Abstract
Background
The characteristics of contemporary Fontan survivors are not well described.
Objective
We characterized a large cohort of children who had a Fontan procedure, using measures of functional health status, ventricular size and function, exercise capacity, heart rhythm, and brain natriuretic peptide (BNP).
Methods
We enrolled 546 children (6–18 years, mean 11.9 years) and compared them within pre-specified anatomic and procedure subgroups. History and outcome measures were obtained within a three month period.
Results
Predominant ventricular morphology was left (LV) 49%, right (RV) 34%, and mixed 19%. Ejection fraction (EF) was normal for 73% of subjects; diastolic function grade was normal for 28%. Child Health Questionnaire mean summary scores were lower than for controls; however, over 80% of subjects were in the normal range. BNP concentration ranged from <4–652 pg/mL (median 13). Mean percent predicted peak oxygen consumption was 65% and decreased with age. EF and EF z-score were lowest, and semilunar and atrioventricular (AV) valve regurgitation were more prevalent in the RV subgroup. Older age at Fontan was associated with more severe AV valve regurgitation. Most outcomes were not associated with a superior cavopulmonary connection prior to Fontan.
Conclusions
Measures of ventricular systolic function and functional health status, although lower on average in the cohort compared to controls, were in the majority of subjects within two standard deviations of the mean for controls. RV morphology was associated with poorer ventricular and valvar function. Effective strategies to preserve ventricular and valvar function, particularly for patients with RV morphology, are needed.
Keywords: Fontan, cardiac magnetic resonance, exercise, brain natriuretic peptide, echocardiography, diastolic function, pediatric
INTRODUCTION
Children who have undergone a Fontan procedure for palliation of a functional single ventricle are at risk for medical complications (1). Current therapy is based on expert opinion, retrospective data collection, and single center small studies. Robust clinical trials are needed to guide care for this population. Trial design requires careful phenotyping and understanding of factors that affect outcomes. To this end, the NHLBI-funded Pediatric Heart Network (PHN) conducted the largest observational study to date in children who have undergone a Fontan procedure. The primary aim of this report is to characterize this cohort and specific subgroups, using state-of-the-science techniques to assess functional health status, ventricular size and function, exercise performance, brain natriuretic peptide (BNP) concentration, and heart rhythm.
METHODS
Study Design and Components
This cross-sectional study recruited subjects 6–18 years old who had not undergone cardiac surgical intervention in the six months prior to enrollment (2). Anatomic, clinical, and surgical data were collected at enrollment (March 2003 to April 2004) by a detailed medical record review using standardized forms. Each subject’s tests were conducted within three months. The protocol was approved by each Center’s Institutional Review Board. Written informed consent and assent were obtained.
Patient Sample
A total of 1,078 subjects from seven centers in the U.S. and Canada were screened, 644 were study eligible, and 546 were enrolled (86% consent rate) (2). Age, time since the Fontan procedure, and functional health status scores, collected for nearly all eligible subjects, were similar for enrolled and eligible but not enrolled subjects.
Outcome Measures
Measures of Functional Health Status
The Physical and Psychosocial Summary scores of the Child Health Questionnaire (CHQ)-Parent Form (PF)-50 were used (3). The CHQ-PF50 has been validated in healthy and chronically ill children and used as a trial endpoint in pediatrics (4).
Measures of Ventricular Function and Size
Echocardiogram
Two-dimensional echocardiograms and Doppler evaluations of standard short- and long-axis views of the ventricle(s) were centrally interpreted by one of two readers. When possible, measurements and derived indices were expressed as z-scores relative to body surface area (BSA) or age in normal children (5). Ventricular anatomic abnormalities (Table 1) were characterized as left (LV), right (RV), or mixed (e.g., unbalanced atrioventricular (AV) canal). Subjects were classified as having moderate/severe valve regurgitation if right, left, or common AV valve regurgitation was moderate or severe; both right and left AV valve regurgitation grades were mild; native aortic valve or native pulmonary valve regurgitation was moderate or severe; or both native aortic valve and native pulmonary valve regurgitation grades were mild. End-diastolic (EDV) and end-systolic volumes (ESV) and mass were obtained using the biplane-modified Simpson’s method. For the mixed morphology group, the volume and mass of each ventricle were measured separately, and the combined values used for data analysis. Tei index was obtained (6). Ventricular diastolic function was assessed using measures derived from pulsed Doppler interrogation: duration of pulmonary vein flow reversal during atrial systole; tissue Doppler peak early diastolic velocity (E’); tissue Doppler peak late diastolic velocity (A’), AV valve peak early diastolic inflow velocity (E); AV valve peak late diastolic inflow velocity (A); deceleration time of the early AV valve inflow (DT); duration of AV valve late diastolic inflow (AT); and systemic ventricular flow propagation rate (FP). Two grading systems (7) were used (Table 2): I) restrictive pattern present vs. absent; II) Grades of 0 (no impairment) to 3 (greatest impairment in diastolic filling).
TABLE 1.
Cardiac Anatomic Diagnosis of 546 Fontan Cross-Sectional Study Subjects*
| Diagnosis | Number | Percent |
|---|---|---|
| Tricuspid Atresia | 119 | 22% |
| Hypoplastic Left Heart Syndrome | 112 | 21% |
| Double Inlet Left Ventricle | 80 | 15% |
| Heterotaxia | 42 | 8% |
| Double Outlet Right Ventricle | 41 | 8% |
| Pulmonary Atresia Intact Ventricular Septum | 33 | 6.0% |
| Mitral Atresia | 31 | 6% |
| Abnormal Tricuspid Valve | 22 | 4% |
| Atrio-Ventricular Canal Defect | 22 | 4% |
| Other | 38 | 7% |
The percentages have been rounded up here and in the other tables.
TABLE 2.
Fontan Cross-Sectional Study Patient Characteristics by Age at Enrollment
| Overall | <9 years | 9 to <11 years |
11 to <15 years |
≥15 years | |||
|---|---|---|---|---|---|---|---|
| Characteristic | N | Mean ± SD Median or % |
Mean ± SD Median or % |
Mean ± SD Median or % |
Mean ± SD Median or % |
Mean ± SD Median or % |
P-value |
| N | 546 | 138(25%) | 120(22%) | 169(31%) | 119(22%) | ||
| Age at enrollment, yr | 11.9±3.4 | 7.9±0.7 | 10.0±0.6 | 12.8±1.2 | 17.0±1.1 | ||
| Age at Fontan, yr | 3.4±2.1 | 3.0±1.3 | 3.0±1.5 | 3.2±1.9 | 4.6±3.0 | <.001 | |
| Age at volume unloading surgery, yr | 1.6±1.6 | 0.9±0.9 | 1.1±1.0 | 1.4±1.0 | 3.4±2.1 | <.001 | |
| Male | 546 | 60% | 58% | 62% | 65% | 55% | .305 |
| Race | 544 | .014 | |||||
