Abstract
Background:
In the present study, the reliability of oral brush biopsy in identifying dysplasia in clinically diagnosed oral potentially malignant and malignant lesions was evaluated while comparing the findings with scalpel biopsy in terms of sensitivity and specificity.
Materials and Methods:
In our study, a total number of 50 patients that included both premalignant and malignant lesions were included. Oral brush cytology using a cytobrush was done for all patients, which was followed by incisional biopsy. Sensitivity, specificity, positive and negative predictive values were obtained. To see the agreement between two modalities Kappa test of agreement was applied. A P < 0.05 was considered to indicate statistical significance. Proportions were compared using Chi-square or Fisher’s exact test.
Results:
Brush cytology using a cytobrush is a reliable adjunct to histopathology in detecting oral premalignant and malignant oral lesions and can be easily performed with less cost and less discomfort. This technique showed a reasonable sensitivity and specificity thus substantiating its reliability in evaluation of oral premalignant and malignant lesions.
Conclusion:
The oral brush biopsy is a simple and rapid, non-invasive and relatively painless and well accepted by patient. It is suitable in population screening programs and for pre- and post-treatment observation of confirmed premalignant and malignant lesions and has proved applications in incapacitated areas.
Keywords: Cytobrush, cytopathology, incisional biopsy, potentially malignant, malignant lesions
Introduction
Cancer is a major cause of fear, morbidity and mortality all over the world. Cancer is one of the main causes of death in all societies, its relative position varying with age and sex.1 Globally, oral cancer is sixth most common cause of deaths because of cancer. The concept of cancer in oral mucosa is a two-step process of cancer i.e., the initial presence of a potentially malignant lesion subsequently developing into cancer, is well-established.2 Several oral potentially malignant lesions such as leukoplakia, erythroplakia, lichen planus, tobacco pouch keratosis and actinic keratosis are considered precursors for oral squamous-cell carcinoma, as there is increased risk of malignant transformation associated with them. In India, the high incidence of oral cancer has emphasized the relationship between tobacco chewing, smoking habits and oral cancer. Oral cancer, when diagnosed at an early stage, is often curable, inexpensive to treat and affords better quality of life. With this aim, various techniques have been developed to supplement clinical examination and improve the diagnosis of premalignant and early malignant lesions. There are various alternatives other than visual detection for the clinician that include iodine blue staining, chemiluminescent illumination, fluorescent techniques, oral brush biopsy, scalpel biopsy etc. Until date, there are no molecular markers, which assist us to identify lesions that may progress to carcinomatous changes.3 Clinical examination and histopathological examination are the established diagnostic methods used for the diagnosis of oral cancerous lesions. Biopsy is a “bloody” technique with surgical implications with certain technique limitations and psychological inference for some patients. In contrast, exfoliative cytology is a non-invasive, easy, reliable, ably accepted technique by the patient and is therefore an attractive adjunct for the early diagnosis of potentially malignant disorders and malignant lesions of oral mucosa.4 Multiple techniques are used to obtain the cells from the oral cavity such as rinsing, taking saliva sample or by scraping the surface of mucosa. An added advantage of oral cytobrush is that it obtains the cells extending up to deeper layers of the epithelium. The computer assisted oral brush cytology scans the cytology slides with oral CDx computer system that consists of an image-processing system based on neural network that is specifically designed to detect oral epithelial premalignant and malignant cells. However, availability and cost subdues its use in all settings. A less costly technique using brush cytology without computer-assisted analysis using cytobrush finds its applications in areas, which are resource-challenged and could be a risk-free method in the evaluation of lesions in the oral cavity.5
In our study, brush cytology of potentially malignant and malignant oral lesions was performed, and cytopathological examination was done. The results of brush cytology obtained were compared with that of conventional incisional biopsy results. In our study, we aimed at assessing the reliability of oral brush cytology in the detection of premalignant and malignant oral lesions in terms of specificity and sensitivity.
