Abstract
Previous studies have identified the relationship between parental loss and psychopathology later in life. However, this relationship varied depending on the kind of loss, the parent involved, and the type of psychopathology. In the present study, we examined the association between parental loss (any loss, death, and separation) during childhood and lifetime risk for seven common psychiatric and substance use disorders in a sample of 2605 male twins from the Virginia population-based twin registry. Using structural equation modeling (SEM), we also examined the extent to which the influence of parental loss contributes to adult psychopathology. Parental separation was associated with a wide range of adult psychopathology, whereas parental death was specifically associated with phobia and alcohol dependence. Maternal and paternal separation were almost equally associated with most forms of psychopathology. SEM suggested that parental loss accounted for about 10% of the variance of adult psychopathology, of which parental separation had the strongest impacts on risk for depression and drug abuse/dependence (11% of the total variance). Our findings suggest that early parental separation has stronger and wider effects on adult psychopathology than parental death.
Keywords: parental loss, separation, death, mental disorders, twins
1. Introduction
In “Mourning and Melancholia” Freud (1917) wrote about the relationship between object loss and depression. Since then, parental loss during childhood has been widely considered as an important risk factor for adult psychopathology such as depression (Brown et al., 1977; Roy, 1983; Kendler et al., 1992), anxiety disorders (Raskin et al., 1982; Faravelli et al., 1985; Torgersen, 1986; David et al., 1995), and alcohol dependence (Lewis and Bucholz, 1991; Isohanni et al., 1994; Kendler et al., 1996). Attachment theory proposed by Bowlby (1980) has postulated that loss experiences have both immediate and long-term consequences and serve as risk factors for adult psychopathology. The onset of depression is earlier for those who experience childhood adversities, suggesting recurrent psychopathology as a potential pathway for the associations (Widom et al., 2007). However, one study reported that childhood adversity was associated with onset but not with persistence of psychopathology (Kessler et al., 1997), while the other reported that the associations between childhood adversities and psychopathology did not greatly attenuate across the lifecourse from adolescence to mid-life (Clark et al., 2010).
Most early research have referred to parental loss without differentiating between parental death and separation. As Tennant emphasized (1988), parental death and separation have different implications. He suggested that parental loss itself is not the critical factor but the consequence of parental loss such as inadequate parental care and family instability is more important as a risk factor for offspring psychopathology. In accordance with this view, several studies have indicated that parental separation, either from divorce or other factors, was strongly associated with increased risk of major depression (MD), while such association was less clear for parental death (Hällström, 1987; Kendler et al., 1992; Agid et al., 1999). Also, since most studies have focused on depression and related conditions, little is known about the relationship between parental loss and other specific types of psychopathology (Canetti et al., 2000; Jacobs and Bovasso, 2009).
Several studies suggest that gender may modify the relationship between parental loss and offspring psychopathology (Tieman et al., 2005; Lizardi et al., 2009). Maternal loss tends to be more strongly associated with offspring psychiatric disorders than paternal loss (Brown et al., 1977; Kunugi et al., 1995). Lloyd (1980) suggested that early permanent separation from the same-sex parent may have more detrimental impacts. Recent research indicated that patients who had experienced the death of or separation from the same-sex parent in childhood reported more severe depressive symptoms (Takeuchi et al., 2002). One of the reasons why maternal separation has been observed to be detrimental more often than paternal separation might be because most previous studies have often been limited to female samples (Hällström; 1987; Kendler et al., 1992; Kendler et al., 1996). On the contrary, Donald et al. (2006) propose that parental loss may be particularly troublesome for males because it is typically the father who is absent. Therefore, more studies are needed to examine the effects of parental loss on psychopathology in male offspring.
The aim of the present study is to examine the impact of parental loss during childhood on risk for adult psychopathology using a large population-based sample of male twins. We tried to answer the following four questions: (1) Which type of parental loss (i.e., death or separation) has more significant effects on risk for adult psychopathology? (2) Does parental loss have any diagnostic specificity as a risk factor? (3) Is maternal loss more strongly associated with psychopathology than paternal loss in male offspring? (4) What is the relative strength of contribution of parental death and separation to adult psychopathology?
2. Methods
2.1. Subjects
We used twin data collected in first (1993-1996) and second (1994-1998) wave interviews with Caucasian adult male twins born between 1940 and 1974 from the population-based Virginia Adult Twin Study of Psychiatric and Substance Use Disorders (VATSPSUD) (Kendler & Prescott, 2006). Of 9417 eligible individuals for the first wave, interviews were completed, typically by telephone, with 6814 (72.4%). At least 1 year later, the twins were recontacted to schedule a second wave interview. This interview was completed, mostly face-to-face, with 5629 (82.6%) of eligible twins. The assessment of parental loss mentioned below was conducted only at the second wave interview. The present study was based on data from the second wave interview of 2605 adult twins from male-male pairs (701 monozygotic (MZ) twin pairs, 485 dizygotic (DZ) twin pairs, and 233 twins without a co-twin report). Zygosity was determined by a combination of standard questions, photographs, and DNA analysis (Kendler & Prescott, 2006). At the time of the second wave interview, the subjects were 20-58 years old (mean age = 36.8 years, SD = 9.1). The two members of each twin pair were interviewed by different interviewers who were clinically trained. Each interview was reviewed twice for completeness and consistency. This project was approved by the Office of Research Subjects Protection at Virginia Commonwealth University. Signed informed or verbal consent was, respectively, obtained prior to face-to-face and telephone interviews.
