Abstract
Ependymoma is a relatively rare malignancy accounting for 2.0% of all primary central nervous system tumors in adults. Extracranial metastasis is a very uncommon complication of gliomas, especially of anaplastic ependymomas. The objective of this paper is to show that ependymomas can metastasize to soft tissue and lymph nodes as well as to share our approach to this challenge. We report a male patient with anaplastic ependymoma that recurred, metastasizing to the neck and lymph nodes. Metastatic disease was diagnosed based on clinical presentation of a palpable nodule on the right neck and diffuse cervical lymphadenopathies. A biopsy was obtained and pathology revealed anaplastic ependymoma. Whole-body fluorodeoxyglucose positron emission tomography scan showed metastatic disease in the right mastoid region with diffuse uptake in the cervical lymph nodes. Clinical and radiologic response was achieved after three chemotherapy cycles of etoposide, cisplatin, vincristine, and cyclophosphamide. This case highlights extracranial metastasis to the soft tissue as an atypical presentation of recurrent anaplastic ependymoma. Other reported instances of extracranial metastatic ependymoma of this presentation are discussed. The possible metastatic pathways of intracranial disease are discussed. It also illustrates how extracranial disease remains stable with systemic chemotherapy.
Keywords: Anaplastic ependymoma, Extracranial metastases, Extraneural metastases
1. Introduction
Ependymomas are glial neoplasms arising from ependymal cells lining the ventricular system, spinal cord and cortical rests [1]. The incidence rates of ependymomas are higher in children, and account for 2% of all adult intracranial tumors [2]. Anaplastic ependymomas are the most aggressive form characterized by increased cellularity, atypia, proliferation indices, mitotic activity, vascular proliferation and necrosis, with a greater propensity to infiltrate the surrounding brain tissue as well as spread to cerebrospinal fluid [3]. Early diagnosis is crucial to the management of these tumors. The mainstay of treatment and key prognostic factor is the extent of surgical resection [4], but this carries a risk of significant neurological complications [5]. Adjuvant radiotherapy has a role prolonging the overall survival, in contradistinction to chemotherapy [6]. Extracranial metastasis is uncommon, with the incidence reported at 0.4–2% for all brain/spine tumors, however it is overestimated [3]. Several mechanisms of metastasis have been reported. This is a case of supratentorial extraventricular anaplastic ependymoma with extracranial metastasis.
2. Case report
A 21-year-old man presented with headaches and neck pain in November 2007. Brain MRI showed an enhancing mass with a cystic component in the right temporoparietal region measuring 5.1 × 3.8 cm. He underwent a gross total resection (GTR), and the pathology revealed anaplastic ependymoma. Then, he received radiation therapy with a total dose of 54 Gy. In October 2010, he developed left arm numbness. Brain MRI showed tumor recurrence in the right parietal lobe measuring 3.7 × 2.9 cm. He underwent a second GTR, followed by stereotactic radiosurgery (SRS) and 12 cycles of standard-dose temozolomide. In December 2011, he had a seizure and brain MRI showed second recurrence in the right occipital lobe. He had a third GTR, and pathology revealed anaplastic ependymoma. Adjuvant therapy consisted of SRS, followed by 16 cycles of temozolomide and bevacizumab. In September 2013, a nodule in the right aspect of the neck was biopsied, and pathology revealed metastatic anaplastic ependymoma, with CDKN2A loss. A fluorodeoxyglucose positron emission tomography (FDG-PET) scan and MRI showed metastatic disease in the right mastoid region with diffuse cervical lymphadenopathies (Fig.1). Spine MRI and CT scan of the thorax, abdomen and pelvis were unremarkable, and 5-fluorouracil did not show radiological response. In February 2014, he started on etoposide, cisplatin, vincristine and cyclophosphamide, completing three cycles in April 2014. Repeat FDG-PET scan showed decreased size and uptake of the neck tumor and brain MRI did not show any disease. Chemotherapy was discontinued as the patient had difficulty tolerating the regimen. On examination, there was no focal neurological deficit. Physical examination revealed a painless, indurated, 10 × 8 cm neck mass and diffuse palpable cervical lymph nodes.