| White | 80% | 70% | 80% | 82% | 87% | ||
| Black | 10% | 14% | 7% | 11% | 8% | ||
| Asian | 3% | 4% | 3% | 2% | <1% | ||
| Other | 8% | 13% | 10% | 4% | 3% | ||
| Hispanic | 517 | 7% | 8% | 10% | 4% | 6% | .318 |
| Growth | |||||||
| Percentile for stature-for-age | 544 | 26 | 22 | 31 | 22 | 31 | 0.242* |
| Z-score for stature-for-age | 544 | −0.7±1.3 | −0.7±1.4 | −0.6±1.3 | −0.8±1.3 | −0.6±1.0 | 0.316 |
| Percentile for weight-for-age | 545 | 37 | 36 | 27 | 29 | 48 | 0.021* |
| Z-score for weight-for-age | 545 | −0.4±1.4 | −0.4±1.2 | −0.5±1.4 | −0.6±1.5 | −0.2±1.2 | 0.085 |
| Body mass index z-score | 544 | −0.05±1.13 | 0.07±0.97 | −0.23±1.25 | −0.15±1.24 | 0.13±0.99 | 0.030 |
| Fontan Type | 513 | <.001 | |||||
| Atriopulmonary connection | 13% | <1% | 3% | 15% | 36% | ||
| TCPC intracardiac lateral tunnel | 59% | 52% | 62% | 70% | 50% | ||
| TCPC extracardiac lateral tunnel | 13% | 26% | 19% | 4% | 3% | ||
| TCPC extracardiac conduit | 13% | 21% | 15% | 9% | 6% | ||
| Other | 2% | 0% | <1% | 2% | 5% | ||
| Ventricular type | 546 | 0.023 | |||||
| Left Ventricular | 49% | 46% | 38% | 53% | 57% | ||
| Right Ventricular | 34% | 36% | 41% | 34% | 24% | ||
| Mixed | 18% | 19% | 22% | 13% | 19% | ||
| Stage II surgery performed | 546 | 75% | 93% | 88% | 78% | 35% | <.001 |
| Predominant rhythm | 518 | 0.255 | |||||
| Normal sinus rhythm | 67% | 63% | 69% | 71% | 63% | ||
| Atrial escape | 9% | 11% | 10% | 7% | 9% | ||
| Junctional escape | 6% | 9% | 6% | 5% | 3% | ||
| Paced | 8% | 10% | 4% | 9% | 11% | ||
| Other | 11% | 8% | 12% | 9% | 15% | ||
| Currently on pacemaker | 546 | 13% | 12% | 12% | 11% | 20% | 0.087 |
| Serology | |||||||
| Brain natriuretic peptide, pg/mL | 510 | 13 (7, 26) |
11 | 11 | 14 | 17 | 0.020* |
| Echocardiographic Measures | |||||||
| Heart rate z-score | 437 | −0.20±0.98 | −0.27±0.95 | −0.05±0.93 | −0.20±0.98 | −0.27±1.04 | 0.318 |
| End-diastolic volume z-score | 414 | −0.7±1.9 | −0.5±1.8 | −0.6±1.9 | −1.0±1.5 | −0.4±2.5 | 0.134 |
| End-systolic volume z-score | 414 | 0.2±2.4 | 0.4±2.1 | 0.2±2.4 | −0.1±2.1 | 0.6±3.3 | 0.206 |
| Ejection fraction z-score | 414 | −0.9±2.0 | −0.8±2.0 | −0.6±1.9 | −0.9±2.1 | −1.2±2.1 | 0.265 |
| Stroke volume z-score | 414 | −1.1±1.8 | −0.9±1.9 | −1.0±1.7 | −1.3±1.5 | −1.0±2.2 | 0.246 |
| Mass z-score | 406 | 1.0±2.3 | 0.7±2.0 | 0.9±2.3 | 0.8±2.1 | 1.7±2.7 | 0.011 |
| Ejection fraction, % | 414 | 59±10 | 59±10 | 60±10 | 59±11 | 57±11 | 0.252 |
| Mass:volume ratio g/mL | 406 | 1.21±0.39 | 1.16±0.41 | 1.20±0.38 | 1.23±0.38 | 1.26±0.38 | 0.321 |
| Mass:volume ratio z-score | 406 | 2.65±3.22 | 1.97±3.06 | 2.41±2.97 | 2.86±3.15 | 3.49±3.63 | 0.011 |
| dP/dtic, mm Hg/s | 449 | 1125 (802,1700) |
1257 (N=115) |
1134 (N=106) |
1114 (N=134) |
997 (N=94) |
0.027* |
| Tei index (by Tissue Doppler) | 462 | 0.64±0.19 | 0.60±0.17 (N=117) |
0.62±0.14 (N=99) |
0.63±0.17 (N=144) |
0.70±0.24 (N=102) |
<.001 |
| E’, cm/sec | 452 | 9.3±3.3 | 9.5±3.3 (N=113) |
9.6±2.9 (N=97) |
9.0±3.3 (N=141) |
9.5±3.8 (N=101) |
0.517 |
| E:A ratio | 344 | 1.48 (1.21,1.92) |
1.45 (N=88) |
1.46 (N=80) |
1.55 (N=105) |
1.48 (N=71) |
0.883* |
| E:E’ ratio | 297 | 7.79 (5.94,9.89) |
8.03 (N=74) |
7.15 (N=66) |
8.12 (N=94) |
7.63 (N=63) |
0.216* |
| Systemic ventricular FP rate, cm/sec | 143 | 64±20 | 63±16 (N=39) |
64±19 (N=40) |
69±24 (N=41) |
57±15 (N=23) |
0.107 |
| Restrictive pattern present | 344 | 52% | 52% | 54% | 56% | 44% | 0.421 |
| Diastolic dysfunction grade | 327 | 0.438† | |||||
| Normal | 28% | 23% | 27% | 25% | 38% | ||
| Impaired relaxation | 9% | 12% | 8% | 9% | 8% | ||
| Pseudonormalization | 41% | 45% | 47% | 42% | 29% | ||
| Restrictive | 22% | 20% | 18% | 24% | 26% | ||
| Overall AV valve regurgitation | 528 | 0.541† | |||||
| None | 26% | 27% | 17% | 33% | 22% | ||
| Mild | 55% | 53% | 59% | 50% | 60% | ||
| Moderate | 19% | 19% | 23% | 17% | 17% | ||
| Severe | <1% | 0% | <1% | 0% | 0% | ||
| Semilunar valve regurgitation | 314 | 0.148† | |||||
| None | 51% | 57% | 52% | 54% | 37% | ||
| Mild | 40% | 37% | 42% | 36% | 50% | ||
| Moderate | 9% | 7% | 6% | 10% | 13% | ||
| Cardiac MRI | |||||||
| N | 161 | 161 | 33 | 37 | 50 | 41 | |
| End-diastolic volume /BSA , mL/m | 85±25 | 96±26 | 89±29 | 81±20 | 79±23 | 0.011 | |
| End-systolic volume /BSA13, mL/m2 | 37±16 | 41±17 | 38±19 | 36±16 | 35±14 | 0.395 | |
| Ejection fraction, % | 57±10 | 58±8 | 59±9 | 56±12 | 56±9 | 0.476 | |
| Stroke volume /BSA, mL/ m2 | 51±14 | 52±12 | 52±14 | 48±14 | 51±15 | 0.500 | |
| Mass/BSA13, g/m2 | 72±21 | 75±17 | 70±18 | 68±19 | 76±26 | 0.182 | |
| Mass:volume ratio g/mL | 0.89±0.31 | 0.83±0.24 | 0.83±0.29 | 0.87±0.25 | 1.01±0.40 | 0.036 | |
| Exercise Performance Measures | |||||||
| N | 412 | 68 | 95 | 152 | 97 | ||
| Peak VO2, mL/kg/min | 403 | 26±7 | 27±8 (N=65) |
28±7 (N=94) |
26±6 (N=148) |
25±7 (N=96) |
0.028 |
| Percent predicted peak VO2 | 403 | 65±16 | 67±19 | 68±17 | 65±15 | 59±14 | <.001 |
| Peak VO2 consumption at AT, mL/kg/min | 317 | 19±6 | 24±8 (N=35) |
20±7 (N=65) |
19±6 (N=131) |
16±5 (N=86) |
<.001 |
| Percent predicted VAT | 317 | 78±25 | 95±30 | 82±26 | 77±22 | 69±20 | <.001 |
| Maximum heart rate, bpm | 405 | 154±23 | 152±22 (N=64) |
156±24 (N=95) |
157±21 (N=150) |
150±26 (N=96) |
0.122 |
| Measures of Functional Status | |||||||
| CHQ-PF Physical Summary Score | 511 | 45.3±11.9 | 45.7±12.1 | 45.8±10.7 | 45.4±12.6 | 44.1±11.7 | 0.689 |
| CHQ-PF Psychosocial Summary Score | 511 | 47.2±10.8 | 47.9±10.6 | 47.2±11.1 | 45.5±10.9 | 49.1±10.5 | 0.052 |
Percentages may not add to 100 due to rounding
P-value is from analysis of variance for continuous outcomes and chi-square test for categorical outcomes unless otherwise specified
Kruskal-Wallis test p-value
Mantel-Haenszel test for linear trend p-value
N = number of subjects for whom data are available
BMI = Body Mass Index
TCPC = Total Cavopulmonary Connection
CHQ-PF = Child Health Questionnaire-Parent Form
dP/dtic = Estimated maximum first derivative of ventricular pressure
E’ = Tissue Doppler peak early diastolic velocity
E:A ratio = Ratio of early to late atrioventricular valve diastolic velocities
E:E’ ratio = Ratio of atrioventricular valve to Tissue Doppler peak early diastolic velocity
FP = Flow propagation
BSA=Body surface area
AV = Atrioventricular
VO2 = Rate of oxygen consumption
AT = Anaerobic threshold
VAT = Peak VO2 consumption at anaerobic threshold
Stage II = Superior cavopulmonary anastomosis
MRI = Magnetic resonance imaging
Restrictive pattern E/A>2, or 1<E/A<2 and DT<140 ms
Diastolic dysfunction grades: 0, Normal = [(1<E/A≤2) and (DT≥140 ms) and (E/E’≤10)]; 1, Impaired relaxation = [E/A=1]; 2, Pseudonormalization = [(1<E/A≤2) and [(DT<140 ms) or (E/E’ >10) or (FP<55 cm/s)]]; 3. Restrictive = [E/A>2]
Cardiac Magnetic Resonance (CMR)
CMR studies performed using 1.5 T scanners were centrally interpreted by a single reader. Subjects were excluded if: unable to cooperate; had a pacemaker, defibrillator, permanent pacemaker lead, implanted device considered a contraindication according to institutional guidelines, or in some instances intravascular coils; or <6 weeks from endovascular device implantation.