2.2. Early parental loss
Childhood parental loss was defined as a disruption of the parent-child relationship prior to age 17. For these analyses, we examined two causes of parental loss: death and all other causes (for simplicity, we refer to the latter as ‘separation’). Of these separations, 79% were due to parental divorce while the remainder was due to prolonged parental absence (> 6 months) without divorce.
2.3. Definitions of psychiatric and substance use disorders
The diagnoses considered in this study included MD, generalized anxiety disorder (GAD), phobia, panic disorder, alcohol dependence, and drug abuse and dependence. These disorders were diagnosed by personal interview using an adaptation of the Structured Clinical Interview for DSM-IV Disorders (SCID) (First et al., 1997) and DSM-IV criteria (American Psychiatric Association, 1994) with three exceptions (phobia, panic disorder, and GAD). Phobia was diagnosed using an adaptation of DSM-III-R criteria (American Psychiatric Association, 1987), which required the presence of one or more of 22 fears that the respondent recognized as unreasonable and that, in the judgment of the interviewer, objectively interfered with the respondent's life. Since a relatively low prevalence of GAD and panic disorder had been problematic in previous analyses (Hettema et al., 2001; Kendler et al., 2001), we adopted broader definitions of these conditions using modified DSM-III-R diagnostic criteria. For panic disorder, a history of panic attacks that met at least 2 symptomatic criteria was required (2.2% for broader definition and 1.0% meeting criteria for the full diagnosis). GAD was diagnosed when the minimum duration of illness was 1-month rather than 6-month (18.2% for broader definition and 8.4% meeting criteria for the full diagnosis). We have shown that these approaches reflect the same continuum of liability as the fully syndromal disorders (Hettema et al., 2001; Kendler et al., 2001). Our estimates of lifetime prevalence for psychopathology were generally greater than those reported in previous studies (Kessler et al., 2005), which was because we utilized methods to encourage ‘effortful responding’ with a semi-structured interview and assessed last-year history and a lifetime history of disorders before the last year in two separate sections, combining these to estimate lifetime prevalence.
2.4. Data analyses
Logistic regression analysis
We examined the relationship between parental loss and risk for lifetime psychiatric and substance use disorders using logistic regression analysis. Odds ratio (OR) of adult psychopathology was calculated by entering parental loss (any loss, death and separation) as an independent predictor. We included the subject's age at interview as a covariate in the model because it significantly predicted premature parental loss. To correct for the non-independence of data from a twin pair, the generalized estimating equation (GEE) implemented in PROC GENMOD (SAS Institute Inc., Cary, NC, USA) was used. We first examined the effect of any loss (including both death and separation) on adult psychopathology and then the effect of any death and any separation. Next, we examined the effect of parental separation from mother and father separately. We did not conduct the same analyses of parental death because it was marginally significantly associated with only two disorders (phobia and alcohol dependence). Earlier parental loss may be critical for onset and persistence of psychopathology (Clark et al., 2010). Therefore, we also examined whether age at loss and duration of the effect (age at interview minus age at loss) had impacts on risk for adult psychopathology, limiting the analyses to those twin families who reported a loss. When there were differences in the reported age of the twins at the time of loss, the mean of the reports of the two twins was used. The analyses conducted here were not corrected for multiple comparisons because they were too conservative for common psychiatric disorders that are often comorbid with each other. The OR was obtained by exponentializing the logistic regression coefficient. P-values less than 0.05 are set as significant and are reported two-tailed.
Structural Equation Modeling (SEM)
SEM was conducted using the program Mx (Neale et al., 2006). In the classical twin model, the goal is to quantify the total phenotypic variance in risk liability into that accounted for by additive genetic (A), common environmental (C), and individual environmental (E) factors. In this model, it is assumed that MZ twins share 100% of their genes and DZ twins share, on average, 50% of their segregating genes. It is the covariance patterns of reared-together MZ and DZ twin pairs that are used to estimate A, C, and E. The model used in this report differs from the traditional twin model in that, in addition to the standard latent common environment component, the model also include a specified common environment: childhood parental loss. Age at interview was also included as a covariate. The full model used in the present study is illustrated in Fig 1.This model included age at interview, parental death, and parental separation in addition to latent ACE factors. It is typical to prune the full model down to the “best” model with fewer parameters using Akaike's Information Criterion (AIC) (Akaike, 1987) in which a more negative AIC value indicates better fit. The model could be divided into two parts; a standard twin model (ACE model depicted in the upper half of Figure 1) and a “loss model” (model including the measured environmental variables of loss depicted in the lower half of Figure 1). First, the best-fitting twin model was determined with all of the variables. After the ACE full model being fit to the data, a series of reduced models was tested. The AE model tested the hypothesis of no effects of shared environment, the CE model tested no additive genetic effects, and the E-only model tested no effects of either shared environment or genetic factors. Next, the best model was determined, eliminating the effects of parental death or separation.
Figure 1.
