Abstract
Objective
Examine the psychometric properties of the Appraisal of Caregiving Scale (ACS).
Methods
Data were collected as part of the FOCUS Program trial in Michigan (N = 484 caregivers).
Results
Exploratory factor analysis found the ACS measured Threat, General Stress, and Benefit appraisals. Cronbach’s alphas for all subscales exceeded 0.70. Construct validity analyses indicated the Threat subscale correlated significantly with concepts of avoidant coping, burden, and dyadic support (r > 0.30). General Stress correlated significantly with burden (r = 0.348) and dyadic support (r = −0.373), and the Benefit subscale correlated significantly with active coping (r = 0.444). Known group analyses indicated that depressed caregivers had higher Threat and General Stress scores than non-depressed caregivers. Also, younger caregivers reported significantly higher scores on the General Stress subscale than older caregivers. Predictive validity analyses found appraisal scores at baseline accounted for 33.3% of the variance in hopelessness and 27.8% of the variance in depression at Time 2.
Conclusion and practice implications
The ACS is a reliable measure of Threat, General Stress, and Benefit appraisals, with some support for its validity. Health professionals may find the ACS useful for guiding intervention development. Future research should continue to examine the ACS’ validity.
Keywords: oncology, cancer, family caregiver, advanced cancer, appraisal, stress and coping, psychometrics
1. Introduction
Family caregivers are the long term care providers for people with cancer, and play a critical role in helping patients maintain their physical and emotional health [1, 2]. The deleterious impact of caregiving is well documented, with a number of studies reporting that up to a third of caregivers report high anxiety [3, 4]. In some contexts, the rate of anxiety among cancer caregivers exceeds the prevalence of anxiety among patients [3, 4] and the general population [5]. These findings are of concern, as caregivers with higher anxiety report a decrease in their own health and well-being [3, 6, 7].
Based on the Stress and Coping Theory [8], determining whether a situation, such as caring for a loved one with cancer, is stressful involves two appraisal processes: primary and secondary appraisal. Primary appraisal consists of determining the significance of a threatening event with respect to its impact on one’s well-being. During this process, a decision is made about whether the event poses a threat, will cause harm or loss, or presents a challenge [8]. Secondary appraisal is an individual’s evaluation of their internal and external resources for coping with the situation [8]. These theoretical concepts have received considerable empirical support, with a number of studies reporting that negative appraisals of the illness or caregiving are associated with poorer caregiver health and well-being outcomes [9–11]. In fact, one study among caregivers of advanced cancer patients found that caregivers’ appraisals were a more important predictor of their outcomes than patients’ symptoms [11]. Similarly, a study among caregivers of patients with colorectal cancer [10] found stress appraisal was the strongest predictor of caregivers’ adjustment outcomes.
Although appraisal is a key factor for understanding how caregivers cope with the demands of their role, few psychometrically sound instruments are available to measure this concept. One exception to this is the Appraisal of Caregiving Scale (ACS) [12].
1.1 Description of the ACS
Based on Lazarus & Folkman’s Stress and Coping Framework [8], the ACS [12] is comprised of three subscales to measure negative (i.e., Threat and General Stress) and positive (i.e., Benefit) appraisals of caregiving. The 27-item self-administered ACS asks caregivers to answer items pertaining to: caregiving tasks and responsibilities, relationships and interpersonal support, impact on lifestyle, effect on their emotional and physical health, and overall personal impact. Each item is rated on a 5-point Likert scale. A mean subscale score is calculated by dividing the total subscale score by the number of items in the subscale (General Stress items are reverse coded). Higher scores represent greater threat, more stress, and higher perceived benefits. The ACS has been used in prior caregiving research, with most of these studies reporting good internal consistency (α = 0.83–0.90) [13–16]. However, the ACS’ validity was only examined during its initial development and testing [12].
1.2 Development and Initial Testing of the ACS
The original ACS [12] consisted of 72 items, and was administered to 240 caregivers. Initially, 25 items that did not meet the following criteria were deleted: missing values < 25% and skewness < 50%, with standard deviation (SD) ≥ 1.2. The remaining items were factor analyzed and 16 items that did not meet the following additional criteria were removed: factor loading ≥ 0.40, no secondary loadings ≤ 50% of primary loading, conceptual fit, and minimal redundancy. The factor analysis of the remaining 31 items, yielded four factors: Threat, General Stress, Benefit, and Challenge. However, the Challenge subscale was deleted, because of a Cronbach’s alpha of 0.53. Cronbach’s alpha for the remaining three subscales (27 items) ranged from 0.73 to 0.90.
The construct validity of the 27-item ACS was assessed by examining the correlation among the General Stress, Threat, and Benefit subscales and theoretically related concepts of family hardiness, economic status, caregiver health, caregiving demands and difficulty, seriousness of illness, patient dependency, and mood dysfunction. The Threat subscale was related with all concepts in the expected direction. Similarly, the General Stress subscale was related to most concepts in the expected direction, with the exception of economic status and caregiver health. However, the Benefit subscale was only positively correlated with family hardiness and negatively correlated with mood dysfunction. Although this initial study examined the construct validity of the ACS, the psychometric properties of the scale need to be further corroborated with a larger sample of caregivers. Therefore, the purpose of the present study was to examine the factor structure, inter-item and inter-factor correlations, internal consistency reliability, and concurrent, construct, and predictive validity of the ACS.
