Abstract
Background In Uganda, community services for febrile children are expanding from presumptive treatment of fever with anti-malarials through the home-based management of fever (HBMF) programme, to include treatment for malaria, diarrhoea and pneumonia through Integrated Community Case Management (ICCM). To understand the level of support available, and the capacity and motivation of community health workers to deliver these expanded services, we interviewed community medicine distributors (CMDs), who had been involved in the HBMF programme in Tororo district, shortly before ICCM was adopted.
Methods Between October 2009 and April 2010, 100 CMDs were recruited to participate by convenience sampling. The survey included questionnaires to gather information about the CMDs’ work experience and to assess knowledge of fever case management, and in-depth interviews to discuss experiences as CMDs including motivation, supervision and relationships with the community. All questionnaires and knowledge assessments were analysed. Summary contact sheets were made for each of the 100 interviews and 35 were chosen for full transcription and analysis.
Results CMDs faced multiple challenges including high patient load, limited knowledge and supervision, lack of compensation, limited drugs and supplies, and unrealistic expectations of community members. CMDs described being motivated to volunteer for altruistic reasons; however, the main benefits of their work appeared related to ‘becoming someone important’, with the potential for social mobility for self and family, including building relationships with health workers. At the time of the survey, over half of CMDs felt demotivated due to limited support from communities and the health system.
Conclusions Community health worker programmes rely on the support of communities and health systems to operate sustainably. When this support falls short, motivation of volunteers can wane. If community interventions, in increasingly complex forms, are to become the solution to improving access to primary health care, greater attention to what motivates individuals, and ways to strengthen health system support are required.
Keywords: Malaria, community health, health workers, community medicine distributors, community health workers, community health volunteers, motivation, case management, Uganda
KEY MESSAGES.
In Uganda, the main benefits for community medicine distributors (CMDs) in their work appeared related to ‘becoming someone important’, with the potential for social (and financial) mobility for self and family, including building relationships with health workers.
At the time of the survey, over half of CMDs felt demotivated due to limited support from communities and the health system, lack of supervision, unrealistic expectations of caregivers, limited drugs and supplies, and lack of compensation.
Our results suggest a disconnect between what is expected from a CMD and what the CMD expects to get out of volunteering, leading to feelings of disappointment, low motivation and isolation, when expectations are not met.
If community interventions, in increasingly complex forms, are to become the solution to improving access to primary health care, greater attention to what motivates individuals, and ways to strengthen health system support, are required.
Introduction
Ensuring access to effective antimalarial treatment remains a long-standing international goal (WHO 2010). Artemisinin-based combination therapy (ACT) is generally recommended as first-line treatment for uncomplicated Plasmodium falciparum malaria, but until recently, access to ACTs within, and beyond, the public sector has been challenged by weak health systems, supply issues and high drug costs (Kager 2002; Moerman et al. 2003; Whitty et al. 2008). To increase access to effective antimalarial treatment in Africa, the World Health Organization (WHO) advocates for community-based case management of malaria, where community members are selected to provide treatment for febrile children (World Health Organization 2004; World Health Organization 2005). Such community-based programmes include home management of malaria, in which febrile children are treated presumptively with antimalarial drugs, and integrated community case management (ICCM), which provides treatment for malaria, pneumonia and diarrhoea (WHO and UNCEF 2012). Increasingly, community-based programmes are also incorporating rapid diagnostic tests (RDTs) for malaria, to aid in diagnosis and targeting appropriate antimalarial treatment (Chanda et al. 2011a,b; Elmardi et al. 2009; Hawkes et al. 2009; Mukanga et al. 2010; Zikusooka et al. 2008).
Shifting tasks from health workers to community members is rooted in the philosophy endorsed in the 1978 Alta Ata Declaration, which promoted equity, universal primary health care, and ‘bringing health care as close as possible to where people live and work’ (World Health Organization 1978). The idea of task-shifting has gained prominence as countries strive to achieve the Millennium Development Goals (MGDs) for child survival, maternal health, HIV, tuberculosis, and malaria. The renewed interest in expanding the role of community health workers has been driven by the human resource crisis in Africa, which limits delivery of essential health interventions (Lehmann et al. 2009). Due to resource limitations, many community-based programmes rely on volunteers, which can present challenges for long-term sustainability (Bhattacharyya et al. 2001). Community-based programmes require support from the existing health system and communities, and community health workers must be trained and supervised, and motivated to perform their job (Young et al. 2012). Although task-shifting to community members has the potential to increase coverage of health services and achieve health gains, this approach is not a substitute for a functional health system (Haines et al. 2007).
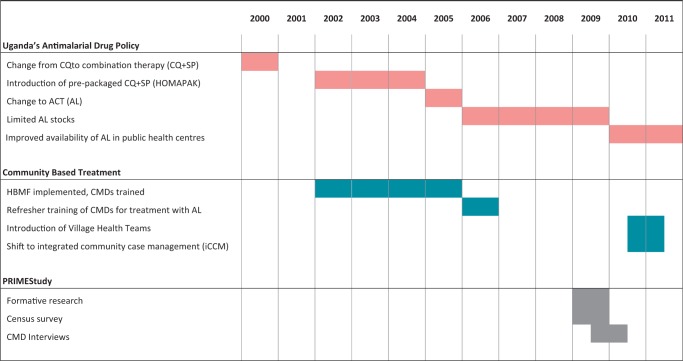
Uganda has adopted a community-based approach to management of febrile illnesses in children. In the home-based management of fever (HBMF) programme, which was introduced in 2002, volunteer community medicine distributors (CMDs) were trained to distribute pre-packaged chloroquine plus sulfadoxine-pyrimethamine (CQ + SP, branded HOMAPAK) free of cost (Figure 1). HBMF was intended to be scaled-up nation-wide over 3 years (Kolaczinski et al. 2006), but the programme was only fully functional in a few areas of the country, and stalled in 2006 due to shortages of artemether-lumefantrine (AL), the new first-line therapy (Batwala et al. 2010). A more comprehensive programme involving Village Health Teams (VHTs), which aims to deliver ICCM, newborn care, immunizations, deworming and health education through volunteers, was introduced in 2010 in Uganda (Nanyonjo et al. 2012).