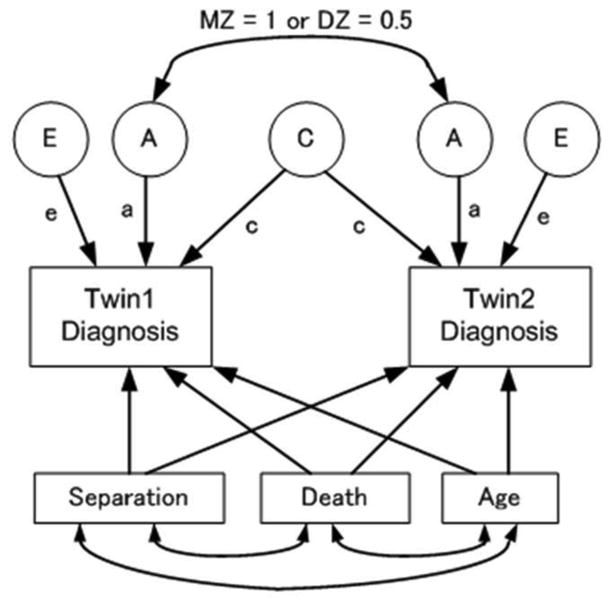
The twin fitting model, incorporating parental loss as a specified common environment. Observed variables are placed in boxes and latent variables are placed in circles. Standardized regressions are depicted as one-headed arrows and correlations are depicted as two-headed arrows. MZ, monozygotic; DZ, dizygotic.
3. Results
Of 2605 twins, 584 (22.4%) reported childhood parental loss. A total of 184 (7.1%) twins reported parental death in childhood, while 400 (15.4%) twins reported parental separation. Of those, 316 (79.0%) twins experienced parental divorce. Paternal loss (death or separation) occurred about three times as frequently as maternal loss. The reports of parental loss (both death and separation) during childhood and age at loss were perfectly concordant between twins.
Table 1 presents the impact of early parental loss (any loss, death, and separation) on risk for adult psychopathology including age at interview as a covariate. Both any parental loss and separation significantly predicted risk for all disorders except phobia (ORs ranged between 1.45 and 2.03). By contrast, parental death was marginally significantly associated with only risk for phobia and alcohol dependence (both of p < 0.05). We also examined the impact of age at parental loss (any loss, death, and separation) and duration (age at interview minus age at loss) on risk for adult psychopathology, although no association was observed (all of p-values > 0.05). However, as we only examined the relationship between these effects (age at loss and its duration) and lifetime risk for psychiatric disorders, our findings did not mean that earlier parental loss had no effect on onset and persistence of psychopathology.
Table 1. Odds ratio of association between parental loss and risk for male offspring psychopathology.
| Diagnosis | Prevalence (%) |
Any Loss (N = 584) |
Death (N = 184) |
Separation (N = 400) |
Separation | |
|---|---|---|---|---|---|---|
|
| ||||||
| Maternal (N =133) | Paternal (N = 362) | |||||
| MD | (26.2) | 1.77**** (1.39-2.27) | 1.04 (0.72-1.51) | 2.01*** (1.38-2.91) | 1.51 (0.99-2.31) | 1.65*** (1.25-2.18) |
| GAD | (18.2) | 1.45** (1.11-1.89) | 0.86 (0.53-1.37) | 1.45** (1.11-1.89) | 1.56 (0.99-2.44) | 1.31 (0.97-1.78) |
| Phobia | (21.9) | 1.28 (0.98-1.68) | 1.42 (1.00-2.00) | 1.29 (0.98-1.68) | 2.09*** (1.35-3.23) | 0.94 (0.68-1.30) |
| Panic disorder | (2.2) | 2.03* (1.10-3.77) | 0.78 (0.24-2.52) | 2.01* (1.09-3.72) | 1.63 (0.59-4.49) | 1.73 (0.83-3.60) |
| Alcohol dependence | (24.0) | 1.56*** (1.20-2.02) | 1.55* (1.05-2.29) | 1.57*** (1.21-2.03) | 2.34**** (1.54-3.55) | 1.13 (0.83-1.52) |
| Drug abuse | (21.6) | 1.87**** (1.42-2.46) | 1.09 (0.71-1.67) | 1.87**** (1.42-2.46) | 1.41 (0.89-2.24) | 1.77*** (1.30-2.41) |
| Drug dependence | (7.6) | 2.02*** (1.39-2.93) | 1.05 (0.54-2.02) | 2.01*** (1.39-2.92) | 2.03* (1.10-3.72) | 1.63* (1.07-2.48) |
N = 2605, Model includes age at interview as a covariate. MD, major depression; GAD, generalized anxiety disorder. 95% confidence intervals (CI) in parentheses.
p < 0.05
p < 0.01
p < 0.001
p < 0.0001.
As parental separation was significantly associated with almost all disorders, the impacts of separation from mother and father were compared. The impact of separation from mother and father on risk for offspring psychopathology was almost equal except phobia and alcohol dependence. For these two, maternal separation was a stronger predictor than paternal separation which was not significantly associated with the disease risk. Among other disorders, paternal separation was significantly associated with MD and drug abuse/dependence, while maternal separation was associated with drug dependence.