2. Methods
This study is a secondary analysis of data obtained from a previous randomized clinical trial (RCT) of the patient-caregiver dyadic intervention called FOCUS. FOCUS was designed to improve the quality of life and other psychosocial outcomes of patients with advanced cancer and their family caregivers (N=484 patient-caregiver dyads) [15]. In this RCT, patients and their caregivers (as a unit) were randomized to one of three arms: 1) Brief 3-session FOCUS program, 2) Extensive 6-session FOCUS program, or 3) Control (i.e., usual care condition). FOCUS was delivered to patient-caregiver dyads in their homes by advanced practice nurses.
2.1 Participants
Patient eligibility criteria for the FOCUS RCT were: a) diagnosed with advanced breast, colorectal, lung, or prostate cancer in the past 6 months (new advanced cancer diagnosis, progression of advanced cancer, or change of treatment for it); b) a life expectancy of ≥ 6 months; c) aged 21 or older; d) living within 75 miles of participating cancer centers; and e) having a primary family caregiver willing to participate. Caregivers were eligible if they were aged 18 or older and had not been diagnosed with cancer in the previous year.
2.2 Procedures
Eligible participants were approached by clinic staff at four cancer centers in Southeast Michigan, U.S. Research staff contacted interested individuals and a home visit was scheduled with those willing to participate. During this visit, participants signed the consent form approved by the ethics committees, and completed the baseline questionnaire. Patients and caregivers completed their questionnaires separately. After the collection of baseline data, dyads were randomized. Throughout the study, data collectors were blinded to the dyads’ group assignments.
Over a four year period of time, 906 patient-caregiver dyads were referred to the study and 484 dyads were randomized (enrollment rate 68.6%). Reasons for refusal were primarily that the patient was too ill, too busy, not interested, or other reasons. There were no significant differences among dyads across study arms on any demographic or medical variables. There were 343 dyads that completed Time 2 surveys three months later (70.9% retention), and 302 dyads that completed Time 3 surveys six months later (62.4% retention). Among dyads who did not complete the study, in the majority of cases the patient had died or was too ill to participate. For the present analysis, Time 1 data (N = 484 caregivers) were used to examine the factor structure, inter-item and inter-factor correlations, internal consistency reliability, and concurrent and construct validity of the ACS. To assess predictive validity, Time 1 and 2 data were used from the control group only (n = 163 caregivers).
2.3 Data Collection
Caregivers completed the ACS, as previously described, and other measures that assessed caregiver burden, depression, benefit finding, coping, dyadic support, and hopelessness.
The impact on daily schedule and lack of family support subscales of the Caregiver Reaction Assessment Scale (CRA) [17] were used to measure caregiver burden. Caregivers were asked to answer these CRA items in terms of their caregiving experience at that time, using a Likert scale. The average subscale score was used in the present analysis. The Cronbach’s alpha of these subscales in this study were 0.78 – 0.84.
The Centre for Epidemiologic Studies Depression Scale (CES-D) is a 20-item scale that measures depression. CES-D total scores range from 0 to 60, with scores of 16 to 26 usually considered indicative of mild depression, whereas scores of 27 or more are indicative of major depression [18]. The CES-D has established reliability and validity among individuals with cancer [19, 20], and in this study the Cronbach’s alpha was 0.90.
Benefit finding was measured by the 11-item Benefit Finding Scale previously used with women with breast cancer [21, 22]. The scale assessed caregivers’ perception that positive contributions were made to their life by caring for someone with cancer. The total mean score was used, where higher scores indicated more perceived benefit. The total mean score was used in this analysis. The Cronbach’s alpha for this scale was 0.91.
Coping strategies were assessed by the 28-item Brief COPE, which asked participants to rate their use of different coping strategies [23]. The coping strategies assessed by this scale were factor analysed into active coping strategies (e.g., use of emotional support, positive reframing) and avoidant coping strategies (e.g., denial, self-distraction, venting), which is consistent with previous caregiver studies [24, 25]. The mean total item score for each subscale was used. The Cronbach’s alpha for the subscales were 0.78 and 0.88, respectively.
Dyadic support was measured with a modified version of the 7-item Family Support subscale of the Social Support Questionnaire [26]. Participants rated the amount of support that they perceived from the person they are caring for, where higher scores indicated more support. The Cronbach’s alpha for this scale was 0.87.
The Beck Hopelessness Scale (BHS) is a 20-item instrument designed to measure three major aspects of hopelessness: feelings about the future, loss of motivation, and expectations [27]. Participants were asked to indicate whether an item was true or false. After reversing relevant items, the total mean score was used. The reliability of the BHS has been supported in other cancer caregiver studies [13, 16]. In this study, the Cronbach’s alpha for the BHS (Time 2) was 0.88.
2.4 Data Analysis
All analyses were conducted using the Statistical Package for Social Sciences (SPSS; version 22, Chicago IL).
2.4.1 Exploratory factor analysis
Factor analysis using principal factor analysis with oblique rotation [28] was performed to identify underlying factors. Initially, to ensure the data were suitable for factor analysis the Bartlett’s test of sphericity and the Kaiser-Meyer-Olkin (KMO) were examined. To continue with the factor analysis, the Bartlett’s test of sphericity had to be significant (p < 0.05) and at minimum the KMO value would be 0.6. To determine the number of factors, three methods were applied: a) the number of factors above the break of the scree plot, b) the number of factors with an eigenvalue greater than 1, and c) parallel analysis [29]. Items were included in the factor where their loading was the highest (minimum accepted 0.30) [28]. Missing values were managed using pairwise deletion.
2.4.2 Inter-item and inter-factor correlations
For inter-item correlation and inter-factor correlations, correlation coefficients between 0.20 and 0.80 were considered acceptable.
