Abstract
Objective
To assess the extent to which initial, intentional weight loss-associated improvements in glucose tolerance and insulin action are diminished with weight regain.
Methods
138 overweight and obese (BMI: 32.4±3.9 kg/m2), adults (59.0±9.7 years), with pre-diabetes were followed through a 6-month weight loss intervention and subsequent 18-month weight maintenance period, or usual care control condition. Longitudinal change in weight (baseline, six, 24-months) was used to classify individuals into weight pattern categories (Loser/Maintainer (LM), n= 50; Loser/Regainer (LR), n=51; and Weight Stable (WS), n=37). Fasting plasma glucose (FPG), insulin, and insulin resistance (HOMA-IR) were measured at baseline, six, 12, 18 and 24-months and model adjusted changes, by weight pattern category, were assessed.
Results
LMs and LRs lost 8.3±4.7 kg (8.7±4.5%) and 9.6±4.7 kg (10.2±4.7%) during the first six months, respectively. LM continued to lose 1.1±3.4 kg over the next 18-months (9.9±6.5% reduction from baseline; p<0.05), while LRs regained 6.5±3.7 kg (3.3±5.3% reduction from baseline; p<0.05). Weight change was directly associated with change in all DM risk factors (all p<0.01). Notably, despite an absolute reduction in body weight (from baseline to 24-months) achieved in the LR group, 24-month changes in FPG, insulin, and HOMA-IR did not differ between WS and LR groups. Conversely, LM saw sustained improvements in all measured DM risk factors.
Conclusions
Significant weight loss followed by weight loss maintenance is associated with sustained improvements in FPG, insulin, and HOMA-IR; conversely, even partial weight regain is associated with regression of initial improvements in these risk factors towards baseline values.
Keywords: Pre-diabetes, weight loss, weight regain, fasting plasma glucose, fasting plasma insulin
Introduction
Type 2 diabetes mellitus (DM) is a prevalent and costly health condition [1] that is preceded by an asymptomatic prodromal period called pre-diabetes. Current estimates suggest one in three adults in the United States has pre-diabetes, with obesity recognized as the strongest modifiable risk factor for the disorder [2]. Indeed, the seminal Diabetes Prevention Program (DPP) demonstrated that the incidence of type 2 DM could be reduced by nearly 60% in patients with pre-diabetes through significant (i.e. 5–10%) weight loss [3]. Since then, several translations of the DPP have consistently demonstrated effectiveness across varied settings [4–9], affirming that intentional weight loss reduces risk of DM progression [10].
Successful long term weight loss maintenance is challenging, however, and most dieters will regress to baseline weight within three to five years [11,12]. Despite the well-known recidivism of obesity, limited data assess the extent to which initial weight loss-associated improvements in glucose tolerance and insulin action are diminished with weight regain, especially in at-risk populations. Although some studies suggest no association between weight fluctuation and DM risk [13–15], it is important to recognize that: (a) intentionality of initial weight loss is not always considered, (b) weight change data is often aggregated (i.e. health effects are not stratified by weight pattern classification) and, (c) ramifications of partial (i.e. 35–50%), not full, weight regain are typically presented. Consideration of each potential confounder is critical in understanding the true legacy effects of intentional weight loss on DM risk.
A recent study reporting on cardiometabolic risk after weight loss and subsequent regain in postmenopausal women found that women who regained 50% of lost weight in the year following a five-month intentional weight loss program had elevated insulin and insulin resistance values at follow-up compared to baseline [16]. These findings suggest that even partial weight regain following intentional weight loss can increase DM risk; although, replication of results is necessary (especially in a population at heightened risk for DM) before definitive conclusions can be drawn.
The purpose of this study was to determine the effect of weight fluctuation in the 18 months following a six month intentional weight loss program on fasting plasma glucose (FPG), insulin, and the homeostatic model assessment of insulin resistance (HOMA-IR) in overweight and obese adults at risk for diabetes and participating in the Healthy Living Partnerships to Prevent Diabetes (HELP PD) study [17]. We hypothesize that weight regain following intentional weight loss will be associated with worsened glucoregulatory function when compared to maintained weight loss or weight stability over the 24-month period.