We also conducted SEM to determine the best-fitting twin model including measured environmental variables of parental loss (death and separation) controlling for age at interview (Figure 1). Consistent with Table 1, the twin model with separation and age was the best fit for MD, GAD, panic disorder, and drug abuse/dependence, suggesting that early parental separation rather than parental death had significant effects on risk for these disorders (Table 2). For phobia and alcohol dependence, the best model included all parameters (death, separation, and age at interview), showing that both parental death and separation had significant impacts on risk for psychopathology (Table 2). When AIC values were compared between the full model (the ACE model with all the parameters) and the best-fitting model, no significant difference was observed for any disorders (p > 0.05, Table 2). Therefore, the parameter estimates and associated 95% confidence intervals (CI) from the full model with all the parameters are presented (Table 3). Parental loss (death and separation) accounted for about 10% of the total variance of each disorder. In most cases, the variance due to parental separation was larger (range from 2 to 11%) than that due to parental death (range from 0 to 5%), although the differences were not statistically significant. The estimates of the variance due to separation significantly deviated from zero for all disorders except phobia. The impacts of the same environmental adversity have been reported to be different across different disorder categories (Hicks et al., 2009a; Hicks et al., 2009b), we also examined whether the effect of parental loss was different between internalizing (MD, GAD, phobia, and panic disorder) and externalizing (alcohol dependence and drug abuse/dependence) disorders. Similar results were found between two disorder groups that parental separation had significant and moderate effects (8% for internalizing disorders and 9% for externalizing disorders), while genetic factors had higher effects on externalizing disorders than on internalizing disorders (54% for externalizing disorders and 14% for internalizing disorders).
Table 2. AIC values of each model with parameters.
| Diagnosis | N | ACE model* | Best fitting model with parameters | X2 | df | p** | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| ACE | AE | CE | model | All (D,S, Age) | D, Age | S, Age | |||||
| INT | 2594 | -1658.6 | -1660.4 | -1659.5 | AE | -1660.4 | -1644.1 | -1658.0 | 1.8 | 1 | 0.18 |
| MD | 2595 | -2235.6 | -2237.6 | -2236.3 | AE | -2237.6 | -2219.6 | -2239.5 | 3.9 | 2 | 0.14 |
| GAD | 2598 | -2713.5 | -2715.3 | -2715.4 | CE | -2715.4 | -2710.4 | -2716.7 | 3.2 | 2 | 0.20 |
| Pho | 2595 | -2455.5 | -2457.5 | -2455.9 | AE | -2457.5 | -2456.2 | -2455.9 | 2.0 | 1 | 0.16 |
| panic | 2594 | -4637.0 | -4639.0 | -4637.9 | AE | -4639.0 | -4636.5 | -4640.9 | 3.9 | 2 | 0.14 |
| EXT | 2594 | -1994.0 | -1996.0 | -1979.9 | AE | -1996.0 | -1979.4 | -1990.5 | 2.0 | 1 | 0.16 |
| ALC | 2594 | -2388.3 | -2390.3 | -2382.9 | AE | -2390.3 | -2382.1 | -2388.1 | 2.0 | 1 | 0.16 |
| Drug abuse | 2606 | -2698.0 | -2700.0 | -2678.3 | AE | -2700.0 | -2684.5 | -2701.9 | 3.9 | 2 | 0.14 |
| Drug dep | 2606 | -3860.1 | -3862.7 | -3855.4 | AE | -3862.7 | -3852.5 | -3864.6 | 4.5 | 2 | 0.11 |
AIC, Akaike Information Criterion; A, additive genetic effects; C, shared environmental effects.
E, non-shared environmental effects; S, Parental separation; D, parental death; Age, age at interview; df, degrees of freedom.
All models included parameters of S, D and Age.
INT, internalizing disorders including MD, GAD, phobia, and panic disorder.
EXT, externalizing disorders including alcohhol dependence and drug abuse/dependence.
Best fitting model was shown in bold
no significance was observed between the model and ACE full model
Table 3. Proportion of variance in liability to male offspring psychopathology.
| Diagnosis | Variance (%) (95% CI) | ||||
|---|---|---|---|---|---|
|
| |||||
| A | C | E | D | S | |
| INT | 14 (0-32) | 8 (0-28) | 67 (58-77) | 2 (0-12) | 8 (2-18) |
| MD | 24 (0-40) | 7 (0-32) | 59 (49-70) | 0 (0-5) | 11 (4-22) |
| GAD | 9 (0-31) | 8 (0-26) | 78 (64-90) | 1 (0-11) | 4 (1-13) |
| Phobia | 20 (0-32) | 0 (0-24) | 73 (62-86) | 4 (0-16) | 2 (0-9) |
| Panic disorder | 38 (0-66) | 0 (0-52) | 52 (25-88) | 1 (0-36) | 9 (1-31) |
| EXT | 54 (27-62) | 2 (0-25) | 29 (23-37) | 6 (0-20) | 9 (2-20) |
| Alcohol dependence | 45 (13-57) | 3 (0-30) | 41 (32-51) | 5 (0-19) | 6 (1-15) |
| Drug abuse | 66 (38-74) | 2 (0-27) | 21 (15-28) | 0 (0-7) | 11 (3-24) |
| Drug dependence | 62 (17-71) | 0 (0-38) | 27 (17-41) | 0 (0-10) | 11 (2-27) |
A, additive genetic effects; C, shared environmental effects; E, non-shared environmental effects.
D, parental death; S, parental separation.
CI, confidence intervals; MD, major epression; GAD, generalized anxiety disorder.
INT, internalizing disorders including MD, GAD, phobia, and panic disorder.
EXT, externalizing disorders including alcohhol dependence and drug abuse/dependence.
The values for age are not shown because it accounted for less than 0.1% of the variance.
