Abstract
Background Despite being central to achieving improved population health outcomes, primary health centres in low- and middle-income settings continue to underperform. Little research exists to adequately explain how and why this is the case. This study aimed to test the relevance and usefulness of an adapted conceptual framework for improving our understanding of the mechanisms and causal pathways influencing primary health centre performance.
Methods A theory-driven, case-study approach was adopted. Four Zambian health centres were purposefully selected with case data including health-care worker interviews (n = 60); patient interviews (n = 180); direct observation of facility operations (2 weeks/centre) and key informant interviews (n = 14). Data were analysed to understand how the performance of each site was influenced by the dynamic interactions between system ‘hardware’ and ‘software’ acting on mechanisms of accountability.
Findings Structural constraints including limited resources created challenging service environments in which work overload and stockouts were common. Health workers’ frustration with such conditions interacted with dissatisfaction with salary levels eroding service values and acting as a catalyst for different forms of absenteeism. Such behaviours exacerbated patient–provider ratios and increased the frequency of clinical and administrative shortcuts. Weak health information systems and lack of performance data undermined providers’ answerability to their employer and clients, and a lack of effective sanctions undermined supervisors’ ability to hold providers accountable for these transgressions. Weak answerability and enforceability contributed to a culture of impunity that masked and condoned weak service performance in all four sites.
Conclusions Health centre performance is influenced by mechanisms of accountability, which are in turn shaped by dynamic interactions between system hardware and system software. Our findings confirm the usefulness of combining Sheikh et al.’s (2011) hardware–software model with Brinkerhoff’s (2004) typology of accountability to better understand how and why health centre micro-systems perform (or under-perform) under certain conditions.
Keywords: Health systems, health system strengthening, primary health centres, service-delivery, accountability, complexity
KEY MESSAGES.
Despite being central to achieving improved population health outcomes, primary health centres in low- and middle-income settings continue to underperform with little research to adequately explain how and why.
This study aimed to test the relevance and usefulness of an adapted health systems framework for application to micro-level health systems
Findings demonstrated that health centre performance is influenced by the dynamic interactions between system hardware and system software, which act on mechanisms of accountability.
Introduction
Health systems are commonly conceptualized as national, macro-level entities, with functions spanning the development of health policies, co-ordination of services and interventions, and the balancing of cross-sectoral health needs (Fulop et al. 2001; van Olmen et al. 2010). Yet health systems also operate at the meso-level—with provincial or other sub-national systems overseeing the adaptation of national policies and guidelines and implementation of institutional responses (Gilson 2012)—and at the micro-level—comprising interactions between providers, patients, managers and citizens.
In low- and middle-income countries (LMICs) micro-level health systems are typically found within a network of primary-level services such as health centres, clinics and/or health posts (van Olmen et al. 2010). Although individually modest in scope, primary-level services are often the only type of formal health care accessible to a majority of the population (Gormley et al. 2011; Komatsu et al. 2008; Schneider et al. 2006a). As such, they play a critical role in both population health and broader human development efforts. Indeed, various international health initiatives [including in the watershed Alma Ata Declaration; Millennium Development Goals 4, 5 and 6; and the post-2015 clarion call for universal health coverage (UHC)] have, both explicitly and implicitly, recognized the importance of such services (Victora et al. 2013; Vega 2013; Shelton 2013; Ooms et al. 2013; Mulley et al. 2013).
Decentralized, equitable and responsive primary health services are essential for achieving population health outcomes. Despite this, research demonstrates that primary-level health services remain weak across many LMICs, with evidence of inconsistent or low quality of care (Das 2004; Nolan et al. 2001; Peabody et al. 2006); poor service environments and drug stockouts (Schneider et al. 2006a); low morale and negative attitudes among front-line health workers (Bassett et al. 1997; Jewkes et al. 1998) and irregular or unethical conduct (Jesani 1998; Maestad and Mwisongo 2011; Sheikh and Porter 2010).
Lack of guidance on how to address such problems (Gilson 2012; Gilson et al. 2001) is, in part, the result of a skewed research focus on questions of whether or not primary services are delivering quality care. By comparison, little empiric research has focused on questions of how and why primary-level health services perform in certain ways and under certain conditions although there are some notable exceptions (Rowe et al. 2005; Gilson and Daire 2011; Ssengooba et al. 2012; Schneider et al. 2006b; Schneider et al. 2008; Schneider and Lehmann 2010; Schneider and Palmer 2002).
The study reported here formed part of a larger research project assessing the impact of HIV service scale-up on front-line health-centre operations in Zambia. Recognizing the dearth of exploratory and explanatory research in this area, a specific objective of the larger study was to first produce theoretically informed insights relating to the mechanisms driving health-centre performance, in order to better understand the ways in which HIV care and treatment services influenced these services. In this article we report findings from this first objective.
Methods
Study setting
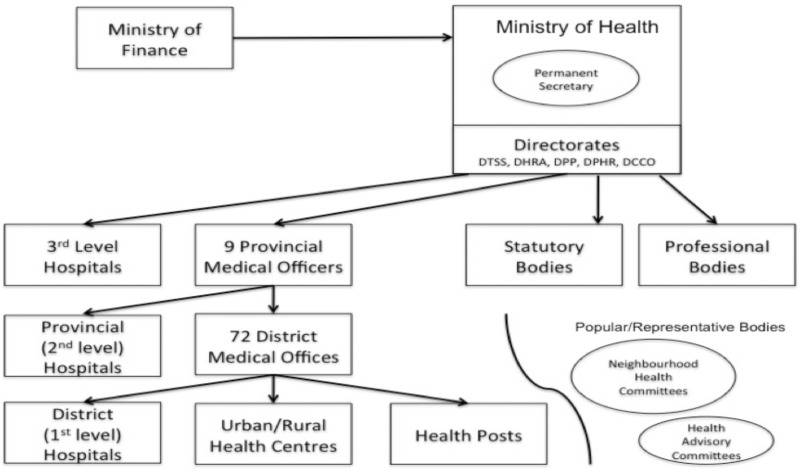
At the time of study Zambia’s health system was relatively centralized with the Ministry of Health (MOH) responsible for all national health policies as well for direct oversight of tertiary hospital operations. Responsibility for the network of 1500 first and second level health facilities (primary health centres and first and second level hospitals) lay with Provincial and District Health Offices (Figure 1).
Figure 1.
Ministry of Health Administrative Structure c. 2011. Adapted from Thet (2007). Arrows indicate channel of authority, financing or influence. DTSS = Directorate of Technical Support Services; DHRA = Directorate of Human Resources and Administration; DPP = Directorate of Policy and Planning; DPHR = Directorate of Public Health and Research; DCCD = Directorate of Clinical Care and Diagnostic Services.
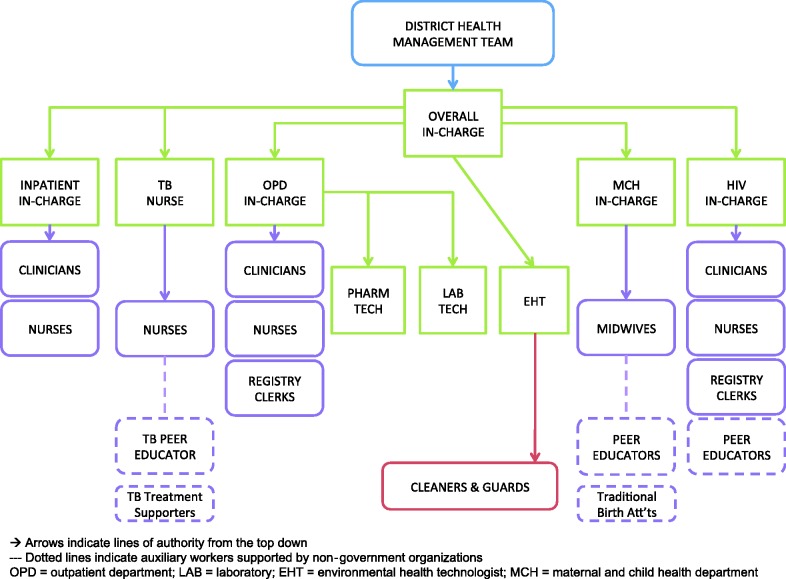
Primary health centres make up the majority (79%) of Zambia’s health facilities with approximately 29% located in in urban areas. Officially, urban health centres serve a catchment population of 30 000 to 50 000, while rural health centres serve a population of up to 10 000 MOH, GRZ (2007). Depending on location and resourcing, urban and rural health centres may include any combination of an outpatient department (OPD), inpatient department (IPD), maternal and child health department (MCH), labour ward, tuberculosis treatment department (TB corner), HIV care and treatment department (HIV department), laboratory and environmental health team (EHT). The administrative structure of a typical health centre is outlined in Figure 2.