2.4.3 Internal consistency reliability
A minimal value of 0.70 was considered acceptable for internal consistency [30].
2.4.4 Validity
All hypotheses examined as part of validity testing were grounded in Lazarus & Folkman’s Stress and Coping Theory [8], the caregiving benefit finding and burden literature [1, 2, 31–39], and/or initial testing of the ACS [12]. Three types of validity were examined: concurrent, construct, and predictive validity.
Concurrent validity examines the scale against a ‘gold standard’ or a benchmark scale that is accepted in the field [40]. As this was a secondary analysis of an existing dataset, concurrent validity could only be tested for the ACS Benefit subscale, using The Benefit Finding Scale [21, 22]. A correlation coefficient above ± 0.30 was considered acceptable.
Construct validity was assessed by examining predefined hypotheses about: 1) expected correlations between the theoretically relevant constructs of coping, burden, and support and 2) expected differences in scores between “known” groups based on level of depression and demographic characteristics [40]. First, it was hypothesized that the General Stress and Threat subscale scores would be associated with high scores on the Avoidant Coping and the CRA Burden subscales, and low scores on the Dyadic Support subscale. Whereas, the ACS Benefit subscale score would be associated with high scores on the Active Coping and Dyadic Support subscales, and low scores on the CRA Burden subscales. A correlation coefficient within the ± 0.30 range was considered acceptable.
Second, construct validity was assessed using the known group approach. In known group analyses, the validity is determined by the degree to which the scale can demonstrate different scores for groups hypothesized to vary on the variables measured [41]. It was hypothesized that depressed, female, and younger caregivers would score higher on the General Stress and Threat subscales and lower on the Benefit subscale than non-depressed, male, and older caregivers. Participants’ CES-D scores were categorized as described in the data collection section. Age was dichotomized as less than 60 years and 60 years and more. T-test and ANOVA with post-hoc Scheffe tests were used and statistical significant differences were determined by p ≤ 0.05.
For predictive validity, the following hypotheses were evaluated using multiple regression: caregivers with higher scores on the General Stress or Threat subscale and lower scores on the Benefit subscale at Time 1 will report higher hopelessness (BHS score) and depression (CES-D score) at Time 2 than those with lower scores on the General Stress or Threat subscale and higher scores on the Benefit subscale (at Time 1).
3. Results
3.1 Sample Characteristics
Caregivers’ demographic characteristics are detailed in Table 1. Caregivers were on average 56.46 years old (SD = 13.43), with slightly more females than males participating in this study (56.8% versus 43.0%). Most caregivers were Caucasian (80.0%) and living with the patient (82.6%). The most common cancer diagnoses for the patients were breast cancer, followed by lung, colorectal, and prostate cancer.
TABLE 1.
Demographic Characteristics of Sample (N = 484, unless otherwise specified)
| Variable | N | % |
|---|---|---|
| Gender | ||
| Male | 208 | 43.0 |
| Female | 275 | 56.8 |
| Missing | 1 | 0.2 |
| Race (N = 494*) | ||
| Caucasian | 395 | 80.0 |
| African American | 80 | 16.2 |
| Asian American | 9 | 1.8 |
| American Indian | 10 | 2. 0 |
| Annual household income | ||
| < 15,000 | 40 | 8.3 |
| 15,001–50,000 | 128 | 26.5 |
| > 50,001 | 248 | 51.2 |
| Missing | 68 | 14.0 |
| Currently living with patient | ||
| Yes | 400 | 82.6 |
| No | 84 | 17.4 |
| Patient’s type of cancer | ||
| Breast | 157 | 32.5 |
| Lung | 141 | 29.1 |
| Colorectal | 123 | 25.4 |
| Prostate | 63 | 13.0 |
Some participants identified to more than one cultural group.
3.2 Exploratory Factor Analysis
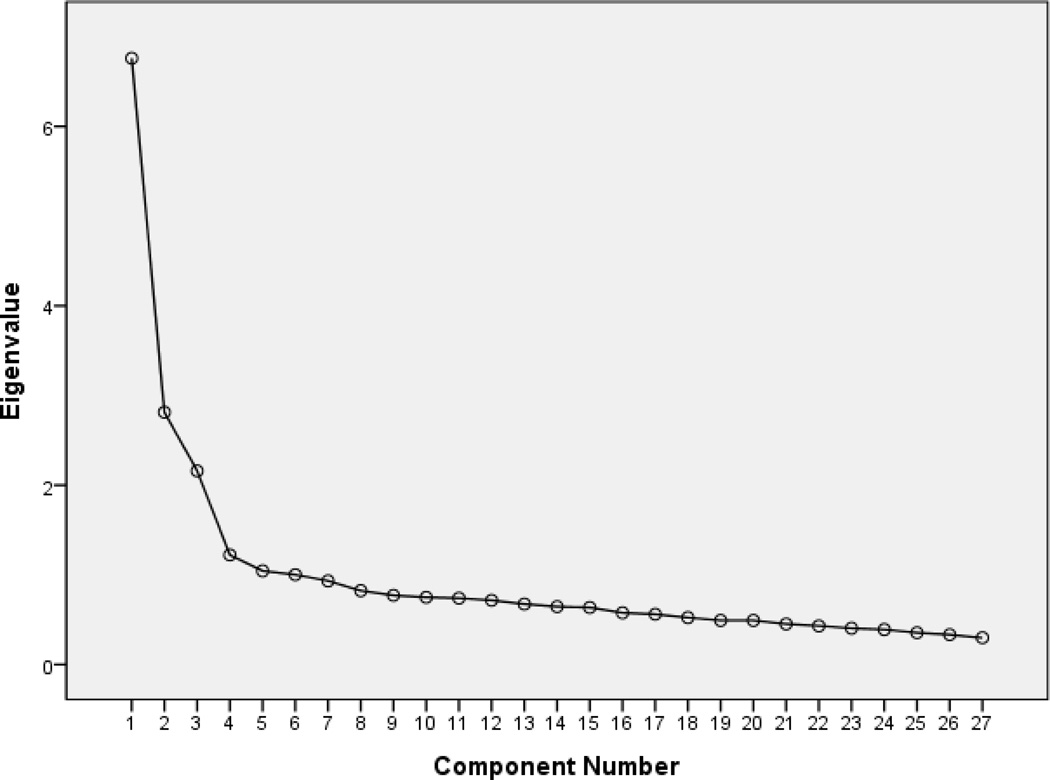
The KMO value was 0.89 and Barlett’s Test of Sphericity value was significant, supporting the use of factor analysis. The eigenvalue < 1 rule identified a five-factor solution, the parallel analysis supported a three-factor solution, and the scree plot was unclear on whether a one or three factors should be retained (two breaks in the curve – see figure 1). The five factors with eigenvalues over 1 explained 25.5%, 10.8%, 7.9%, 4.6%, and 3.9% of the variance, respectively (Total = 52.7%). Of the five factors, factors one, two and three closely reflected the original structure of the ACS (with the exception of item 27). However, this solution was deemed inappropriate, as the fourth factor only retained one unique item and most items included in the fifth factor had high cross-loadings.