Materials and Methods
The patients reported to Department of Oral Medicine and Radiology, were selected for study purpose. Patients with suspicious premalignant and malignant lesions were selected irrespective of age and gender. Oral premalignant disorders such as Homogenous leukoplakia, speckled leukoplakia, verrucous leukoplakia, erythroplakia, tobacco pouch keratiosis, erosive lichen planus, oral carcinoma and patients with history of tobacco and related products and alcohol consumption were included in the study. Submucosal lesions, including the hemangioma, mucocele, papilloma, aphthous ulcer, fibroma and medically compromised patients (bleeding disorders, clotting disorders, systemic illness) where incisional biopsy could not be performed were excluded from the study. We conducted our study on 50 patients with clinically diagnosed premalignant and malignant lesions. We obtained a written informed consent from the patients, and every patient was subjected to a complete examination both extra-oral and intraoral. A detailed evaluation of various lesions was done. An oral brush cytology, followed by incisional biopsy was performed for every patient. Patients were made to rinse the oral cavity thoroughly with water, and the lesion was visualized. The brush was repeatedly brushed in one direction over entire lesion many times with moderate pressure until pinpoint bleeding was obtained, and thus obtaining epithelial cells through the full thickness of the epithelium (Figures 1 and 2).
Figure 1.

Intraoral picture showing non homogenous leukoplakia involving left buccal mucosa.
Figure 2.

Picture showing sample collection with cytobrush from left buccal mucosa.
Removed cells were transferred to a glass slide by distributing the obtained material evenly over the glass surface, and smear was made. The slides were then flooded with fixative solution (95% alcohol). The cellular sample on the slide was stained with Hematoxylin and Eosin and Papanicolaou method and scanned by light microscopy. Dysplastic features were looked for cells as the variation in nuclear size and shape (pleomorphism), nuclear borders, nucleo: Cytoplasmic ratio, number of nuclei, binucleation, tadpole forms, keratinization and hyperchromatism, chromatin pattern and distribution as well as discrepancy in nucleo-cytoplasmic maturation and a cytological diagnosis was given (Figures 3 and 4).6
Figure 3.
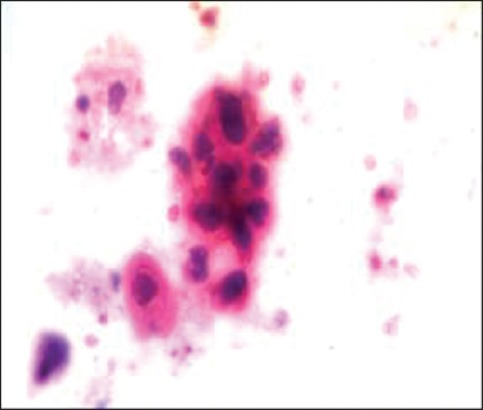
Cytopatholgy picture showing Class V smear showing loose cohesive clusters of pleomorphic cancer cells with scanty cytoplasm and enlarged nuclei containing numerous nucleoli suggestive of moderately differentiated squamous-cell carcinoma.
Figure 4.
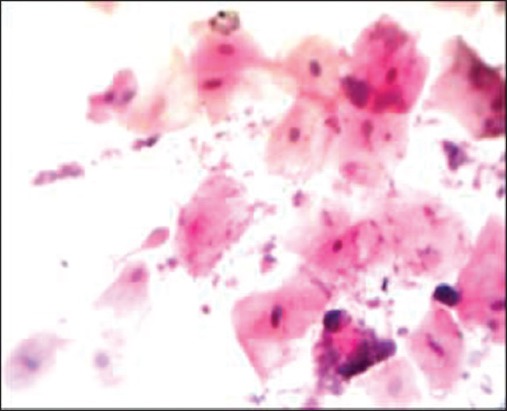
Cytopathology picture showing Class III cytosmear with tadpol cells present.
According to the classification of Papanicolaou (1960),7,8 cases were classified as:
CLASS I (Normal): Indicate that only normal cells were observed.
CLASS II (Atypical): Indicate minor atypia but no evidence of malignant changes.
CLASS III (Intermediate): The cells display wider atypia that may be suggestive of cancer, but they are not clear cut.