The standardized imaging protocol included electrocardiographically-triggered gradient echo cine MR acquisitions in the vertical and horizontal long-axis planes, followed by contiguous short-axis imaging from the atrioventricular junction through the cardiac apex. Outcomes included EDV, ESV, mass indexed to BSA1.3, stroke volume (SV) indexed to BSA, and mass:EDV ratio (5).
Exercise Protocol
A maximal ramp exercise test was performed. Percent predicted of normal for maximum oxygen consumption (%predicted peak VO2) and VO2 at anaerobic threshold (%predicted VAT) were calculated (8).
Electrocardiogram
A standard 12-lead electrocardiogram (ECG) was performed and locally interpreted.
Serology
Resting BNP plasma concentration was centrally measured using the Shiniogi BNP-32 Human Assay (2).
Statistical Methods
Pre-specified subgroups were defined by ventricular morphology, Fontan procedure type, age at enrollment quartile (Table 2), age at Fontan procedure quartile (Table 4), and history of Stage II procedure (superior cavopulmonary connection or hemi-Fontan procedure). Subgroup differences in continuous outcomes were assessed using the t-test and analysis of variance, or nonparametric testing for highly skewed outcomes. Differences in categorical outcome measures were assessed using the chi-square test and, if ordinal, the Mantel-Haenszel test for linear trend. Modified Bonferroni and exact testing were applied to bootstrapped samples to obtain a p-value adjusted for multiple pairwise comparisons (9). Analysis of covariance and multivariate logistic regression were used to determine whether outcomes differed by subgroup after adjustment for age, with log transformation for BNP. Additional multivariate linear, logistic and multinomial regression modeling was used to analyze outcomes by age at Fontan and history of a Stage II procedure. All analyses were conducted using SAS version 9.1 and S-Plus version 6.2.
Table 4.
Fontan Cross-Sectional Study Patient Characteristics by Age at Fontan Procedure
| <2 yr | 2 to <3 yr | 3 to <4 yr | ≥4 yr | |||
|---|---|---|---|---|---|---|
| Characteristic | Mean ± SD Median or % |
Mean ± SD Median or % |
Mean ± SD Median or % |
Mean ± SD, Median or % |
P-value | Age-adj. P-value |
| N | 113 | 191 | 104 | 138 | ||
| Age at enrollment, yr | 11.1 | 10.8 | 10.8 | 13.3 | <.001* | |
| Age at volume unloading surgery, yr | 0.9±0.5 | 1.2±0.8 | 1.7±1.2 | 2.8±2.4 | <.001 | |
| Fontan type | <.001 | <.001 | ||||
| Atriopulmonary connection | 6% | 15% | 15% | 15% | ||
| TCPC intracardiac lateral tunnel | 81% | 62% | 54% | 42% | ||
| TCPC extracardiac lateral tunnel | 6% | 9% | 15% | 21% | ||
| TCPC extracardiac conduit | 4% | 13% | 12% | 20% | ||
| Other | 2% | 1% | 4% | 2% | ||
| Ventricular type | 0.200 | 0.150 | ||||
| Left ventricular | 40% | 49% | 57% | 49% | ||
| Right ventricular | 42% | 35% | 28% | 30% | ||
| Mixed | 19% | 16% | 15% | 21% | ||
| Stage II surgery performed | 69% | 77% | 73% | 78% | 0.365 | <.001 |
| Serology | ||||||
| Brain natriuretic peptide, pg/mL | 15 | 12 | 15 | 13 | 0.661* | 0.418 |
| Echocardiographic Measures | ||||||
| Heart rate z score | −0.14±0.82 | −0.36±1.04 | −0.32±1.00 | 0.07±0.95 | 0.003 | 0.002 |
| End-diastolic volume z-score | −0.9±1.8 | −0.6±1.7 | −0.5±2.3 | −0.6±1.9 | 0.471 | 0.470 |
| End-systolic volume z-score | 0.0±2.3 | 0.2±2.6 | 0.4±2.8 | 0.2±2.2 | 0.739 | 0.730 |
| Ejection fraction z-score | −0.9±2.0 | −0.8±2.1 | −1.0±1.8 | −1.0±2.2 | 0.839 | 0.924 |
| Stroke volume z-score | −1.4±1.6 | −1.0±1.6 | −1.0±2.0 | −1.0±2.0 | 0.407 | 0.378 |
| Mass z-score | 1.1±2.5 | 0.8±2.1 | 1.1±2.3 | 1.1±2.2 | 0.806 | 0.895 |
| Ejection fraction, % | 58±10 | 59±11 | 58±9 | 58±11 | 0.837 | 0.924 |
| Mass:volume ratio, g/mL | 1.29±0.41 | 1.18±0.37 | 1.19±0.37 | 1.20±0.41 | 0.166 | 0.154 |
| Mass:volume ratio z-score | 3.27±3.32 | 2.34±2.97 | 2.51±3.00 | 2.68±3.62 | 0.205 | 0.205 |
| dP/dtic, mm Hg/s | 1209 | 1164 | 1039 | 1081 | 0.257* | 0.595 |
| Tei index (by Tissue Doppler) | 0.57 | 0.60 | 0.62 | 0.65 | <.001* | 0.012 |
| E’, cm/sec | 8.7±3.2 | 9.2±3.2 | 9.8±2.9 | 9.8±3.9 | 0.054 | 0.035 |
| E:A ratio | 1.50 | 1.50 | 1.49 | 1.37 | 0.047* | 0.052 |
| E:E’ ratio | 8.37 | 7.46 | 7.78 | 7.75 | 0.363* | 0.034 |
| Systemic ventricular FP rate, cm/sec | 62±17 | 64±20 | 68±20 | 62±20 | 0.555 | 0.583 |
| Restrictive pattern present | 47% | 58% | 54% | 45% | 0.228 | 0.324 |
| Diastolic dysfunction grade | 0.218† | 0.515 | ||||
| Normal | 30% | 22% | 33% | 31% | ||
| Impaired relaxation | 8% | 7% | 7% | 14% | ||
| Pseudonormalization | 41% | 45% | 38% | 39% | ||
| Restrictive | 21% | 26% | 22% | 17% | ||
| Overall AV valve regurgitation | 0.002† | 0.010 | ||||
| None | 32% | 27.1% | 26.7% | 18.8% | ||
| Mild | 55% | 57.5% | 50.5% | 55.6% | ||
| Moderate | 13% | 14.9% | 22.8% | 25.6% | ||
| Severe | 0% | <1% | 0% | 0% | ||
| Semilunar valve regurgitation | 0.314† | 0.620 | ||||
| None | 53% | 56% | 46% | 46% | ||
| Mild | 39% | 38% | 48% | 40% | ||
| Moderate | 8% | 6% | 7% | 15% | ||
| Cardiac MRI | ||||||
| N | 39 | 65 | 35 | 54 | ||
| End-diastolic volume /BSA1.3, mL/m2 | 82±24 | 88±27 | 86±27 | 84±22 | 0.739 | 0.785 |
| End-systolic volume /BSA1.3, mL/m2 | 35±15 | 38±16 | 37±17 | 39±16 | 0.635 | 0.477 |
| Ejection fraction, % | 58±9 | 58±8 | 58±10 | 54±11 | 0.112 | 0.206 |
| Stroke volume /BSA, mL/m2 | 50±13 | 53±13 | 51±14 | 49±16 | 0.622 | 0.748 |
| Mass / BSA1.3, mL/m2 | 70±20 | 70±18 | 69±17 | 77±26 | 0.236 | 0.252 |
| Mass:volume ratio, g/mL | 0.90±0.32 | 0.86±0.36 | 0.85±0.23 | 0.94±0.27 | 0.538 | 0.859 |
| Exercise Performance Measurements | ||||||
| N | 80 | 140 | 81 | 111 | ||
| Peak VO2, mL/kg/min | 26±7 | 27±7 | 27±8 | 25±7 | 0.132 | 0.425 |
| Percent predicted peak VO2 | 64±16 | 66±17 | 65±18 | 63±15 | 0.441 | 0.893 |
| Peak VO2 consumption at AT, mL/kg/min | 18±6 | 20±7 | 20±7 | 17±6 | 0.006 | 0.102 |
| Percent predicted VAT | 74±23 | 83±27 | 80±26 | 74.4±20.8 | 0.049 | 0.151 |
| Maximum heart rate, bpm | 156±21 | 155±22 | 153±26 | 153±25 | 0.695 | 0.736 |
| Measures of Functional status | ||||||
| CHQ-PF Physical Summary Score | 45.4±12.2 | 45.0±12.8 | 44.8±12.4 | 46.0±9.6 | 0.862 | 0.736 |
| CHQ-PF Psychosocial Summary Score | 45.4±11.8 | 47.2±11.1 | 48.4±9.5 | 47.9±10.3 | 0.210 | 0.227 |
Percentages may not add to 100 due to rounding
P-value is from analysis of variance for continuous outcomes and chi-square test for categorical outcomes unless otherwise specified
Kruskal-Wallis test p-value
Mantel-Haenszel test for linear trend p-value
See Table 1 footnote for abbreviations legend
N = number of subjects for whom data are available
RESULTS
Overall Cohort
The 546 subjects were 11.9±3.4 years old at enrollment; 60% were male. The cohort was short (mean±SD, 34±30 percentile) and underweight (40±32 percentile). The most common diagnoses were tricuspid atresia and hypoplastic left heart syndrome (Table 1) and 59% had an intracardiac lateral tunnel Fontan procedure. A fenestration was performed in 68% and was found to be patent by echocardiography in 32%. Following the Fontan procedure, stroke and/or thrombosis occurred in 8%, seizures in 3%, and protein-losing enteropathy in 4%. The prevalences of developmental and cognitive abnormalities and surgical and catheter-based interventions have been published (10).