Figure 2.
Typical reporting structure in a Zambian primary health centre.
Conceptual framework
Both this study and the larger research project were located within the field of health policy and systems research (HPSR). This multi-disciplinary domain is informed by insights from complexity science and systems thinking (de Savigny and Adams 2009) and can be distinguished from traditional health services research due to its whole-of-system focus (Gilson and Daire 2011). Insights from HSPR of particular importance to this study included the notion that health systems are open (influenced by the social, political and cultural context in which they operate); social (shaped by the decisions, actions and interactions between humans within the system); and dynamic (continually influenced by the nature and bi-directionality of interactions between human actors and their environment). Although such notions have most often been applied to macro-level health system analyses, it is our contention that they are equally applicable to micro-level systems including those found in localized service-delivery platforms such as primary health centres.
We took as a starting point Sheikh et al.’s (2011) ‘Hardware–Software’ framework as one of the comparatively few frameworks adopting an explicitly analytical approach to systems analysis while also being applicable to micro-level health systems. The framework posits that health system performance is not mechanical, but the product of interactions between system ‘hardware’—defined as tangible or material resources in a health system, such as infrastructure, drugs, information systems and human resources—and system ‘software’—intangible components such as the values, power dynamics and norms that shape the decisions, behaviours and relationships of actors within the system. Critically, the framework emphasizes the mutually constitutive nature of the physical and material, and behavioural and relational components of a health system, for understanding its overall performance (K. Sheikh et al. 2011).
Study aims and design
The dual aims of this study were to document and characterize service operations in four Zambian health centre ‘micro-systems’ and to use (and adapt as needed) the Hardware–Software framework to explore how interactions between different health system components influenced overall health-centre performance.
In order to address these objectives we adopted a multi-case study design. Case-study research has explicit strengths in relation to ‘investigating the complex behaviours of, and relationships among, actors and agencies as well as for understanding how those relationships influence institutional change’ (Gilson 2012; Yin 2009). While much case study research focuses on a single case (chosen because of its unique or defining characteristics) we adopted a multi-case design using a theoretical replication strategy (Yin 2009). Cases were selected (as far as possible) to confirm or disprove, and subsequently explore the reasons underpinning, certain patterns of service delivery.
Four health centres, each representing a case unit, were chosen purposively from two districts within Lusaka Province, based on established (>36 months) HIV care and treatment service1 and a catchment population characterizing the health centre as either a large urban facility (>100 000), small urban facility (40 000–70 000), peri-urban facility (<40 000) or rural facility (<30 000), respectively. A list of all facilities in the Districts that fitted selection criteria was initially developed and case selection was conducted in collaboration with District Medical Officers (DMOs) and local colleagues accounting for both logistical issues and accessibility. Final selection was subject to the informed consent of each health centre in-charge.
Data collection
Data were collected between June and December 2011 from multiple sources in each facility. Table 1 details the principles used to frame each study phase and Table 2 summarizes data collection and sampling approach for each method. Methods included in-depth interviews with a proportionate sample of health-care workers (HCW); semi-structured interviews with a quasi-random sample of patients; direct observation of facility operations (formal, using the National Healthcare Standards Assessment tool for Zambian Health Facilities, and informal using research memos to record observations) over several weeks at each site; key informant interviews with government and non-government officials, and a review of health centres’ routine (paper-based) health information registers.
Table 1.
Processes for ensuring rigour of case-study research
| Research Phase | Principles for Ensuring Rigour* | Methods Used in this Study |
|---|---|---|
| Design | Guiding conceptual theory or framework | Conceptual framework adapted from previous work of Sheikh et al. (2011), and theories of power and trust in health-care settings. Theory used in case selection triangulation (see below). |
| Data collection | Justified Case selection | Four health centres selected based on assumptions that interaction between system hardware & software will differ for health centres in urban, peri-urban and rural settings. Selection of centres from single province was based on timing of HIV service scale-up. |
| Multiple methods | For each health centre: key informant interviews with staff; in-clinic observations; patient interviews; interviews with administrators and implementing partners. | |
| Sampling | Smaller health centres included interviews with all staff & approximately 45 patients. | |
| Larger health centres included interviews with representative sample of staff from each dept & approximately 45 patients. | ||
| Prolonged engagement | Case: 2-3 weeks in each facility. | |
| Respondents: At least one formal interview with respondents and informal engagement over several weeks pre-/post-interview. | ||
| Analysis | Triangulation | Within case: Initial case reports based on triangulation across all data sets for each case (critical comparison of observation & interview findings), generating overall judgements about facility-wide experience & notes on variation in health-centre cases. |
| Cross-case: Initial case reports generated to look for common and differing experiences across sites, and subsequently compared with theory to assess convergence or divergence. | ||
| Negative Case analysis | Within case: Identification of experiences that contradicted initial assumptions, drawing on notes from initial case-data triangulation. | |
| Across-case: cross-case analysis to compare negative cases and test initial assumptions underpinning the study. | ||
| Peer Debriefing & Support | Preliminary case reports reviewed by four colleagues (non-government, government & community-sector) working in Zambian health sector. | |
| Respondent validation | Preliminary cross-case analysis presented for review and comment to select respondents (clinic managers and provincial officials); feedback incorporated into final analysis. |
*Source: Gilson et al.(2011).
Table 2.
Summary of data collection and sampling at four health centres
| Method | Source | Sampling Approach | Rationale for Data Collection | Number Conducted |
||||
|---|---|---|---|---|---|---|---|---|
| HC1 | HC2 | HC3 | HC4 | All | ||||
| Document review | Health centre records | Purposive | Contributed to building a picture of day-to-day health centre operations and to supplement interview data in relation to the decisions and actions involved in establishing HIV care and treatment services at the primary level. | n/a | n/a | n/a | n/a | n/a |
| Direct observations | Facility audit | – | Designed to provide a snap-shot of physical, material and administrative structures in place. Conducted with facility in-charges. | 1 | 1 | 1 | 1 | 4 |
| Unstructured Observations & Research memos | 2 weeks per facility | Contributed to building a picture of typical workflows and human interactions that influenced health centre operations. Provided important data to supplement structured health centre audit and direct observation of patient visits. | 3 wks | 2 wks | 2.5 wks | 2 wks | n/a | |
| Structured Observations of Patient Visits | Proportional, quasi-random sample | Provided evidence of the actual care pathways and waiting times involved and the nature of patient–provider interactions across all major departments. This evidence provided a quantifiable basis for comparing patient and provider perceptions of health centre service operations | 47 | 48 | 46 | 44 | 185 | |
| Interviews | Health Providers | Proportional from all health centre departments | Interviews were built around four major themes; (1) providers’ role in the health centre, their typical routine, and their position in relation to others in the facility; (2) the challenges faced in day-to-day work; (3) perceptions of the work patterns and work culture in the facility, including the role of health centre managers; (4) their understanding of, and attitudes towards, the introduction of HIV services. | 23 | 8 | 16 | 17 | 64 |
| Patients | Proportional quasi-random | Questions were designed to provide an insight into the patient’s reasons for attending the clinic, their perceptions about what happened during the visit, their understanding of processes and relationships driving service delivery, and how provider behaviour & services met their expectations. | 47 | 48 | 46 | 44 | 185 | |
| Non-government (NGO) & District officials | Purposive & name generation | Interviews covered respondent’s perceptions about primary-level health centre functionality generally, and where relevant, participants were asked to describe their role in, and perceptions of, the introduction of HIV care and treatment services. Interview questions were designed to facilitate a reconstruction of the activities that took place in the process of implementation, the way relationships within the team and at the clinic evolved, and how actual implementation varied from the plans. Respondents from NGOs were probed about their role in, and perceptions of, health centre service systems and how they interacted with these systems during implementation. Zambian officials were questioned about activities and decisions that shaped planners’ approach to HIV service implementation, their understanding of, and assumptions about existing health centre systems, and the degree to which they considered (a priori) the interaction between HIV services and current health centre operations. | n/a | n/a | n/a | n/a | 13 | |
| Archival | Health management information system (HMIS) Data | Register Audit | HMIS data were initially intended to provide a quantitative basis for evaluating the impact of new HIV services on non-HIV service functions. However, clinic observations and archival review revealed significant gaps / inconsistencies in HMIS data, making it difficult to use as a valid basis for assessing quality or coverage. In final analysis, information was used to reflect on the approach to gathering/transmitting routine health information and implications of this approach for mechanisms of accountability. | 1 | 1 | 1 | 1 | 4 |
Written informed consent was obtained from all participants (patients, providers and key informants) for any observations or interviews. The study received ethical clearance from the Human Research Ethics Committee of the University of Melbourne (REF #: 1035194) and the University of Zambia Biomedical Research Ethics Committee (REF #: 004-03-011).