Figure 1.
Timeline of malaria treatment policies in Uganda and study period
Studies suggest that ICCM is feasible under trial conditions, but the capacity for community workers to sustainably deliver this complex package under real-life conditions remains unclear (Chanda et al. 2011b; Mukanga et al. 2010, 2011; Yeboah-Antwi et al. 2010). In order for ICCM to be successful, countries need to be able to provide policy support, training, supervision, performance monitoring and regular supplies (WHO and UNCEF 2012). Additionally, key areas such as work motivation, needs satisfaction, community health worker identity, motivation (Strachan et al. 2012) and links to community and health system are critical (Campbell and Scott 2011). However, social factors that impact on the implementation of community-based programmes, such as community perceptions and acceptability and community health worker motivation, remain understudied (Callaghan-Koru et al. 2012; Marsh et al. 2012).
We conducted a situational analysis of CMDs in Eastern Uganda as the community-based programme was scheduled to transition from HBMF to ICCM. We aimed to assess the level of programme support provided to CMDs, to evaluate the capacity of CMDs to treat febrile children and to explore factors that motivate community members to volunteer and participate in community-based programmes.
Methods
Study site
The study was conducted between October 2009 and April 2010 in the five sub-counties of West Budama North Health Sub-district in Tororo district, an area with high malaria transmission intensity [estimated entomologic inoculation rate (EIR) of 562 infective bites per person-year in 2002] (Okello et al. 2006). In 2009, the total population of West Budama North was estimated to be 144 216, with 25 560 households and 26 905 children under five, in a census survey conducted by the study team (Staedke 2010). A total of 17 functional public health centres (HC) are located in the study area, and nearly all households in the study area are within a 5 km radius of a public health centre. In 2002, the HBMF programme using CQ + SP was launched in Tororo with a 2-day training workshop for the selected CMDs. In late 2006, a 2-day refresher training workshop was held for CMDs coinciding with the transition from CQ + SP to AL as first-line therapy for malaria. However, AL was never fully introduced into the HBMF programme due to limited ACT stocks, and as of November 2013, the comprehensive ICCM programme has not been implemented in Tororo.
Data collection and analysis
A list of the CMDs engaged in the delivery of antimalarial drugs in the study area was generated with the assistance of the local health inspector and 100 CMDs (five per parish) were invited to participate in the survey using convenience sampling (typically, the first five CMDs per parish who agreed or could be found). CMDs were interviewed at their homes or at a central place (such as a nearby health facility) within their parish. Information sheets were used to describe the purpose of the survey and prior to the interview witnessed verbal consent was obtained for the participation in and recording of the interview. The interviews were carried out in teams consisting of an interviewer and a note-taker who had been trained by study investigators prior to the commencement of the study using established training materials (Haaland et al. 2006). The interviewer facilitated and guided the interview while the note-taker observed and recorded notes about the interview. All interviews were recorded using a digital voice recorder, with the recordings used to support notes taken by hand in the field.
The interview was comprised of three components. The first section was a structured quantitative questionnaire to collect information from each CMD on their work, including patient load, available local health services, referral practices, training and supervision, drug supply, and logistical support. The next section was a questionnaire to assess the CMDs’ knowledge of fever case management. This section contained both structured and open ended questions. The final section was an in-depth interview to explore experiences as a CMD including motivation, supervision, and relationships with patients, communities and others.
Detailed contact summaries were made for each of the 100 in-depth interviews. These were reviewed for emerging themes, with transcription and coding carried out first on those interviews with the most forthcoming participants who covered the widest range of themes and geographic locations. Interviews were fully transcribed in their original languages (English, Japadhola, Luganda and a few in Lusoga) and then if required later translated into English. Once saturation of emerging themes was reached, the detailed transcription and analysis was terminated.
Prior to data entry, the questionnaires were reviewed and coded by the study team based on a previously defined coding scheme. Quantitative data collected from the first two sections of the interview questionnaire were then double-entered into Microsoft Access 2000 (Microsoft Inc., Redmond, Washington) and analysed using STATA Data Analysis and Statistical Software, version 10 (StataCorp, College Station, Texas) statistical software.
In-depth interview recordings and notes (component three) were transcribed into Microsoft Word (Microsoft Inc., Redmond, Washington) by the members of the study team who carried out the interviews. These were systematically cross-checked with the audio files by other members of the study team. Where translation was necessary, initial transcription was made first in the original language and then translation was carried out by the same researcher in order to rely on their interpretation of the meaning as conveyed during the interview. This process allowed the research team to cross-check translations as well as to revisit words in the original language during the analysis process. Transcripts were imported into qualitative data management software NVivo 8 (QSR International) and coded by two members of the study team under the guidance of a senior social scientist. The coding was inductive, labelling repeating ideas and grouping these into themes emerging across participant responses and narratives.
Results
Study population
A total of 100 CMDs were interviewed (Table 1) and analysis was based on 35 fully transcribed, translated and coded interviews and 65 detailed contact summaries. Just over half of the CMDs were women, and two-thirds were between 30 and 45 years of age, with a mean age of 40.2 years. Nearly all CMDs were originally from the study area. Most CMDs had attended primary or secondary school, but one-quarter had attended only primary school and only 14% of CMDs had gone beyond secondary school achieving a certificate or diploma.
Table 1.