The distribution of ventricular morphologic subgroups was: LV, 49%; RV, 34%; and mixed, 18% (Table 2). One-third of subjects had predominant non-sinus rhythm, 10% a history of atrial tachycardia, and 13% a pacemaker. Ventricular mass and volume were obtained using echocardiography in 406 and 414 subjects, respectively, and by CMR in 161. Mean EF was 59±10% by echocardiography and 57±10% by CMR. EF was normal (echocardiographic z-score>-2) in 73%, although mean echocardiographic EDV, SV, and EF were lower and mass greater than those of normal subjects. The higher values of mass-to-volume ratio measured by echocardiography as compared with CMR reflect known echocardiography underestimating ventricular volume and overestimating mass (11). Forty nine percent of subjects had semilunar valve regurgitation, and 74% had AV valve regurgitation. Fifty-eight percent of subjects were taking an ACE inhibitor at enrollment. Diastolic function grade was normal in 28%. Median dP/dtic was 1125 mmHg/s (normal range 850–1350 mmHg/sec) (12). Tei index was 0.64±0.19 (normal range, 0.29 to 0.41). Median BNP was 13 pg/mL (range <4–652, mean 26±48 pg/mL).
The cohort had impaired exercise performance: mean %predicted peak VO2 65±16%; %predicted VAT 78±25%. Peak VO2 and VAT were in the normal range for 28% and 63%, respectively, independent of whether maximal effort was achieved.
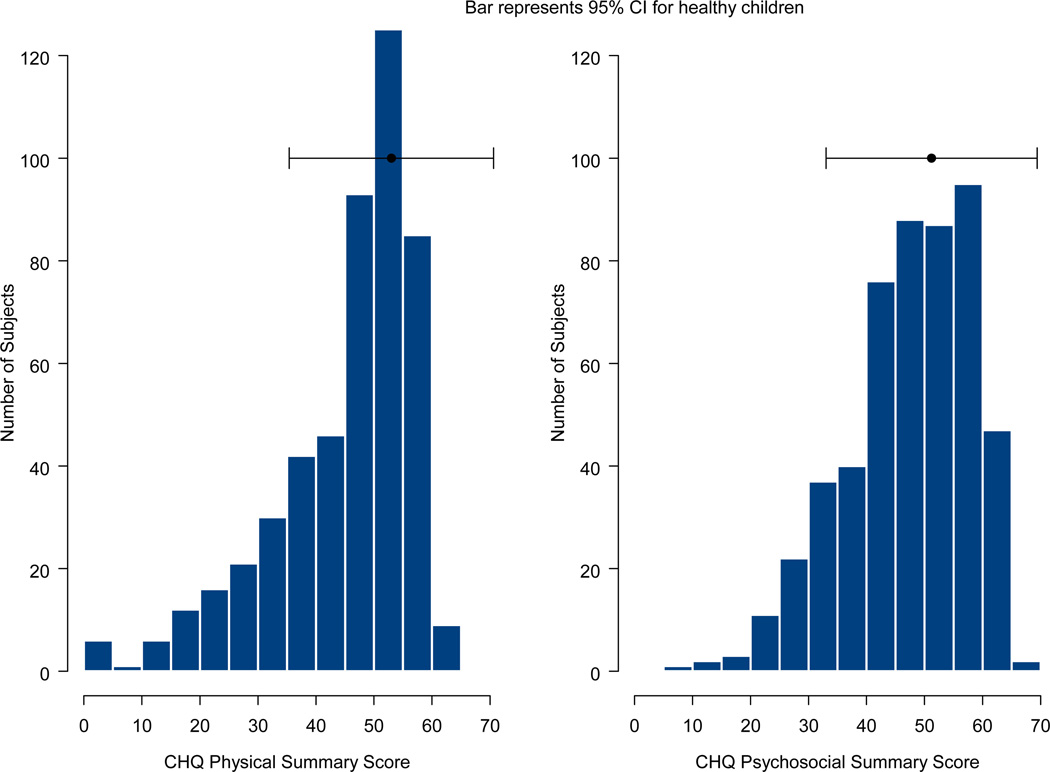
Mean CHQ summary scores were lower than those of historical healthy controls (3) (45±12 vs. 53±9 for Physical and 47±10 vs. 51±9 for Psychosocial). Individual scores were in the normal range in 81% and 87%, respectively (Figure 1).
Figure 1. CHQ-PF Summary Scores.
The distribution of CHQ-PF Physical and Psychosocial Summary Scores from 543 children enrolled in the Pediatric Heart Network Fontan Cross-Sectional Study. The bar represents the 95% confidence interval around the historical mean score for healthy children.
Gender
Males had lower BNP levels than females, even after adjustment for age (p=0.04). No gender differences were present for %predicted peak VO2 and %VAT. By both echocardiography and CMR, boys had larger EDV than girls (P=0.04), lower mass:EDV ratio (median by echocardiography 1.1 vs. 1.2, p=0.002), and higher SV/BSA by CMRI (53±14 vs. 48±14, p=0.03).
Age at Enrollment
The type of Fontan procedure differed by age at enrollment (p<0.001). Older children were more likely to have undergone an atrio-pulmonary connection (36% in ≥15 year old group vs. 1%–15% in younger age groups), while younger children were more likely to have received a total cavopulmonary connection (TCPC) lateral tunnel (26% and 19% in the two younger age groups vs. <5% otherwise). Ventricular morphology differed by age (p=0.02), in particular the ≥15 year old group had a greater proportion with LV morphology than the 9 to < 11 year old group (pairwise adjusted p=0.03). BNP increased with age (medians 11 to 14 for three youngest cohorts vs. 17 pg/mL for, the ≥15 year old group, p=0.020). Most other findings on echocardiography and CMR did not differ by age. Tei index increased with age (p<.001). Exercise performance differed among age groups and decreased with age (p<0.001).
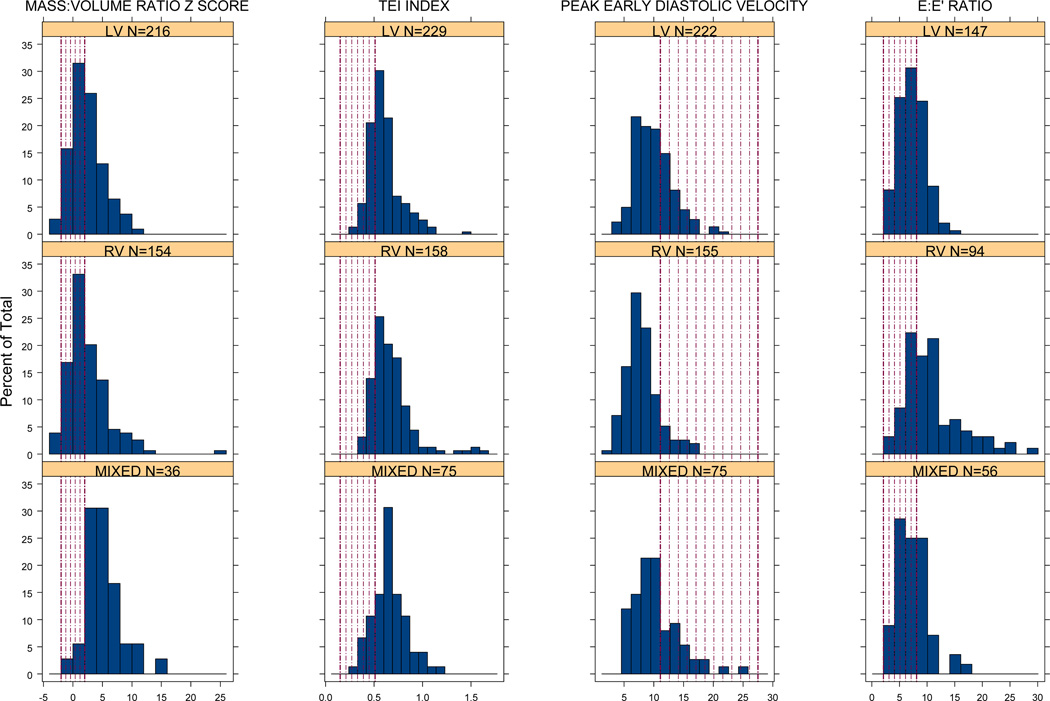
Ventricular Morphology
In general, ventricular function outcomes were worse for the RV subgroup compared with the LV, and to a lesser extent, the mixed, subgroups. EF z-score was −0.6±1.8, −1.4±2.3, and −0.5±2.1 for LV, RV, and mixed subgroups, respectively (p<0.001). Even after age adjustment, E’ was lower and E:E’ was higher in the RV subgroup (p<0.001, Figure 2). AV valve regurgitation was worst in the RV subgroup as was semilunar valve regurgitation (present in 65% for RV vs. 42% in LV and mixed subgroups, pairwise adjusted p<0.001).