Figure 1.
Screeplot of the ACS
Next, a three-factor solution was forced and examined (Table 2). This solution was conceptually and practically relevant, with minimal cross-loading both in terms of number of items and strength of the loadings. All three factors were consistent with the original ACS subscales of Threat (factor 1), Benefit (factor 2), and General Stress (factor 3). Therefore, all subsequent analyses were conducted using this factor structure.
TABLE 2.
Item mean and underlying factor structure
| Item | Item mean (SD) |
Factor 1 (Threat) |
Factor 2 (Benefit) |
Factor 3 (General Stress) |
|---|---|---|---|---|
| 1. Made me feel more appreciated by others | 3.39 (0.95) | 0.459 | ||
| 2. Situation it not very stressful for me | 3.66 (1.08) | 0.500 | ||
| 3. I feel things are going to get worse for me | 3.09 (1.22) | 0.617 | ||
| 4. I haven’t been doing well since this most recent situation started | 2.62 (1.06) | 0.557 | ||
| 5. This situation does not affect my independence | 3.13 (1.18) | 0.541 | ||
| 6. I feel a sense of loss at not being able to meet all my responsibilities | 2.87 (1.15) | 0.537 | ||
| 7. I worry that I’ll have to give up a lot of things in the future | 2.68 (1.16) | 0.649 | ||
| 8. My relationships with friends and family are not affected by this situation | 3.11 (1.18) | 0.646 | ||
| 9. This situation does not affect how I feel about myself | 2.84 (1.19) | 0.716 | ||
| 10. I’m afraid that in the future I won’t have the energy and endurance I have now | 2.95 (1.12) | 0.726 | ||
| 11. I’ve grown a lot since this most recent situation began | 3.61 (0.89) | 0.609 | ||
| 12. It seems like there is nothing more I can do that makes a difference in how the person needing my care feels | 2.57 (1.17) | 0.519 | ||
| 13. My responsibilities will continue to be what they’ve always been | 2.75 (1.24) | 0.405 | ||
| 14. This situation does not affect my lifestyle | 3.60 (1.07) | 0.580 | ||
| 15. This situation threatens to overwhelm me | 2.87 (1.13) | 0.563 | ||
| 16. My relationships with others have become more meaningful since this situation began | 3.57 (0.95) | 0.673 | ||
| 17. I’m afraid my own physical health will begin to suffer | 2.73 (1.12) | 0.688 | ||
| 18. I worry that in the future I will be less able to do the things I like to do | 2.92 (1.08) | 0.715 | ||
| 19. This situation does not affect my relationship with the person needing my care | 2.73 (1.31) | 0.556 | ||
| 20. I believe good things will come my way because of how I am handling this difficult situation | 3.22 (1.00) | 0.423 | ||
| 21. I worry that in the future I will not be able to help the person needing my care | 2.74 (1.23) | 0.550 | ||
| 22. I worry that my emotional health will suffer | 2.89 (1.11) | 0.648 | ||
| 23. Each day has become more meaningful since this most recent situation started | 3.77 (0.93) | 0.586 | ||
| 24. I’m concerned that this situation will cause financial hardship for me in the future | 2.78 (1.23) | 0.533 | ||
| 25. I’ve discovered resources I never knew I had | 3.21 (0.98) | 0.556 | ||
| 26. I’m not sure I will be able to handle this situation in the future | 2.54 (1.07) | 0.628 | ||
| 27. This situation does not affect my emotional state | 3.63 (1.05) | 0.488 |
3.3 Inter-Item and Inter-Factor Correlations
With the exception of the correlation of 0.169 between General Stress subscale items 2 “This situation is not very stressful for me” and 13 “My responsibilities will continue to be what they’ve always been”, all inter-item correlations were within an acceptable range (Table 3). Inter-factor correlations were in the expected direction; however, only the correlation between the Threat and General Stress subscale met the accepted value of 0.20.
TABLE 3.