CMD demographics
| Characteristics | Proportion of CMDs (n = 100) |
|---|---|
| Gender (% female) | 56% |
| Age (mean years, SD, range) | 40.2 (8.2) 26–65 |
| <30 years | 10% |
| 30–45 years | 66% |
| >45 years | 24% |
| Originally from the area | 91% |
| Education | |
| Primary | 28% |
| Secondary | 58% |
| Certificate | 10% |
| Diploma | 4% |
| Duration worked (mean years, SD, range) | 4.9 (1.7) 0.5 – 11 |
| <5 years | 38% |
| ≥5 years | 62% |
| Active during the time of the survey | 47% |
| Supportive supervision of active CMDs in past 6 months | 0% |
| Training | |
| Treatment of fever | 33% |
| Treatment of malaria with AL | 61% |
| Stock of any malaria drug (HOMAPAK, AL and others) | |
| Sufficient | 72% |
| Stockouts greater than 1 month | 45% |
SD = Standard Deviation.
The mean duration CMDs had worked was almost 5 years, with over half working for 5 years or more. All interviewees had been part of the government’s HBMF programme, which was stalled at the time of the interviews, and many CMDs reported that they were actively working within a community-based programme at the time of the survey, including other Ministry of Health (MoH) and non-governmental organization (NGO) programmes. CMDs reported working on a number of non-malaria initiatives including family planning, prevention of mother to child transmission of HIV, and circumcision programmes.
Patient load
When the HBMF programme was active, the CMDs reported receiving 20 patients per week, including approximately 15 patients with suspected malaria, and 5 non-malaria patients. CMDs reported that patients sought care at all times of day. This could be problematic if the visit occurred in the middle of the night, or if the CMD was engaged in their main, non-volunteer, work. CMDs were particularly keen to note the cost of patients who present at night as they were often required to provide their own source of light (kerosene, candles, and torch/flashlight) or even accommodate the family until the morning light due to fears of insecurity.
The other problem … .is that if someone comes at night with a sick child and you do not have paraffin in [the] house and yet you have to give her the service you are forced to go to the neighbourhood to ask for some light or a lamp. In the process you see that you are sometimes delaying and the malaria is increasing. One time a woman almost lost her child because I went to a neighbour to beg for a lamp, I had no torch so I learned a lesson and I bought one. (CMD #303)
Programme support
Training and supervision
Sixty-one CMDs had received training in management of malaria with AL in the past 2 years, in addition to their initial HBMF training. One-third of the CMDs reported receiving some additional training on management of children with fever within the past 2 years. The training was most commonly provided by members of the district health team, or health workers from local health centres Health Centre III (HCIII) and Health Centre IV (HCIV).
Only four CMDs reported that they had been supervised in the previous 6 months. Some CMDs reported that they had never been supervised in their home village; others said that the only form of supervision they received was from health workers who reviewed their patient registers when they collected drugs from the health centre. However, these types of supervision activities were dictated by the availability of drugs and health workers.
You just work on your own, you bring back the report here [to the health facility] but nobody will follow you to see what you are doing. (CMD #371)
Drug supplies
CMDs reported that lack of antimalarial drugs severely compromised their work. Drugs were supplied to CMDs through the health centres, but drug stocks were often insufficient. Faced with shortages, drugs were allocated to the health centres first, which were the top priority, leaving the CMDs without drugs. When the first-line therapy was changed from CQ + SP to AL, the situation worsened, and the HBMF programme was stalled due to lack of sufficient quantities of drugs, leaving the CMDs unsure of their role.
There are no drugs and there’s nothing much I can do though I am dedicated [to] my work. (CMD #349)
Logistical supplies
CMDs were not provided with any form of transport by the MoH, such as a bicycle, or an allowance to cover the costs of transporting themselves and/or patients. As a result, CMDs had to provide or fund their own transport in order to collect drugs from the health centre or to follow up patients in neighbouring villages. Without a bicycle, CMDs often had to walk long distances. This also affected patients, who sometimes asked CMDs for transport money to facilitate their referral to a health centre.
Transport, when you are coming to collect the drugs from the health centre here, I just use my [own] transport to and fro and am not paid. In [the] village there I work for no payment but I just volunteer to help my children and my neighbours too. (CMD #351)
CMDs listed many other supplies they were lacking, including boxes or containers to store drugs, bags to transport drugs from the health centre to their homes, boots and rain gear, and stationery to keep patient records. CMDs reported that without these essential supplies it was difficult to perform their jobs (Box 1). They also noted that lack of proper storage containers to safely store drugs put children, including their own, at risk.
We were given medicine, there is even no box for storing them so you store on your own risk. (CMD #371)
CMDs stated that while they were expected to see patients at all times of day or night, without a torch or paraffin for lamps, they were unable to examine patients, distribute drugs, or complete records at night (Box 1).
Box 1. CMD Logistical ‘Tools’.
‘For my work as a community distributor, where we keep our drugs is not all that sufficient because we could just bring boxes you go and just dump the drugs there, it needed something may be like a proper box which can keep drugs out of reach of children because it is a risk to us as drug distributors to distribute these drugs here you may have a small child who can even come and swallow these drugs eventually you find that the child is dead so it needs something safe enough where you can lock these drugs and they are safe.’ (CMD #350)
‘At night somebody can just come to you [and say] that my son is sick … so moving from here to there and the place is darkness, it’s even raining so you just move like that, so if they can provide for us with some rain coats.’ (CMD #305)
‘We were given registers without a pen, they want us to write, they want us to refer, there is no referral form, [and] there is no exercise book for writing.’ (CMD #371)
‘Sometimes you may be there without any money for buying paraffin then a patient may come at night and the lamp doesn’t have paraffin and sometimes you don’t even have a matchbox. Isn’t that a challenge? You may go the fireplace and find the fire went out.’ (CMD #340)
‘the challenge is financial support because especially those patients who come at night when they come and you really do not have paraffin and a match box you really feel very sorry for that patient because there is (not) any other way you can help him or her but when you have this (money for paraffin and match box) I think it is easy to help such a person.’ (CMD #350)
‘The government has given this free treatment to our community … . the problem I can face; I don’t have this lamp because a patient might come at night time when I don’t have this lamp.’ (CMD #319)
The CMDs also reported that without uniforms, they could not be distinguished as community health workers. Respondents commented that wearing ‘uniforms’ or other forms of identification would allow CMDs to be identified in the community and at the health centres when they went to collect their drugs.