CLASS IV (Suggestive of cancer): Few epithelial cell with malignant character or many cells with borderline characteristic.
CLASS V (Positive cancer): Cells that are obviously malignant.
The biopsy sections obtained by incisional biopsy were interpreted by an oral pathologist and based on WHO, dysplasia and squamous-cell carcinoma were graded. Grading of dysplasia was done as mild, moderate, severe and carcinoma in situ while squamous cell carcinoma (SCC) was graded as well-differentiated, moderately differentiated and poorly differentiated. Considering the histopathological diagnosis as the gold standard, the cytopathological scores were compared. From the findings obtained altogether, the specificity and sensitivity of the oral brush biopsy were assessed by statistical analysis.
Statistical analysis
The statistical analysis of the samples was done in terms of sensitivity and specificity. All calculations were performed using SPSS® version 17 (Statistical Packages for the Social Sciences, Chicago, IL, USA). Qualitative or categorical variables were described as frequencies and proportions. Proportions were compared using Chi-square or Fisher’s exact test. To see the agreement between two modalities Kappa test of agreement was applied. A P < 0.05 was considered to indicate statistical significance. All tests were 2 sided. Sensitivity, specificity, positive predictive value (PPV) negative predictive value (NPV) and diagnostic accuracy were calculated for dysplasia in cytology while keeping histology as gold standard.
Results
Gender, age and site of involvement distribution in patients with pre malignant and malignant lesions (Tables 1a and b)
Table 1a.
Gender distribution in patients with pre malignant and malignant lesions.
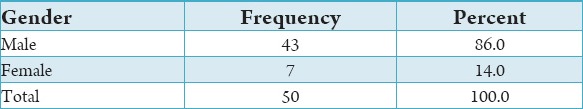
Table 1b.
Age and site of involvement distribution in patients with pre malignant and malignant lesions.
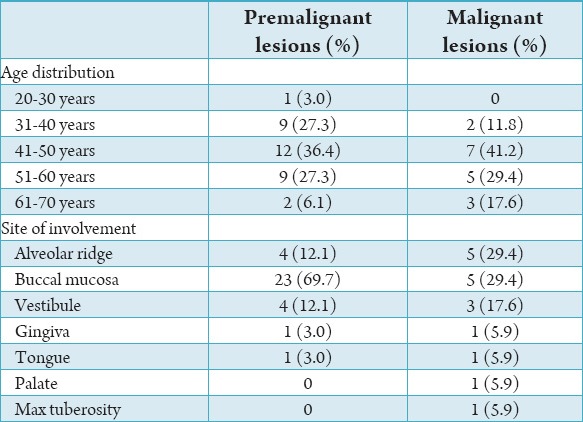
It was observed that out of the total of 50 patients, 43 patients (86%) were males, and 7 (14%) were females. Patients with premalignant lesions average age group ranged from 20 to 70 years which was subdivided into various age groups such as 20-30 years in which 1 (3%) patient was affected, at 31-40 years of age group 9 (27.3%) patients were affected at 41-50 years of age group 12 (36.4%) patients were affected, at age group 51-60 years of age group 9 (27.3%) patients were affected. And at age group of 61-70 years, 2 (6.1%) patients were affected. The patients with malignant lesions the average age group ranged from 20 to 70 years, which was subdivided into various age groups as 20-30 years, in which none of the patient reported, at 31-40 years of age group 2 (11.8%) patients were affected, at 41-50 years of age group 7 (41.2%) patients were affected, at age group 51-60 years of age group 5 (29.4%) patients were affected, at age group of 61-70 years 3 (17.63%) patients were affected. It was observed that the patients with premalignant lesions, 04 patients (12.1%) involving alveolar ridge, 23 patients (69.7%) involving buccal mucosa, 04 patients (12.1%) involving vestibule, 1 patient (3.0%) involving gingiva and none of the patient were reported with involvement of palate and maxillary tuberosity. Of 17 cases of malignant lesions, 5 patients were found in alveolar ridge (29.4%), 5 patients involving buccal mucosa (29.4%), 3 patients involving vestibule (17.6%), 1 patient involving gingiva (5.9%), 1 patient involving palate (5.9%) and 1 patient involving maxillary tuberosity (5.9%).
