 | −0.02 | 0.17 | 0.00 | −0.06 | 0.02 | 0.03 | 0.01 |
| EKG-to-Activation | <0.001 | <0.001 | <0.001 | 0.08 | 0.64 | 1 | −0.06 | −0.17 | −0.05 | 0.01 | 0.06 | 0.09 |
| Activation-to-Exit | <0.001 | <0.001 | 0.00 | 0.00 | <0.001 | 0.13 | 1 | −0.18 | −0.08 | 0.00 | −0.12 | −0.01 |
| Number of Transfers | <0.001 | <0.001 | <0.001 | 0.22 | 0.97 | <0.001 | <0.001 | 1 | 0.05 | −0.02 | 0.03 | 0.06 |
| Gender | 0.00 | 0.00 | 0.00 | 0.54 | 0.12 | 0.20 | 0.04 | 0.18 | 1 | −0.19 | 0.06 | 0.09 |
| Age | 0.12 | 0.92 | 0.00 | 0.05 | 0.56 | 0.77 | 0.93 | 0.59 | <0.001 1 | −0.03 | −0.20 | |
| White | 0.02 | 0.36 | 0.11 | 0.00 | 0.53 | 0.11 | 0.00 | 0.40 | 0.13 | 0.48 | 1 | 0.00 |
| BMI | 0.14 | 0.52 | 0.22 | 0.56 | 0.85 | 0.08 | 0.88 | 0.28 | 0.08 | 0.00 | 0.93 | 1 |
Note: BMI, body mass index; DIDO, door-in-door-out; EKG, electrocardiogram; IQR, inter-quartile range; MCTB, Medical Contact-to-Balloon; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Michael J. Ward, Department of Emergency Medicine Vanderbilt University School of Medicine 1313 21st Ave Nashville, TN 37232.
Sunil Kripalani, Section of Hospital Medicine, Division of General Internal Medicine and Public Health, Center for Clinical Quality and Implementation Research Vanderbilt University School of Medicine.
Alan B. Storrow, Department of Emergency Medicine Vanderbilt University School of Medicine.
Dandan Liu, Department of Biostatistics Vanderbilt University School of Medicine.
Theodore Speroff, Departments of Medicine and Biostatistics Division of General Internal Medicine and Public Health, Center for Health Services Research Vanderbilt University School of Medicine, Geriatric Research, Education, and Clinical Center, Veterans Affairs Tennessee Valley Healthcare System, Nashville, TN.
Michael Matheny, Departments of Biomedical Informatics and Medicine Division of General Internal Medicine and Public Health, Center for Health Services Research Vanderbilt University School of Medicine, Geriatric Research, Education, and Clinical Center, Veterans Affairs Tennessee Valley Healthcare System Nashville, TN.
Eric J. Thomassee, Division of Cardiology Vanderbilt University School of Medicine.
Timothy J. Vogus, Owen Graduate School of Management Vanderbilt University.
Daniel Munoz, Division of Cardiology Vanderbilt University School of Medicine.
Carol Scott, Division of Cardiology Vanderbilt University School of Medicine.
Joseph L. Fredi, Division of Cardiology Vanderbilt University School of Medicine.
Robert S. Dittus, Department of Medicine, Institute for Medicine and Public Health Vanderbilt University School of Medicine Geriatric Research, Education, and Clinical Center VA Tennessee Valley Healthcare System, Nashville, TN.
REFERENCES
- 1.Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283(22):2941–2947. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 2.O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(4):e362–425. doi: 10.1161/CIR.0b013e3182742cf6. [DOI] [PubMed] [Google Scholar]
- 3.Langabeer JR, Henry TD, Kereiakes DJ, et al. Growth in percutaneous coronary intervention capacity relative to population and disease prevalence. Journal of the American Heart Association. 2013;2(6):e000370. doi: 10.1161/JAHA.113.000370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Menees DS, Peterson ED, Wang Y, et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369(10):901–909. doi: 10.1056/NEJMoa1208200. [DOI] [PubMed] [Google Scholar]
- 5.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation. 2004;110(5):588–636. doi: 10.1161/01.CIR.0000134791.68010.FA. [DOI] [PubMed] [Google Scholar]
- 6.Jollis JG, Roettig ML, Aluko AO, et al. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA. 2007;298(20):2371–2380. doi: 10.1001/jama.298.20.joc70124. [DOI] [PubMed] [Google Scholar]
- 7.Chakrabarti A, Krumholz HM, Wang Y, Rumsfeld JS, Nallamothu BK, National Cardiovascular Data R. Time-to-reperfusion in patients undergoing interhospital transfer for primary percutaneous coronary intervention in the U.S: an analysis of 2005 and 2006 data from the National Cardiovascular Data Registry. Journal of the American College of Cardiology. 2008;51(25):2442–2443. doi: 10.1016/j.jacc.2008.02.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nallamothu BK, Bates ER, Herrin J, et al. Times to treatment in transfer patients undergoing primary percutaneous coronary intervention in the United States: National Registry of Myocardial Infarction (NRMI)-3/4 analysis. Circulation. 2005;111(6):761–767. doi: 10.1161/01.CIR.0000155258.44268.F8. [DOI] [PubMed] [Google Scholar]
- 9.Wang TY, Peterson ED, Ou FS, Nallamothu BK, Rumsfeld JS, Roe MT. Door-to-balloon times for patients with ST-segment elevation myocardial infarction requiring interhospital transfer for primary percutaneous coronary intervention: a report from the national cardiovascular data registry. Am Heart J. 2011;161(1):76–83. e71. doi: 10.1016/j.ahj.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Wang TY, Nallamothu BK, Krumholz HM, et al. Association of door-in to door-out time with reperfusion delays and outcomes among patients transferred for primary percutaneous coronary intervention. JAMA. 2011;305(24):2540–2547. doi: 10.1001/jama.2011.862. [DOI] [PubMed] [Google Scholar]