4. Discussion
We examined the association between parental loss and risk for seven common psychiatric and substance use disorders in a population-based sample of male twins. We also estimated the degree to which specific environmental risk factors (parental death and separation) contribute to individual differences in adult psychopathology. We will review our findings in turn.
We first examined the association between parental loss prior to age 17 and risk for seven common psychiatric and substance use disorders in male offspring. Parental loss due to any loss or separation was associated with all disorders except phobia, whereas parental death was associated with only phobia and alcohol dependence. The associations were not specific to age at parental loss and its duration. Also, the effect of loss due to separation was more striking than loss due to death, which is consistent with the findings in previous studies (Kendler et al., 1992; Canetti et al., 2000; Kendler et al., 2002). We note that there is generally greater power to detect effects of separation than death due to the greater frequency with which the former occurred. However, caution would be needed to interpret the results of psychopathology such as phobia because its onset (typically in childhood) may be earlier than the occurrence of parental loss. Furthermore, it might not be loss itself but other mediating factors related to the family environment prior to and following the loss that predisposes to psychopathology (Tennant, 1988; Agid et al., 1999; Jordan, 2001). It has been shown that inadequate parenting and the quality of the relationship with the parent, irrespective of early loss, may be associated with the development of psychopathology (Breier et al., 1988; Tennant, 1988; Hovens et al., 2010; Otowa et al., 2013).
In accordance with previous studies (Agid et al., 1999; Kendler et al., 2002; Stikkelbroek et al., 2012), we found no or weak associations between parental death and psychiatric disorders. Most studies that detected the association between parental death and offspring psychopathology assessed relatively short-term outcomes after parental death (Brent et al., 2009; Kuramoto 2009). Our previous study demonstrated that the risk for depressive onsets due to parental death returned to baseline within a limited time whereas a much longer time period was required for the risk due to parental separation to return to baseline (Kendler et al., 2002). Furthermore, a large number of animal and human studies suggest long lasting effects of chronic stress on the brain structure involved in psychiatric disorders (Lupien et al., 2009). In addition, these studies suggest that there may be early windows of vulnerability in certain area of developing brain that is most susceptible to adversity. These reports support the reasons why we could not detect strong associations between parental death and lifetime psychopathology, because the effect of parental death persists relatively a short time and has weaker impact on adult psychopathology than that of parental separation.
When the impact of parental separation from mother and father was examined separately, separation from mother and father was associated with comparable increase in risk for most disorders except phobia and alcohol dependence. The results are consistent with the findings showing that MD was equally associated with maternal and paternal separation in females (Kendler et al., 1992) but are inconsistent with some other studies suggesting that maternal separation was more important than paternal separation in the pathogenesis of illness (Kunugi et al., 1995; Agerbo et al., 2002). We noted that the analyses of paternal separation tended to be more powerful since the prevalence of paternal loss was observed to be greater than that of maternal separation. For phobia and alcohol dependence, however, the impact of maternal separation on risk for these disorders was significantly larger than that of paternal separation. These results are incompatible with prior studies suggesting that loss of the same-sex parent (i.e., father in this study) may have a more detrimental impact (Lloyd, 1980; Takeuchi et al, 2002). In the present study, a stronger risk for phobia and alcohol dependence associated with maternal separation than paternal separation may be attributed to the separation from the primary caregiver, who usually is the mother (Harris et al., 1986). For example, phobias or other anxiety disorders may be related to fear of abandonment from the parent on whom children cannot rely for their future care (Schoenfelder et al., 2011). In the present study, we could not conclude that paternal separation has stronger effects on psychopathology in male offspring than maternal separation.
Using SEM, we examined the extent to which this specified environmental factor contributes to risk of adult psychopathology. We found moderate impact of parental loss on risk of adult psychopathology. As also shown by logistic regression analyses, SEM suggested that parental separation had higher impact on disease risk than parental death (2-11% vs. 0-5% of the total variance). For all disorders except phobia, our variance estimates for separation significantly deviated from zero, suggesting that parental separation was a significant predictor of a wide variety of adult psychopathology. We also examined whether the impacts of parental loss were different between internalizing and externalizing disorders. Our results showed similar impacts of parental separation and death across the two disorder categories, while genetic factors had stronger effects on externalizing disorders than internalizing disorders. Our findings are consistent with the results reported in previous studies that genetic factors were important in the etiology of externalizing disorders while individual environmental factors were important in the etiology of internalizing disorders (Hicks et al., 2009a; Hicks et al., 2009b). The amount of variance in liability for each disorder was larger than that reported in previous studies in which parental loss accounted for less than 5% of variance (Kendler et al., 1992; Battaglia et al., 2009). The differences in the amount of variance in liability for disorders may be attributable to the differences in population (all subjects were males in the present study), sample size, and measurements for diagnosis. Also, considering the evidence that childhood adversities are highly comorbid, it is likely that other adversities and indirect effects of parental loss (such as child abuse and family pathology) may inflate the associations.
In the present study, parental loss was conceptualized as a specified form of family environment which was perfectly concordant between twins. However, as reviewed by Turkheimer et al. (2005), twin studies including a family variable could provide misleading estimates of environmental effects that may be biased by genetic factors. Because parental loss could be mediated by genetic and other environmental confounding factors (e.g., parental psychopathology and socioeconomic status), it would be difficult to determine whether the effect of parental loss was genetic or environmental. In future research, twin model including gene x environmental interaction (Purcell, 2002) and family based studies (such as the twin-family design incorporating measures of parental psychopathology and the children of twins (CoT) design with genetic and environmental variation in family-level risk factors (D'Onofrio et al, 2013)) would be needed to examine actual environmental causation.