Cytopathological findings in premalignant and malignant lesions (Tables 2a and b)
Table 2a.
Cytopathological classification of premalignant lesions.
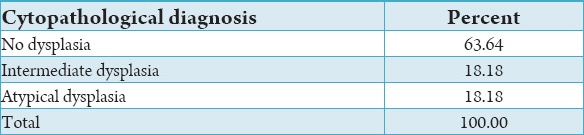
Table 2b.
Cytopathological classification of malignant lesions.
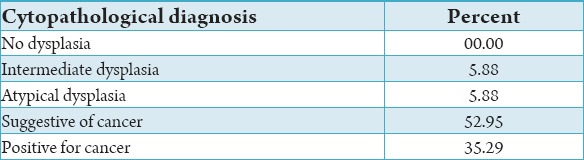
In a total number of 33 premalignant lesions, out of which 21 (63.64%) cases reported with no dysplasia, 06 (18.18%) cases reported with intermediate dysplasia, 06(18.18%) cases reported with atypical dysplasia on cytopathology. It was observed that 17 malignant lesions, 1 (5.88%) case reported with intermediate dysplasia, 01 (5.88%) case reported with atypical dysplasia, 09 (52.95%) cases reported with suggestive of dysplasia, 6 (35.29%) cases reported as positive for cancer.
Histopathological findings in premalignant and malignant lesions (Tables 3a and b)
Table 3a.
Histopathological classification in premalignant lesions.
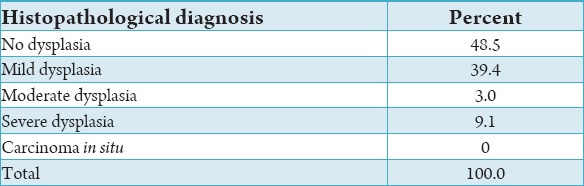
Table 3b.
Histopathological classification in malignant lesions.
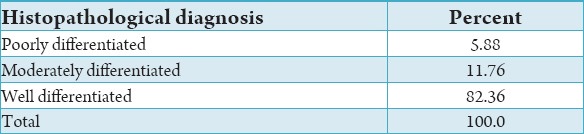
In patients with premalignant lesions, 16 (48.5%) cases reported with no dysplasia, 13 (39.4%) cases reported with mild dysplasia, 1 (3%) case reported with moderate dysplasia, 3 (9.1%) cases reported with severe dysplasia and no case reported with carcinoma in situ on histopathology. A total of 17 malignant lesions, out of which 1 (5.88%) case reported as poorly differentiated SCC, 2 (11.76%) cases reported as moderately differentiated SCC, 14 (82.36%) cases reported as well differentiated SCC.
Comparison of histopathology and cytopathology
Cytopathological scores and histopathological scores of premalignant and malignant lesions were compared and kappa test showed P < 0.05 indicating of statistically significant difference.
Sensitivity and specificity of oral brush cytology (Table 4)
Table 4.
Sensitivity and specificity of oral brush biopsy for premalignant and malignant lesions.
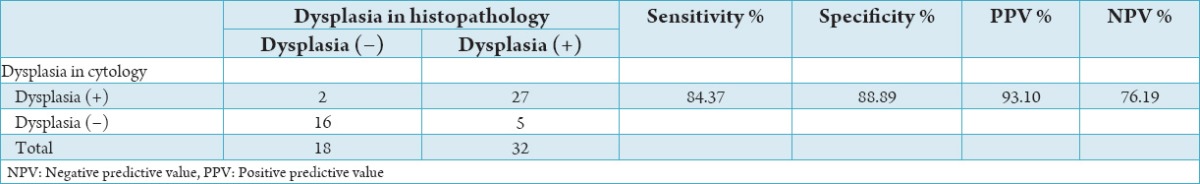
Twenty-seven cases as true positive, 2 cases as false positive, 5 cases as false negative and 16 cases as true negative. We found statistical sensitivity and specificity of brush biopsy as 84.37% and 88.89% respectively. The PPV and NPV obtained were 93.10%, 76.19% respectively with 86% as diagnostic accuracy.