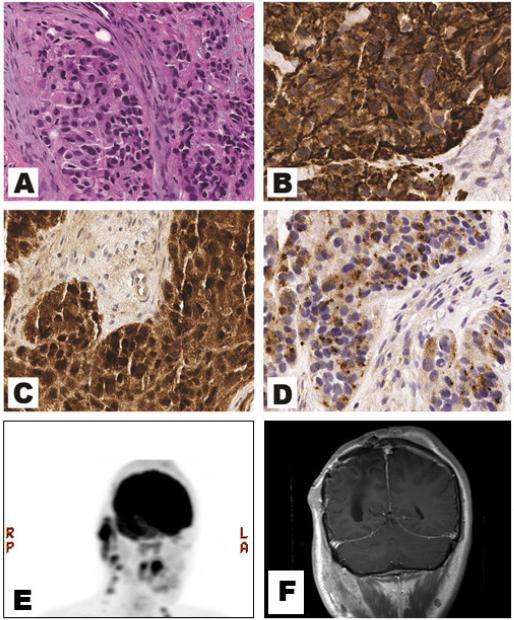
Fig. 1.
Right occipital subcutaneous mass. Biopsy showed islands of tumor cells separated by fascicles of fibroconnective tissue with few scattered adipocytes. (A) Mitotic activity, microvascular proliferation, and necrosis were inconspicuous (hematoxylin and eosin, original magnification × 200). (B) The tumor cells showed diffuse cytoplasmic glial fibrillary acidic protein (GFAP) immunoexpression (GFAP, original magnification × 200), (C) diffuse cytoplasmic and nuclear S100 immunoexpression (S100, original magnification × 200) and (D) diffuse perinuclear “dot-like” and “ring-like” epithelial membrane antigen (EMA) immunoexpression suggestive of ependymal differentiation (EMA, original magnification × 200). (E) The corresponding positron emission tomography scan showing fluorodeoxyglucose avidity in right mastoid and cervical lymphadenopathy and (F) a T1-weighted post-contrast coronal MRI of the brain shows enhancing lesion in the right neck soft tissue (F).
3. Discussion
As extracranial metastasis of anaplastic ependymoma has rarely been reported in the literature, it is difficult to calculate its occurrence accurately. There are several hypotheses regarding the metastatic spread of intracranial tumors, including surgical manipulation with breach of anatomic barriers, hematogeneous spread after tumor invasion of the dural veins, via the ventricular system (drop or retrograde metastases), via ventriculoperitoneal shunts, and via hematogeneous or lymphatic spread after tumor invasion of the skull and extracranial tissues [7]. Three other patients in addition to ours had metastatic spread after a surgical procedure; manipulation of the tumor site and seeding during the invasive procedure may have a role in the development of metastasis (Table 1) [8-10].
Table 1.
Demographics, clinical presentation, treatment and outcome in patients with metastatic ependymoma
| Authors | Sex/age, years | Location of tumor | Site of metastasis | Clinical presentation | Initial therapy | Number of recurrences | Treatment of metastasis | Time elapsed between diagnosis and metastasis | Overall survival |
|---|---|---|---|---|---|---|---|---|---|
| Davis et al. (8) |
F/22 | Frontal and temporal lobe |
Scalp nodule, neck, parotid gland, cervical lymph nodes |
Headaches, dysarthria |
GTR and XRT | 0 | Neck dissection and XRT |
12 months | 54 months |
| Itoh et al. (9) |
M/59 | Cerebellar hemisphere |
Lungs, subcutaneous tissue |
Headache, vomiting, ataxia |
Subtotal resection with XRT, recurrence 14 months later at resection site, re-resected followed by XRT and human interferon |
1 | Cyclophosphamide doxorubicin and etoposide |
28 months | 36 months |
| Donepudi et al. (10) |
M/57 | Parietal lobe | Scalp nodule, right parotid gland, cervical lymph nodes |
Not described in article |
Five intracranial recurrences, initially treated with subtotal resection and XRT with a short course of carmustine, first 4 recurrences treated with GTR, 5th recurrence treated with SRS radiosurgery and 4 cycles of TMZ |
5 | Superficial parotidectomy and extended modified radical neck dissection, irinotecan and bevacizumab |
108 months | 180 months |
| Present study |
M/21 | Temporal and parietal lobe |
Neck, cervical lymph nodes |
Severe headaches, neck pain |
GTR and XRT; 1st recurrence GTR followed by SRS followed by TMZ for 1 year; 2nd recurrence GTR, followed by SRS, 16 cycles of adjuvant TMZ and bevacizumab were then administered |
2 | 5-FU, followed by etoposide, cisplatin, vincristine and cyclophosphamide |
60 months | 69 months |
F = female, GTR = gross total resection, M = male, SRS = stereotactic radiosurgery, TMZ = temozolomide, XRT = radiation therapy, 5-FU = 5-fluorouracil.