Inter-item correlations range, inter-factor correlations, score range, mean, standard deviation, and internal consistency for the ACS subscales
| Subscales | Inter-item correlations range |
Inter-factor correlations | Score range* | M | SD | α | |||
|---|---|---|---|---|---|---|---|---|---|
| General Stress |
Threat | Benefit | Minimum | Maximum | |||||
| General Stress | 0.169 – 0.550 | 1.00 | 1.00 | 4.86 | 3.12 | 0.77 | 0.793 | ||
| Threat | 0.260 – 0.576 | 0.406 | 1.00 | 1.00 | 4.69 | 2.80 | 0.75 | 0.892 | |
| Benefit | 0.208 – 0.447 | −0.185 | −0.055 | 1.00 | 1.33 | 5.00 | 3.46 | 0.61 | 0.721 |
Potential range 1 – 5
3.4 Internal Consistency Reliability
The Cronbach’s alpha for all subscales exceeded the minimal value of 0.70 (Table 3).
3.5 Validity
3.5.1 Concurrent validity
As expected, the correlation between the Benefit subscale and the Benefit Finding Scale exceeded the minimal accepted value of 0.30 (r = 0.557).
3.5.2 Construct validity
As illustrated in Table 4, construct validity hypotheses among the ACS subscales and related concepts were partially supported. For the General Stress subscale, half of the hypotheses were supported: the General Stress subscale was positively related with the Burden subscale-impact on daily schedule (r = 0.348) and Dyadic Support (r = −0.373). For the Threat subscale, all hypothesized relationships were found to be significant (i.e., r > 0.30). As expected, correlations among the Benefit subscale and the Active Coping subscale met the minimal accepted value of 0.30 (r = 0.444). Although the Benefit subscale was associated with Dyadic Support in the expected direction, the correlation was below the accepted threshold.
TABLE 4.
Correlations of ACS subscale with coping, burden, and dyadic support
| General Stress |
Threat | Benefit | |
|---|---|---|---|
| Active Coping | -- | -- | 0.444* |
| Avoidant Coping | 0.199 | 0.462* | -- |
| Burden - impact on daily schedule | 0.348* | 0.393* | 0.110 |
| Burden - lack of family support subscales | 0.212 | 0.312* | −0.130 |
| Dyadic Support | −0.373* | −0.435* | 0.251 |
Note.
= meets the ± 0.30 criterion
Table 5 presents the results of the known group analyses. As expected, caregivers reporting mild or major depression scored significantly higher on the General Stress subscale than those reporting no depression (F (2, 462) = 18.60, p < 0.001). Similar results were noted for the Threat subscale (F (2, 457) = 90.78, p < 0.001). However, there were no significant differences according to depression on the Benefit subscales. There were no significant differences in ACS subscale scores according to gender. Although younger caregivers reported significantly higher scores on the General Stress subscale than older caregivers (t (477) = 4.107, p < 0.001), there were no significant differences between younger and older caregivers’ scores on the Threat or Benefit subscale.
TABLE 5.
Known group analyses
| N | Mean | Test statistics results | Significant post-hoc tests |
||
|---|---|---|---|---|---|
| Depression | |||||
| General Stress | No | 287 | 2.87 | F (2, 462) = 18.60, p < 0.001 | No versus mild No versus major |
| Mild | 110 | 3.21 | |||
| Major | 68 | 3.37 | |||
| Threat | No | 284 | 2.44 | F (2, 457) = 90.78, p < 0.001 | No versus mild No versus major |
| Mild | 109 | 2.80 | |||
| Major | 69 | 3.45 | |||
| Benefit | No | 284 | 3.44 | F (2, 459) = 2.95, p = 0.054 | Not applicable |
| Mild | 109 | 3.46 | |||
| Major | 69 | 3.51 | |||
| Gender | |||||
| General Stress | Male | 207 | 3.05 | t (476) = −1.84, p = 0.07 | Not applicable |
| Female | 271 | 3.18 | |||
| Threat | Male | 202 | 2.74 | t (470) = −1.56, p = 0.12 | |
| Female | 270 | 2.85 | |||
| Benefit | Male | 207 | 3.45 | t (472) = −0.372, p = 0.710 | |
| Female | 267 | 3.47 | |||
| Age | |||||
| General Stress | less than 60 | 274 | 3.25 | t (477) = 4.107, p < 0.001 | Not applicable |
| 60 years and more | 205 | 2.96 | |||
| Threat | less than 60 | 267 | 2.80 | t (471) = −0.123, p = 0.902 | |
| 60 years and more | 206 | 2.80 | |||
| Benefit | less than 60 | 269 | 3.44 | t (473) = −0.709, p = 0.479 | |
| 60 years and more | 206 | 3.48 | |||
Note.
= p ≤ 0.05
3.5.3 Predictive validity
Half of the predictive validity hypotheses were supported (see Table 6). Mainly, the ACS subscales measured at Time 1 explained 33.3% of the variance in hopelessness among participants at Time 2. Of the ACS subscales, Threat made the largest unique contribution to hopelessness at Time 2 (20.7%, beta = 0.546). Benefit also made a statistically significant contribution (9.7%, beta = −0.321), but General Stress did not. For depression, the three subscales explained 27.8% of the variance in depression (Table 6), but only the Threat subscale made a significant contribution to participants’ reported depression (18.1%, beta = 0.512).
TABLE 6.