Analysis
Analysis was carried out in three phases. Phase one was conducted concurrently with data collection, as collated notes and summaries of evidence were generated for each health centre. Transcribed interviews were imported into NVivo QSR™ for electronic coding. In phase two, data were organized to produce a case description for each health centre (Yin 2009). Qualitative and observational data were synthesized and compared in order to develop as comprehensive a picture as possible of the operational reality at each site. This phase included comparison and cross-checking of all data to generate cohesive and consistent case descriptions and to identify unusual or exceptional experiences. Preliminary case descriptions were disseminated to the health-centre managers and DMOs to garner feedback. Phase three focused on cross case comparisons using both deductive and inductive analysis. Deductive analysis was guided by codes developed from the conceptual framework including: system hardware—financing, governance and human resources; system software—leadership, workplace norms and patient expectations; accountability—incorporating mechanisms for and responses to transparency, justifiability and enforcement. Coded text and its (anonymized) source were collated in a word document and printed to enable synthesis of major findings relating to hardware–software interactions and their impact on mechanisms of effect within the health centres. Theoretically generated codes were compared and commonalities identified across the four cases. Negative case analysis was conducted through the identification of experiences or interactions that appeared to contradict the theoretical assumptions underpinning this study. Results and discussion presented in this article draw most heavily on in-person observations and provider interviews, but are critically informed by patient and key informant interviews as well.
Results
Findings from this study are presented in three sections. The first section provides a summary profile of the four health centres, evidence of the common service characteristics across the four sites and the elements of system hardware and software identified as influential in shaping these characteristics. In the second section we discuss the adaptation of the Hardware–Software framework to take account of the findings in the preliminary analysis. Finally, we present findings from an analysis that used the adapted framework to explore in greater depth the way hardware/software interactions influenced mechanisms of effect in the health centres, and through this, overall service performance.
Service profiles
Evidence from our case-data shows that each health centre had a distinct combination of structural, organizational, relational and cultural components that produced some differences in style and quality of care between and within the four sites. Table 3 summarizes each health centre’s structural and demographic information and, based on various data sources, provides a summary description of each facility's infrastructure and environmental health, service operations, stewardship and patient provider relationships.
Table 3.
Health centre demographic information
| Demographic features a | Health centre 1 | Health centre 2 | Health centre 3 | Health centre 4 |
|---|---|---|---|---|
| Designation | Urban | Rural | Urban | Peri-Urban |
| Official catchment | 62,579 | 15,000 | 101,972 | 43,850 |
| Official opening hours | Day: 08:00–17:00 | Day: 08:00–17:00 | Day: 08:00–17:00 | Day: 08:00–17:00 |
| Night: 17.30–07.30 | Night: 17.30–07.30 | Night: 17.30–07.30 | Night: 17.30–07.30 | |
| Service departmentsc | OPD, MCH, TB, HIV, LAB, EH | OPD, MCH, TB, HIV, IPD, LABOR LAB, EH | OPD, MCH, TB, HIV, LAB, EH | OPD, MCH, TB, HIV, IPD, LABOR, LAB, EH |
| Number of Professional staff | 41 | 5 | 46 | 22 |
| Number of Lay staff b | 29 | 5 | 46 | 12 |
| Operational characteristicsa | Health centre 1 | Health centre 2 | Health centre 3 | Health centre 4 |
| Infrastructure & environmental health | Lack of space—rooms frequently multi-tasked; OPD with broken taps; lack of patient privacy in OPD/TB/MCH; lack occupational safety especially with sharps. | Generally good space; frequent power-cuts & new generator not in operation; OPD pit-latrines out of use; lab shut because of sink blockage. | Run-down infrastructure and severe overcrowding in all departments; lack of patient privacy; taps/sewerage system functional; adequate occupational safety standards. | Adequate space and ventilation throughout; functional taps and sewerage; high occupational safety standards. |
| Service operations | Siloed departmental operations; weak communication systems; reliance on largely unsupervised lay personnel; frequent absenteeism; non-integrated record keeping; frequent OPD stockouts. | Severe HR shortages; semi-harmonized depts; good inter-cadre communication; but lack of up-to-date clinical training & substantial task shifting; non-integrated medical records; frequent OPD stock-outs. | Large cadre of professional staff but absenteeism frequent; strong, multi-functional lab system; high standards in TB dept; reliance on unsupervised lay staff to manage OPD/HIV files. | Comparatively well-harmonized inter-department operations & communication; weak (+missing) medical filing; functional laboratory; strong community involvement. |
| Stewardship | Various committees formed but are weak forums for active decision-making; facility in-charge largely focused on admin tasks; absence of strategic leadership; overall weak staff morale. | Flat structure with ‘team leader’ instead of ‘in-charge’; good team work but lack of strategic leadership or problem solving capacity. | Hierarchical and siloed management structure; varying morale, weaker in OPD/HIV, stronger in MCH and TB; strong administrative focus by managers & little proactive strategizing. | Very strong presence by overall in-charge with strategic vision and active planning; weaker departmental managers but ameliorated by strong facility-wide communication systems. |
| Patient–provider relations | Confrontational relations in OPD and HIV—patient complaints re. long waiting times and lack of HCW respect; greater mutual respect between patients and providers in TB (operated by lay staff member) and MCH (operated by midwives). | Confrontational relations in OPD, HIV, MCH—patient complaints re. long waiting times and lack of HCW respect. greater mutual respect between patients and providers in TB (operated by lay staff members). | Confrontational relations in OPD and HIV—patient complaints re. long waiting times and lack of HCW respect; greater mutual respect between patients and providers in TB (operated by nurses) and MCH (operated by midwives). | Confrontational relations in OPD, HIV and MCH—patient complaints re. long waiting times and lack of HCW respect. greater mutual respect between patients and providers in TB (operated by nurses). |
a At time of data collection between Jun. - Dec. 2011.
b Includes paid or stipendiary lay staff with a formal terms of reference; does not include ad hoc voluntary lay staff.
c OPD = outpatient department; MCH = maternal and child health department; TB = tuberculosis treatment department; HIV = human immunodeficiancy virus treatment department; IPD = inpatient department; LAB= laboratory; EH = environmental health department.