Materials and Methods
Study Design and Participants
This paper presents data from a randomized, controlled trial (HELP PD; NCT00631345), originally designed to test the effectiveness of a translation of the DPP lifestyle weight loss intervention in overweight and obese adults with pre-diabetes. Study design [17] and recruitment [18] details, as well as one and two year main outcome results [8,19] have been previously published. Briefly, HELP PD was a 24-month trial comparing a community-based translation of the DPP lifestyle weight loss (LWL) intervention to enhanced usual care (UC) with regard to change in weight, glycemic control, and related outcomes. Data were collected at baseline and every six months up to 24 months of follow-up. The study was conducted in accordance with the Declaration of Helsinki, approved by the Wake Forest University Health Sciences Institutional Review Board, and all participants signed an approved informed consent document prior to enrolling in the study. 301 overweight and obese (BMI 25–39.9 kg/m2) adults (≥21 years), with pre-diabetes (FPG 95–125 mg/dl, on two separate occasions) and no medical contraindications to participate were eligible and agreed to participate in the study. Baseline participant characteristics are previously reported [18], with all covariates relevant to the current analysis (i.e. age, sex, race/ethnicity, educational attainment) captured via self-report.
Interventions
Eligible participants were randomized into two treatment groups, a LWL intervention and an enhanced UC comparison condition. The LWL intervention was designed to target 5–7% weight loss through caloric restriction and increased moderate intensity physical activity. Participants in the LWL group were placed in groups of 8–12, led by trained community health workers who were supervised by two dietitians. These groups met weekly during the first six months (intensive phase) and monthly thereafter (maintenance phase; 7–24 months). Participants in the LWL group also received three individual sessions with a registered dietitian during the intensive phase. Participants randomized to the UC comparison condition received monthly newsletters and two individual sessions with a registered dietitian during the first six months of the study.
Anthropometric Assessment and Weight Pattern Classification
Trained clinic staff collected all anthropometric measures with participants wearing light weight clothing and without shoes. Weight was measured in duplicate every six months (from baseline to 24 months) using a digital scale [17], with the average measurement at each exam used in subsequent analyses. Longitudinal measures of body weight were used to classify individuals into three distinct weight pattern categories: Loser/Maintainer (LM), Loser/Regainer (LR), and Weight Stable (WS), utilizing a two kg change in weight from baseline to six, and six to 24 months. This cut-point has been used previously [16,20] and was selected to overcome day-to-day variation in body weight. Height was also assessed at baseline using a wall-mounted stadiometer, and baseline body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters.
Biomarkers of Glucoregulatory Function
Blood samples were collected at baseline, six, 12, 18 and 24 months in EDTA-treated evacuated tubes by venipuncture in the early morning after an eight-hour fast. FPG and insulin were measured following standardized hospital laboratory methods and insulin sensitivity (HOMA-IR) was calculated as the product of the fasting values of glucose (expressed as mg/dL) and insulin (expressed as μU/mL) divided by the constant 22.5 [21].
Statistical Analysis
Descriptive statistics were calculated overall and by weight pattern group at baseline, and differences in groups were assessed using chi-square tests for categorical characteristics and analysis of variance for continuous variables. DM risk factor values were summarized by simple means and standard deviations (SD) at each time point for each weight pattern category. Analysis of covariance was used to assess the association between weight pattern category and changes in DM risk factors, adjusting for age, sex, race/ethnicity, education, and baseline BMI. The six and 24-month models are also adjusted for the baseline levels of the risk factors. Linear regression was used to estimate the change in diabetes risk factors for unit changes in weight. All analyses were performed using SAS v9.3 and p-values less than 0.05 were considered statistically significant.