Discussion
Oral cancer is a world-wide health problem with its increased incidence and mortality rates. In the Indian subcontinent, the prevalence of oral cancer is the highest among all cancers in men even though it is only the sixth most common cancer worldwide. About 92-95% of all oral malignancies are oral SCC. Although scalpel biopsy is considered as the gold standard in diagnosing the premalignant and malignant lesions, but it is not feasible to use the procedure in all suspected cases. In such cases, brush cytology offers an attractive alternative. Scheifele et al. suggested that the oral brush biopsy has an advantage of identifying the dysplastic cells or molecular variations indicating for histological control, even in apparently benign oral lesions clinically.4,6,8
This study was undertaken to assess the reliability of oral brush biopsy in terms of sensitivity, specificity.1,4
The present study comprised of 50 patients, of which 43 patients (86%) were males and 7 (14%) were females (Table 1a). The changes in the gender differences occur in both premalignant and malignant lesions appeared due to differences in risk exposure. Males are affected two to three times as often as females largely because of their indulgence in the most important risk factors, such as alcohol and tobacco consumption. Oral cancer represents more than 4% males and 2% in females of total body cancers. This statistically similar throughout and higher rates are reported in India reflecting toward higher male indulgence into various risk factors such as tobacco smoking and alcohol consumption when compared to females.1 We found male predominance in both premalignant and malignant lesions which is in accordance with studies done by Mehrotra et al.,6 Rahman et al.,7 Singh,9 Scheifele et al.10
In the present study, we found that premalignant and malignant lesions occur in older age group with age group of 41-50 years predominantly affected (Table 1b). The overall age-related incidence of premalignant and malignant lesion suggests the time-dependent factors results in initiation and promotion of genetic events that results in changes. Oral cancer is disease of increasing age about 95% of the cases occur in patients older than 40 years, with an average age of about 60 years at diagnosis. Our findings are in accordance to studies done by Mehrotra et al.,6 Rahman et al.,7 Kumar et al.11
Clinically the variations in site were found in premalignant lesions and malignant lesions (Table 1b). The premalignant lesions showed 69.7% involving buccal mucosa, 12.1% involving alveolar ridge, 12.1% involving vestibule, 3.0% involving gingiva and none of the patient was reported with involvement of palate and maxillary tuberosity. Out of 17 cases of malignant lesions, 29.4% were found in the alveolar ridge and buccal mucosa, 17.6% involving vestibule, 5.9% involving gingiva, palate, maxillary tuberosity. The variation in site of involvement may be due to the regional differences as extensive use and site of placement of chewing tobacco in Indian subcontinent with prolonged contact with the carcinogen. Secondly, buccal mucosa is covered with a thinner, non-keratinized mucosa that provides less protection against carcinogen. The variation in site was also found in patients with malignant lesions.12
Similarly studies done by Sciubba,13 Scheifele et al.10 found in their study that site for predilection for premalignant lesions in buccal mucosa. Mishra et al.14 found in their study that the common site of involvement for leukoplakia was buccal mucosa. Similar studies done by Babshet et al.4 observed buccal mucosa was most frequently involved site for premalignant and malignant lesions. Mehrotra et al.6 done a similar study and stated that buccal mucosa and tongue were the most frequently involved site for premalignant and malignant lesions. In our study we found the buccal mucosa as a predominant site for premalignant and malignant lesions which is in accordance with the studies done by Mehrotra et al.,6 Babshet et al.,4 Scheifele et al.,10 Sciubba,13 Mishra et al.14