Health centre 1 (HC1) is an urban facility centrally located in one of the oldest residential and commercial areas of Zambia’s capital city. The facility comprises an OPD, MCH department, TB treatment department, HIV treatment department and a small in-house laboratory. At the time of study, running water was available, but not all rooms had taps and not all taps were working. Infrastructure was rundown in most departments and environmental health was poor, failing most checks against the National Healthcare Standards Assessment (NHSA) tool for Zambian Health Facilities. Observations and provider and patient interviews demonstrated a heavy emphasis on episodic and curative services. With the exception of the MCH department, little effort was put into preventive services and poor maintenance of medical records and registers limited the possibility of follow-up care. Both in-person observations and qualitative data from patient and provider interviews demonstrated that quality and responsiveness of care were strongest in the TB department and weakest in the OPD, where clinical consultations were cursory and short (averaging <5 minutes/patient in a quasi-random sample). Patient–provider relations in the OPD and HIV departments were also very tense, linked to patients’ perception that waiting times were too long and health workers inefficient. Reliance on ad hoc communication by facility management meant there was limited capacity to systematically address chronic performance issues. Overall, staff morale was low.
Health centre 2 (HC2) is located in a rural district of Lusaka Province with a catchment population of 15 000 and travel distances of up to 25 kilometres. HC2 incorporated an OPD, HIV, TB and MCH department, laboratory, IPD and labour ward. At the time of study, the facility had running water but the plumbing to the laboratory was blocked rendering it out of service. Additionally, pit latrines for outpatients were full and out of operation, requiring patients to defecate in an open field nearby. Power outages occurred regularly and a donor-funded generator was yet to be connected. Lack of staff and constant multi-tasking contributed to rapid and often sub-standard screening practices in the OPD, HIV and MCH departments. With the exception of the HIV department, medical records and attendance registers were poorly maintained. Inconsistent availability of laboratory services weakened the facility’s diagnostic capacity. Many routine tasks (e.g. prescription of antiretroviral therapy and dispensing of medications) were carried out by staff who lacked training. Health workers demonstrated comparatively strong teamwork but many expressed frustration related to weak support by District and Ministry officials.
Health centre 3 (HC3) is one of the largest primary health facilities in Lusaka with a catchment population of over 100 000 that is more than double the official ‘ceiling’ for an urban health centre (MOH and GRZ 2007). At the time of study the facility housed an OPD, IPD, MCH, TB and HIV department and a substantial in-house laboratory. Infrastructure was mostly over 50 years old and in poor repair, with the MCH, IPD, OPD and HIV departments all fairly cramped and poorly ventilated. Running water and pit latrines were available. MCH and TB services at HC3 were delivered in a comparatively timely and respectful manner with providers demonstrating strong rapport with patients. Observations of staff in the laboratory also demonstrated a strong sense of mission and internal systems designed to ensure effective use of limited resources. Within the partially integrated OPD and HIV departments, however, a strong professional cohort (full range of clinical staff) was undermined by weak internal co-ordination and poor integration of administrative and clinical processes.
Health centre 4 (HC4) is a peri-urban facility located on the northern periphery of Zambia’s capital city in an unplanned squatter settlement with no site-and-service water or electricity. Despite being considered a ‘small’ facility, the health centre comprises an OPD, HIV, TB and MCH department, IPD, labour ward and small in-house laboratory. At the time of study, running water was available but not all rooms had taps. Electricity failures were a daily occurrence with no generator back-up. While not exemplary, service delivery in HC4 was comparatively well integrated. Initiatives to harmonize patient identification, medical record keeping and patient care pathways improved continuity of care for OPD, HIV and TB patients and was supported by auxiliary workers providing ‘linkage services’. The recent (facility self-funded) renovation of an in-house laboratory strengthened HC4’s diagnostic capacity although this service was yet to be fully utilized by on-site clinicians who were used to making clinical diagnoses.
Despite some clear operational and contextual differences between the four health centres, the case descriptions revealed a set of service characteristics common to all facilities and linked to various common hardware/software interactions. Described in more detail in Table 4, these shared characteristics and the hardware/software interactions that influenced them included:
Weak continuity of care (influenced by structurally separate departmental organization and weak inter-cadre communication),
Sub-standard clinical practices (influenced by the high patient–provider ratios and lack of effective quality assurance mechanisms)
Skewed focus on curative services (arising from providers’ strong focus on episodic services and ‘clearing’ the queue and a general lack of orientation towards preventive care or patient self-management)
Confrontational relations between patients and providers (influenced by poor environmental conditions in the facilities and weak inter-personal trust)
Table 4.
Characteristics of service delivery and contributing factors
| Features of De Facto service delivery | Supporting evidence | Hardware factors (human resources, health information, drugs and equipment) | Software factors (values, norms, power relations) |
|---|---|---|---|
| Weak continuity |
|
|
|
| Sub-Standard clinical & administrative practices |
|
|
|
| Episodic care |
|
|
|
| Confrontational care |
|
|
|
An explicit aim of this research was to move beyond a simple list of contributing factors in order produce generalizable assertions about drivers of service quality in health systems. While the case descriptions were helpful in identifying some of the common factors, this analysis falls short of providing an analytical frame for understanding health system performance more generally. With the aim of developing a deeper understanding of how these hardware–software interactions influenced health centre performance we thus adapted Sheikh et al.’s (2011) framework (Figure 3) to incorporate more explicit mechanisms of effect that shape service delivery across the four sites.
Figure 3.
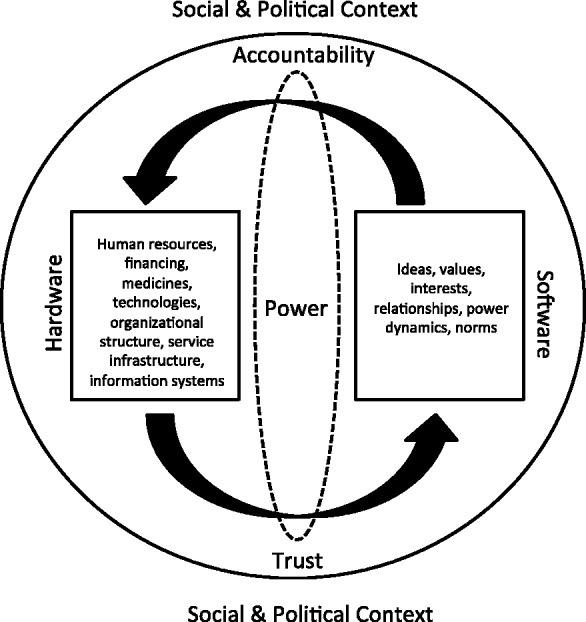
Conceptual framework for analysis of health micro-systems (adapted from Sheikh et al., 2011).
Based on our case analysis that demonstrated how provider behaviours and attitudes were a key determinant of service quality, and supported by a cross-disciplinary literature review, we came to focus on two mechanisms—those of accountability and trust—as central determinants of quality and responsive service delivery (Gilson et al. 2005; Rittenhouse et al. 2009). In this article we focus primarily on the findings in relation to accountability with future papers dedicated to an exploration of trust.
We adapted Brinkerhoff’s (2003, 2004) typology of accountability2 in order to focus more closely on two domains relevant to front-line health services; that is administrative and social accountability. Although both domains relate to provider performance, the former—administrative accountability—represents ‘upwards’ accountability to supervisors and managers with reference to established policies, guidelines and clinical standards. The latter—social accountability—represents ‘downwards’ accountability to meet the needs and expectations of patients and community members. While our larger analysis focused on both administrative and social accountability, this article (in the interests of brevity) focuses exclusively on administrative accountability.
Following Brinkherhoff, we understand administrative accountability to be the product of two interconnected mechanisms—answerability and enforceability. Mechanisms of answerability provide information that makes transparent and justifies the nature of health providers’ decisions or actions. Examples of such mechanisms include clinical performance reviews or routine data on service quality and coverage. Mechanisms of enforceability provide a form of reward or sanction when providers succeed or fail to meet these pre-defined standards (Brinkerhoff 2004) and in this setting may include disciplinary measures, performance incentives and so forth.