Results
Study Sample
Of the 301 original HELP PD participants, 257 had baseline, six and 24 month weight data (LWL: n=126, UC: n=131). Because this study was primarily interested in the effects of weight fluctuation following intentional weight loss on glucoregulatory function, only participants randomized to LWL were eligible for inclusion in the LM or LR categories. WS participants in either LWL or UC served as the aging-control group. In the LWL arm, 101 participants lost at least two kg during the initial six months; during the subsequent 18 month period, 14 of these participants lost at least two additional kg, 36 maintained their initial weight loss within two kg, and 51 regained at least two kg. The 14 who lost weight during both time periods plus the 36 who lost initially and then maintained their weight loss comprise the LM group (n=50). The 51 who lost weight initially and then regained at least two kg between six and 24 months comprise the LR group. Finally, seven participants in the LWL arm who did not lose two kg during the first six months and maintained their initial weight within two kg at the 24-month visit were classified as WS. To this group, we also add 30 participants from the UC group who maintained their baseline weight within two kg at both 6 and 24 month time-points (n=37).
Participant Descriptive Characteristics
Baseline descriptive statistics according to weight pattern category are presented in Table I. Briefly, participants were 59.0±9.7 years of age (range: 36–82 years), with the majority being female (58%) and Non-Hispanic white (78%), and half of the study sample received at least a bachelor’s degree. Average BMI was 32.4±3.9 kg/m2 and 70% of participants were classified as obese. As expected, glucoregulatory function was slightly impaired at baseline, with FPG of 104.7±10.2 mg/dl, insulin 16.1±9.3 μU/mL, and HOMA-IR 4.3±2.7 mg/dl × μU/mL. No differences in baseline characteristics were observed by group (all p>0.14). Further, differences in baseline characteristics for HELP PD participants included (n=138) and excluded (n=163) from analyses were not significantly different.
Table I.
Baseline descriptive characteristics according to weight pattern classification.
| Participant Characteristics | Loser/Maintainer (n=50) |
Loser/Regainer (n=51) |
Weight Stable (n=37) |
Overall (n=138) |
|---|---|---|---|---|
| Age (years) | 59.2 ± 9.9 | 57.8 ± 9.8 | 60.3 ± 9.2 | 59.0 ± 9.7 |
| Female, n (%) | 25 (52) | 30 (59) | 24 (65) | 80 (58) |
| Race/Ethnicity | ||||
| Non-Hispanic white, n (%) | 36 (72) | 40 (78) | 32 (86) | 108 (78) |
| Non-Hispanic black, n (%) | 13 (26) | 11 (22) | 4 (11) | 28 (20) |
| Hispanic/Other, n (%) | 1 (2) | 0 (0) | 1 (3) | 2 (1) |
| Educational attainment | ||||
| ≤ High school | 9 (18) | 12 (24) | 5 (14) | 26 (19) |
| Associate degree/other | 14 (28) | 16 (31) | 13 (35) | 43 (31) |
| Bachelor’s degree | 15 (30) | 11 (22) | 11 (30) | 37 (27) |
| Beyond bachelor’s degree | 12 (24) | 12 (24) | 8 (22) | 32 (23) |
| Weight (kg) | 94.4 ± 15.4 | 94.3 ± 13.5 | 88.8 ± 15.4 | 92.9 ± 14.8 |
| Body mass index (kg/m2) | 32.5 ± 4.1 | 32.7 ± 3.8 | 31.8 ± 4.0 | 32.4 ± 3.9 |
| Glucose (mg/dL) | 104.1 ± 9.8 | 104.2 ± 9.3 | 106.1 ± 12.0 | 104.7 ± 10.2 |
| Insulin (μU/mL) | 14.9 ± 9.2 | 15.8 ± 8.8 | 18.0 ± 10.2 | 16.1 ± 9.3 |
| HOMA-IR (mg/dL × μU/ml) | 3.96 ± 2.70 | 4.09 ± 2.32 | 4.85 ± 3.03 | 4.25 ± 2.67 |
Data are presented as means ± SD or n (%). All p-values > 0.14.