In our study, premalignant and malignant lesions have been categorized on the basis of cytological changes according to criteria given by Papanicolaou (1960). He has categorized the cytological changes according to cellular feature variation. Potentially malignant lesions are reported into 5 categories according to the severity of their component cells. They are Class I (Normal): Indicate that only normal cells are observed, Class II (Atypical): Indicate minor atypia, but no evidence of malignant changes, Class III (intermediate): The cells display wider atypia that may be suggestive of cancer, but they are not clear cut, Class IV (suggestive of cancer): Few epithelial cells with malignant character or many cells with borderline characteristic, Class V (positive cancer): Cells that are obviously malignant. Feature variations that increase with increased severity of dysplasia include the mitosis, N/C ratio, anischromatism, nuclear membrane irregularities, nuclear hypertrophy, anisokaryosis, hyperchromatism, nucleoli.4-6 In a total number of 33 premalignant lesions, out of which 21 cases reported with no dysplasia, 6 cases reported with intermediate dysplasia, 6 cases reported with atypical dysplasia on cytopathology, a total number of 17 malignant lesions, out of which 1 case reported with intermediate dysplasia, 1 case reported with atypical dysplasia, 9 cases reported with suggestive of dysplasia, 6 cases reported as positive for cancer (Table 2a and b). In our study, the premalignant and malignant lesions have been categorized on the basis of dysplastic changes on histopathology, according to criteria given by WHO 2005. In a total number of 33 premalignant lesions, 16 (48.5%) cases reported with no dysplasia, 13 (39.4%) cases reported with mild dysplasia, 1 (3%) case reported with moderate dysplasia, 3 (9.1%) cases reported with severe dysplasia and no case reported with carcinoma in situ on histopathology. In 17 malignant lesions, out of which 1 case reported as poorly differentiated SCC, 2 cases reported as moderately differentiated SCC, 14 cases reported as well-differentiated SCC (Table 3b).
It is always assumed that there is temporal progression of premalignant lesions related to multistage carcinogenesis and there is progression of mild dysplasia to severe dysplasia to malignancy. There are no molecular markers, which will differentiate the lesions that may progress to carcinomatous changes, at present.5
Although clinical examination and histopathological studies are considered the classical diagnostic methods used for the diagnosis of oral malignant lesions. Biopsy is a “bloody” technique along with surgical implications, technique limitations and psychological factors associated. Invariance, exfoliative cytological procedure is an uncomplicated, dependable technique that is beneficial for the early diagnosis of oral cancers.4 The cytopathological study is proposed to be useful early diagnostic method for epithelial atypia and for also malignant oral lesions.6,7
The cytopathological scores and histopathological scores of premalignant and malignant lesions were compared, and kappa test showed P < 0.05 suggestive of statistically significant. Similarly studies done by Scuibba for oral cdx as method of detecting oral precancerous and cancerous lesions who found similar significant values. Mehrotra et al. found statistically significant difference while finding statistical sensitivity and specificity of brush biopsy in detecting dysplastic changes in oral lesions.6,13
In our study, we found 27 cases as true positive, 2 cases as false positive, 5 cases as false negative and 16 cases as true negative. The statistical sensitivity of brush biopsy is 84.37% and specificity is 88.89%. The PPV and NPV obtained are 93.10%, 76.19%, respectively. The results obtained in our study showed specificity (88.89%) is greater than sensitivity (84.37%), which is in accordance to studies done by Mehrotra et al.,6 Driemel et al.,15 Edris et al.16
Conclusion
This study suggests that the early detection of oral malignant lesions is possible at the premalignant stages using oral brush biopsy without computer-assisted analysis upsurging the spectrum of chairside investigations. It is a non-invasive technique that is well accepted by the patient and an adjunct to early diagnosis of premalignant and malignant lesions of the oral mucosa. There is statistically significant association found between histopathological and cytopathological diagnosis in diagnosing dysplasias or carcinoma. This technique showed a reasonable specificity and sensitivity to rule out dysplasia in oral precancerous and cancerous lesions. Thus, oral brush cytology is a convenient diagnostic procedure as it is non-invasive, inexpensive, cognizant, reliable and can be used in medically compromised patients. Further studies with larger sample size are required to evaluate the role of oral brush biopsy in oral premalignant and malignant lesions and to support the results of our study.