Overall, we theorized that dynamic interactions between system hardware and system software influence mechanisms of answerability and enforceability, and through these, the production of accountability (administrative and social) in each health centre as a whole (Figure 3). Based on our first round analysis, we also theorized that these mechanisms are mediated by the trust and power dynamics inherent to the relationships between actors within the health system—although this remains a secondary focus of this particular article. As with Sheikh et al.’s (2011) original, the adapted framework recognizes that health systems are open and social and subject to contextual influences from larger systems in which they are embedded and the broader social and political environments in which they operate.
Findings in relation to mechanisms of answerability
In the context of Zambian health-centre operations, effective mechanisms of administrative answerability should enable health-centre managers and/or District officials to request information about a provider or health-centre’s performance, and would ensure they were capable of, and willing to, supply that information. In the health centres in this study mechanisms of answerability included documentation of service activities in medical records, hard-copy registers and tally sheets, production of summary activity reports, and performance review and feedback from District administrators.
Data from our case findings indicated that, in general, mechanisms of administrative answerability were weak with a variety of hardware–software interactions contributing.
Perhaps the most significant hardware factor was the chronic human resource shortage experienced across all four sites. Staff shortages not only impeded the provision of quality services (directly undermining health workers’ capacity to make good on their service obligations) but also impeded the timely and accurate collection of health information about those services. Health-care workers interviewed in all four facilities described the time pressure they experienced and the impact this had on their clinical and administrative performance.
When you are examining 300 patients in five hours you are literally saying two [sic] minutes per patient. The patients can’t express themselves [in that time]; so you use what we call spotter diagnosis. You look at the patient and see, well, is he sick or not? Then you move on. Clinician, HC3
Lack of time to complete point-of-care data or summary reports led many professional HCW to delegate (‘task shift’) data-entry and data collation tasks to auxiliary staff. Some auxiliary workers were highly competent and demonstrated the capacity to take on these additional tasks quickly and efficiently. Others (such as the cleaner responsible for dispensing drugs to OPD patients in HC2) had weak literacy and almost no training and little capacity to maintain records. Auxiliary workers were receiving either very small stipends or no payment at all, and were required to take on informal responsibilities as well as completing the ‘core’ tasks for which they had been originally recruited. Structural human resource shortages (a hardware factor) thus contributed to a high burden of work and pressure to complete tasks quickly, which, compounded in some cases by lack of capacity, contributed to data-entry errors, shortcuts or shirking of these duties altogether.
Exacerbating staff shortages, the cumbersome nature of the hard-copy data-collection tools added to time pressures that affected both clinical and administrative standards. Tally sheets and health-centre registers, for example, involved complicated and sometimes repetitive entries that were frequently difficult to interpret. Where official registers were available, both professional and auxiliary staff complained that data entry was overly time-consuming (Filling those tally sheets is complicated and just takes time; so we would prefer to concentrate on the next patient. Clinician, HC3). During the period of study, moreover, HC1 and HC2 were observed to lack several up-to-date registers, resulting in temporary and improvised data collection tools that did not mirror official documents.
Observations and interview findings demonstrated that monthly reports collated from health-centre registers were generally compiled hastily and with few, if any, quality checks. As one nurse observed: after we compile our report we don’t sit down to say: ‘was it done correctly?’ or ‘what does it tell us?’ Everybody just does their own report [and] someone hands it to the District. (Nurse, HC2). The poor quality of data entry and reporting undermined providers’ answerability to District officials. The ad hoc and often impersonal nature of the performance reviews further weakened the efficacy of this mechanism. While some providers (e.g. HC1, 3) described performance reviews in a positive light (we can see our strengths and our weaknesses; Nurse, HC3), many others complained that they were unhelpful: because by the time you get it you will have forgotten what they are reporting on; Nurse; HC4.
Findings in relation to mechanisms of enforceability
In the context of primary health-centre operations, effective mechanisms of administrative enforceability should enable health-centre managers or District administrators to invoke positive rewards for good performance, or sanctions for inappropriate behaviour or poor performance. In the Zambian context, we found that there were comparatively few formal mechanisms of enforceability. Poor performance of any sort could be disciplined via a formal system of written warning letters issued by an overall in-charge and referred upwards through the District, Provincial and Ministry administration. However, the bureaucratic nature of this sanction meant that formal decisions could take months and as one in-charge explained:
The Ministry system […] can be quite difficult because you have civil service rules, where to give warnings everything goes in written form. It’s not you who can [act on the problem]. You have to recommend. Then the recommendation goes to [the District] and then to the Province, and then [the Ministry of Health]. It takes forever and ever. Now you can suspend a few people but even then it’s tedious. And to fire is even more difficult. In-Charge, HC3
A second formal mechanism of enforceability was the use of horizontal transfers either within, or between, health centres. Transfers were described by one District official as a pre-emptive mechanism to ‘keep health care workers on their toes’ District Official, as well as a sanction used on those not performing to standard. Yet as another official noted: ‘we have those transfers […] but then the transfer does not change the health-care worker. They take their problems to the new place and infect it too’; District Official. Continued reliance on such highly centralised and weakly regulated sanctions constituted an ongoing impediment to enforceability within these clinics.
We identified no formal mechanisms to reward strong performance, although some in-charges described their own improvised mechanisms of reward, such as approving informal (non-recorded) days-off on the implicit agreement that professional staff would work harder on their remaining rostered shifts (HC4).3
Beyond the limited formal disciplinary sanctions, weak enforceability in the four health centres was also influenced by software factors including the power dynamics between different health worker cadres and the leadership qualities of various in-charges. Findings indicated that in all four facilities there was a tension between the administrative hierarchy (from which in-charges drew their authority) and the medical hierarchy in which clinicians, based on their more prestigious training, were senior. In all but one of the health centres (HC4) the overall in-charge was a registered nurse and implicit tension was evident in the comments of several clinical officers regarding the competency of their administrative superior.
You know ideally, the administration of clinics is supposed to be done by the clinical officers, [because] we know how to run a clinic. Apart from administration, we know how to deal with the community. And we can mobilise people that are influential, politicians for instance. Nurses have no training for that Clinician, HC3.
Such tensions undermined in-charges’ authority (albeit to varying degrees), making it more difficult for nurse managers to bring sanctions to bear on providers above them or on equal standing in the medical hierarchy (I was hoping that the Clinical Officer would come back before I write [to the District] … this is the third week [she has been absent] without a reason; In-Charge HC3/With respect to leading […] the challenges are there in every aspect, especially if you are not a doctor. You have to be tactical; EHT, HC2).
Weak leadership skills constituted an additional barrier to administrative enforceability. Although the in-charges interviewed in this study were clearly well intentioned, many lacked the capacity or where with all to enforce performance standards among their frequently disaffected staff. Direct observation in all sites demonstrated that most managers focussed their energy on administrative functions such as creating staff rosters and monthly reports while performance-related issues were often deferred or, where possible, referred to the next level of authority (There are certain challenges with the [but] it’s incredibly difficult and usually I hand over to my [supervisor]; Dept. In-Charge HC4).
Weak capacity to lead or affect attitudinal change was manifest in various in-charges’ descriptions of their interaction with their staff. In all four sites, for example, departmental in-charges reported how some professional staff would only perform to standard if their supervisor was physically present (They expect me to be there, my actual presence, to say ‘do this, do this, like this’. If I’m not there in person, well […]; Dept. In-Charge, HC2). Others described cases where professional staff had threatened poor performance or absenteeism if they were criticized by their superiors (When you are good, [your staff] also become good. But if you are harsh and criticize them, they are also harsh. They will come in late or just take sick days to punish you as the in-charge; Dept. In-Charge, HC3).
Moreover, many departmental and overall in-charges expressed a sense of hopelessness in relation to holding their staff accountable (they always have excuses, so there is nothing you can do. There is nothing I can do; Dept. In-Charge, HC4) with several describing how they adopted consciously liberal approach to enforcing performance standards in order to cope (They just don’t care. And you can’t make them; In-Charge HC4/ You just have to understand they are human beings; they have got their own personal programs they need to attend to; In-Charge, HC1).
