Abstract
Background:
This study aimed to evaluate the accuracy of two imaging methods in detecting the apical pathology in endodontically treated teeth.
Material and Methods:
A clinical examination from a sample of 156 teeth of patients treated by students of masters in endodontics at the Care Center of the Faculty of Dentistry at St. Joseph University, Beirut was done after 5 years of follow-up. Periradicular digital radiographs and a cone-beam computed tomography (CBCT)scans were taken and analyzed statistically using both the Exact Fisher tests and McNemar tests.
Results:
The prevalence of lesions was significantly higher with CBCT (34.8%), whereas for digital radiography (13.8%). The CBCT was revealed more precise to identify periapical lesions. As for the clinical success, the rate was 82.5%.
Conclusion:
Within the limitations of the present study, CBCT was more reliable in detecting periapical lesions compared with digital periapical radiographs.
Keywords: Cone-beam computed tomography, endodontic treatment, periapical radiograph, periapical periodontitis
Introduction
The success rates of endodontic treatment are an important part of evidence-based practice; periapical status outcome of an endodontically treated tooth determines whether the ultimate goal of endodontics has been reached or not. Therefore, the presence of the newly formed or persistent apical periodontitis lesion in postoperative radiographs with or without clinical symptoms must be regarded as treatment failure.1
In most of the randomized clinical trials and systematic reviews, methods used for success evaluation are based on clinical examination and periapical radiographs, consisting in general on intra-oral radiography.2,3 When postoperative lesions exist, they are often asymptomatic and cannot be detected on a periapical radiograph. Studies have shown that lesions confined within the cancellous bone cannot be detected, and the bone resorption should reach nearly 30-50% of bone mineral loss to be visible radiographically.4 Furthermore, radiographic detection of periapical lesions is affected by bone density, X-ray angulations, location and lesion’s shape.5,6 These limitations may lead to an overestimation of the success rate.1,7
Nowadays, cone-beam computed tomography (CBCT)is confirmed as the most effective radiographic tool for diagnostic procedures in endodontics.6 It has been used to improve the limitations of conventional radiography with a higher accuracy in detecting periapical lesions.8-10 In fact, CBCT gives a tridimensional reproduction of the teeth, anatomical noise is largely eliminated, and geometric distortion is minimal.5,11 Clinical studies have demonstrated increased accuracy of CBCT in the evaluation of periradicular healing and endodontic outcome assessment. Fernández et al. showed that CBCT detected a higher number of periradicular lesions in the CBCT (18.7%, n = 39 roots), then in the digital periapical radiograph (7.7%, n = 16 roots).3 Therefore, an increase of 63% in the amount of periapical lesions detection was observed using CBCT. Consequently, more treatments will definitely be considered as unsuccessful in the future when using the CBCT. Authors in several studies have recommended the reevaluating of the endodontic treatment and success with long-term follow-up using CBCT for the evaluation.1
The purpose of this study is to analyze retrospectively the outcome of the endodontic treatment after a follow-up period of 5 years and to compare the accuracy of the digital and conventional radiography in the detection of periapical radiolucencies.
Materials and Methods
This retrospective cohort study evaluates the outcome of 156 root canal treatments performed between 2007 and 2008. The subjects recruited are treated by the first and second-year postgraduate students in Endodontic Department of St. Joseph University, under the supervision of qualified and experienced endodontists.
All patients were contacted by phone and invited to a follow-up with a free cleaning, between September 2013 and January 2014. When the patient could not be directly contacted, a message was left with the person who answered the call. Patient’s non-participation was mostly due to the inability to be contacted by lack of motivation, the telephone number not in service, or because of the patients’ death.
The study’s protocol was approved by the research ethics committee of St. Joseph University. All participants were informed and signed a consent form before radiographic examination.
Clinical and radiographic evaluation at follow-up
Clinical and radiographic evaluation was done 5 years after the nonsurgical endodontic treatment. All teeth were examined for any signs of infection and inflammation using the percussion and probing tests. The presence of provoked or spontaneous pain and sinus tracts were considered as failure criteria.
A Kodak long-cone X-ray unit with the exposure time of 70 kV and 0.4 s was used to take radiographs using digital phosphoric plate of 30 mm × 40 mm. Intraoral radiographs were achieved using the paralleling technique. Images were developed using an automatic device Vista scan with the resolution of 500 dpi.