Multiple regression results
| Hopelessness | Depression | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Standardized Coefficients Beta |
t | Sig. | 95.0% Confidence Interval for B |
Standardized Coefficients Beta |
t | Sig. |
95.0% Confidence Interval for B |
|||
| Lower bound |
Upper bound |
Lower bound |
Upper bound |
|||||||
| (Constant) | 1.684 | 0.095 | −0.803 | 9.870 | −0.269 | 0.788 | −17.924 | 13.634 | ||
| General Stress | −0.055 | −0.580 | 0.563 | −1.460 | 0.799 | 0.034 | 0.343 | 0.732 | −2.762 | 3.917 |
| Threat | 0.546 | 5.892 | < 0.001 | 2.223 | 4.477 | 0.512 | 5.260 | < 0.001 | 5.509 | 12.173 |
| Benefit | −.0321 | −4.034 | < 0.001 | −3.468 | −1.183 | 0.139 | −1.665 | 0.099 | −6.216 | 0.540 |
4. Discussion and Conclusion
4.1 Discussion
Based on Lazarus & Folkman’s framework [8], the Appraisal of Caregiving Scale (ACS) [12] was developed as a self-report measure of the multidimensional concept of caregiving appraisal. Overall, the analyses supported the three-factor structure of the ACS consisting of the General Stress, Threat, and Benefit subscales. The strength of this factor structure was that items loaded on the expected factor and with no significant cross-loadings noted. The internal consistency reliability of all subscales was also found to be adequate (i.e., exceeding 0.70).
The validity of the ACS subscales was partially supported. In terms of the negative appraisal subscales, the correlations between the Threat subscale and avoidant coping, burden, and dyadic support were all supported, consistent with the scale’s theoretical underpinning. These findings further corroborated those from the initial testing of the ACS [12]. Also in line with the initial testing of the ACS, the General Stress subscale was significantly positively associated to higher caregiver burden (impact on daily schedule). The significant negative relationship between general stress and dyadic support further support its construct validity as measure of negative appraisal.
The known group hypotheses were also partially supported. The ACS General Stress and Threat subscales were able to differentiate caregivers who were depressed from those who were not. The construct validity analyses (i.e., known groups analyses) also added to the literature by documenting that younger caregivers scored significantly higher on the General Stress subscale than their older counterparts, possibly due to the multiple demands (e.g., work, family) on younger caregivers’ schedule. This finding is consistent with studies reporting that younger caregivers are more likely to report higher negative outcomes in comparison to older caregivers (e.g., anxiety, depression) [14, 36, 37]. Of note, the relationships between the ACS General Stress and Threat subscales with caregivers’ gender was not significant. Although this is consistent with the initial testing of the ACS [12], this is contrary to a study by Kim et al. [9], who found that female caregivers reported more stress appraisal than their male counterpart.
Although negative effects of caregiving tend to dominate the literature, an important aspect of the ACS is that it captures positive caregiving appraisal. The items of the ACS Benefit subscale capture many of the benefits reported by a recent review by Li & Loke [42], including feeling appreciated, personal growth, and enhanced relationships. Concurrent validity of this subscale was supported by testing it against the widely used Benefit Finding Scale [21, 22]. However, hypotheses to test construct validity were only partially supported. As expected, the Benefit subscale was significantly related to the Active Coping subscale [23]. However, hypothesized relationships between benefit and burden and depression were not supported. To a certain extent these findings are consistent with those of Narayan et al. [43] who found that, among caregivers of individuals with dementia, positive and negative aspects of caregiving were not related, suggesting that these are independent. Another explanation is that benefit finding might lead to a reluctance to acknowledge the degree of distress one might be experiencing [44]. The known group hypotheses pertaining to benefit finding and gender and age were also not supported. Kim et al. [31] found that demographic characteristics might only be related to certain aspects of benefit finding, like appreciation of life, but not others such as acceptance and empathy. The ACS Benefit subscale does not differentiate among different types of benefit finding, and that may explain the lack of relationship with demographic factors in this study. Overall, reliability and concurrent validity tests supported continued use of the ACS Benefit subscale. However, further assessment of its construct validity is needed with other measures.
The present study is the first one to examine the longitudinal adverse impact of some appraisal patterns. The predictive validity analyses indicated that caregivers’ baseline appraisal scores on the Benefit and Threat subscales of the ACS accounted for a significant amount of variance in their hopelessness (33%) and depression (27.8%) at Time 2 (3 months later). Of note, the baseline Threat score was most predictive of these two outcomes, supporting the robustness of this subscale as a measure of intense negative experiences.
Although this study has supported some of the psychometric properties of the ACS, a few limitations are noteworthy. Even though the sample was recruited across four sites, it was comprised mainly of middle- and upper-middle class, Caucasian caregivers. Therefore, the data are not reflective of the ethnic/racial diversity of the population of cancer caregivers as a whole. Also, since this was a secondary analysis, only instruments that were part of the initial FOCUS trial could be used to assess construct validity. A related limitation is that validity testing of the ACS was determined by the hypotheses put forward, which in turn were constrained by the data that are available to support these and the measures used to capture related concepts. Another limitation is the enrollment rate of 68.6%; however, this is comparable to other caregiver research [5].
4.2 Conclusion
The ACS has many psychometric strengths to measure caregiving appraisal and identify caregivers at risk of negative outcomes. With corroboration of findings and additional testing, this measure may be useful as an outcome measure to examine the efficacy of interventions. Future studies, using confirmatory factor analysis are needed to further examine the structure of the ACS. Also, testing the ACS among a more diverse group of caregivers of cancer patients is recommended. More studies focusing on testing the ACS among other caregiver groups (e.g., caregivers of dementia patients) and continuing to establish its validity against other concepts are also needed (e.g., anxiety, empowerment, quality of life). In addition, even if some of the hypotheses were supported statistically, further studies are needed to examine whether these are clinically significant.