Previous research has demonstrated that facility-level oversight or regulatory capacity can be weakened where material and human resource constraints are already a factor (Bloom and Standing 2008). While such hardware factors were certainly a consideration in this setting, the quality and capacity of individual in-charges remained a distinct factor, as a district official noted: the in-charges, they are the managers of these health facilities. But it’s not [all of them] who have that leadership skill. Some only rise up just because they are the most senior; District Official.
This interpretation is supported by two exceptions to the more general finding of weak leadership identified in this study and outlined in Box 1. These examples provide insight into the way strong(er) leadership, as oppose to formal disciplinary mechanisms, may influence the production of accountability by appealing to providers’ service-values. The exceptional leadership in HC4 also demonstrates how accountability may be effectively enforced even in systems that are otherwise generally weak.
BOX 1. Strong leadership.
- Example 1: A former overall in-charge at Health Centre 2 was described by both professional and auxiliary staff as an unusually strong leader with ‘strategic’ capacity.
- The [former in-charge] was unusual. […] He was very creative, very tactical and he wanted to do things in the right way. He was a motivator […] everyone liked him very much. Environmental Health Technologist, HC2
- He was tough, but kind and intelligent. He was tough, in the sense that, whatever he wants done, he wants it done. If you were assigned to do something and you did not do it, you would not be on good terms with him. But even then, he used to find out why you didn’t do it and he would help you. He might be annoyed, but at the end of the day he would still come back to you and help you finish. Lay Counsellor, HC2.
- Example 2: The overall in-charge at Health Centre 4 displayed a strong commitment to hands-on leadership and an ability to overcome the ineffectual formal sanctions through active and persuasive communication. This was illustrated in the account of a laboratory technologist who described how the overall in-charge dealt with the reticence of clinical officers to make use of the clinic’s new laboratory facilities.
- When the [clinicians] were not sending any patients to the lab [because they were used to conducting one-off clinical assessments] the in-charge was on his feet trying to sensitize members of staff to use the lab. He was preaching every day and now it’s getting there, they’re starting to shift. Lab Tech, HC4.
A culture of impunity
Brinkerhoff (2003) notes that the ‘ability of overseeing actor(s) to impose punishment […] for failures and transgressions [is what] gives ‘teeth’ to accountability’. He asserts, moreover, that the presence of de jure sanctions without the de facto capacity to enforce them may diminish or lead to a general failure in administrative accountability, contributing to a series of work norms that underpin a ‘culture of impunity’. Work or social norms are expectations shared by members of a group about appropriate ways to behave in given situations (Marshall 2009). They represent the potential pressure or expectations that form the basis of decisions about how to behave or interact and provide a yard-stick or referent for members of a group to assess themselves. In the sense that norms may increase (in both positive and negative ways) feelings of personal and group identity, research has demonstrated how they help shape health providers’ behaviour by providing limits within which individuals receive social approval (or at least avoid overt disapproval) (Dabney 1995; Ehrhart and Naumann 2004).
In the four health centres in this study, we found evidence of three particular service patterns underpinned by permissive work norms that permeated the health centre setting.
The first was laxity in relation to clinical and administrative standards. This included avoidance of measuring patients’ vital signs (HC1, 2, 3), repackaging of bulk-delivered drugs into single-dose packets without counting the dose (HC 1, 3, 4) and clinicians skipping physical examinations (HC1, 2, 3, 4). These short cuts and omissions were linked to a second work pattern—queue clearing—characterized by rapid consultations in which providers aimed to ‘clear’ patient queues as quickly as possible in order to be able ‘to relax and refresh a bit’; Midwife, HC2, or, to leave the clinic altogether.
A third work pattern suggestive of permissive work norms and a culture of impunity was the frequency of absenteeism. The most common form of absenteeism was tardiness, including late arrival and early departures from work. In the urban and peri-urban facilities (HC1, 3, 4) providers’ linked their tardiness with ‘moonlighting or ‘double shifting’ and justified these behaviours as a way of supplementing their income (we don’t just depend on this clinic, we have to do other part time [jobs]; Nurse HC1). Providers linked their need to take on additional work to poor public sector salaries and benefits (when you calculate for a month, then you get a small salary, that can’t even sustain you; Clinician, HC3 / The way we are working is not OK. There are no uniforms, no transport refund, and people get to work late because of that; Nurse, HC4). In the rural facility (HC2), there were few opportunities to moonlight, but direct observation demonstrated that professional staff nonetheless operated significantly shorter (daytime) hours than the official schedule. In this rural setting the perception of overwork and the need to rest and recuperate were the primary justifications for foreshortened hours.
Another common type of absenteeism was duty station absence, most frequently observed in the larger departments (OPD, HIV) in the urban and peri-urban facilities (HC1, 3, 4). During interviews, providers attributed their duty station absences to the constant pressure to multi-task. While this pressure was real, some providers deliberately took advantage of the scattered nature of their work. In HC3, for example, five nurses were routinely allocated to the OPD during the morning, but during four separate observed morning shifts, between one and three of these nurses were absent from their duty station by mid-morning and subsequently located in the staff lounge. Clinical officers and/or the doctor working in the OPD in HC3 were also observed to be absent from their station on six occasions across the study period, five of which were afternoon shifts. In both HC1 and HC4, a number of nurses working in the outpatient and HIV departments during the afternoon shift were observed absent from their duty stations, later to be located in the pharmacy (nominally counting medication into packages). Such practices were not one-off occurrences, but represented consistent work patterns underpinned by permissive work norms.
Discussion
This study contributes to the limited body of theoretically informed empirical work exploring mechanisms of effect at the micro-level in low-resource health systems.
Challenging the implicit assumptions of more reductionist health system frameworks, our findings illuminate the complex, social and adaptive nature of micro-level health systems and demonstrate the usefulness of combining Sheikh et al.’s (2011) hardware–software model with a typology of accountability in order to explain how and why primary-level health services perform (or under-perform) under certain conditions.
The quality and responsiveness of service delivery within primary-level health facilities are demonstrably influenced by mechanisms of accountability, which are in turn influenced by a range of hardware–software interactions. In the case of the four health centres in this study, structural constraints such as limited material and human resources (system hardware) created incredibly difficult service environments for health workers in which work overload and resource shortages were common.
In many health systems, including Zambia’s, hardware factors such as human resourcing, health financing and drug and procurement systems lie largely beyond the control of front-line providers. This challenge is reflective of ‘principal-agent’ issue discussed in health related accountability literature (Brinkerhoff and Bossert 2008; Buchanan 1988; Smith et al. 1997) in which state actors cannot be held fully responsible for performance due to the hierarchy and multiple levels of delegation that impede decision-making and/or action. Indeed, providers in this study emphatically described the locus of control for their own and their health centres’ wider performance as being largely external, making assertions such as ‘we have no option’ when it came to delivering sub-standard care.
Despite this, our findings clearly demonstrate the way providers’ personal choices and actions also influence service quality and responsiveness. Providers’ frustration with poor work conditions, for example, interacted with widespread dissatisfaction with salary levels to erode service-values and act as a catalyst in many individuals’ decision to seek other forms of compensation (moonlighting) or to foreshorten work hours. Such behaviours, in turn, exacerbated the high patient–provider ratios and increased the frequency of clinical and/or administrative shortcuts.
In both Sheikh et al.’s original Hardware–Software model and our adaption, it is theorized that values and norms play an important role in health system performance. Our findings confirm that, inter-cadre tensions aside, providers’ almost universally identified as ‘overworked public service health providers’. Based on a common understanding of certain practices (notably various forms of absenteeism) as a form of compensation for the real or perceived work pressures associated with this role, certain work patterns became accepted norms within the health-centre settings irrespective of the fact that these practices ran counter to providers‘ service mission. Weak health information systems produced little useful performance data to expose these work patterns, while facility managers—who were well aware of the problem— generally lacked the power or the leadership skills to challenge them.