- 11.Miedema MD, Newell MC, Duval S, et al. Causes of delay and associated mortality in patients transferred with ST-segment-elevation myocardial infarction. Circulation. 2011;124(15):1636–1644. doi: 10.1161/CIRCULATIONAHA.111.033118. [DOI] [PubMed] [Google Scholar]
- 12.Herrin J, Miller LE, Turkmani DF, et al. National performance on door-in to door-out time among patients transferred for primary percutaneous coronary intervention. Arch Intern Med. 2011;171(21):1879–1886. doi: 10.1001/archinternmed.2011.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355(22):2308–2320. doi: 10.1056/NEJMsa063117. [DOI] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henry TD, Sharkey SW, Burke MN, et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116(7):721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 16.Bland M. An introduction to medical statistics. 3rd ed. Oxford University Press; Oxford ; New York: 2000. [Google Scholar]
- 17.Bradley EH, Nallamothu BK, Curtis JP, et al. Summary of evidence regarding hospital strategies to reduce door-to-balloon times for patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Critical pathways in cardiology. 2007;6(3):91–97. doi: 10.1097/HPC.0b013e31812da7bc. [DOI] [PubMed] [Google Scholar]
- 18.Haines A, Jones R. Implementing findings of research. BMJ. 1994;308(6942):1488–1492. doi: 10.1136/bmj.308.6942.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McMullan JT, Hinckley W, Bentley J, et al. Ground emergency medical services requests for helicopter transfer of ST-segment elevation myocardial infarction patients decrease medical contact to balloon times in rural and suburban settings. Acad Emerg Med. 2012;19(2):153–160. doi: 10.1111/j.1553-2712.2011.01273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mixon TA, Colato L. Impact of Mode of Transportation on Time to Treatment in Patients Transferred for Primary Percutaneous Coronary Intervention. J Emerg Med. 2014 doi: 10.1016/j.jemermed.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 21.Munoz D, Roettig ML, Monk L, Al-Khalidi H, Jollis JG, Granger CB. Transport time and care processes for patients transferred with ST-segment-elevation myocardial infarction: the reperfusion in acute myocardial infarction in Carolina emergency rooms experience. Circulation. Cardiovascular interventions. 2012;5(4):555–562. doi: 10.1161/CIRCINTERVENTIONS.112.968461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Landman AB, Spatz ES, Cherlin EJ, Krumholz HM, Bradley EH, Curry LA. Hospital collaboration with emergency medical services in the care of patients with acute myocardial infarction: perspectives from key hospital staff. Ann Emerg Med. 2013;61(2):185–195. doi: 10.1016/j.annemergmed.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O'Connor Robert E, Gonzales Louis NG, Manoukian Steven V, Moyer Peter H, Ivan Rokos, Sayre Michael R, Solomon Robert C, Wingrove Gary L, Brady William J, Susan McBride, Lorden Andrea L, Mayme Lou Roettig, Anna Acuna, Jacobs Alice K. Emergency Medical Services Management of STEMI in the United States - A Report From The AHA Mission: Lifeline Program. American Journal of Emergency Medicine. 2014 doi: 10.1016/j.ajem.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 24.Shah R, Goldstein SM, Unger BT, Henry TD. Explaining Anomalous High Performance in a Health Care Supply Chain*. Decision Sciences. 2008;39(4):759–789. [Google Scholar]
- 25.Baruch T, Rock A, Koenig WJ, Rokos I, French WJ. Call 911” STEMI protocol to reduce delays in transfer of patients from non primary percutaneous coronary intervention referral Centers. Critical pathways in cardiology. 2010;9(3):113–115. doi: 10.1097/HPC.0b013e3181e9d410. [DOI] [PubMed] [Google Scholar]
- 26.Laker LF, Froehle CM, Lindsell CJ, Ward MJ. The Flex Track: Flexible Partitioning Between Low- and High-Acuity Areas of an Emergency Department. Ann Emerg Med. 2014 doi: 10.1016/j.annemergmed.2014.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ward MJ, Ferrand YB, Laker LF, et al. The Nature and Necessity of Operational Flexibility in the Emergency Department. Ann Emerg Med. 2014 doi: 10.1016/j.annemergmed.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McLay LA, Mayorga ME. Evaluating emergency medical service performance measures. Health Care Manag Sci. 2010;13(2):124–136. doi: 10.1007/s10729-009-9115-x. [DOI] [PubMed] [Google Scholar]
- 29.Salhi RA, Edwards JM, Gaieski DF, Band RA, Abella BS, Carr BG. Access to Care for Patients With Time-Sensitive Conditions in Pennsylvania. Ann Emerg Med. 2013 doi: 10.1016/j.annemergmed.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 30.Ward MJKS, Zhu Y, Storrow AB, Dittus RS, Harrell FE, Self WH. Incidence of Emergency Department Visits for ST-Elevation Myocardial Infarction in a Recent 6-Year Period in the United States. Am J Cardiol. 2014 doi: 10.1016/j.amjcard.2014.10.020. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]