CBCT images were obtained with NewTomVGi scanner CBCT scanner which was operated at 110 kV, 1-20 mA, 99 µSv of field vision, voxel size 150 µ, 16 bits, XX seconds of exposure time. Images were examined using specific NewTom NNT software on a PC operating on Microsoft Windows XP program.
Two blinded examiners, an endodontist and a radiologist evaluated all the images independently. Findings were noted in Microsoft excel 2010.
A periapical lesion was defined as a radiolucency located in the periapical area of the tooth at the apex with at least twice the width of the periodontal ligament space.12
Treatment outcome was classified into two categories:
“Favorable,” when there are no signs or symptoms associated with a tooth and no periapical rarefaction.
“Failure” when the tooth is associated with a periapical lesion or a radiolucent area of any size. The treatment is also deemed to be a failure if the tooth is symptomatic at recall, regardless of the radiographic appearance.
The date of any retreatment or extraction or any endodontic surgery done to a sampled tooth during these 5 years was recorded. The cause was then evaluated, if it was related to reinfection of the root canal treatment; it was considered as failure if not it was excluded from this study.
Statistical analysis
The Statistical Package for Social Sciences Software (SPSS for Windows, version 18.0, Chicago, IL, USA) is the statistical software was used to perform statistical analysis of the data with a level of significance chosen “P ≤ 0.05.” Fisher Exact tests and McNemar tests were used to compare the sample results obtained by the two independent observers.
Results
Five years after the endodontic treatment was performed, 82.7% of the teeth were asymptomatic, 5.8% of the teeth presented sensitivity to percussion and 11.5% were extracted (Graph 1).
Graph 1.
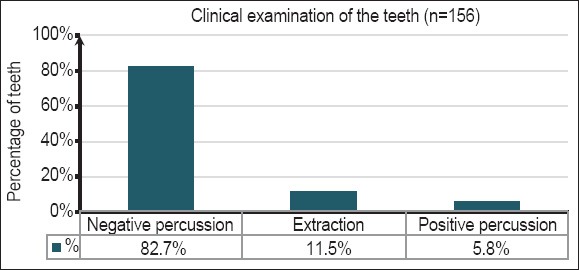
Percentage of clinical examination of the 156 teeth.
The lesions were correctly identified in 13.8% of the cases on digital periapical radiography and 34.8% on CBCT (radiologist). The accuracy of the CBCT is significantly higher than that of the digital radiography (P < 0.001) (Graph 2).
Graph 2.
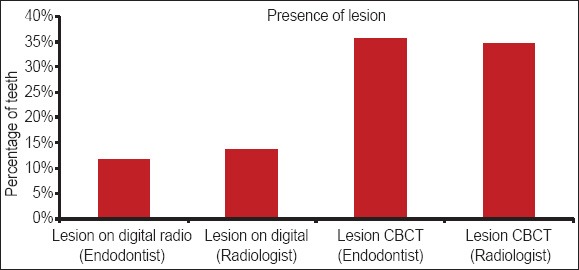
The presence of lesions noted by the radiologist and endodontist on digital radiography and cone-beam computed tomography.
Regarding the visualization of the lesions, both radiologist and endodontist found that the presence of lesions was higher on the CBCT compared with the digital radiograph (P < 0.001) (Graph 2).
There was a significant difference between the presence of the lesion and the location of the tooth (P < 0.0001). In molar teeth, CBCT identified a higher number of lesions (41,7%) than the digital periapical radiograph (25%) (Table 1, Figures 1 and 2).
Table 1.
Correlation between the incidence of the lesions and the tooth type.
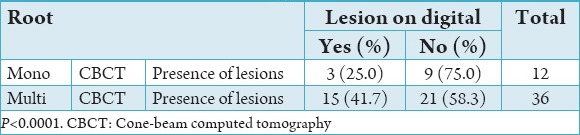
Figure 1.