Figure 2. Mass/EDV Ratio and Diastolic Function.
Histograms of echocardiographic mass to EDV ratio z score and measures of diastolic function assessed from tissue Doppler techniques, by ventricular morphology. Shaded regions indicate the 95% confidence interval for normal children aged 6 to 18 years old (19).
Age-adjusted exercise performance was weakly associated with ventricular morphology, with the LV subgroup having higher %predicted peak VO2 (3-group p=0.03) and %predicted VAT (3-group p=0.06) than the non-LV groups. Diastolic function grade, BNP, and CHQ summary scores did not differ by ventricular morphology (Table 3).
Table 3.
Fontan Cross-Sectional Study Patient Characteristics by Ventricular Morphology
| Characteristic | LV | RV | MIXED | ||
|---|---|---|---|---|---|
| Mean ± SD, Median or % |
Mean ± SD, Median or % |
Mean ± SD, Median or % |
P-value | Age-adj. P-value |
|
| N | 265(49%) | 184(34%) | 97(18%) | ||
| Age at enrollment, yr | 12.0 | 10.8 | 10.7 | 0.011* | |
| Age at Fontan, yr | 3.5±2.0 | 3.2±2.1 | 3.7±2.4 | 0.240 | |
| Age at volume unloading surgery, yr | 1.2 | 0.7 | 1.2 | <.001* | |
| Fontan Type | 0.017 | .102 | |||
| Atriopulmonary Connection | 19% | 7% | 10% | ||
| TCPC intracardiac lateral tunnel | 54% | 67% | 60% | ||
| TCPC extracardiac lateral tunnel | 11% | 14% | 13% | ||
| TCPC extracardiac conduit | 14% | 11% | 11% | ||
| Other | 2% | 1% | 3% | ||
| Stage II surgery performed | 68% | 88% | 69% | <.001 | <.001 |
| Serology | |||||
| Brain natriuretic peptide, pg/mL | 12 | 15 | 13 | 0.553* | 0.417 |
| Echocardiographic Measures | |||||
| Heart rate z-score | −0.27±0.99 | −0.10±0.97 | −0.21 ±0.93 | 0.238 | 0.243 |
| End-diastolic volume z-score | −0.8±1.9 (N=219) |
−0.4±2.0 (N=156) |
−1.1±1.5 (N=39) |
0.044 | 0.045 |
| End-systolic volume z-score | −0.1±2.2 | 0.8±2.7 | −0.4±2.1 | <.001 | <.001 |
| Ejection fraction z-score | −0.6±1.8 | −1.4±2.3 | −0.5±2.1 | <.001 | <.001 |
| Stroke volume z-score | −1.0±1.8 | −1.1±1.9 | −1.4±1.4 | 0.460 | 0.384 |
| Mass z-score | 0.8±2.2 (N=216) |
1.1±2.3 (N=154) |
1.9±1.8 (N=36) |
0.018 | 0.006 |
| Ejection fraction, % | 60±9 (N=219) |
56±12 (N=156) |
61±11 (N=39) |
<.001 | <.001 |
| Mass:volume ratio, g/mL | 1.17±0.33 (N=216) |
1.19±0.43 (N=154) |
1.52±0.42 (N=36) |
<.001 | <.001 |
| Mass:volume ratio z score | 2.37±2.74 | 2.50±3.63 | 4.99±3.18 | <.001 | <.001 |
| dP/dtic, mm Hg/s | 1209 (N=220) |
1077 (N=150) |
1073 (N=79) |
0.071* | 0.062 |
| Tei index (by Tissue Doppler) | 0.58 (N=216) |
0.63 (N=158) |
0.64 (N=75) |
<.001* | <.001 |
| E’, cm/sec | 10.0±3.2 (N=222) |
8.0±2.8 (N=155) |
10.4±3.9 (N=75) |
<.001 | <.001 |
| E:A ratio | 1.48 (N=169) |
1.45 (N=109) |
1.54 (N=66) |
0.730* | 0.593 |
| E:E’ ratio | 7.21 (N=147) |
10.00 (N=94) |
6.96 (N=56) |
<.001* | <.001 |
| Systemic ventricular FP rate, cm/sec | 64±18 (N=71) |
64±22 (N=51) |
62±19 (N=21) |
0.907 | 0.899 |
| Restrictive pattern present | 53% | 51% | 52% | 0.974 | 0.879 |
| Diastolic dysfunction grade | 0.035 | 0.100 | |||
| Normal | 32% | 19% | 32% | ||
| Impaired relaxation | 9% | 10% | 8% | ||
| Pseudonormalization | 33% | 53% | 42% | ||
| Restrictive | 26% | 18% | 18% | ||
| Overall AV valve regurgitation | <.001 | <.001 | |||
| None | 38% | 12% | 20% | ||
| Mild | 48% | 69% | 49% | ||
| Moderate | 15% | 18% | 31% | ||
| Severe | 0% | <1% | 0% | ||
| Semilunar valve regurgitation ** | .004 | 0.001 | |||
| None | 58% | 35% | 58% | ||
| Mild | 34% | 55% | 32% | ||
| Moderate | 8% | 10% | 10% | ||
| Cardiac MRI | |||||
| N | 100 | 55 | 38 | ||
| End-diastolic volume /BSA1.3, mL/m2 | 79±22 (N=86) |
93±29 (N=44) |
92±24 (N=31) |
0.003 | 0.012 |
| End-systolic volume /BSA1.3, mL/m2 | 34±14 | 43±21 | 38±11 | 0.011 | 0.019 |
| Ejection fraction, % | 57±9 | 55±11 | 59±7 | 0.176 | 0.122 |
| Stroke volume /BSA, mL/ m2 | 49±13 | 51±13 | 57±16 | 0.015 | 0.019 |
| Mass / BSA1.3, mL/m2 | 70±20 | 75±21 | 73±20 | 0.328 | 0.290 |
| Mass:volume ratio, mL/mL | 0.92±0.32 | 0.87±0.33 | 0.82±0.22 | 0.274 | 0.402 |
| Exercise Performance Measures | |||||
| N | 219 | 128 | 65 | ||
| Peak VO2, mL/kg/min | 27±7 (N=216) |
26±7 (N=124) |
26±7 (N=50) |
0.445 | 0.226 |
| Percent predicted peak VO2 | 66±17 | 63±16 | 63±16 | 0.141 | 0.031 |
| Peak VO2 consumption at AT, mL/kg/min | 19±6 (N=173) |
19±7 (N=94) |
18±6 (N=50) |
0.795 | 0.352 |
| Percent predicted VAT | 80±24 | 76±25 | 75±24 | 0.269 | 0.061 |
| Maximum heart rate, bpm | 155±23 (N=215) |
153±23 (N=126) |
153±25 (N=64) |
0.837 | 0.795 |
| Measures of Functional Status | |||||
| CHQ-PF Physical Summary Score | 44.7±12.4 | 45.5±11.4 | 46.4±11.0 | 0.487 | 0.531 |
| CHQ-PF Psychosocial Summary Score | 48.0±10.0 | 46.4±11.8 | 46.7±11.1 | 0.261 | 0.288 |
Percentages may not add to 100 due to rounding
P-value is from analysis of variance for continuous outcomes and chi-square test for categorical outcomes unless otherwise specified
Kruskal-Wallis test p-value
See Table 1 footnote for abbreviations legend
N = number of subjects for whom data are available
Type of Fontan Procedure
Few differences were found by type of Fontan procedure after adjustment for age. They included higher BNP in subjects with atriopulmonary connection (raw median 18 pg/mL) compared with BNP in subjects with extracardiac conduits and lateral tunnels (raw medians 13 and 10 pg/mL, respectively, pairwise adjusted p=0.01 and p=0.03). Age-adjusted %predicted VAT differed by type of Fontan procedure (p<0.001); those who received an intracardiac lateral tunnel (adjusted mean±SE, 73±2%) had lower %predicted VAT than those with an atriopulmonary connection (84±3%) or with an extracardiac conduit (92±4%).