Twenty-four month weight histories by group and time-point are presented in Figure I. On average, participants classified as LMs lost 8.3±4.7 kg (8.7±4.5%) during the initial six month period, and continued to lose 1.1±3.4 kg over the next 18 months (9.9±6.5% reduction from baseline). The LR group lost 9.6±4.7 kg (10.2±4.7%) during the initial six month period, and regained 6.5±3.7 kg over the next 18 months (3.3±5.3% reduction from baseline). The WS group fluctuated only 0.3 ± 0.9 kg from baseline to six months, and 0.2 ± 1.2 kg from baseline to 24-months, with no difference seen between participants randomized to LWL or UC (all p>0.05).
Figure I.
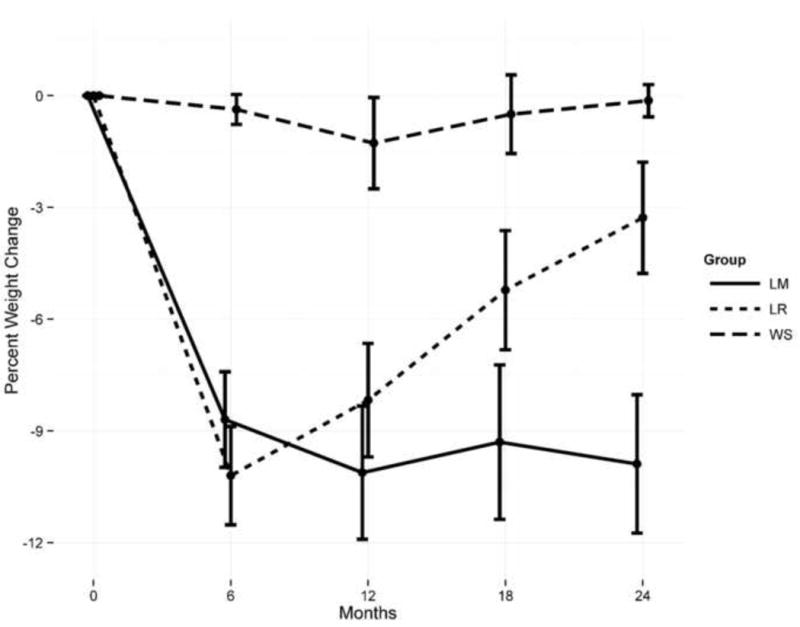
Percent weight change by pattern category and time-point. LM = Loser/Maintainer; n=50. LR = Loser/Regainer; n=51. WS = Weight Stable, n=37.
Risk Factors for DM by Weight Change and Weight Pattern Classification
Change in all DM risk factors was strongly and directly associated with change in weight (all p<0.01). Table II presents unadjusted DM risk factors by weight pattern classification and time point. As expected, both LM and LR groups saw improvements in all risk factors from baseline to six months when compared to the WS group. Participants categorized as LMs saw sustained improvements in all risk factors from six to 24 months while participants categorized as LRs regressed to baseline values. Interestingly, WS participants had relatively stable (FPG) or slightly reduced (insulin, HOMA-IR) risk factor values at 24-months compared to baseline.
Table II.
Unadjusted diabetes risk factors by weight pattern classification and time point.