Despite having little power to shape the formal organizational structure or environmental conditions of their work place, providers were thus able to exercise considerable influence over service quality and responsiveness via work norms that constituted a source of ‘hidden’ power. The consistency of the data in relation these findings, as well as the authors’ experience in other facilities around Zambia, suggest that these work norms are likely influencing the ethos and service patterns of the Zambian public health sector at large.
Policy implications
Traditionally, primary-level service interventions in LMIC have tended to focus on elements of system ‘hardware’—most notably through training or similar ‘up-skilling’ programmes or allocations of new resources. Confirming a basic hypothesis of our conceptual framework, which emphasizes the social and adaptive nature of health systems, our findings demonstrate that system software such as work norms and providers’ service values play an equally important role in determining health-centre performance.
The importance of health system software has long been a focus of research in high-income settings, notably in the organizational management and quality improvement literature. What our findings highlight, is that far more work must be done to ensure that interventions in LMIC are equally holistically developed in order to take explicit account of the social adaptation and responsivness of human actors in these systems. This is particularly important to avoid ‘blaming’ software factors for performance breakdowns, when structural conditions play such a central role in shaping the conditions for such failures.
Our findings point to specific opportunities in the Zambia setting vis-à-vis strengthening mechanisms of answerability and enforceability. These include stronger production, analysis and flow of both health and service information enabling individual performance review, decentralized disciplinary mechanisms and greater investment in facility-level leadership capacity.
Analytical and methodological considerations
The approach to health systems analysis adopted in this research makes explicit reference to the context-specificity. Since every context, by definition, is unique, it could be argued that the findings presented here are specific to the experience of the four health centres. We have sought to address this limitation by presenting data specific to each case and the Zambian setting separately from the theoretical discussion, to allow readers to more easily assess the relevance of the examples in this study to their own or other settings. To the extent possible, we tried to maintain a distinction between the context specific analysis that addressed the study’s ‘how’ and ‘why’ questions on the one hand, and theoretical insights related to health system performance more generally.
We acknowledge that the research team’s disciplinary and professional background (including significant prior experience working in Zambian health centres) represents a potential source of bias that may have predisposed the team to understand and analyse certain issues in certain ways. However, this experience also provided specific advantages, including a deeper understanding of the context in which the health centres were operating and the complex and often apparently paradoxical nature of providers’ and patients’ actions, decisions and relationships.
Although beyond the scope of this particular analysis, more detailed examination of the role that power dynamics and various forms of trust have on the production of accountability in this setting, is also warranted. Such research could contribute substantially to the development of context-appropriate interventions to strengthen behavioural and relational components of health-centre operations. (Gilson 2003; McPake and Mills 2000).
Conclusion
Strong health systems are critical not only for delivering health services to those who have fallen ill (often the most vulnerable in society) but also for providing redress to deeply embedded social inequities (Freedman et al. 2005). Within health systems of LMIC such as Zambia, primary health centres represent the most basic type of formal health care. Understanding how and why such services operate is critical to providing guidance in relation to strengthening their performance in the long term.
Resonating strongly with the hypothesis that local health systems should be understood as complex and adaptive in their own right this study revealed many otherwise hidden dynamics and interactions that shaped health-centre performance. The findings confirm the relevance of the Sheikh et al.’s (2011) hardware–software model and demonstrates how the original framework may be adapted to achieve greater analytical and explanatory power by examining first, the way hardware–software interactions act positively or negatively on particular mechanisms of accountability, and through these, health system performance. The study constitutes an important contribution to the field of health policy and systems research, generating findings that may act as a building block within this still emerging field and be replicated and further tested in other settings.
Acknowledgements
The authors would like to thank the health-care workers, patients and district officials interviewed during this research for their willing participation and time given. S.M.T. would like to thank the Nossal Institute for Global Health at the University of Melbourne, Australia, and Associate Professor Jim Black and Dr Martha Morrow for their support.
Footnotes
1 Since one of the study’s overall goals was to assess the impact of introducing HIV services into primary health centres, this was a necessary criteria.
2 Brinkerhoff refers to these domains as ‘performance’ and ‘political’ accountability respectively with his analyses focusing largely on macro-level accountability of governments to their citizens.
3 Unfortunately this mechanism resulted in even worse provider-to-patient ratios with the perverse outcome of increasing the pressure on staff to engage in ‘queue clearing’ and shortcuts, effectively undermining the reason for the incentive in the first place.
Funding
This work was supported by an Australian Post Graduate Award for Doctoral Research, through the University of Melbourne, Australia. The funders had no influence over the subject matter or reporting of this study.
Conflict of interest statement. None declared.
References
- Bassett MT, Bijlmakers L, Sanders DM. Professionalism, patient satisfaction and quality of health care: experience during Zimbabwe's structural adjustment programme. Social Science & Medicine. 1997;45:1845–52. doi: 10.1016/s0277-9536(97)00122-6. [DOI] [PubMed] [Google Scholar]
- Bloom G, Standing H. Future health systems: Why future? Why now? Social Science & Medicine. 2008;66:2067–75. doi: 10.1016/j.socscimed.2008.01.032. [DOI] [PubMed] [Google Scholar]
- Brinkerhoff DW. Accountability and Health Systems: Overview, Framework, and Strategies. Bethesda: 2003. Partners for Health Reform Plus, Abt Associates Inc. [Google Scholar]
- Brinkerhoff DW. Accountability and health systems: toward conceptual clarity and policy relevance. Health Policy & Planning. 2004;19:371–9. doi: 10.1093/heapol/czh052. [DOI] [PubMed] [Google Scholar]
- Brinkerhoff DW, Bossert TJ. Bethesda: Health Systems 20/20; 2008. Health governance: concepts, experience, and programming options. [Google Scholar]
- Buchanan A. Principal/agent theory and decision making in health care. Bioethics. 1988;2:317–33. [PubMed] [Google Scholar]
- Dabney D. Workplace deviance among nurses. The influence of work group norms on drug diversion and/or use. J Nurs Adm. 1995;25:48–55. doi: 10.1097/00005110-199503000-00009. [DOI] [PubMed] [Google Scholar]
- Das A. Ensuring quality of care in sterilisation services. Indian Journal of Medical Ethics. 2004;1:79–80. doi: 10.20529/IJME.2004.041. [DOI] [PubMed] [Google Scholar]
- De savigny D, Adams T. Systems Thinking for Health Systems Strengthening. Geneva: World Health Organization; 2009. [Google Scholar]
- Ehrhar MG, Naumann SE. Organizational citizenship behavior in work groups: a group norms approach. Journal of Applied Psychology. 2004;89:960–74. doi: 10.1037/0021-9010.89.6.960. [DOI] [PubMed] [Google Scholar]