Age at Fontan Procedure
Type of Fontan procedure differed by age at Fontan procedure (p<0.001). Intracardiac lateral tunnel was most commonly used for Fontan procedures performed at <2 years of age (81%), and decreased steadily with age. Conversely, extracardiac tunnel procedures were performed in 6% of subjects who underwent Fontan at <2 years and in 21% of subjects who underwent Fontan at ≥4 years. Age at Fontan was similar for those who did and did not undergo a Stage II procedure (3.5±2.0 vs. 3.2±2.3 years).
Rhythm status was associated with age at Fontan (p<0.0001). Normal sinus rhythm was present in 70%–74% of those with Fontan performed under age 3 years, and 59%–62% of those with Fontan performed ≥3 years. This association remained after adjustment for age at enrollment (p=0.01).
Age-adjusted mean Tei index (0.60, 0.62, 0.66, and 0.68 in the four Fontan age groups, p<0.001) was significantly worse for subjects who had a Fontan at later ages, even after adjustment for age at enrollment and for ventricular morphology. Moderate to severe AV valve regurgitation was more common in children with Fontan performed at ≥3 years (23%–26%) compared to children with Fontan performed at <2 or 2-<3 years (13%–16%). After adjustment for age at enrollment, greater severity of AV valve regurgitation was associated with older age at Fontan (p=0.010). Subjects with RV or mixed ventricular morphology who underwent the Fontan at older ages were more likely to have worse E’, and RV subjects who underwent Fontan at older ages had worse E/E’, even after adjustment for age at enrollment (morphology by age at Fontan interactions p≤0.05).
BNP, CHQ summary scores, and systolic function did not differ by age at Fontan (Table 4) and, after adjusting for age, exercise performance was also unrelated to age at Fontan.
Stage II Procedure
Subjects who underwent a Stage II procedure (66%) were younger at enrollment (10.9±2.9 vs. 14.7±3.2 years) and were less likely to have undergone an atrio-pulmonary connection (7% vs. 33%) even after age adjustment. The distribution of LV, RV, and mixed subgroup subjects who underwent a Stage II procedure (44%, 40%, 16%) was different than in those who did not (62%, 16%, 22%; p<0.001). No differences were found in predominant rhythm by Stage II status. After adjustment for age, Stage II surgery was not associated with ventricular function or exercise performance, except for higher ventricular mass in subjects who underwent Stage II surgery (age-adjusted mean±SE 1.2±0.1 vs. 0.4±0.3, p=0.008).
Stage II surgery was associated with lower age-adjusted mean log BNP for LV subgroup but not RV and mixed subgroups (Stage II by ventricular morphology interaction p=0.008). The Psychosocial summary score was lower in Stage II subjects (age-adjusted mean±SE 46.4±0.6 vs. 49.7±1.0, p=0.008) and was not explained by ventricular morphology or other factors. No other age-adjusted study outcomes differed significantly by Stage II surgery status within morphologic subgroup.
DISCUSSION
This study is the largest to date of children who have undergone the Fontan operation. Systematic data on medical history, demographic variables and quantitative measures of ventricular systolic and diastolic function, exercise performance, neurohormonal response, heart rhythm, and functional health status were obtained. Strengths of the study design are contemporaneous data collection, central interpretation of key measures, and large cohort size from multiple geographically dispersed centers. The novelty of the study follows, in part, from sophisticated measurement of ventricular diastolic function, using tissue Doppler echocardiography, BNP plasma concentration measurement, and large size of the study that permitted for the first time a statistically robust assessment of how outcomes differ by ventricular morphology, age at Fontan, and history of Stage II procedure.
OVERALL COHORT
Ventricular Function
EF was normal in the majority (73%) of subjects. Our finding of smaller-than-normal EDV contrasts with a study where EDV was 1.6 times larger than normal (13). Such differences are most likely related to changes in management over time such as earlier volume-unloading surgery. Smaller EDV, as compared with normal subjects, may be a reflection of aerobic deconditioning and may contribute to the blunted ability to increase stroke volume with exercise (14).
Our finding of abnormal diastolic function in 72% of children who had undergone a Fontan has not been previously reported and is concerning. These indices are dependent on cardiac loading conditions and are unable to distinguish between enhanced chamber compliance and impaired relaxation (7). However, given our findings, future studies, using invasive approaches, are needed to ascertain whether these children are at risk for diastolic heart failure.
Functional Health Status
Over 80% of subjects scored in the normal range on the CHQ. However, on average the parents perceived their children as having lower physical and psychosocial functional status than that of historic healthy controls. The lower Physical summary scores are similar to those for children who have undergone thoracic organ transplantation or cardioverter defibrillator implantation (15,16).
Exercise Performance
Maximal exercise performance was lower than normal and worse in older subjects, consistent with previous studies (14). The same mechanisms proposed previously to impair exercise performance in single ventricle subjects, including absence of a subpulmonary pumping chamber, abnormal endothelial cell function, increased systemic vascular resistance, decreased muscle mass, and deconditioning, are likely present in our subjects (1,14). The finding that exercise performance (%predicted VAT) was lowest in the intracardiac lateral tunnel group, among Fontan types, was an unexpected and unexplained finding.
Brain-Type Natriuretic Peptide (BNP)
The subjects demonstrated a wide range of BNP plasma concentrations. The mean concentration was similar to subjects without congenital heart disease and those with congenital heart disease without ventricular dysfunction, and lower than that of single ventricle patients with systemic ventricular failure (17). Our finding of lower age-adjusted BNP concentrations in male versus female subjects is consistent with adult data, but not with a report of a gender difference only in healthy post-pubertal children (18).
VENTICULAR MORPHOLOGIC SUBGROUPS
Systolic and Diastolic Function
Our finding of apparently impaired systolic function in the RV subgroup relative to the LV and mixed subgroups is consistent with the general opinion that the structure of the right ventricle is suboptimal for a systemic ventricle (1). The greater prevalence of diastolic dysfunction in the RV subgroup, measured by E’ and E:E’, is not likely a consequence of difference in loading conditions compared to the LV and mixed subgroups (19). Of note, the majority of subjects in each morphologic subgroup had Tei Index, E’, and E:E’ values outside a two-standard deviation range for normal children (20).
Valve regurgitation
Similar to concerns about the relative inadequacy of the RV as a systemic ventricle, the tricuspid valve is thought to be more likely to fail as a systemic AV valve. Consistent with that notion, subjects with RV morphology were most likely and those with LV morphology least likely to have AV valve regurgitation. The higher prevalence of semilunar valve regurgitation in subjects with RV morphology may be related to the aortic reconstruction and intrinsic characteristics of the pulmonary (neo-aortic) valve in patients with hypoplastic left heart syndrome.
Functional Health Status and BNP
Although measures of ventricular performance and exercise capacity varied according to ventricular morphology, CHQ scores and BNP levels did not.
AGE AT FONTAN
Subjects who were older at time of Fontan had worse AV valve function and decreased likelihood of being in sinus rhythm. Poorer valve function and a decrease in sinus rhythm may be related to a longer period of volume overloading (21). These negative associations with older age at Fontan might be used as a rationale to complete the Fontan at an earlier age.
HISTORY OF STAGE II PROCEDURE
The performance of a Stage II procedure in single ventricle patients follows from the general assumption that this procedure decreases volume loading and its negative effects. Although we postulated that Stage II surgery might be beneficial in some patients, we found that a Stage II procedure was not associated with laboratory measures except for BNP and ventricular mass and a negative association with Psychosocial Summary score. Our findings suggest that further study is needed to assess the impact of performing a Stage II procedure.
STUDY LIMITATIONS
This study was limited in several respects. Because only survivors of the Fontan procedure were studied, our findings may not reflect the characteristics of subjects who died in the years following the Fontan. Although the generalizability of our findings is supported by the enrolled subjects being of similar age and functional health status as the eligible but non-consenting subjects (2) and being from geographically dispersed regions, our subjects were recruited exclusively from major medical centers. Functional health status was measured using parental report instruments which may not match child perception (22).