| Diabetes Risk Factors by Weight Pattern | N | Baseline | 6 Months | 12 Months | 18 Months | 24 Months | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Glucose (mg/dL) | |||||||||||
| Loser/Maintainer | 50 | 104.1 | 9.8 | 101.6 | 9.7 | 100.4 | 10.3 | 99.6 | 11.1 | 99.8 | 10.4 |
| Loser/Regainer | 51 | 104.2 | 9.3 | 98.9 | 8.0 | 100.5 | 9.1 | 103.2 | 8.6 | 104.9 | 8.9 |
| Weight Stable | 37 | 106.1 | 12.0 | 106.3 | 9.0 | 103.6 | 12.0 | 106.7 | 11.0 | 106.5 | 10.1 |
| Insulin (μIU/mL) | |||||||||||
| Loser/Maintainer | 50 | 14.9 | 9.2 | 9.0 | 6.6 | 7.9 | 4.6 | 7.8 | 4.4 | 8.4 | 6.6 |
| Loser/Regainer | 51 | 15.8 | 8.8 | 8.8 | 4.5 | 9.6 | 4.6 | 10.3 | 5.4 | 12.1 | 10.3 |
| Weight Stable | 37 | 18.0 | 10.2 | 14.7 | 7.6 | 11.7 | 4.9 | 12.7 | 5.8 | 13.9 | 7.4 |
| HOMA-IR (mg/dl*μIU/ml) | |||||||||||
| Loser/Maintainers | 50 | 4.0 | 2.7 | 2.3 | 2.1 | 2.0 | 1.3 | 2.0 | 1.3 | 2.2 | 1.9 |
| Loser/Regainers | 51 | 4.1 | 2.3 | 2.2 | 1.2 | 2.4 | 1.2 | 2.7 | 1.5 | 3.2 | 2.8 |
| Weight Stable | 37 | 4.8 | 3.0 | 3.9 | 2.0 | 3.0 | 1.4 | 3.3 | 1.6 | 3.7 | 2.2 |
Adjusted least squares means estimates for the DM risk factor values at baseline and their changes over time by group are presented in Table III. As in unadjusted models, at six months, both LM and LR groups saw similar improvements in FPG, insulin and HOMA-IR (p>0.05 for LM vs. LR), while the WS group changes were much smaller (p<0.05 for WS vs. LM and LR). For the change between 6 and 24 months, the LR group had significantly increased FPG, insulin, and HOMA-IR compared to the LM group, and higher FPG compared to the WS group. No differences were seen between LM and WS groups. When comparing 24 month to baseline values, all DM risk factors still differed significantly between groups, with major differences observed between LM and the other two weight pattern categories. Specifically, the LM group had significantly lower FPG, insulin and HOMA-IR than LR or WS categories (all p<0.05). Of note, the changes in DM risk factors from baseline to 24 months did not differ significantly between the LR and WS groups, despite the fact that participants categorized as LRs only regained two-thirds of lost weight and still weighed significantly less at 24 months than at baseline (p<0.05).
Table III.
Least squares means (standard errors) for DM risk factors at baseline, 6 months and 24 months.
| Diabetes Risk Factor | Timepoint | Loser/Maintainers | Loser/Regainer | Weight Stable | Overall p-value |
|---|---|---|---|---|---|
| Glucose (mg/dL) | Baseline | 104.2 (1.5) | 104.4 (1.5) | 105.9 (1.7) | 0.74 |
| 0–6 Months | −2.87 (1.06) | −5.47 (1.05) | 0.91 (1.24) | <0.01 | |
| 6–24 Months | −1.78 (1.10) | 5.11 (1.11) | 1.25 (1.33) | <0.01 | |
| 0–24 Months | −4.58 (1.26) | 0.46 (1.25) | 0.93 (1.48) | <0.01 | |
| Insulin (μIU/mL) | Baseline | 14.85 (1.32) | 15.52 (1.30) | 18.47 (1.54) | 0.19 |
| 0–6 Months | −6.69 (0.65) | −7.21 (0.64) | −1.96 (0.76) | <0.01 | |
| 6–24 Months | −0.98 (0.98) | 2.91 (0.97) | 0.35 (1.22) | 0.02 | |
| 0–24 Months | −7.11 (0.91) | −3.76 (0.89) | −3.10 (1.07) | <0.01 | |
| HOMA-IR (mg/dl*μIU/ml) | Baseline | 3.94 (0.38) | 4.03 (0.38) | 4.96 (0.44) | 0.27 |
| 0–6 Months | −1.81 (0.18) | −2.02 (0.18) | −0.58 (0.22) | <0.01 | |
| 6–24 Months | −0.29 (0.27) | 0.91 (0.27) | 0.16 (0.34) | <0.01 | |
| 0–24 Months | −1.99 (0.27) | −0.97 (0.27) | −0.78 (0.32) | <0.01 |
All models adjusted for age, sex, race/ethnicity, education, and baseline BMI.