4.3 Practice implications
There is a growing interest in family caregivers among clinicians, as their key role in helping patients with cancer maintain their health is increasingly recognized [1, 2]. How caregivers appraise their roles and responsibilities has been shown to be a robust predictor of their own quality of life [9–11], with negative appraisals compromising caregivers’ ability to provide high quality care, and ultimately, having a detrimental effect on patients’ health and well-being. To develop psychosocial interventions to help caregivers cope with the demands of their role, more information is needed about how caregivers appraise their caregiving situation. The strengths of the ACS, including its multi-dimensional factor structure, internal consistency, and ability to measure both negative and positive aspects of caregiving, makes it a valuable instrument for clinicians to assess appraisal of caregiving.
Research highlights.
-
-
Appraisal is at the center of understanding how caregivers cope with the demands of their role.
-
-
Few attempts have been made to measure caregiving appraisal.
-
-
Exploratory factor analysis found that the ACS measured three types of appraisal: Threat, General Stress, and Benefit appraisals.
-
-
The Cronbach’s alpha reliability coefficients for all ACS subscales exceeded the minimal value of 0.70.
-
-
The validity of the ACS subscales was partially supported.
Acknowledgement
Study funded by Grant #R01CA107383 from National Cancer Institute, National Institutes of Health, U.S. (L. Northouse PI).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Contributor Information
Sylvie D. Lambert, Email: sylvie.lambert@mcgill.ca.
Hyojin Yoon, Email: hyojiny@umich.edu.
Katrina R. Ellis, Email: kahe@umich.edu.
Laurel Northouse, Email: lnortho@umich.edu.
References
- 1.Girgis A, Lambert SD. Caregivers of cancer survivors: the state of the field. Cancer Forum. 2009;33:167–171. [Google Scholar]
- 2.Girgis A, Lambert SD, Johnson C, Waller A, Currow D. Physical, psychosocial, relationship and economic burden of caring for people with cancer: a review. J Oncol Pract. 2013;9:197–202. doi: 10.1200/JOP.2012.000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hagedoorn M, Sanderman R, Bolks H, Tuinstra J, Coyne JC. Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol Bull. 2008;134:1–30. doi: 10.1037/0033-2909.134.1.1. [DOI] [PubMed] [Google Scholar]
- 4.Resendes LA, McCorkle R. Spousal responses to prostate cancer: an intergrative review. Cancer Invest. 2006;24:192–198. doi: 10.1080/07357900500524652. [DOI] [PubMed] [Google Scholar]
- 5.Lambert S, Girgis A, Lecathelinais C, Stacey F. Walking a mile in their shoes: anxiety and depression among caregivers of cancer survivors at six and 12 months post-diagnosis. Support Care Cancer. 2012;21:75–85. doi: 10.1007/s00520-012-1495-7. [DOI] [PubMed] [Google Scholar]
- 6.Segrin C, Badger T, Dorros SM, Meek P, Lopez AM. Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psychooncology. 2007;16:634–643. doi: 10.1002/pon.1111. [DOI] [PubMed] [Google Scholar]
- 7.Kim Y, Spillers RL, Hall DL. Quality of life of family caregivers 5 years after a relative's cancer diagnosis: follow-up of the national quality of life survey for caregivers. Psychooncology. 2012;21:273–281. doi: 10.1002/pon.1888. [DOI] [PubMed] [Google Scholar]
- 8.Lazarus R, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company Inc; 1984. [Google Scholar]
- 9.Kim Y, Baker F, Spillers RL. Cancer caregivers' quality of life: effects of gender, relationship, and appraisal. J Pain Symptom Manag. 2007;34:294–304. doi: 10.1016/j.jpainsymman.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 10.Fitzell A, Pakenham KI. Application of a stress and coping model to positive and negative adjustment outcomes in colorectal cancer caregiving. Psychooncology. 2010;19:1171–1178. doi: 10.1002/pon.1666. [DOI] [PubMed] [Google Scholar]
- 11.Aranda SK, Hayman-White K. Home caregivers of the person with advanced cancer: an Australian perspective. Cancer Nurs. 2001;24:300–307. doi: 10.1097/00002820-200108000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Oberst MT, Thomas SE, Gass KA, Ward SE. Caregiving demands and appraisal of stress among family caregivers. Cancer Nurs. 1989;12:209–215. [PubMed] [Google Scholar]
- 13.Northouse L, Kershaw T, Mood D, Schafenacker A. Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psychooncology. 2005;14:478–491. doi: 10.1002/pon.871. [DOI] [PubMed] [Google Scholar]
- 14.Harden J, Northouse L, Cimprich B, Pohl JM, Liang J, Kershaw T. The influence of developmental life stage on quality of life in survivors of prostate cancer and their partners. J Cancer Surviv. 2008;2:84–94. doi: 10.1007/s11764-008-0048-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Northouse LL, Mood DW, Schafenacker A, Kalemkerian G, Zalupski M, LoRusso P, et al. Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psychooncology. 2013;22:555–563. doi: 10.1002/pon.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Northouse LL, Mood DW, Schafenacker A, Montie JE, Sandler HM, Forman JD, et al. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer. 2007;110:2809–2818. doi: 10.1002/cncr.23114. [DOI] [PubMed] [Google Scholar]