There is another challenge that we don’t have [uniforms] … like [the] Red cross they have T-shirts now for us we have no [sic] anything like a uniform … Maybe you are called in a meeting you find that you cannot differentiate people. (CMD #335)
Some CMDs also felt that uniforms would benefit them personally. Rather than having to wait with other patients, if they were recognized at the health centres as a CMD they could receive preferential treatment.
Maybe whenever I would fall sick, I would also join the line and wait like an ordinary person, we were not recognized as we even had no uniforms to identify us. (CMD #400)
CMD Capacity
Knowledge
Overall, the CMDs performed poorly on the malaria knowledge questionnaire (Table 2). The lack of drug supplies, and lapse in the HBMF programme, meant that CMDs were unable to put their training into practice, which may have adversely impacted on their ability to recall information and their performance on the knowledge questionnaires.
Ever since we were trained for Coartem, we have never seen Coartem and it may even cause us to forget as mothers we easily forget after training [when] we are not given something to practise. (CMD #349)
When asked to define malaria, one-quarter of CMDs mentioned ‘fever or high temperature or hot body’, but only one mentioned ‘disease caused by a parasite’. Fewer than half of CMDs reported that malaria was transmitted through the bite of a mosquito, and few said that the female mosquito was responsible.
Table 2.
Proportion of correct responses to the knowledge questions (n = 100)
| Question | Correct responses, n (%) |
|---|---|
| ‘What is malaria?’ | |
| Fever or high temperature or hot body | 28 (28%) |
| Parasites | 1 (1%) |
| ‘How does someone get malaria?’ | |
| Bite of a mosquito | 41 (41%) |
| Female mosquito | 10 (10%) |
| Anopheles mosquito | 7 (7%) |
| ‘What is the most common symptom of malaria in children?’ | |
| Fever or high temperature or hot body | 74 (74%) |
| ‘What signs suggest that a child with malaria is very sick? (also called ‘danger signs’ for severe malaria) | |
| Convulsions | 34 (34%) |
| Unable to sit/stand due to weakness | 32 (32%) |
| Lethargy (prostration or extreme weakness) | 13 (13%) |
| Unable to drink or breastfeed | 11 (11%) |
| Vomiting everything | 7 (7%) |
| Respiratory distress (laboured breathing) | 10 (10%) |
| Jaundice (yellow colouring of eyes) | 7 (7%) |
| Severe anaemia | 2 (2%) |
| ‘What illnesses, other than malaria, commonly cause fever in children?’ | |
| Measles | 46 (46%) |
| Respiratory tract infection (pneumonia) | 44 (44%) |
| Viral infection (common cold, HIV/AIDS, etc.) | 14 (14%) |
| Skin infection (abscess) | 9 (9%) |
| Throat or ear infection | 2 (2%) |
| ‘How should a child with uncomplicated malaria be treated?’ | |
| HOMOPAK (CQ + SP) | 57 (57%) |
| Coartem (artemether-lumefantrine) | 32 (32%) |
| Dose based on child’s age or weight | 10 (10%) |
| Complete 3 days of treatment | 8 (8%) |
| ‘How should you follow-up a child that you start on treatment?’ | |
| If child does not improve in 2 days, refer | 23 (23%) |
| Visit the child daily for the first 2 days | 3 (3%) |
| If child improves, visit again in 1 week | 0 (%) |
Most CMDs correctly identified fever as the most common symptom of uncomplicated malaria in children, but knowledge of danger signs of severe disease was limited. No CMD correctly identified all danger signs, although ‘convulsions’ and ‘unable to sit/stand due to weakness’ were mentioned by one-third of respondents, respectively. CMDs were aware that measles (46%) and respiratory infections (44%) cause fever in children. Fewer CMDs mentioned other causes of fever such as infections of the skin, ear, or throat, and urinary tract infection was not mentioned.
Just over half (57%) of CMDs reported that children with uncomplicated malaria should be treated with CQ + SP. Although one-third of CMDs did mention AL, the first-line recommended antimalarial treatment; few knew the correct dosing or timing for administration. Only one-quarter stated that the child should be referred if they had not improved after two days.
Relationship with the community
Respondents felt that community members understood their roles as CMDs. However, we observed that some tensions and misunderstandings still existed. CMDs reported that community members often accused them of selling drugs when treatment was not available, and to interpret a CMD’s inability to provide treatment as a personal slight rather than the result of a stock-out. Some respondents were concerned that community members mistakenly believed that the CMDs were getting paid for their work and in some cases had expectations for services beyond drug provision.
Nobody could give you a chicken … after knowing that this is a government thing and you are working there, they may even expect you to give them something, they may think that you are being paid. (CMD #387)
Like … if you refer the child, they say they have no transport [except] of walking. If you can get for her somebody to escort, now they want transport from you. (CMD #371)
Motivation
A range of motivations for wanting to participate in the CMD programme were evident in respondent accounts. Statements that CMDs had enrolled to ‘help the community’ and ‘to volunteer’ were frequent, in 80% (28/35) of coded transcripts; however, a solely altruistic interpretation of these statements was not supported by analysis of respondent narratives. Rather, CMDs often went on to describe how assisting the community, and volunteering, could position them not only to provide immediate help for their families, but allowed them to gain social status and to garner future opportunities for work. Motivation was similar for both men and women; however, a larger proportion of women perceived working as a CMD as a way to secure future employment and/or to benefit them personally. An immediate advantage of the training and access to supplies of malaria medicines was to help family members, specifically children, by having an enhanced understanding of malaria and ability to treat swiftly.