- Freedman LP, Waldman RJ, De pinho H, et al. Transforming health systems to improve the lives of women and children. Lancet. 2005;365:997–1000. doi: 10.1016/S0140-6736(05)71090-4. [DOI] [PubMed] [Google Scholar]
- Fulop N, Allen P, Clarke A, Black N. Issues in studying the organisation and delivery of health services. In: Fulop N, Allen P, Clarke A, Black N, editors. Studying the Organisation and Delivery or Health Services. London: Routledge; 2001. [Google Scholar]
- Gilson L. Trust and the development of health care as a social institution. Social Science & Medicine. 2003;56:1453–68. doi: 10.1016/s0277-9536(02)00142-9. [DOI] [PubMed] [Google Scholar]
- Gilson L, editor. Health Policy and Systems Research: A Methodology Reader. Geneva: World Health Organization; 2012. [Google Scholar]
- Gilson L, Daire J. Leadership and Governance within the South Africa Health System. In: Padarath A, English R, editors. South African Health Review 2011. 2011. http://www.hst.org.za/publications/south-african-health-review-2011, accessed 23 July 2013. Durban: Health Systems Trust. [Google Scholar]
- Gilson L, Kalyalya D, Kuchler F, et al. Strategies for promoting equity: experience with community financing in three African countries. Health Policy. 2001;58:37–67. doi: 10.1016/s0168-8510(01)00153-1. [DOI] [PubMed] [Google Scholar]
- Gilson L, Palmer N, Schneider H. Trust and health worker performance: exploring a conceptual framework using South African evidence. Social Science & Medicine. 2005;61:1418–29. doi: 10.1016/j.socscimed.2004.11.062. [DOI] [PubMed] [Google Scholar]
- Gormley W, Mccaffery J, Quain EE. Moving forward on human resources for health: next steps for scaling up toward universal access to HIV/AIDS prevention, treatment, and care. Journal of Acquire Immune Deficiency Syndrome, 2011;57:S113–5. doi: 10.1097/QAI.0b013e31821e9320. [DOI] [PubMed] [Google Scholar]
- Jesani A. Ethics, rights and strike of health workers. Issues Med Ethics. 1998;6:73, 103. [PubMed] [Google Scholar]
- Jewkes R, Abrahams N, Mvo Z. Why do nurses abuse patients? Reflections from South African obstetric services. Social Science & Medicine. 1998;47:1781–95. doi: 10.1016/s0277-9536(98)00240-8. [DOI] [PubMed] [Google Scholar]
- Komatsu R, Low-beer D, Schwartlander B. Towards Universal Access: Scaling up the Priority HIV/AIDS Interventions in the Health Sector. Progress Report Global Fund-supported programmes contribution to international targets and the Millennium Development Goals: an initial analysis. Bullettin of World Health Organization. 2008;85:805–11. doi: 10.2471/BLT.06.038315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobis S, Mbaruku G, Kamwendo F, Mcauliffe E, Austin J, De pinho H. Expected to deliver: alignment of regulation, training, and actual performance of emergency obstetric care providers in Malawi and Tanzania. Int J Gynaecol Obstet. 2011;115:322–7. doi: 10.1016/j.ijgo.2011.09.008. [DOI] [PubMed] [Google Scholar]
- Maestad O, Mwisongo A. Informal payments and the quality of health care: mechanisms revealed by Tanzanian health workers. Health Policy. 2011;99:107–15. doi: 10.1016/j.healthpol.2010.07.011. [DOI] [PubMed] [Google Scholar]
- Marshall G. In: A Dictionary of Sociology. 3rd. Scott J, Marshall G, editors. Oxford: Oxford University Press; 2009. [Google Scholar]
- Mcauliffe E, Daly M, Kamwendo F, et al. The critical role of supervision in retaining staff in obstetric services: a three country study. PLoS One. 2013;8:e58415. doi: 10.1371/journal.pone.0058415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcpake B, Mills A. What can we learn from international comparisons of health systems and health system reform? Bulletin of World Health Organization. 2000;78:811–20. [PMC free article] [PubMed] [Google Scholar]
- MOH, GRZ. Zambia Health Facility Census Analytical Report. Lusaka: Ministry of Health, Government of the Republic of Zambia; 2007. [Google Scholar]
- Mulley A, Wennberg J, Weinstein J, Fisher E, Binagwaho A. Embracing delivery science for universal health coverage. Lancet. 2013;382:25–6. doi: 10.1016/S0140-6736(13)61523-8. [DOI] [PubMed] [Google Scholar]
- Nolan T, Angos P, Cunha AJ, et al. Quality of hospital care for seriously ill children in less-developed countries. Lancet, 2001;357:106–10. doi: 10.1016/S0140-6736(00)03542-X. [DOI] [PubMed] [Google Scholar]
- Ooms G, Brolan C, Eggermont N, et al. Universal health coverage anchored in the right to health. Bullettin of World Health Organization. 2013;91:2–2A. doi: 10.2471/BLT.12.115808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peabody JW, Taguiwalo MM, Robalino DA, Frenk J. Improving the Quality of Care in Developing Countries. 2006 [PubMed] [Google Scholar]
- Pfeffer J, Veiga JF. Putting people first for organizational success. The Academy of Management Executive, 1999;13:37–48. [Google Scholar]
- Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care–two essential elements of delivery-system reform. N Engl J Med. 2009;361:2301–3. doi: 10.1056/NEJMp0909327. [DOI] [PubMed] [Google Scholar]
- Rowe AK, De savigny D, Lanata CF, Victora CG. How can we achieve and maintain high-quality performance of health workers in low-resource settings? Lancet. 2005;366:1026–35. doi: 10.1016/S0140-6736(05)67028-6. [DOI] [PubMed] [Google Scholar]
- Schneider H, Blaauw D, Gilson L, Chabikuli N, Goudge J. Health systems and access to antiretroviral drugs for HIV in Southern Africa: service delivery and human resources challenges. Reprod Health Matters. 2006a;14:12–23. doi: 10.1016/S0968-8080(06)27232-X. [DOI] [PubMed] [Google Scholar]
- Schneider H, Gilson L, Ogden J, Lush L, Walt G. Health systems and the implementation of disease programmes: case studies from South Africa. Global Public Health. 2006b;1:49–64. doi: 10.1080/17441690500361083. [DOI] [PubMed] [Google Scholar]
- Schneider H, Hlophe H, Van rensburg D. Community health workers and the response to HIV/AIDS in South Africa: tensions and prospects. Health Policy & Planning. 2008;23:179–87. doi: 10.1093/heapol/czn006. [DOI] [PubMed] [Google Scholar]
- Schneider H, Lehmann U. Lay health workers and HIV programmes: implications for health systems. AIDS Care. 2010;22:60–7. doi: 10.1080/09540120903483042. [DOI] [PubMed] [Google Scholar]
- Schneider H, Palmer N. Getting to the truth? Researching user views of primary health care. Health Policy & Planning. 2002;17:32–41. doi: 10.1093/heapol/17.1.32. [DOI] [PubMed] [Google Scholar]
- Sheikh K, Gilson L, Agyepong IA, et al. Building the field of health policy and systems research: framing the questions. PLoS Medicine. 2011;8:e1001073. doi: 10.1371/journal.pmed.1001073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikh K, Porter J. Discursive gaps in the implementation of public health policy guidelines in India: The case of HIV testing. Social Science & Medicine. 2010;71:2005–13. doi: 10.1016/j.socscimed.2010.09.019. [DOI] [PubMed] [Google Scholar]
- Shelton JD. Ensuring health in universal health coverage. Nature. 2013;493:453. doi: 10.1038/493453a. [DOI] [PubMed] [Google Scholar]
- Smith PC, Stepan A, Valdmanis V, Verheyen P. Principal-agent problems in health care systems: an international perspective. Health Policy. 1997;41:37–60. doi: 10.1016/s0168-8510(97)00012-2. [DOI] [PubMed] [Google Scholar]
- Ssengooba F, Mcpake B, Palmer N. Why performance-based contracting failed in Uganda - An ‘open-box’ evaluation of a complex health system intervention. Social Science & Medicine. 2012;75:377–83. doi: 10.1016/j.socscimed.2012.02.050. [DOI] [PubMed] [Google Scholar]
- THET. Mapping of Health Links in the Zambian Health Services and Associated Academic Institutions under the Ministry of Health. Lusaka: Tropical Health and Education Trust (THET) and Ministry of Health; 2007. [Google Scholar]
- Van olmen J, Criel B, Devadasan N, et al. Primary Health Care in the 21st century: primary care providers and people's empowerment. Trop Med Int Health. 2010;15:386–90. doi: 10.1111/j.1365-3156.2010.02475.x. [DOI] [PubMed] [Google Scholar]
- Vega J. Universal health coverage: the post-2015 development agenda. Lancet. 2013;381:179–80. doi: 10.1016/S0140-6736(13)60062-8. [DOI] [PubMed] [Google Scholar]
- Victora C, Saracci R, Olsen J. Universal health coverage and the post-2015 agenda. Lancet. 2013;381:726. doi: 10.1016/S0140-6736(13)60581-4. [DOI] [PubMed] [Google Scholar]
- Yin RK. Case Study Research: Design and Methods, 4th edn. London: Sage; 2009. [Google Scholar]