4.1. Limitations
The results in the present study should be interpreted in the context of several limitations. First, this study included only Caucasian male twins. It cannot be assumed that parental loss is associated with risk for psychiatric disorders in the same way in families with non-twin offspring or in other races and cultures. Second, we largely relied on retrospective reports of both parental loss and onset of disorders. Patients with current psychiatric disorders might have exaggerated the relationship between parental loss and subsequent onset of illness. In this study, however, this is less likely because, although twin and his co-twin were interviewed individually, reports of parental loss during childhood were perfectly concordant between twins. Third, in the present study, we did not control for other adverse childhood experiences such as parental conflict and parent-child relationship due to our detailed focus on effects of loss across psychopathology. More complex models have been tested with these data for MD only (Kendler et al., 2006). Since childhood adversities are highly comorbid (Benjet et al., 2009) and correlated with each other (Hicks et al., 2007a), parental loss could be a representative of childhood adversities. However, multiple adversities have a cumulative impact on later psychopathology (Melchior et al., 2007), a broad range of such variables should be included in the future analysis. Fourth, in the cross-sectional design, we cannot draw any conclusions about the causal role of parental loss in the onset and development of psychopathology in later life. Longitudinal studies are needed to understand the biological and psychological mechanisms by which types of parental loss (death, divorce, and other types of separation) may contribute to the development and course of psychopathology.
4.2. Conclusion
Our findings suggest that parental separation has stronger and wider effects on offspring psychopathology than parental death in males as observed in females. Further research is warranted in larger prospective cohorts to confirm our findings and elucidate the mechanisms by which parental loss impacts risk.
Highlights.
Parental separation has stronger and wider effects on mental illness than death.
Maternal and paternal separation were almost equally associated with psychopathology.
Parental loss accounted for about 10% of the variance of adult psychopathology,
Acknowledgments
This work was supported by NIH grants MH-40828, AA-09095, AA-00236, DA-11287, and MH/AA/DA-49492. Carol A. Prescott provided critical help in the collection of the Virginia Adult Twin Study of Psychiatric and Substance Use Disorders (VATSPSUD) sample. We acknowledge the contribution of the Virginia Twin Registry, now part of Mid-Atlantic Twin Registry (MATR), for the ascertainment of subjects for this study. MATR is supported by NIH grant UL1TR000058. Takeshi Otowa was supported by research fellowship from the Japan Society for the Promotion of Science (no. 21-8373). We also would like to thank the twins for their participation in this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agerbo E, Nordentoft M, Mortensen PB. Familial, psychiatric, and socioeconomic risk factors for suicide in young people: nested case-control study. British Medical Journal. 2002;325:74. doi: 10.1136/bmj.325.7355.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agid O, Shapira B, Zislin J, Ritsner M, Hanin B, Murad H, Troudart T, Bloch M, Heresco-Levy U, Lerer B. Environment and vulnerability to major psychiatric illness: a case control study of early parental loss in major depression, bipolar disorder and schizophrenia. Molecular Psychiatry. 1999;4:163–172. doi: 10.1038/sj.mp.4000473. [DOI] [PubMed] [Google Scholar]
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. American Psychiatric Association; Washington DC: 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd. American Psychiatric Association; Washington DC: 1987. Revised. [Google Scholar]
- Battaglia M, Pesenti-Gritti P, Medland SE, Ogliari A, Tambs K, Spatola CA. A genetically informed study of the association between childhood separation anxiety, sensitivity to CO2, panic disorder, and the effect of childhood parental loss. Archives of General Psychiatry. 2009;66:64–71. doi: 10.1001/archgenpsychiatry.2008.513. [DOI] [PubMed] [Google Scholar]
- Benjet C, Borges G, Medina-Mora ME. Chronic childhood adversity and onset of psychopathology during three life stages: childhood, adolescence and adulthood. Journal of Psychiatric Research. 2010;44:732–740. doi: 10.1016/j.jpsychires.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Sadness and Depression. New York: Basic Books; 1980. Attachment and Loss. 3: Loss. [Google Scholar]
- Breier A, Kelsoe JR, Jr, Kirwin PD, Beller SA, Wolkowitz OM, Pickar D. Early parental loss and development of adult psychopathology. Archives of General Psychiatry. 1988;45:987–993. doi: 10.1001/archpsyc.1988.01800350021003. [DOI] [PubMed] [Google Scholar]
- Brent D, Melhem N, Donohoe MB, Walker M. The incidence and course of depression in bereaved youth 21 months after the loss of a parent to suicide, accident, or sudden natural death. American Journal of Psychiatry. 2009;166:786–794. doi: 10.1176/appi.ajp.2009.08081244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GW, Harris T, Copeland JR. Depression and loss. British Journal of Psychiatry. 1977;130:1–18. doi: 10.1192/bjp.130.1.1. [DOI] [PubMed] [Google Scholar]