It was good because the knowledge I had in the training at least it helped me in my home because I can tell the symptoms of malaria, the causes and all that which I used not to know much. (CMD #350)
Almost all respondents spoke of the benefit of working as a CMD for their social status. This involved ‘getting many friends’, including with health workers at formal facilities, an opportunity they recognised as important for increasing their exposure to different ideas as well as to a wider social circle that linked them to other benefits. It also involved ‘becoming known’ as someone who can help with health issues locally, often being called musawo, ‘health worker’. Being well known held many benefits, including social recognition at community functions such as funerals, as well as the possibility for accruing reciprocal favours from others, as described by this CMD,
What I have got first and foremost right now, if I have a problem or am going somewhere, I can’t have difficulties because my people if I go there and tell them ‘I have such a problem’, they hurry to help me. Because even when they come to me, even at night, I do not give them difficulties, I help them quickly. (CMD #303)
Becoming known also linked CMDs to further opportunities relating to health programmes,
It is like I stand as a key person in the area. Whenever there is a health programme in the zone, they just come and consult me. (CMD #349)
Respondents described other programmes they had been able to work with, including immunization, mass drug administration and bednet distribution, each with different benefits for participation, as this CMD describes,
The other good thing I have got is that one time, nets were brought at the sub county and we are the ones who distributed them. We first got ours as the workers then we distributed the rest and we even got an allowance so I felt very good. (CMD #340)
The possibility of further opportunities after working as a volunteer for the HBMF programme formed an important incentive to be a CMD. This was discussed by over half of respondents, often in terms of positioning for the future, for example, ‘I know that I can reach ahead and some good thing happens for me in future’ (CMD #326). This appeared to have been encouraged by supervisors of the programme, as exemplified by this respondent,
As we are volunteers, she [the supervisor] said we should continue [and] keep it up … the harder you work the more you will be recognized. (CMD #356)
While these motivators were important for CMDs to continue to operate, in spite of challenges of supplies and other logistics, respondents also reported feeling dissatisfied with the lack of remuneration from the government for their work. Some suggested lack of pay was a sign of disrespect from the MoH programme, affecting the level of respect they could accrue from community members in an unpaid position,
I don’t feel comfortable because we are not recognized, there is no motivation … Because we are not paid, so people don’t even respect us. (CMD #309)
In part, the desire for compensation for their work as a CMD for the government-sponsored HBMF programme appeared to relate to expectations built up from experiences with other programmes or organizations that provided various incentives, such as T-shirts or bicycles, as well as some financial incentives such as generous transport refunds.
The dissatisfaction with lack of respect represented by pay was underscored when the HBMF programme stalled due to lack of drugs, when CMDs felt that they may have been forgotten, and were concerned about losing their position and the status associated with being a CMD.
I feel so discouraged because I used to be called ‘musawo’ [health worker] now these days I do not distribute these drugs [so] people are almost forgetting me and I was being given much respect so I had the love for the work I was doing though voluntary. (CMD #350)
As the MoH in Uganda begins to revitalize the community case management activities by training VHTs, current CMDs are anxious about whether they will be selected to participate in the programme.
Okay like in Gwaragwara, we have the VHTs … they are there but you find that we who were trained for this work, it is like they have taken up our work. Like instead of looking for me who was trained for this work, you find that maybe they [are] doing a CMD’s work. (CMD #349)
Discussion
We conducted a situational analysis of CMDs who had participated in Uganda’s HBMF programme to assess the level of support provided to this community-based programme, and to evaluate the capacity and motivation of CMDs to successfully and sustainably deliver more complex interventions, such as ICCM. We found that multiple challenges and limitations were likely to affect the ability of CMDs to provide good health care, including high patient load, limited training and supervision, lack of drugs and logistical supplies, lack of compensation, limited knowledge of malaria case management, and unrealistic expectations of caregivers and community members. CMDs’ motivation to provide good care despite these factors waned when opportunities that they initially had hoped to receive by volunteering did not materialize, resulting in a sense of disappointment and isolation.
Our analysis suggested a disconnect between what is expected from a CMD and how the CMD expects to benefit from volunteering, leading to feelings of disappointment, low motivation and isolation when these expectations are not met. CMDs in this study appeared initially to sign up for the spirit of volunteerism inherent in community health worker programmes and reported being motivated by helping others in their communities. However, their narratives suggested on-going motivation drew from possibilities of social (and potential financial) mobility for them and their families, particularly ‘becoming someone important’ through their work. This is consistent with other studies that found a combination of altruism, self-efficacy, peer approval and status were important personal motivators for volunteers (Amare 2009; Bhattacharyya et al. 2001; Ludwick et al. 2013; Rahman et al. 2010) as well as for formally trained health workers (Chandler et al. 2009; Dambisya 2007; Mathauer and Imhoff 2006; Willis-Shattuck et al. 2008). In addition, we found that being a CMD enabled individuals to position themselves for future opportunities, which has also been reported as a motivating factor for CMDs in southwest Uganda (Ludwick et al. 2013). The observation of community members becoming ‘career volunteers’ has been made elsewhere, for example in Ethiopia and Uganda where ethnographic studies have shown that volunteering in community health projects is seen as an opportunity to position oneself for future paid opportunities (Maes and Kalofonos 2013; Whyte et al. 2013). It is interesting to note that nearly half of all CMDs in our sample were men – a departure from the taken-for-granted nature of the unpaid carework sector, typically comprising of women (Glazer 1988). The possibility of future paid work appeared to motivate both men and women in this study.