Lastly, linear changes in weight change and DM risk factor change during the weight loss (0–6 months) and weight regain (6–24 months) period for participants in the LR group (only) were assessed. For every 1 kg of weight lost between baseline and 6 months, FPG, insulin, and HOMA-IR were reduced by 0.19±0.27 mg/dL, 0.46±0.19 μIU/mL, and 0.10±0.05 mg/dl*μIU/ml, respectively. Conversely, for every 1 kg of weight regained between 6 and 24 months, FPG, insulin, and HOMA-IR increased by 0.27±0.31 mg/dL, 0.42±0.31 μIU/mL, and 0.12±0.08 mg/dl*μIU/ml.
Discussion
The purpose of this study was to explore the long-term effects of weight regain following a successful (i.e. ~9% of baseline weight) six month intentional weight loss intervention on traditional DM risk factors (FPG, insulin, and HOMA-IR) in overweight and obese adults with pre-diabetes. Unsurprisingly, weight change was strongly and directly associated with change in DM risk factors, with significant weight loss followed by weight loss maintenance associated with sustained improvements in FPG, insulin, and HOMA-IR. Conversely, even partial (i.e. 2/3rds) weight regain was associated with regression of initial improvements in these risk factors to values similar to those seen in the control group. Results underscore the importance of stable, weight loss maintenance following intentional weight loss for prevention of diabetes in this population.
Although HELP PD participants were enrolled in an active weight loss/maintenance intervention for the duration of the study, the magnitude of observed weight change in the Loser/Regainer group from six to 24 months is consistent with prior research suggesting approximately two-thirds of lost weight is regained within two years [12,22]. That being said, data also show that enrollment in an 18-month weight loss maintenance program was successful at preventing weight regain of at least 2 kg in approximately 50% of participants. Findings are also consistent with other work showing weight-loss associated improvements in insulin action [23] are preserved with long-term weight loss maintenance [15], and credit absolute weight reduction, rather than negative energy balance, to metabolic improvements. Results presented here suggesting that weight regain during the 18-month follow up period negates prior improvements in glucoregulatory function are notable, and add to a limited, but mixed, body of literature assessing the health ramifications of weight regain following intentional weight loss.
Two early epidemiologic studies in Pima Indians conclude that weight fluctuation over time is not associated with incidence of diabetes [13] or detrimental effects on insulin action, insulin secretion, or glucose tolerance [15], as all measures were similar to baseline after a single bout of weight loss and subsequent regain. Although intentionality of weight change is not accounted for these analyses, regression of weight loss-associated improvements in glucoregulatory function towards baseline values with weight regain is in agreement with the current report. And, while we are careful not to extrapolate beyond the time-points measured, one could speculate, based on linear change data presented for the LR group, that total weight regain (which is likely to happen within five years under free-living conditions [12,22]) may have detrimental effects on glucoregulatory function, particularly FPG, when compared to baseline values or a weight stable condition.
Studies by Haufe [14] and Beavers [16] et al. more closely resemble the current analysis, in that authors report on the metabolic effects of weight change following an intentional weight loss intervention. In contrast to findings of the present study, Haufe et al. [14] report that initial weight loss-associated improvements in insulin sensitivity persist, despite weight regain in the two years following intervention. In their study, however, percentage of weight regained was relatively small (40% [14] vs. 68% in the present study) and aggregated effects were presented; that is, individuals who regained weight and maintained weight were combined, which may have dampened the true effect of weight regain on insulin action.
Beavers et al. [16] followed a cohort of postmenopausal women through a five-month weight loss intervention and a year of observational follow-up. Authors report that women who regained 50% of lost weight in the year following the weight loss program had elevated insulin and insulin resistance values at follow-up compared to baseline [16]. Although results presented here do not suggest a worsening in glucoregulatory function (compared to baseline levels) with a bout of weight regain, they certainly support diminished improvements. Interestingly, a separate analysis of the same cohort of women revealed that a cycle of weight regain is also associated with preferential fat mass, compared to lean mass, accretion [20]. This shift in body composition may offer a plausible biologic mechanism underlying observed associations between partial weight regain and glucogregulatory function, as lean mass is a major sink for glucose disposal. Unfortunately, we are unable to test this hypothesis in the present study as (DXA-acquired) body composition was not assessed.