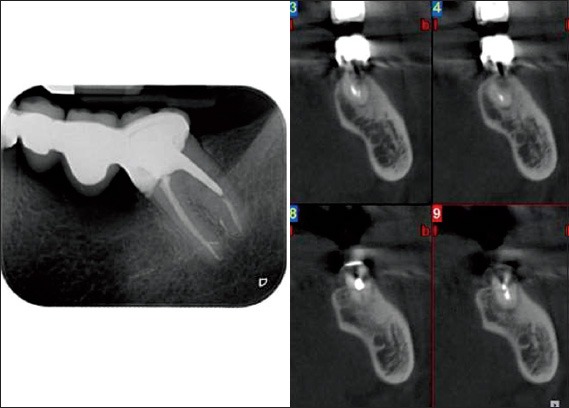
Cone-beam computed tomography image in a sagittal view showing the presence of periapical radiolucency on mandibular molar and digital periapical radiography of the same tooth showing a normal aspect.
Figure 2.
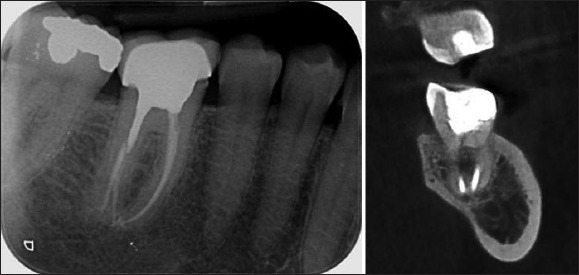
Digital periapical radiography of a mandibular molar showing a normal periapical aspect and cone-beam computed tomography image of the same tooth revealing the presence of periapical radiolucency.
Discussion
The 5-year recall rate was 52%, which is lower than those reported by the high level of evidence-based guidelines studies2 but similar to other retrospective studies.3 The low recall rate was not expected because of the free cleaning offered to enhance the patient’s participation.
Clinical and radiographic evaluation was both used in our study as recommended by other researchers,2,3,13,14 to evaluate the endodontic treatment outcome. The presence of anatomical noise, the two-dimensional image, and geometric distortion are the major drawbacks of periapical radiographs that remain so far the routinely employed method. CBCT provides more significant information than periapical images and eliminates the superimposition of anatomical structures.15 A digital intraoral radiography was used in this study rather than a conventional X-ray film. Thus, the resulting image of digital periapical radiography could be easily enhanced (brightness and contrast)6 to improve the interpretation of the image. Several studies have shown no significance difference between both techniques.16
Despite the limitations of a retrospective study, our data illustrates a follow-up period of 5 years. Several authors17 found that 91-95% of periapical lesions healed completely after 4 years of treatment, suggesting that a period of more than 24 months of follow-up may be required to minimize the number of false negative results regarding the diagnosis of lesions.3 It was recommended in the Toronto studies that the follow-up period should be long enough to observe the complete process of wound healing.2
While there is scientific evidence that in a patient’s perspective, functionality of the teeth indicates the success of the nonsurgical endodontic treatment,18 in our study, endodontic treatment versus tooth extraction was associated with the full functionality of the teeth after 5 years of the treatment, which was independent from radiographic findings. 88.5% of the total number of teeth were present (of which 82.7% were asymptomatic) while 11.5% were extracted.
Considering the importance of the method used to evaluate the outcome of endodontic treatment, the present study was performed to compare the accuracy of the digital radiograph and CBCT scans in detecting of periapical radiolucencies. Results revealed very good agreement between the two observers for both methods. Of 138 teeth, 48 lesions (34.8%)where identified by means of CBCT, and 19 lesions (13.8%)using digital radiograph. Radiographic success is 65,2% with the CBCT (radiologist) and 86,2 % on digital radiograph which is similar to results found other studies of Estrela et al. 2008, Fernández et al. 2013 (87.4% à 97%).3,13 The success rate determined by CBCT was reduced by 10-40% then of that of the digital radiography.5,13,19,20
A similar study, done by Stavropoulos and Wenzel, also verified the accuracy of the same CBCT (NewTom 3G; NewTom Germany, Germany) in comparison with the digital and conventional radiography in mechanically created lesions in pig jaws. The result showed higher precision of CBCT over the digital and conventional radiography.16
The prevalence of apical pathology undetected on periapical radiographs is considerably high. 30-50% of mineral loss is needed to visualize the lesions.5 The limitations of periapical radiographs as a diagnostic tool should not be overlooked, mainly to reduce false-negative results.