- Canetti L, Bachar E, Bonne O, Agid O, Lerer B, Kaplan De-Nour A, Shalev AY. The impact of parental death versus separation from parents on the mental health of Israeli adolescents. Comprehensive Psychiatry. 2000;41:360–368. doi: 10.1053/comp.2000.9002. [DOI] [PubMed] [Google Scholar]
- Clark C, Caldwell T, Power C, Stansfeld SA. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Annals of Epidemiology. 2010;20:385–394. doi: 10.1016/j.annepidem.2010.02.008. [DOI] [PubMed] [Google Scholar]
- David D, Giron A, Mellman TA. Panic-phobic patients and developmental trauma. Journal of Clinical Psychiatry. 1995;56:113–117. [PubMed] [Google Scholar]
- Donald M, Dower J, Correa-Velez I, Jones M. Risk and protective factors for medically serious suicide attempts: a comparison of hospital-based with population-based samples of young adults. Australian and New Zealand Journal of Psychiatry. 2006;40:87–96. doi: 10.1080/j.1440-1614.2006.01747.x. [DOI] [PubMed] [Google Scholar]
- D'Onofrio BM, Lahey BB, Turkheimer E, Lichtenstein P. Critical need for family-based, quasi-experimental designs in integrating genetic and social science research. American Journal of Public Health. 2013;103:S46–55. doi: 10.2105/AJPH.2013.301252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faravelli C, Webb T, Ambonetti A, Fonnesu F, Sessarego A. Prevalence of traumatic early life events in 31 agoraphobic patients with panic attacks. American Journal of Psychiatry. 1985;142:1493–1494. doi: 10.1176/ajp.142.12.1493. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders -Clinician Version (SCID-CV) American Psychiatric Press; Washington DC: 1997. [Google Scholar]
- Freud S. Mourning and melancholia In: Standard Edition of the Complete Psychological Works of Sigmund Freud. Hogarth; London: 1917. p. 237. [Google Scholar]
- Jacobs JR, Bovasso GB. Re-examining the long-term effects of experiencing parental death in childhood on adult psychopathology. The Journal of Nervous and Mental Disease. 2009;197:24–27. doi: 10.1097/NMD.0b013e3181927723. [DOI] [PubMed] [Google Scholar]
- Hällström T. The relationships of childhood socio-demographic factors and early parental loss to major depression in adult life. Acta Psychiatrica Scandinavica. 1987;75:212–216. doi: 10.1111/j.1600-0447.1987.tb02777.x. [DOI] [PubMed] [Google Scholar]
- Harris T, Brown GW, Bifulco A. Loss of parent in childhood and adult psychiatric disorder: the role of lack of adequate parental care. Psychological Medicine. 1986;16:641–659. doi: 10.1017/s0033291700010394. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Prescott CA, Kendler KS. A population-based twin study of generalized anxiety disorder in men and women. Journal of Nervous and Mental Disease. 2001;189:413–420. doi: 10.1097/00005053-200107000-00001. [DOI] [PubMed] [Google Scholar]
- Hicks BM, DiRago AC, Iacono WG, McGue M. Gene-environment interplay in internalizing disorders: consistent findings across six environmental risk factors. Journal of Child Psychology and Psychiatry. 2009a;50:1309–1317. doi: 10.1111/j.1469-7610.2009.02100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks BM, South SC, Dirago AC, Iacono WG, McGue M. Environmental adversity and increasing genetic risk for externalizing disorders. Archives of General Psychiatry. 2009b;66:640–648. doi: 10.1001/archgenpsychiatry.2008.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill J, Pickles A, Burnside E, Byatt M, Rollinson L, Davis R, Harvey K. Child sexual abuse, poor parental care and adult depression: evidence for different mechanisms. British Journal of Psychiatry. 2001;179:104–109. doi: 10.1192/bjp.179.2.104. [DOI] [PubMed] [Google Scholar]
- Hovens JG, Wiersma JE, Giltay EJ, van Oppen P, Spinhoven P, Penninx BW, Zitman FG. Childhood life events and childhood trauma in adult patients with depressive, anxiety and comorbid disorders vs. controls. Acta Psychiatrica Scandinavica. 2010;122:66–74. doi: 10.1111/j.1600-0447.2009.01491.x. [DOI] [PubMed] [Google Scholar]
- Isohanni M, Oja H, Moilanen I, Koiranen M. Teenage alcohol drinking and non-standard family background. Social Science & Medicine. 1994;38:1565–1574. doi: 10.1016/0277-9536(94)90118-x. [DOI] [PubMed] [Google Scholar]
- Jordan JR. Is suicide bereavement different? A reassessment of the literature. Suicide and Life-Threatening Behavior. 2001;31:91–102. doi: 10.1521/suli.31.1.91.21310. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Childhood parental loss and adult psychopathology in women. A twin study perspective. Archives of General Psychiatry. 1992;49:109–116. doi: 10.1001/archpsyc.1992.01820020029004. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Prescott CA, Kessler RC, Heath AC, Corey LA, Eaves LJ. Childhood parental loss and alcoholism in women: a causal analysis using a twin-family design. Psychological Medicine. 1996;26:79–95. doi: 10.1017/s0033291700033730. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Panic syndromes in a population-based sample of male and female twins. Psychological Medicine. 2001;31:989–1000. doi: 10.1017/s0033291701004226. