Abstract
Background
Early detection of pneumothorax is critically important. Several studies have shown that chest ultrasonography (CUS) is a highly sensitive and specific tool. The present systematic review and meta-analysis was designed to evaluate the diagnostic accuracy of CUS and chest radiography (CXR) for detection of pneumothorax.
Materials and Methods
The literature search was conducted using PubMed, EMBASE, Cochrane, CINAHL, SUMSearch, Trip databases, and review article references. Eligible articles were defined as diagnostic studies on patients suspected for pneumothorax who underwent chest computed tomography (CT) scan and those assessing the screening role of CUS and CXR.
Results
The analysis showed the pooled sensitivity and specificity of CUS were 0.87 (95% CI: 0.81-0.92; I2= 88.89, P<0.001) and 0.99 (95% CI: 0.98-0.99; I2= 86.46, P<0.001), respectively. The pooled sensitivity and specificity of CXR were 0.46 (95% CI: 0.36-0.56; I2= 85.34, P<0.001) and 1.0 (95% CI: 0.99-1.0; I2= 79.67, P<0.001), respectively. The Meta regression showed that the sensitivity (0.88; 95% CI: 0.82 - 0.94) and specificity (0.99; 95% CI: 0.98 - 1.00) of ultrasound performed by the emergency physician was higher than by non-emergency physician. Non-trauma setting was associated with higher pooled sensitivity (0.90; 95% CI: 0.83 – 0.98) and lower specificity (0.97; 95% CI: 0.95 – 0.99).
Conclusion
The present meta-analysis showed that the diagnostic accuracy of CUS was higher than supine CXR for detection of pneumothorax. It seems that CUS is superior to CXR in detection of pneumothorax, even after adjusting for possible sources of heterogeneity.
Keywords: Pneumothorax, Ultrasonography, Radiography, Diagnostic tests, Routine
INTRODUCTION
Thoracic cavity injuries include 25% of mortalities in traumatic events and are associated with a 40% mortality rate, generally (1, 2). Studies have shown that early diagnosis of such traumas can decrease the mortality rate and the resultant burden, significantly. CT scan with a high priority for detection of chest traumas is the gold standard for diagnosis of thoracic traumas (3–5). Although this diagnostic test has high accuracy, patients undergoing CT scan receive a high radiation dose; thus, it is recommended to use this test only when it is indicated (6–8). In addition, CXR is used as the early diagnostic test in patients with thoracic injuries, yet the accuracy of it is not very high (9–14).
CUS can be a reliable and accurate alternative to CXR. However, diagnostic yield of CUS largely depends on the operator's expertise (15–17). However, structural changes of CUS in recent years have led to higher quality and spatial resolution, resulting in greater accuracy in the critical care and emergency management services (18–23).
One of the most common thoracic injuries is pneumothorax and its early detection in multiple trauma patients is critically important. Several studies have demonstrated the high sensitivity and specificity of CUS (24–28). In this regard, three meta-analyses during the past 5 years showed that the sensitivity and specificity of CUS in diagnosis of pneumothorax varied between 78.6-90.9% and 98.2-99%, respectively (29–31). But, these studies have some limitations such as the small number of included articles, lack of evaluating the inter-study threshold variation, lack of publication bias assessment, and evaluation of only English-language articles. Thus, it seems that another meta-analysis is needed to overcome these limitations. The present systematic review and meta-analysis was designed to evaluate the diagnostic accuracy of CUS and CXR for detection of pneumothorax in comparison with CT scan as the gold standard.
MATERIALS AND METHODS
Search strategy
The study was conducted according to the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) statement providing a detailed guideline of preferred reporting style for systematic reviews and meta-analyses (32). Relevant articles were identified through a literature search of online databases (PubMed, SCOPUS, EMBASE, Cochrane, CINAHL, and Trip databases) with no time or language limitation. The initial search was broad and included the following words: (“ultrasound” or “sonography” or “ultrasonography” or “radiography” or “chest film” or “chest radiograph”) and (“pneumothorax” or “aerothorax”) and (“sensitivity” and “specificity” or “diagnostic accuracy” or “diagnostic yield”). In addition, we ran a hand search in the reference lists of all articles meeting the inclusion criteria and previous meta-analysis studies to find more studies. In addition, it was attempted to contact the authors of all studies that met the inclusion criteria and request unpublished data and abstracts.
Study Selection and Definitions
Two authors (M.Y, H.A) independently reviewed all potentially relevant studies. Disagreements were solved by discussion and using the viewpoint of a third author (A.M.J). We included all diagnostic accuracy studies regarding patients with pneumothorax from all age groups. These studies had to be prospective, blinded, and original comparing the diagnostic value of CUS and CXR for detection of pneumothorax. Studies also compared the two tests with one gold standard (CT scan) and described the diagnostic criteria for pneumothorax in each test, clearly. Those including patients with known pneumothorax and poor quality studies based on the 14-item Quality Assessment of Diagnostic Accuracy Studies (QUADAS2) tool (33) were excluded. Only pneumothorax cases with CT scan verification were included.
Data extraction and management
Two authors (M.Y, H.A) extracted data independently from studies, using a standardized data abstraction form. They collected data related to study design, patient characteristics, CUS diagnosis criteria and operator, CUS transducer, blinding status, and sampling method. The authors were contacted for clarification of study sample, regarding missing or insufficient data, if necessary. In cases of duplicate reporting, data were used from the study on the largest number of patients or individual patient data from each study, if available.