It is possible that tumor growth may breach the normal anatomical site and spread tumor cells into the general circulation [7]. Primary brain tumors often have a poor response to chemotherapy due to the poor blood–brain barrier penetration [8]. There is evidence that extracranial metastasis is not subject to this same restriction, allowing chemotherapy be more successful than in intracranial tumors [11]. Our case supports this theory as the tumor had a complete response to chemotherapy. It is also significant that while his tumor metastasized, his intracranial disease is stable and has not shown evidence of recurrence in 34 months. Supratentorial ependymomas are characterized by connection to the ventricular system, but our patient does not reflect this generalization [8].
Propensity of anaplastic ependymoma to metastasize as well as its aggressiveness may be correlated to a Ki67 index above 10% [8]. The current case was also significant for CDKN2A loss which has been associated with unfavorable prognosis in ependymoma [12]. This case is unique in that a more aggressive chemotherapy regimen was used for recurrent metastatic disease. After three cycles of etoposide, cisplatin, vincristine, and cyclophosphamide, a decrease in size and uptake was observed on FDG-PET scan. This is evidence that this regimen may be useful in the treatment of ependymoma.
Highlights For Review.
A case of metastatic anaplastic ependymoma to the neck in an adult male
Tumor seeding and metastasis may have been caused by surgery
Treatment consisted of etoposide, cisplatin, vincristine, and cyclophosphamide
Clinical and radiological response achieved 3 cycles
Acknowledgements
This study did not involve use of any grant funds. A. Olar was supported by the National Institutes of Health/National Cancer Institute (Training Grant No.5T32CA163185).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest/Disclosures
L.A. Pachella, C. Kamiya-Matsuoka, E.L.T. Lee, and W.K.A. Yung report no disclosure.
References
- 1.Gilbert MR, Ruda R, Soffietti R. Ependymomas in adults. Curr Neurol Neurosci Rep. 2010;10(3):240–7. doi: 10.1007/s11910-010-0109-3. [DOI] [PubMed] [Google Scholar]
- 2.Dolecek TA, et al. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005-2009. Neuro Oncol. 2012;14(Suppl 5):v1–49. doi: 10.1093/neuonc/nos218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armstrong TS, et al. Adult ependymal tumors: prognosis and the M. D. Anderson Cancer Center experience. Neuro Oncol. 2010;12(8):862–70. doi: 10.1093/neuonc/noq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinoshita M, et al. Long-term control of recurrent anaplastic ependymoma with extracranial metastasis: importance of multiple surgery and stereotactic radiosurgery procedures--case report. Neurol Med Chir (Tokyo) 2004;44(12):669–73. doi: 10.2176/nmc.44.669. [DOI] [PubMed] [Google Scholar]
- 5.Wetjen N, Raffel C. Ependymomas. In: Tonn J-C, Westphal M, Rutka J, editors. Oncology of CNS Tumors. Springer; Berlin Heidelberg: 2010. pp. 503–512. [Google Scholar]
- 6.Chao MM, et al. Isolated extracranial recurrence of anaplastic ependymoma. Pediatr Blood Cancer. 2011;56(2):317–8. doi: 10.1002/pbc.22764. [DOI] [PubMed] [Google Scholar]
- 7.Mondin V, et al. A survey of metastatic central nervous system tumors to cervical lymph nodes. Eur Arch Otorhinolaryngol. 2010;267(11):1657–66. doi: 10.1007/s00405-010-1357-1. [DOI] [PubMed] [Google Scholar]
- 8.Davis MJ, et al. Extraventricular anaplastic ependymoma with metastasis to scalp and neck. J Neurooncol. 2011;104(2):599–604. doi: 10.1007/s11060-010-0525-x. [DOI] [PubMed] [Google Scholar]
- 9.Itoh J, et al. Extracranial metastases of malignant ependymoma--case report. Neurol Med Chir (Tokyo) 1990;30(5):339–45. doi: 10.2176/nmc.30.339. [DOI] [PubMed] [Google Scholar]
- 10.Donepudi SK, Tennant PA, Samant S. Anaplastic ependymoma metastatic to the neck. Laryngoscope. 2009;119(SUPPL. 1):66. [Google Scholar]
- 11.Friedman HS, et al. Activity of temozolomide in the treatment of central nervous system tumor xenografts. Cancer Research. 1995;55(13):2853–2857. [PubMed] [Google Scholar]
- 12.Korshunov A, et al. Molecular staging of intracranial ependymoma in children and adults. J Clin Oncol. 2010;28(19):3182–90. doi: 10.1200/JCO.2009.27.3359. [DOI] [PubMed] [Google Scholar]