CONCLUSIONS
This largest-to-date multi-center study of children who have undergone a Fontan procedure provides an overview of functional health status, ventricular performance and exercise performance in current survivors of the Fontan procedure. Ventricular systolic function and functional health status were within normal range in the majority of subjects. Ventricular function and valvar function were negatively associated with RV morphology. AV valve function was negatively associated with older age at Fontan completion. Continued follow-up of these subjects will determine if functional health status is eventually related to measures of ventricular diastolic function. Effective strategies to preserve ventricular and valvar function, particularly for patients with RV morphology, are needed.
Supplementary Material
Table 5.
Fontan Cross-Sectional Study Patient Characteristics by Superior Cavopulmonary Connection (Stage II Surgery) Performed
| With Stage II | Without Stage II | |||
|---|---|---|---|---|
| Characteristic | Mean ± SD Median Or % |
Mean ± SD Median Or % |
P-value | Age-adjusted pvalue |
| N | N=408 | N=138 | ||
| Age at enrollment, yr | 10.3 | 15.7 | <.001* | − |
| Age at Fontan, yr | 3.5±2.0 | 3.2±2.3 | 0.318 | <.001 |
| Age at volume unloading surgery, yr | 0.8 | 2.8 | <.001* | <.001 |
| Male | 60% | 60% | 1.00 | .497 |
| Race | 0.024 | .491 | ||
| White | 78% | 86% | ||
| Black | 11% | 9% | ||
| Asian | 2% | 3% | ||
| Other | 9% | 2% | ||
| Hispanic | 7% | 5% | 0.550 | .588 |
| Growth | ||||
| Percentile for stature-for-age | 24 | 31 | 0.085* | .195 |
| Z-score for stature-for-age | −0.7±1.3 | −0.5±1.1 | 0.056 | .054 |
| Percentile for weight-for-age | 32 | 48 | <.001* | .005 |
| Z-score for weight-for-age | −0.5±1.4 | −0.1±1.1 | 0.001 | <.001 |
| Body mass index z-score | −0.13±1.17 | 0.18±1.00 | 0.004 | .003 |
| Fontan type | <.001 | .022 | ||
| Atriopulmonary connection | 7% | 33% | ||
| TCPC Intracardiac lateral tunnel | 61% | 56% | ||
| TCPC extracardiac lateral tunnel | 16% | 3% | ||
| TCPC extracardiac conduit | 16% | 2% | ||
| Other | <1% | 7% | ||
| Ventricular type | <.001 | .108 | ||
| Left Ventricular | 44% | 62% | ||
| Right Ventricular | 40% | 16% | ||
| Mixed | 16% | 22% | ||
| Currently on pacemaker | 14.2% | 13.8% | 1.000 | .059 |
| Serology | ||||
| BNP, pg/ml† | 11.8 | 17.6 | 0.001* | .066 |
| Predominant rhythm | 0.772 | .292 | ||
| Normal sinus rhythm | 66% | 70% | ||
| Atrial escape | 9% | 9% | ||
| Junctional escape | 6% | 4% | ||
| Paced | 9% | 6% | ||
| Other | 10% | 11% | ||
| Echo | ||||
| Heart rate z-score | −0.17±0.99 | −0.29±0.92 | 0.267 | .247 |
| End-diastolic volume z-score | −0.6±1.8 | −0.9± 2.3 | 0.167 | .111 |
| End-systolic volume z-score | 0.3± 2.2 | −0.0±3.0 | 0.400 | .190 |
| Ejection fraction z-score | −0.9±2.1 | −0.9±2.0 | 0.983 | .340 |
| Stroke volume z-score | −1.0±1.8 | −1.3±1.8 | 0.086 | .168 |
| Mass z-score | 1.0±2.1 | 0.8±2.6 | 0.323 | .008 |
| Ejection fraction, % | 59±11 | 58±10 | 0.966 | .343 |
| Mass:volume ratio, g/ml | 1.21±0.39 | 1.21±0.39 | 0.957 | .316 |
| Mass:volume ratio z-score | 2.57±3.10 | 2.92±3.63 | 0.356 | .380 |
| dp/dtic, mmHg/s | 1182 (N=341) |
1030 (N=108) |
0.044* | .368 |
| Tei index (by Tissue Doppler) | 0.6 (N=346) |
0.6 (N=116) |
0.303* | .175 |
| E’, cm/sec | 9.5±3.4 (N=338) |
9.0±3.2 (N=114) |
0.226 | .293 |
| E: A ratio | 1.48 (N=247) |
1.48 (N=97) |
0.985* | .530 |
| E: E’ ratio | 7.79 (N=215) |
7.80 (N=82) |
0.400* | .177 |
| Systemic ventricular FP rate, cm/sec | 65±21 | 60±15 | 0.111 | .219 |
| Restrictive pattern present | 53% | 49% | 0.472 | .932 |
| Diastolic dysfunction grade | 0.280 | .830 | ||
| Normal | 25% | 33% | ||
| Impaired relaxation | 9% | 9% | ||
| Pseudonormalization | 44% | 33% | ||
| Restrictive | 21% | 24% | ||
| Overall AV valve regurgitation grade | 0.725 | .406 | ||
| None | 25% | 29% | ||
| Mild | 56% | 54% | ||
| Moderate | 19% | 17% | ||
| Severe | <1% | 0% | ||
| Semilunar valve regurgitation grade | 0.830 | .482 | ||
| None | 52% | 48% | ||
| Mild | 39% | 44% | ||
| Moderate | 9% | 8% | ||
| Cardiac MRI | ||||
| N | 108 | 53 | ||
| End-diastolic volume / BSA1.3, ml/m2 | 87±27 | 81±21 | 0.109 | .658 |
| End-systolic volume / BSA1.3, ml/m2 | 38±17 | 36±14 | 0.391 | .739 |
| Ejection Fraction, % | 57±10 | 56±9 | 0.555 | .986 |
| Stroke volume/ BSA, mL/m2 | 51±14 | 50±13 | 0.596 | .884 |
| Mass / BSA1.3, g/m2 | 73±21 | 69±19 | 0.205 | .130 |
| Mass:volume ratio g/mL | 0.88±0.28 | 0.90±0.36 | 0.751 | .455 |
| Exercise Performance Measurements | ||||
| Peak VO2, ml/kg/min | 27±7.0 | 25±7 | 0.015 | .207 |
| Percent predicted peak VO2 | 66±17 | 60±15 | <.001 | .067 |
| Peak VO2 consumption at AT, ml/kg/min | 20±7 | 17±6 | 0.001 | .658 |
| Percent predicted VAT | 81±26 | 72±21 | 0.001 | .346 |
| Max heart rate, bpm | 155±24 | 153 ± 22 | 0.390 | .490 |
| Measures of Functional Status | ||||
| CHQ-PF Physical Summary Score | 45.3±12.1 | 45.3±11.3 | 0.974 | .555 |
| CHQ-PF Psychosocial Summary Score | 46.5±11.1 | 49.3±9.8 | 0.010 | .008 |
Percentages may not add to 100 due to rounding
P-value is from analysis of variance for continuous outcomes and chi-square test for categorical outcomes unless otherwise specified
Wilcoxon rank sum test p-value
There was significant age-adjusted interaction of Stage II status and ventricular morphologic subtype (p=0.008), with lower BNP for subjects who underwent Stage II surgery compared with those who did not in the LV subgroup (log BNP 2.51±0.07 vs. 2.98±0.11, p<.001), but no difference in BNP by Stage II surgery status for subjects with RV or mixed type morphology.
N = number of subjects for whom data are available
See Table 1 footnote for abbreviations legend
ACKNOWLEDGEMENTS
The authors thank Minmin Lu for her dedicated assistance with graphics and analysis of the data.
This work was supported by the National Heart, Lung, and Blood Institute, NIH/DHHS, U01 HL68269 (Anderson), HL68270 (Sleeper, Colan, Gallagher, Mahony, Geva, Margossian, Schwartz), HL68292 (Williams), HL68290 (Gersony), HL68288 (McCrindle), HL68285 (Breitbart), HL68281 (Atz), and HL68279 (Clark, Paridon).