On the other hand, results in our study revealed that the limitation of the digital periapical radiography was more evident in identifying periapical lesions on molar teeth. This is in agreement with a study done by Gao et al. in 2010.21 In fact, the presence of the zygomatic process in the region of the maxillary molars and the cortical bone thickness in the mandible can limit periapical radiographs lesions identification. Nevertheless, false negative diagnosis is the main reason why conventional radiographic images should be used with care in detecting apical periodontitis.13
Other studies have shown the superiority of CBCT over conventional radiography in diagnosing other complications such as vertical root fracture,22-24 and root resorption.25-27 The drawbacks of CBCT include high cost and potentially higher dose of radiation, which should be kept as low as possible.28 The new AAE recommendations are that: “CBCT should only be used when the question for which imaging is required cannot be answered adequately by lower dose conventional dental radiography or alternate imaging modalities.”29
Conclusion
Within the limitations of the present study, it can be concluded that CBCT was more reliable in detecting periapical lesions compared with digital periapical radiographs in the long-term evaluation of root canal treatment success. The prevalence of AP was correctly identified in 34.8% of the cases with the CBCT and 13.8% with periapical radiographs, but clinical success was highly detected in all cases. Further studies with higher recall rate should be done to evaluate the factors affecting the outcome of the endodontic treatments and to confirm the results found in this study.
Footnotes
Conflicts of Interest: None
Source of Support: Nil
References
- 1.Wu MK, Shemesh H, Wesselink PR. Limitations of previously published systematic reviews evaluating the outcome of endodontic treatment. Int Endod J. 2009;42(8):656–66. doi: 10.1111/j.1365-2591.2009.01600.x. [DOI] [PubMed] [Google Scholar]
- 2.Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: The Toronto Study. Phase 1: Initial treatment. J Endod. 2003;29(12):787–93. doi: 10.1097/00004770-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Fernández R, Cadavid D, Zapata SM, Alvarez LG, Restrepo FA. Impact of three radiographic methods in the outcome of nonsurgical endodontic treatment: A five-year follow-up. J Endod. 2013;39(9):1097–103. doi: 10.1016/j.joen.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone. Part I. J Am Dent Assoc. 1961;62:152–60. [Google Scholar]
- 5.Huumonen S, Ørstavik D. Radiological aspects of apical periodontitis. Endod Topics. 2002;1:3–25. [Google Scholar]
- 6.Patel S. New dimensions in endodontic imaging: Part 2. Cone beam computed tomography. Int Endod J. 2009;42(6):463–75. doi: 10.1111/j.1365-2591.2008.01531.x. [DOI] [PubMed] [Google Scholar]
- 7.Webber RL, Messura JK. An in vivo comparison of diagnostic information obtained from tuned-aperture computed tomography and conventional dental radiographic imaging modalities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(2):239–47. doi: 10.1016/s1079-2104(99)70122-8. [DOI] [PubMed] [Google Scholar]
- 8.Cheung GS, Wei WL, McGrath C. Agreement between periapical radiographs and cone-beam computed tomography for assessment of periapical status of root filled molar teeth. Int Endod J. 2013;46(10):889–95. doi: 10.1111/iej.12076. [DOI] [PubMed] [Google Scholar]
- 9.Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod. 2007;33(9):1121–32. doi: 10.1016/j.joen.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 10.Low KM, Dula K, Bürgin W, von Arx T. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J Endod. 2008;34(5):557–62. doi: 10.1016/j.joen.2008.02.022. [DOI] [PubMed] [Google Scholar]
- 11.Grohndal H, Huumonen S. Radiographic manifestations of periapical inflammatory lesions. Endod Topics. 2004;8:55–67. [Google Scholar]