Footnotes
Conflicts of Interest: None
Source of Support: Nil
References
- 1.Shah JP, Johnson NW, Batsakis JG, editors. Oral Cancer. London: Martin and Dunitz, Taylor & Francis Group; 2003. pp. 3–165. [Google Scholar]
- 2.Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36(10):575–80. doi: 10.1111/j.1600-0714.2007.00582.x. [DOI] [PubMed] [Google Scholar]
- 3.Burkhardt A. Advanced methods in the evaluation of premalignant lesions and carcinomas of the oral mucosa. J Oral Pathol. 1985;14(10):751–78. doi: 10.1111/j.1600-0714.1985.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 4.Babshet M, Nandimath K, Pervatikar S, Naikmasur V. Efficacy of oral brush cytology in the evaluation of the oral premalignant and malignant lesions. J Cytol. 2011;28(4):165–72. doi: 10.4103/0970-9371.86342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Acha A, Ruesga MT, Rodríguez MJ, Martínez de Pancorbo MA, Aguirre JM. Applications of the oral scraped (exfoliative) cytology in oral cancer and precancer. Med Oral Patol Oral Cir Bucal. 2005;10(2):95–102. [PubMed] [Google Scholar]
- 6.Mehrotra R, Singh MK, Pandya S, Singh M. The use of an oral brush biopsy without computer-assisted analysis in the evaluation of oral lesions: A study of 94 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(2):246–53. doi: 10.1016/j.tripleo.2008.02.030. [DOI] [PubMed] [Google Scholar]
- 7.Rahman F, Tippu SR, Khandelwal S, Girish KL, Manjunath BC, Bhargava A. A study to evaluate the efficacy of toluidine blue and cytology in detecting oral cancer and dysplastic lesions. Quintessence Int. 2012;43(1):51–9. [PubMed] [Google Scholar]
- 8.Bancroft JD. Theory and Practice of Histological Techniques. 5th ed. New York: Churchill Livingstone; 2008. pp. 125–35. 631. [Google Scholar]
- 9.Singh A. Role of exfoliative cytology in oral lesions: With special reference to rule out malignancy. J Coll Med Sci. 2010;6(2):29–37. [Google Scholar]
- 10.Scheifele C, Schmidt-Westhausen AM, Dietrich T, Reichart PA. The sensitivity and specificity of the OralCDx technique: Evaluation of 103 cases. Oral Oncol. 2004;40(8):824–8. doi: 10.1016/j.oraloncology.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Kumar S, Vezhavendhan N, Priya S. Role of oral exfoliative cytology in oral leukoplakia and squamouscell carcinoma. IJCDS. 2011;2(1):93–7. [Google Scholar]
- 12.Venkataraman BK Oral premalignancy and oral cancer. Diagnostic Oral Medicine. Ch. 29. Baltimore: Lippincott Williams & Wilkins Year; 2013. pp. 556–75. [Google Scholar]
- 13.Sciubba JJ. Oral leukoplakia. Crit Rev Oral Biol Med. 1995;6(2):147–60. doi: 10.1177/10454411950060020401. [DOI] [PubMed] [Google Scholar]
- 14.Mishra M, Mohanty J, Sengupta S, Tripathy S. Epidemiological and clinicopathological study of oral leukoplakia. Indian J Dermatol Venereol Leprol. 2005;71(3):161–5. doi: 10.4103/0378-6323.16229. [DOI] [PubMed] [Google Scholar]
- 15.Driemel O, Dahse R, Berndt A, Pistner H, Hakim SG, Zardi L, et al. High-molecular tenascin-C as an indicator of atypical cells in oral brush biopsies. Clin Oral Investig. 2007;11(1):93–9. doi: 10.1007/s00784-006-0086-8. [DOI] [PubMed] [Google Scholar]
- 16.Edris A, Gadelkarim H, Mohammed E. Accuracy of oral exfoliative cytology in Sudanese patients undergoing oral biopsy. RSBO. 2011;8(3):255–60. [Google Scholar]