Strengths of the current study include repeated measures of weight change over a two-year period, including an intensive weight loss and weight loss maintenance phase. Moreover, the study design allowed for inclusion of a weight-stable group to control for aging-related variability in glucoregulatory function. Interpretation of our findings, however, must take into consideration limitations of our study design. First, HELP PD subjects were always enrolled in some type of active intervention (i.e. weight loss or weight loss maintenance), and effects of weight regain may differ under free-living conditions. Second, weight pattern categories were defined based on change from baseline to six and six to 24 months, which ignores weight fluctuation occurring between these time points. Third, intervention-related factors, such as dietary advice and behavioral counseling, may have influenced DM risk independent of weight change, and were not accounted for in our analytic strategy. Lastly, a general limitation in this field of research is the lack of an operational definition to classify “weight regain”. Although our choice of a two kg weight change is empirically based, we acknowledge that our conclusions could differ by the definition used. Similarly, the use of categorical classifications of weight loss is problematic as weight change is naturally continuous and variability exists within categories.
In sum, data presented here suggest intentional weight loss of approximately 9% is associated with immediate improvements in glucoregulatory function in adults with pre-diabetes. Improvements are sustained with weight loss maintenance, but diminish with weight regain. Given the known immediate benefit of weight loss on DM risk reduction, results highlight the need for future research to develop effective strategies to promote long-term maintenance of weight loss in this population.
Acknowledgments
This study was funded by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (R18-DK-69901). The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
All authors significantly contributed to the completion of this manuscript: DCG, CSB, and MZV: designed the research; CSB, JAK, and MZV: conducted the research; DC: analyzed the data; KMB and DC: interpreted the data and drafted the manuscript; and KMB: had primary responsibility for the final content. All authors read and approved the final manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No potential conflicts of interest relative to this article were reported.
References
- 1.Fast Facts: Data and Statistics about Diabetes. 2013 [article online] Available from http://professional.diabetes.org/admin/UserFiles/0%20–%20Sean/FastFacts%20March%202013.pdf.
- 2.National Diabetes Prevention Program: Division of Diabetes Translation National Center for Chronic Disease Prevention and Health Promotion. 2013 [article online] Available from http://www.cdc.gov/diabetes/prevention/prediabetes.htm.
- 3.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the Diabetes Prevention Program into the community. The DEPLOY Pilot Study. Am J Prev Med. 2008;35(4):357–363. doi: 10.1016/j.amepre.2008.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boltri JM, Davis-Smith YM, Seale JP, Shellenberger S, Okosun IS, Cornelius ME. Diabetes prevention in a faith-based setting: results of translational research. J Public Health Manag Pract. 2008;14(1):29–32. doi: 10.1097/01.PHH.0000303410.66485.91. [DOI] [PubMed] [Google Scholar]
- 6.Absetz P, Valve R, Oldenburg B, Heinonen H, Nissinen A, Fogelholm M, Ilvesmaki V, Talja M, Uutela A. Type 2 diabetes prevention in the “real world”: one-year results of the GOAL Implementation Trial. Diabetes Care. 2007;30(10):2465–2470. doi: 10.2337/dc07-0171. [DOI] [PubMed] [Google Scholar]
- 7.McBride PE, Einerson JA, Grant H, Sargent C, Underbakke G, Vitcenda M, Zeller L, Stein JH. Putting the Diabetes Prevention Program into practice: a program for weight loss and cardiovascular risk reduction for patients with metabolic syndrome or type 2 diabetes mellitus. J Nutr Health Aging. 2008;12(10):745S–749S. doi: 10.1007/BF03028624. [DOI] [PubMed] [Google Scholar]