This utilitarian perception of volunteering challenges assumptions made by programmes as to the altruistic nature of volunteering. Programmes based on a Western conceptualisation of volunteerism, rooted in the idea of altruism, may not fulfil the wider social and economic needs of those expected to volunteer as community health workers, especially in the long-term. Research on the motivation of formal health workers has led to an appreciation of both financial and non-financial incentives in supporting a motivated workforce (Chandler et al. 2009; Dambisya 2007; Mathauer and Imhoff 2006; Willis-Shattuck et al. 2008) who deliver good quality health care (Rowe et al. 2005). Our findings suggest that this appreciation needs to be extended to community health workers: greater attention to their motivation (both monetary and non-monetary) is essential for such programmes to be sustainable at scale (Adams and Hicks 2000; Amare 2009; Dambisya 2007).
This study found that feelings of dissatisfaction amongst CMDs grew when the programme for which they were trained became only partially functional. Community health worker programmes rely on the support of communities and health systems to operate (Abbatt 2005), but in our study, over half of CMDs felt demotivated due to unrealistic expectations of caregivers, limited drugs and supplies, poor supervision, and lack of compensation. This finding was similar for both men and women CMDs in our sample and is consistent with observations in other countries. A study in Nigeria also found that village health workers were discouraged due to lack of credibility with the community and poor supervision (Gray and Ciroma 1988). In Malawi, health surveillance assistants reported that insufficient supplies, limited supervision and unrealistic community expectations were demotivating and affected their performance to do their work (Callaghan-Koru et al. 2012).
Task shifting has become increasingly popular in response to limited skilled health personnel, aiming to reduce disparities in coverage, by targeting interventions to improve coverage (Bhutta et al. 2010). However, strong links between community programmes and the formal health system are required to ensure appropriate training and supervision, and adequate remuneration of community health workers (Haines et al. 2007). Despite the knowledge of their importance, these components still remain weak in many community health worker programmes (Strachan et al. 2012), and our results suggest that CMDs were demotivated by the lack of adequate support from the health system. For community-based programmes to successfully fill the health care gap, it will be necessary to address these health systems challenges and ensure that community health workers are well-supported and fully integrated into the system (Singh and Sachs 2013). Most importantly, implementation of community programmes should be ‘part of a comprehensive primary health care system and should not be viewed as an inexpensive or low cost measure’ (WHO and UNCEF 2012) and should not divert attention away from longer-term interventions to improve health care infrastructure and delivery of good quality health care by trained practitioners. Although community health volunteer programmes can be successful and appropriate in certain settings, generic models replicated irrespective of context may not be the answer; a more dynamic model that can be adapted to the local needs and available support should be considered instead (Standing and Chowdhury 2008).
Our study has several limitations. First, we provide a snap shot of the malaria community case management programme in Uganda at a certain point in time, many years after the HBMF programme was initiated. The policy on first-line antimalarial drugs had changed over this time, and country-wide stockouts of the new ACT drugs had occurred in the months prior to the assessment. Many CMDs interviewed were inactive at the time of the assessment, and their most recent training and supervision had often occurred more than 1 year prior to the survey. This dormant nature of the malaria case management programme at the time of the study is likely to have affected perspectives of the programme by CMDs, estimated patient loads, as well as their scores in the knowledge questionnaire. Second, our findings are subject to the methodological approaches we used. We were able to carry out interviews with a large number of respondents, which provides a measure of confidence in the representativeness of the findings to this study population, and enabled our qualitative analysis to reach saturation in analysis on key issues. However, use of convenience sampling may have introduced an element of selection bias as we cannot guarantee that the study population is fully representative of all CMDs. Additionally, our approach to knowledge assessment relied on statements and narratives of respondents rather than vignettes or direct observation, as used previously in Tanzania and Uganda (Leonard and Masatu 2005; Namagembe et al. 2012). Therefore our methods have limited our ability to relate what CMDs know and do in practice, restricting us to present their knowledge in theory, and their interpretations of their work in relation to their experiences and expectations. The strength of the approach we take is the ability to relate the perspectives of these crucial front-line workers and to bring their voices to the fore where they are often overlooked.
Conclusion
Community programmes have the potential to improve access to care and fill gaps in health systems, particularly in low-resource settings. Uganda has adopted community-based treatment of febrile illnesses in children, but a misalignment between CMD expectations and programme provisions together with inadequate health system support demotivate CMDs and hinder the success of the programme. If community interventions, in increasingly complex forms, are to become the solution to improve access to primary health care, greater importance needs to be placed on the sustainability of community health volunteer programmes, in particular individual motivation and greater support to the wider health systems to which they belong. Further investment is required to address individual and health system challenges to enhance capacity and motivation for volunteers to provide effective treatment at the community level.
Ethics
The study was approved by the Ugandan National Council for Science and Technology (UNCST), the Makerere University School of Medicine Research & Ethics Committee (SOMREC), and the London School of Hygiene and Tropical Medicine (LSHTM) Ethics Committee.
Acknowledgements
The authors thank the ACT social science team (Christine Nabirye, Miriam Kayendeke, James Kizito, Loy Sentumbwe, and Grace Nyabwolo) for conducting the interviews; the ACT Census survey team, district leadership, local council leaders and Nicholas Wendo, who served as their community liaisons and guides; other ACT project team members (Rita Kabuleta Luswata, Robert Senyonga, Tema Kizito, Faith Mukoya, Levi Mugenyi, Geoff Lavoy) and the IDRC administration and finance department for their contributions; and the ACT Consortium (including the core team and secretariat) for all of their support and guidance. Finally, they would like to thank all of the CMDs for participating in the study.
Funding
Funding. The study was funded by the ACT Consortium through a grant to the London School of Hygiene & Tropical Medicine from the Bill & Melinda Gates Foundation (ITGB-VG01). Kristin Banek is supported by an American Association of University Women (AAUW) dissertation fellowship.
Conflict of interest statement. None declared.