- 12.Bornstein MM, Lauber R, Sendi P, von Arx T. Comparison of periapical radiography and limited cone-beam computed tomography in mandibular molars for analysis of anatomical landmarks before apical surgery. J Endod. 2011;37(2):151–7. doi: 10.1016/j.joen.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 13.Estrela C, Bueno MR, Leles CR, Azevedo B, Azevedo JR. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J Endod. 2008;34(3):273–9. doi: 10.1016/j.joen.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 14.Paredes-Vieyra J, Enriquez FJ. Success rate of single- versus two-visit root canal treatment of teeth with apical periodontitis: A randomized controlled trial. J Endod. 2012;38(9):1164–9. doi: 10.1016/j.joen.2012.05.021. [DOI] [PubMed] [Google Scholar]
- 15.Low KM, Dula K, Bürgin W, von Arx T. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J Endod. 2008;34(5):557–62. doi: 10.1016/j.joen.2008.02.022. [DOI] [PubMed] [Google Scholar]
- 16.Stavropoulos A, Wenzel A. Accuracy of cone beam dental CT, intraoral digital and conventional film radiography for the detection of periapical lesions. An ex vivo study in pig jaws. Clin Oral Investig. 2007;11(1):101–6. doi: 10.1007/s00784-006-0078-8. [DOI] [PubMed] [Google Scholar]
- 17.Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int Endod J. 2011;44(7):583–609. doi: 10.1111/j.1365-2591.2011.01872.x. [DOI] [PubMed] [Google Scholar]
- 18.Friedman S, Mor C. The success of endodontic therapy – Healing and functionality. J Calif Dent Assoc. 2004;32(6):493–503. [PubMed] [Google Scholar]
- 19.Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl HG. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(1):114–9. doi: 10.1016/j.tripleo.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Liang YH, Li G, Wesselink PR, Wu MK. Endodontic outcome predictors identified with periapical radiographs and cone-beam computed tomography scans. J Endod. 2011;37(3):326–31. doi: 10.1016/j.joen.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 21.Gao Y, Haapasalo M, Shen Y, Wu H, Jiang H, Zhou X. Development of virtual simulation platform for investigation of the radiographic features of periapical bone lesion. J Endod. 2010;36(8):1404–9. doi: 10.1016/j.joen.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Brady E, Mannocci F, Brown J, Wilson R, Patel S. A comparison of cone beam computed tomography and periapical radiography for the detection of vertical root fractures in nonendodontically treated teeth. Int Endod J. 2014;47:735–46. doi: 10.1111/iej.12209. [DOI] [PubMed] [Google Scholar]
- 23.Varshosaz M, Tavakoli MA, Mostafavi M, Baghban AA. Comparison of conventional radiography with cone beam computed tomography for detection of vertical root fractures: An in vitro study. J Oral Sci. 2010;52(4):593–7. doi: 10.2334/josnusd.52.593. [DOI] [PubMed] [Google Scholar]
- 24.Hassan B, Metska ME, Ozok AR, van der Stelt P, Wesselink PR. Comparison of five cone beam computed tomography systems for the detection of vertical root fractures. J Endod. 2010;36(1):126–9. doi: 10.1016/j.joen.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 25.Durack C, Patel S, Davies J, Wilson R, Mannocci F. Diagnostic accuracy of small volume cone beam computed tomography and intraoral periapical radiography for the detection of simulated external inflammatory root resorption. Int Endod J. 2011;44(2):136–47. doi: 10.1111/j.1365-2591.2010.01819.x. [DOI] [PubMed] [Google Scholar]
- 26.Bernardes RA, de Paulo RS, Pereira LO, Duarte MA, Ordinola-Zapata R, de Azevedo JR. Comparative study of cone beam computed tomography and intraoral periapical radiographs in diagnosis of lingual-simulated external root resorptions. Dent Traumatol. 2012;28(4):268–72. doi: 10.1111/j.1600-9657.2011.01113.x. [DOI] [PubMed] [Google Scholar]
- 27.Tyndall DA, Kohltfarber H. Application of cone beam volumetric tomography in endodontics. Aust Dent J. 2012;57(Suppl 1):72–81. doi: 10.1111/j.1834-7819.2011.01654.x. [DOI] [PubMed] [Google Scholar]
- 28.Ball RL, Barbizam JV, Cohenca N. Intraoperative endodontic applications of cone-beam computed tomography. J Endod. 2013;39(4):548–57. doi: 10.1016/j.joen.2012.11.038. [DOI] [PubMed] [Google Scholar]
- 29.AAE, AAOMR. Use of Cone Beam Computed Tomography in Endodontics. Chicago, IL: American Association of Endodontists; 2011. [PubMed] [Google Scholar]