- 17.Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health. 1992;15:271–283. doi: 10.1002/nur.4770150406. [DOI] [PubMed] [Google Scholar]
- 18.Zich JM, Attkisson CC, Greenfield TK. Screening for depression in primary care clinics: the CES-D and the BDI. Int J Psychiat Med. 1990;20:259–277. doi: 10.2190/LYKR-7VHP-YJEM-MKM2. [DOI] [PubMed] [Google Scholar]
- 19.Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) J Psychosom Res. 1999;46:437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- 20.Vodermaier A, Linden W, Siu C. Screening for emotional distress in cancer patients: a systematic review of assessment instruments. J Natl Cancer Inst. 2009;101:1464–1488. doi: 10.1093/jnci/djp336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Antoni M, Lehman J, Kilbourn K, Boyers A, Culver J, Alferi S, et al. Cognitive–behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol. 2001;20:20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- 22.Carver CS, Antoni MH. Finding benefit in breast cancer during the year after diagnosis predicts better adjustment 5 to 8 years after diagnosis. Health Psychol. 2004;23:595–598. doi: 10.1037/0278-6133.23.6.595. [DOI] [PubMed] [Google Scholar]
- 23.Carver CS. You want to measure coping but your protocol's too long: consider the Brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 24.Kershaw T, Mood D, Newth G, Ronis DL, Sanda MG, Vaishampayan U, et al. Longitudinal analysis of a model to predict quality of life in prostate cancer patients and their spouses. Ann Behav Med. 2008;36:117–128. doi: 10.1007/s12160-008-9058-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kershaw T, Northouse L, Kritpracha C, Schafenacker A, Mood D. Coping strategies and quality of life in women with advanced breast cancer and their family caregivers. Psychol Health. 2004;19:139–155. [Google Scholar]
- 26.Northouse LL. Social support in patients' and husbands' adjustment to breast cancer. Nurs Res. 1988;37:91–95. [PubMed] [Google Scholar]
- 27.Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 28.Costello AB, Osborne JW. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment, Research & Evaluation. 2005:10. [Google Scholar]
- 29.Pallant J. SPSS Survival Manual: A step-by-step guide to data analysis. Crows Nest, Australia: Allen & Unwin; 2007. [Google Scholar]
- 30.Nunnally J, Bernstein I. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994. [Google Scholar]
- 31.Kim Y, Schulz R, Carver CS. Benefit finding in the cancer caregiving experience. Psychosom Med. 2007;69:283–291. doi: 10.1097/PSY.0b013e3180417cf4. [DOI] [PubMed] [Google Scholar]
- 32.Kim Y, Carver CS, Schulz R, Lucette A, Cannady RS. Finding benefit in bereavement among family cancer caregivers. J Palliat Med. 2013;16:1040–1047. doi: 10.1089/jpm.2013.0049. [DOI] [PubMed] [Google Scholar]
- 33.Cassidy T. Benefit finding through caring: the cancer caregiver experience. Psychol Health. 2013;28:250–266. doi: 10.1080/08870446.2012.717623. [DOI] [PubMed] [Google Scholar]
- 34.Northouse LL, Mood D, Templin T, Mellon S, George T. Couples' patterns of adjustment to colon cancer. Soc Sci Med. 2000;50:271–284. doi: 10.1016/s0277-9536(99)00281-6. [DOI] [PubMed] [Google Scholar]
- 35.Northouse L, Mood D, Kershaw T, Schafenacker A, Mellon S, Walker J, et al. Quality of life of women with recurrent breast cancer and their family members. J Clin Oncol. 2002;20:4050–4064. doi: 10.1200/JCO.2002.02.054. [DOI] [PubMed] [Google Scholar]
- 36.Valeberg BT, Grov EK. Symptoms in the cancer patient: of importance for their caregivers' quality of life and mental health? Eur J Oncol Nurs. 2013;17:46–51. doi: 10.1016/j.ejon.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 37.Harden JK, Sanda MG, Wei JT, Yarandi H, Hembroff L, Hardy J, et al. Partners' long-term appraisal of their caregiving experience, marital satisfaction, sexual satisfaction, and quality of life 2 years after prostate cancer treatment. Cancer Nurs. 2013;36:104–113. doi: 10.1097/NCC.0b013e3182567c03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grov EK, Dahl AA, Moum T, Fossa D. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Ann Oncol. 2005;16:1185–1191. doi: 10.1093/annonc/mdi210. [DOI] [PubMed] [Google Scholar]
- 39.Ferrario SR, Cardillo V, Vicario F, Balzarini E, Zotti A. Advanced cancer at home: caregiving and bereavement. Palliat Med. 2004;18:129–136. doi: 10.1191/0269216304pm870oa. [DOI] [PubMed] [Google Scholar]
- 40.Streiner D, Norman G. Health Measuremnt Scales: A Practical Guide to their Development and Use. 3rd ed. New York: Oxford University Press; 2003. [Google Scholar]
- 41.Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. 8th edition. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 42.Li Q, Loke AY. The positive aspects of caregiving for cancer patients: a critical review of the literature and directions for future research. Psychooncology. 2013;22:2399–2407. doi: 10.1002/pon.3311. [DOI] [PubMed] [Google Scholar]
- 43.Narayan S, Lewis M, Tornatore J, Hepburn K, Corcoran-Perry S. Subjective responses to caregiving for a spouse with dementia. J Gerontol Nurs. 2001;27:19–28. doi: 10.3928/0098-9134-20010301-05. [DOI] [PubMed] [Google Scholar]
- 44.Tomich PL, Helgeson VS. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychol. 2004;23:16–23. doi: 10.1037/0278-6133.23.1.16. [DOI] [PubMed] [Google Scholar]