References
- Abbatt F. Scaling Up Health and Education Workers: Community Health Workers. London: United Kingdom Department for International Development (DfID) Health Systems Resource Centre; 2005. [Google Scholar]
- Adams O, Hicks V. WHO's Workshop on a Global Health Workforce Strategy, Annecy, France. 2000. Pay and non-pay incentives, performance and motivation. [Google Scholar]
- Amare Y. Non-Financial Incentives for Voluntary Community Health Workers: A Qualitative Study. 2009. JSI Research & Training Institute, Inc., Addis Ababa, Ethiopia. [Google Scholar]
- Batwala V, Magnussen P, Nuwaha F. Challenges to implementation of artemisinin combination therapy policy in Uganda. Int Health. 2010;2:262–68. doi: 10.1016/j.inhe.2010.07.002. [DOI] [PubMed] [Google Scholar]
- Bhattacharyya K, Winch PJ, LeBan K, Tien M. Community Health Worker Incentives and Disincentives: How they Affect Motivation, Retention and Sustainability. 2001. Basic Support for Institutionalizing Child Survival Project (BASICS II) [Google Scholar]
- Bhutta ZA, Lassi ZS, Pariyo G, Huicho L. Global Experience of Community Health Workers for Delivery of Health Related Millennium Development Goals: A Systematic Review, Country Case Studies and Recommendations for Integration into National Health Systems. World Health Organization; 2010. Global Health Workforce Alliance. [Google Scholar]
- Callaghan-Koru JA, Hyder AA, George A, et al. Health workers' and managers' perceptions of the integrated community case management program for childhood illness in Malawi: the importance of expanding access to child health services. Am J Trop Med Hygiene. 2012;87:61–68. doi: 10.4269/ajtmh.2012.11-0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell C, Scott K. Retreat from Alma Ata? The WHO's report on Task Shifting to community health workers for AIDS care in poor countries. Global Public Health. 2011;6:125–38. doi: 10.1080/17441690903334232. [DOI] [PubMed] [Google Scholar]
- Chanda P, Hamainza B, Moonga HB, et al. Relative costs and effectiveness of treating uncomplicated malaria in two rural districts in Zambia: implications for nationwide scale-up of home-based management. Malaria J. 2011a;10:159. doi: 10.1186/1475-2875-10-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanda P, Hamainza B, Moonga HB, Chalwe V, Pagnoni F. Community case management of malaria using ACT and RDT in two districts in Zambia: achieving high adherence to test results using community health workers. Malaria J. 2011b;10:158. doi: 10.1186/1475-2875-10-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler CIR, Chonya S, Mtei F, Reyburn H, Whitty CJM. Motivation, money and respect: a mixed-method study of Tanzanian non-physician clinicians. Soc Sci Med. 2009;68:2078–88. doi: 10.1016/j.socscimed.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Dambisya YM. A Review of Non-financial Incentives for Health Worker Retention in East and Southern Africa. South Africa: Health Systems Research Group, Department of Pharmacy, School of Health Sciences, University of Limpopo; 2007. [Google Scholar]
- Elmardi KA, Malik EM, Abdelgadir T, et al. Feasibility and acceptability of home-based management of malaria strategy adapted to Sudan's conditions using artemisinin-based combination therapy and rapid diagnostic test. Malaria J. 2009;8:39. doi: 10.1186/1475-2875-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glazer NY. Overlooked, Overworked: Women's Unpaid and Paid Work in the Health Serivces' ‘Cost Crisis’. Int J Health Serv. 1988;18:119–37. doi: 10.2190/2WKD-WAK9-27JK-MBHP. [DOI] [PubMed] [Google Scholar]
- Gray HH, Ciroma J. Reducing attrition among village health workers in rural Nigeria. Sociao-Economic Planning Sciences. 1988;22:39–43. [Google Scholar]
- Haaland A, Molyneux CS, Marsh V. Geneva. 2006. Quality information in field research:Training manual on practical communication skills for field researchers and project personnel, (Ed.) WHO/TDR. Available online < http://whqlibdoc.who.int/hq/2006/TDR_IRM_PCT_05.1_eng.pdf>. [Google Scholar]
- Haines A, Sanders D, Lehmann U, et al. Achieving child survival goals: potential contribution of community health workers. The Lancet. 2007;369:2121–31. doi: 10.1016/S0140-6736(07)60325-0. [DOI] [PubMed] [Google Scholar]
- Hawkes M, Katsuva JP, Masumbuko CK. Use and limitations of malaria rapid diagnositc testing by community health workers in war-torn Democratic Republic of Congo. Malaria J. 2009;8:308. doi: 10.1186/1475-2875-8-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kager PA. Malaria control: constraints and opportunities. Trop Med Int Health. 2002;7:1042–46. doi: 10.1046/j.1365-3156.2002.00981.x. [DOI] [PubMed] [Google Scholar]
- Kolaczinski JH, Ojok N, Opwonya J, Meek S, Collins A. Adherence of community caretakers of children to pre-packaged antimalarial medicines (HOMAPAK) among internally displaced people in Gulu district, Uganda. Malaria J. 2006;5:40. doi: 10.1186/1475-2875-5-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann U, Van Damme W, Barten F, Sanders D. Task shifting: the answer to the human resources crisis in Africa? Human Resour Health. 2009;7:49. doi: 10.1186/1478-4491-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard KL, Masatu MC. The use of direct clinician observation and vignettes for health services quality evaluation in developing countries. Soc Sci Med. 2005;61:1944–51. doi: 10.1016/j.socscimed.2005.03.043. [DOI] [PubMed] [Google Scholar]