APPENDIX
National Heart, Lung, and Blood Institute
Gail Pearson, Mario Stylianou, Judith Massicot-Fisher, Marsha Mathis, Victoria Pemberton
Data Coordinating Center
New England Research Institutes, Lynn Sleeper, Steven Colan, Paul Mitchell, Dianne Gallagher, Patti Nash, Gloria Klein, Minmin Lu
Network Chair
Lynn Mahony, University of Texas Southwestern Medical Center
Clinical Site Investigators
Children’s Hospital Boston, Jane Newburger (PI), Stephen Roth, Roger Breitbart, Jonathan Rhodes, Jodi Elder, Ellen McGrath; Children’s Hospital of New York, Welton M. Gersony (PI), Seema Mital, Beth Printz, Ashwin Prakash, Darlene Servedio; Children’s Hospital of Philadelphia, Victoria Vetter (PI), Bernard J. Clark, Mark Fogel, Steven Paridon, Jack Rychik, Margaret Harkins, Jamie Koh; Duke University, Page A. W. Anderson (PI), Rene Herlong, Lynne Hurwitz, Jennifer S. Li, Ann Marie Nawrocki; Medical University of South Carolina, J. Philip Saul (PI), Andrew M. Atz, Andrew D. Blaufox, Girish Shirali, Jon Lucas, Amy Blevins; Primary Children’s Medical Center, Salt Lake City, Utah, LuAnn Minich (PI), Richard Williams, Linda Lambert, Michael Puchalski; Hospital for Sick Children, Toronto, Brian McCrindle (PI), Timothy Bradley, Kevin Roman, Jennifer Russell, Shi-Joon Yoo, Elizabeth Radojewski, Nancy Slater
Core Laboratories
Cardiac MRI, Children’s Hospital Boston: Tal Geva (Director); Andrew J. Powell Echocardiography, Children’s Hospital Boston: Steven Colan (Director), Marcy Schwartz, Renee Margossian
Protocol Review Committee
Michael Artman, Chair; Dana Connolly, Timothy Feltes, Julie Johnson, Jeffrey Krischer, G. Paul Matherne.
Data and Safety Monitoring Board
John Kugler, Chair; Kathryn Davis, David J. Driscoll, Mark Galantowicz, Sally A. Hunsberger, Thomas J. Knight, Catherine L. Webb, Lawrence Wissow.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors state no conflicts of interest exist.
Contributor Information
Page A. W. Anderson, Duke University Medical Center, Durham, NC.
Lynn A. Sleeper, New England Research Institutes, Watertown, MA.
Lynn Mahony, University of Texas Southwestern Medical Ctr, Dallas, TX.
Steven D. Colan, Children’s Hospital Boston, Boston, MA.
Andrew M. Atz, Medical University of South Carolina, Charleston, SC.
Roger E. Breitbart, Children’s Hospital Boston, Boston MA.
Welton M. Gersony, Columbia University Medical Center, New York, NY.
Dianne Gallagher, New England Research Institutes, Watertown, MA.
Tal Geva, Children’s Hospital Boston, Boston MA.
Renee Margossian, Children’s Hospital Boston, Boston MA.
Brian W. McCrindle, The Hospital for Sick Children, Toronto ON.
Stephen Paridon, Children’s Hospital of Philadelphia, Philadelphia, PA.
Marcy Schwartz, Children’s Hospital Boston, Boston MA.
Mario Stylianou, National Heart, Lung, and Blood Institute, Bethesda, MD.
Richard V. Williams, Primary Children’s Medical Center, Salt Lake City, UT.
Bernard J. Clark, III, Children’s Hospital of Philadelphia, Philadelphia, PA.
REFERENCES
- 1.Khairy P, Poirier N, Mercier LA. Univentricular heart. Circulation. 2007;115:800–812. doi: 10.1161/CIRCULATIONAHA.105.592378. [DOI] [PubMed] [Google Scholar]
- 2.Sleeper LA, Anderson P, Hsu DT, et al. Design of a large cross-sectional study to facilitate future clinical trials in children with the Fontan palliation. Am Heart J. 2006;152:427–433. doi: 10.1016/j.ahj.2006.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landgraf JM, Abetz L, Ware JE. The Child Health Questionnaire (CHQ) User's Manual. Second Printing. Boston, MA: HealthAct; 1999. [Google Scholar]
- 4.Perwien AR, Kratochvil CJ, Faries DE, Vaughan BS, Spencer T, Brown RT. Atomoxetine treatment in children and adolescents with attention-deficit hyperactivity disorder: what are the long-term health-related quality-of-life outcomes? J Child Adolesc Psychopharmacol. 2006;16:713–724. doi: 10.1089/cap.2006.16.713. [DOI] [PubMed] [Google Scholar]
- 5.Sluysmans T, Colan SD. Theoretical and empirical derivation of cardiovascular allometric relationships in children. J Appl Physiol. 2005;99:445–457. doi: 10.1152/japplphysiol.01144.2004. [DOI] [PubMed] [Google Scholar]
- 6.Tei C, Ling LH, Hodge DO, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function--a study in normals and dilated cardiomyopathy. J Cardiol. 1995;26:357–366. [PubMed] [Google Scholar]
- 7.Nishimura RA, Tajik AJ. Evaluation of diastolic filling of left ventricle in health and disease: Doppler echocardiography is the clinician's Rosetta Stone. J Am Coll Cardiol. 1997;30:8–18. doi: 10.1016/s0735-1097(97)00144-7. [DOI] [PubMed] [Google Scholar]
- 8.Cooper DM, Weiler-Ravell D. Gas exchange response to exercise in children. Am Rev Respir Dis. 1984;129:S47–S48. doi: 10.1164/arrd.1984.129.2P2.S47. [DOI] [PubMed] [Google Scholar]
- 9.Westfall PH, Young SS. Resampling-Based Multiple Testing. New York: John Wiley & Sons, Inc; 1993. [Google Scholar]
- 10.McCrindle BW, Williams RV, Mitchell PD, et al. Relationship of patient and medical characteristics to health status in children and adolescents after the Fontan procedure. Circulation. 2006;113:1123–1129. doi: 10.1161/CIRCULATIONAHA.105.576660. [DOI] [PubMed] [Google Scholar]
- 11.van den Bosch AE, Robbers-Visser D, Krenning BJ, et al. Comparison of realtime three-dimensional echocardiography to magnetic resonance imaging for assessment of left ventricular mass. Am J Cardiol. 2006;97:113–117. doi: 10.1016/j.amjcard.2005.07.114. [DOI] [PubMed] [Google Scholar]
- 12.Rhodes J, Fulton DR, Levine JC, Marx GR. Comparison between the mean dP/dt during isovolumetric contraction and other echocardiographic indices of ventricular function. Echocardiography. 1997;14:215–222. doi: 10.1111/j.1540-8175.1997.tb00713.x. [DOI] [PubMed] [Google Scholar]
- 13.Sluysmans T, Sanders SP, van der Velde M, et al. Natural history and patterns of recovery of contractile function in single left ventricle after Fontan operation. Circulation. 1992;86:1753–1761. doi: 10.1161/01.cir.86.6.1753. [DOI] [PubMed] [Google Scholar]
- 14.McCrindle BW, Williams RV, Mital S, et al. Reduced physical activity levels after the Fontan procedure: Related to exercise capacity or own health perception? Arch Dis Child. 2007 Feb 16; doi: 10.1136/adc.2006.105239. EPub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DeMaso DR, Lauretti A, Spieth L, et al. Psychosocial factors and quality of life in children and adolescents with implantable cardioverter-defibrillators. Am J Cardiol. 2004;93:582–587. doi: 10.1016/j.amjcard.2003.11.022. [DOI] [PubMed] [Google Scholar]
- 16.Hirshfeld AB, Kahle AL, Clark BJ, 3rd, Bridges ND. Parent-reported health status after pediatric thoracic organ transplant. J Heart Lung Transplant. 2004;23:1111–1118. doi: 10.1016/j.healun.2003.08.016. [DOI] [PubMed] [Google Scholar]
- 17.Law YM, Ettedgui J, Beerman L, Maisel A, Tofovic S. Comparison of plasma B-type natriuretic peptide levels in single ventricle patients with systemic ventricle heart failure versus isolated cavopulmonary failure. Am J Cardiol. 2006;98:520–524. doi: 10.1016/j.amjcard.2006.02.058. [DOI] [PubMed] [Google Scholar]
- 18.Koch A, Singer H. Normal values of B type natriuretic peptide in infants, children, and adolescents. Heart. 2003;89:875–878. doi: 10.1136/heart.89.8.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation. 2002;105:1387–1393. doi: 10.1161/hc1102.105289. [DOI] [PubMed] [Google Scholar]
- 20.Eidem BW, McMahon CJ, Cohen RR, et al. Impact of cardiac growth on Doppler tissue imaging velocities: a study in healthy children. J Am Soc Echocardiogr. 2004;17:212–221. doi: 10.1016/j.echo.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 21.Milanesi O, Stellin G, Colan SD, et al. Systolic and diastolic performance late after the Fontan procedure for a single ventricle and comparison of those undergoing operation at <12 months of age and at >12 months of age. Am J Cardiol. 2002;89:276–280. doi: 10.1016/s0002-9149(01)02227-5. [DOI] [PubMed] [Google Scholar]
- 22.Levi RB, Drotar D. Health-related quality of life in childhood cancer: discrepancy in parent-child reports. Int J Cancer Suppl. 1999;12:58–64. doi: 10.1002/(sici)1097-0215(1999)83:12+<58::aid-ijc11>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.