- 8.Katula JA, Vitolins MZ, Rosenberger EL, Blackwell CS, Morgan TM, Lawlor MS, Goff DC., Jr One-year results of a community-based translation of the Diabetes Prevention Program: Healthy-Living Partnerships to Prevent Diabetes (HELP PD) Project. Diabetes Care. 2011;34(7):1451–1457. doi: 10.2337/dc10-2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katula JA, Vitolins MZ, Morgan TM, Lawlor MS, Blackwell CS, Isom SP, Pedley CF, Goff DC., Jr The Healthy Living Partnerships to Prevent Diabetes study: 2-year outcomes of a randomized controlled trial. Am J Prev Med. 2013;44(4):S324–S332. doi: 10.1016/j.amepre.2012.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Will JC, Williamson DF, Ford ES, Calle EE, Thun MJ. Intentional weight loss and 13-year diabetes incidence in overweight adults. Am J Public Health. 2002;92(8):1245–1248. doi: 10.2105/ajph.92.8.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiss EC, Galuska DA, Kettel KL, Gillespie C, Serdula MK. Weight regain in U.S. adults who experienced substantial weight loss, 1999–2002. Am J Prev Med. 2007;33(1):34–40. doi: 10.1016/j.amepre.2007.02.040. [DOI] [PubMed] [Google Scholar]
- 12.Methods for voluntary weight loss and control. NIH Technology Assessment Conference Panel. Consensus Development Conference, 30 March to 1 April 1992. Ann Intern Med. 1993;119(7):764–770. [PubMed] [Google Scholar]
- 13.Hanson RL, Narayan KM, McCance DR, Pettitt DJ, Jacobsson LT, Bennett PH, Knowler WC. Rate of weight gain, weight fluctuation, and incidence of NIDDM. Diabetes. 1995;44(3):261–266. doi: 10.2337/diab.44.3.261. [DOI] [PubMed] [Google Scholar]
- 14.Haufe S, Haas V, Utz W, Birkenfeld AL, Jeran S, Bohnke J, Mahler A, Luft FC, Schulz-Menger J, Boschmann M, Jordan J, Engeli S. Long-lasting improvements in liver fat and metabolism despite body weight regain after dietary weight loss. Diabetes Care. 2013;36(11):3786–3792. doi: 10.2337/dc13-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weyer C, Hanson K, Bogardus C, Pratley RE. Long-term changes in insulin action and insulin secretion associated with gain, loss, regain and maintenance of body weight. Diabetologia. 2000;43(1):36–46. doi: 10.1007/s001250050005. [DOI] [PubMed] [Google Scholar]
- 16.Beavers DP, Beavers KM, Lyles MF, Nicklas BJ. Cardiometabolic risk after weight loss and subsequent weight regain in overweight and obese postmenopausal women. J Gerontol A Biol Sci Med Sci. 2013;68(6):691–698. doi: 10.1093/gerona/gls236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katula JA, Vitolins MZ, Rosenberger EL, Blackwell C, Espeland MA, Lawlor MS, Rejeski WJ, Goff DC. Healthy Living Partnerships to Prevent Diabetes (HELP PD): design and methods. Contemp Clin Trials. 2010;31(1):71–81. doi: 10.1016/j.cct.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blackwell CS, Foster KA, Isom S, Katula JA, Vitolins MZ, Rosenberger EL, Goff DC., Jr Healthy Living Partnerships to Prevent Diabetes: recruitment and baseline characteristics. Contemp Clin Trials. 2011;32(1):40–49. doi: 10.1016/j.cct.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rejeski WJ, Axtell R, Fielding R, Katula J, King AC, Manini TM, Marsh AP, Pahor M, Rego A, Tudor-Locke C, Newman M, Walkup MP, Miller ME. Promoting physical activity for elders with compromised function: the lifestyle interventions and independence for elders (LIFE) study physical activity intervention. Clin Interv Aging. 2013;8:1119–1131. doi: 10.2147/CIA.S49737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beavers KM, Lyles MF, Davis CC, Wang X, Beavers DP, Nicklas BJ. Is lost lean mass from intentional weight loss recovered during weight regain in postmenopausal women? Am J Clin Nutr. 2011;94(3):767–774. doi: 10.3945/ajcn.110.004895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 22.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1):222S–225S. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]
- 23.Petersen KF, Dufour S, Befroy D, Lehrke M, Hendler RE, Shulman GI. Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes. 2005;54(3):603–608. doi: 10.2337/diabetes.54.3.603. [DOI] [PMC free article] [PubMed] [Google Scholar]