- Ludwick T, Brenner JL, Kyomuhangi T, Wotton KA, Kabakyenga JK. Poor retention does not have to be the rule: retention of volunteer community health workers in Uganda. Health Policy Plan. 2013 doi: 10.1093/heapol/czt025. May 6. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes K, Kalofonos I. Becoming and remaining community health workers: perspectives from Ethiopia and Mozambique. Soc Sci Med. 2013;87:52–59. doi: 10.1016/j.socscimed.2013.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh DR, Hamer DH, Pagnoni F, Peterson S. Introduction to a special supplement: evidence for the implementation, effects, and impact of the integrated community case management strategy to treat childhood infection. Am J Trop Med Hygiene. 2012;87:2–5. doi: 10.4269/ajtmh.2012.12-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathauer I, Imhoff I. Health worker motivation in Africa: the role of non-financial incentives and human resource management tools. Human Resour Health. 2006;4:24. doi: 10.1186/1478-4491-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moerman F, Lengeler C, Chimumbwa J, et al. The contribution of health-care services to a sound and sustainable malaria-control policy. Lancet Infect Dis. 2003;3:99–102. doi: 10.1016/s1473-3099(03)00518-8. [DOI] [PubMed] [Google Scholar]
- Mukanga D, Babirye R, Peterson S, et al. Can lay community health workers be trained to use diagnostics to distinguish and treat malaria and pneumonia in children? Lessons from rural Uganda. Trop Med Int Health. 2011;16:1234–42. doi: 10.1111/j.1365-3156.2011.02831.x. [DOI] [PubMed] [Google Scholar]
- Mukanga D, Tibenderana JK, Kiguli J, et al. Community acceptability of use of rapid diagnostic tests for malaria by community health workers in Uganda. Malaria J. 2010;9:203. doi: 10.1186/1475-2875-9-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Namagembe A, Ssekabira U, Weaver MR, et al. Improved clinical and laboratory skills after team-based, malaria case management training of health professionals in Uganda. Malaria J. 2012;11:1. doi: 10.1186/1475-2875-11-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanyonjo A, Nakirunda M, Makumbi F, et al. Community acceptability and adoption of integrated community case management in Uganda. Am J Trop Med Hygeine. 2012;87:97–104. doi: 10.4269/ajtmh.2012.11-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okello PE, Van Bortel W, Byaruhanga AM, et al. Variation in malaria transmission intensity in seven sites throughout Uganda. Am J Trop Med Hygeine. 2006;75:219–25. [PubMed] [Google Scholar]
- Rahman SM, Ali NA, Jennings L, et al. Factors affecting recruitment and retention of community health workers in newborn care intervention in Bangladesh. Hum Resour Health. 2010;8:12. doi: 10.1186/1478-4491-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe AK, de Savigny D, Lanata CF, Victora CG. How can we achieve and maintain high-quality performance of health workers in low-resource settings? The Lancet. 2005;366:1026–35. doi: 10.1016/S0140-6736(05)67028-6. [DOI] [PubMed] [Google Scholar]
- Singh P, Sachs JD. 1 million community health workers in sub-Saharan Africa by 2015. The Lancet. 2013;14:17. doi: 10.1016/S0140-6736(12)62002-9. [DOI] [PubMed] [Google Scholar]
- Staedke SG. Phase 1 Report: Tororo District Survey Project. Characterizing the Population and Local Health Services. Kampala, Uganda: Uganda Malaria Surveillance Project. 2010. http://www.actconsortium.org/data/files/actc_tororo_phase_i_report_final_10june10.pdf. [Google Scholar]
- Standing H, Chowdhury AMR. Producing effective knowledge agents in a pluralistic environment: What future for community health workers? Soc Sci Med. 2008;66:2096–107. doi: 10.1016/j.socscimed.2008.01.046. [DOI] [PubMed] [Google Scholar]
- Strachan DL, Källander K, ten Asbroek AH, et al. Interventions to improve motivation and retention of community health workers delivering integrated community case management. (iCCM): stakeholder perceptions and priorities. Am J Trop Med Hygiene. 2012;87:111. doi: 10.4269/ajtmh.2012.12-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitty CJM, Chandler C, Anasah E, Leslie T, Staedke SG. Deployment of ACT antimalarials for treatment of malaria: challenges and opportunities. Malaria J. 2008;7(Suppl I) doi: 10.1186/1475-2875-7-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Guidelines for the Treatment of Malaria. Second ed. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- WHO and United Nations Children's Fund (UNICEF) 2012. Joint Statement – Integrated Community Case Management. June 2012. [Google Scholar]
- Whyte SR, Whyte M, Meinert L, Twebaze J. Therapeutic clientship: Belonging in Uganda's projectified landscape of AIDS care. In: Biehl J, Petryna A, editors. When People Come First: Critical Studies in Global Health. Princeton: Princeton University Press, 140–165; 2013. [Google Scholar]
- Willis-Shattuck M, Bidwell P, Thomas S, et al. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Services Research. 2008;8:247. doi: 10.1186/1472-6963-8-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Declaration of Alma-Ata. International Conference on Primary Health Care. 1978;Vol. 6 Alma-Ata, USSR, 12. [Google Scholar]
- World Health Organization. Scaling up Home-Based Management of Malaria: From Research to Implementation. Geneva: 2004. [Google Scholar]
- World Health Organization. The Roll Back Malaria Strategy for Improving Access to Treatment Through Home Management of Malaria. Geneva: 2005. [Google Scholar]
- Yeboah-Antwi K, Pilingana P, Macleod WB, et al. Community case management of fever due to malaria and pneumonia in children under five in Zambia: a cluster randomized controlled trial. PLoS Med. 2010;7:e1000340. doi: 10.1371/journal.pmed.1000340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young M, Wolfheim C, Marsh DR, Hammamy D. World Health Organization/United Nations Children’s Fund Joint Statement on integrated community case management: an equity-focused strategy to improve access to essential treatment services for children. Am J Trop Med Hygeine. 2012;87:6–10. doi: 10.4269/ajtmh.2012.12-0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zikusooka CM, McIntyre D, Barnes KI. Should countries implementing an artemisinin-based combination malaria treatment policy also introduce rapid diagnostic tests? Malaria J. 2008;7:176. doi: 10.1186/1475-2875-7-176. [DOI] [PMC free article] [PubMed] [Google Scholar]