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Sheth K, Gardner CO, Prescott CA. Childhood parental loss and risk for first-onset of major depression and alcohol dependence: the time-decay of risk and sex differences. Psychological Medicine. 2002;32:1187–1194. doi: 10.1017/s0033291702006219. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA. Genes, environment, and psychopathology: Understanding the causes of psychiatric and substance use disorders. 1st. Guilford Press; New York: 2006. [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. American Journal of Psychiatry. 2006;163:115–124. doi: 10.1176/appi.ajp.163.1.115. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kunugi H, Sugawara N, Aoki H, Nanko S, Hirose T, Kazamatsuri H. Early parental loss and depressive disorder in Japan. European Archives of Psychiatry and Clinical Neuroscience. 1995;245:109–113. doi: 10.1007/BF02190737. [DOI] [PubMed] [Google Scholar]
- Kuramoto JS, Brent DA, Wilcox HC. The impact of parental suicide on child and adolescent offspring. Suicide and Life-Threatening Behavior. 2009;39:137–151. doi: 10.1521/suli.2009.39.2.137. [DOI] [PubMed] [Google Scholar]
- Lewis CE, Bucholz KK. Alcoholism, antisocial behavior and family history. British journal of addiction. 1991;86:177–194. doi: 10.1111/j.1360-0443.1991.tb01768.x. [DOI] [PubMed] [Google Scholar]
- Lizardi D, Thompson RG, Keyes K, Hasin D. Parental divorce, parental depression, and gender differences in adult offspring suicide attempt. The Journal of Nervous and Mental Disease. 2009;197:899–904. doi: 10.1097/NMD.0b013e3181c299ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd C. Life events and depressive disorder reviewed. I. Events as predisposing factors. Archives of General Psychiatry. 1980;37:529–535. doi: 10.1001/archpsyc.1980.01780180043004. [DOI] [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Review Neuroscience. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Melchior M, Moffitt TE, Milne BJ, Poulton R, Caspi A. Why do children from socioeconomically disadvantaged families suffer from poor health when they reach adulthood? A life-course study. American Journal of Epidemiology. 2007;166:966–974. doi: 10.1093/aje/kwm155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neale MC, Boker SM, Xie G, Maes HH. Mx: Statistical Modeling. 7th. Medical College of Virginia; Richmond: 2006. [Google Scholar]
- Otowa T, Gardner CO, Kendler KS, Hettema JM. Parenting and risk for mood, anxiety and substance use disorders: a study in population-based male twins. Social Psychiatry and Psychiatric Epidemiology. 2013 doi: 10.1007/s00127-013-0656-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell S. Variance components models for gene-environment interaction in twin analysis. Twin Research. 2002;5:554–571. doi: 10.1375/136905202762342026. [DOI] [PubMed] [Google Scholar]
- Raskin M, Peeke HV, Dickman W, Pinsker H. Panic and generalized anxiety disorders. Developmental antecedents and precipitants. Archives of General Psychiatry. 1982;39:687–689. doi: 10.1001/archpsyc.1982.04290060047009. [DOI] [PubMed] [Google Scholar]
- Roy A. Early parental separation and adult depression. Archives of General Psychiatry. 1985;42:987–991. doi: 10.1001/archpsyc.1985.01790330067008. [DOI] [PubMed] [Google Scholar]
- Schoenfelder EN, Sandler IN, Wolchik S, MacKinnon D. Quality of social relationships and the development of depression in parentally-bereaved youth. Journal of Youth and Adolescence. 2011;40:85–96. doi: 10.1007/s10964-009-9503-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stikkelbroek Y, Prinzie P, de Graaf R, Ten Have M, Cuijpers P. Parental death during childhood and psychopathology in adulthood. Psychiatry Research. 2012;198:516–520. doi: 10.1016/j.psychres.2011.10.024. [DOI] [PubMed] [Google Scholar]
- Takeuchi H, Hiroe T, Kanai T, Morinobu S, Kitamura T, Takahashi K, Furukawa TA. Childhood parental separation experiences and depressive symptomatology in acute major depression. Psychiatry and Clinical Neurosciences. 2003;57:215–219. doi: 10.1046/j.1440-1819.2003.01103.x. [DOI] [PubMed] [Google Scholar]
- Tennant C, Bebbington P, Hurry J. Social experiences in childhood and adult psychiatric morbidity: a multiple regression analysis. Psychological Medicine. 1982;12:321–327. doi: 10.1017/s0033291700046651. [DOI] [PubMed] [Google Scholar]
- Tennant C. Parental loss in childhood. Its effect in adult life. Archives of General Psychiatry. 1988;45:1045–1050. doi: 10.1001/archpsyc.1988.01800350079012. [DOI] [PubMed] [Google Scholar]
- Tieman W, van der Ende J, Verhulst FC. Psychiatric disorders in young adult intercountry adoptees: an epidemiological study. American Journal of Psychiatry. 2005;162:592–598. doi: 10.1176/appi.ajp.162.3.592. [DOI] [PubMed] [Google Scholar]
- Torgersen S. Childhood and family characteristics in panic and generalized anxiety disorders. American Journal of Psychiatry. 1986;143:630–632. doi: 10.1176/ajp.143.5.630. [DOI] [PubMed] [Google Scholar]
- Turkheimer E, D'Onofrio BM, Maes HH, Eaves LJ. Analysis and interpretation of twin studies including measures of the shared environment. Child Development. 2005;76:1217–1233. doi: 10.1111/j.1467-8624.2005.00846.x. [DOI] [PubMed] [Google Scholar]
- Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]