Quality assessment
We assessed the quality of the included studies using the QUADAS2. Two reviewers (MY, HA) independently reviewed each study and rated their quality as “good,” “fair,” or “poor”. Quality assessment was conducted based on criteria of diagnostic studies, accounting for study design and presence of bias including selection, performance, recording, and reporting bias. The studies with high risk of bias were defined as poor quality, presence of moderate risk (did not affect the results) was considered as fair quality, and those with minimal risk as good quality. In this regard, inter-rater reliability was acceptably high (95%). Disagreements were discussed by a third reviewer (A.M.J) and settled with consensus decision.
Data synthesis and statistical analysis
Statistical analysis was performed using STATA software version 12.0 (StataCorp, College Station, TX, USA). After selecting the relevant studies, data were presented as true positive (TP), true negative (TN), false positive (FP), and false negative (FN) values. In cases reported as hemi-thorax by the findings of the study, the authors were contacted to find the total sample size (number of patients). If they did not respond, estimation methods were used to calculate the TP, TN, FP, and FN values using a web based calculator. If the information had been reported in graphs, data extracted from them as recommended by Sistrom et al. (34).
In analyses, the mixed-effects binary regression model was used, a type of random effect model used when the heterogeneity source is not clear. Statistical heterogeneity was measured using the I2 and χ2 tests (P<0.10 was representative of significant statistical heterogeneity) (35). Sensitivity and subgroup analyses were performed to check the expected or measured heterogeneity. The sensitivity analysis was done using studies with good and fair quality levels and applied based on a bivariate meta-regression model. All possible causes of heterogeneity including the operator, ultrasound probe, CUS frequency, study subjects (trauma/non-trauma), CUS signs, and type of sampling (consecutive versus convenience sampling) were included as covariates in the meta-regression model. Publication bias was assessed by funnel plot and associated regression test of asymmetry, introduced by Deeks et al. (36).
To determine whether the patient had pneumothorax, CT scan results were assessed. Patients were divided into two groups: CT positive (CT+: patients with pneumothorax) and CT negative (CT-: patients without any signs of pneumothorax). Finally, the pooled sensitivity and specificity were calculated with 95% confidence intervals (CIs). Diagnostic odds ratio (DOR) and receiver operative curves (ROCs) were also obtained.
RESULTS
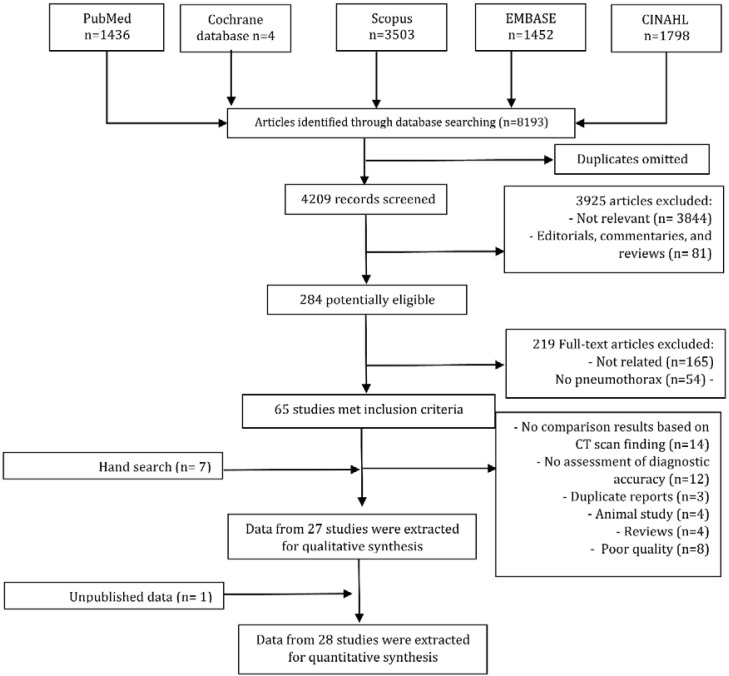
A total of 4,209 non-duplicate citations were identified by using search strategies from which 284 potentially relevant papers were screened. Finally, 65 studies were eligible and 28 full-text articles included in meta-analysis and studied in detail (10, 37–63) (Table 1, Figure 1). These articles totally contained 5,314 patients, 1159 cases with CT scan positive and 4,155 cases with CT scan negative findings. The diagnostic accuracy of CUS and CXR was reported in 28 and 22 studies (10, 37, 39–43, 46–49, 51–59, 62, 63), respectively.
Table 1.
Studies on diagnostic accuracy of ultrasound (US) and chest radiography (CXR) for detection of pneumothorax.
| Study | No. of patients | Age1 (years) | Sex (male, %) | Outcome measure | Transducer / Operator | Sampling / subject | US signs | Results | Limitations | Quality | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity (95%CI) | Specificity (95% CI) | ||||||||||
| Goodman 1999 | 13 PTX+ / 36 PTX- | NP | NP | CT, US, CXR | 7.5 MHz linear / Radiologist | Consecutive / Iatrogenic | LS, CTA | CXR: 46.2 (20.4-73.9) US: 87.5 (46.7-99.3) |
CXR: 100 (88.0-100) US: 100 (89.3-100) |
Small sample size | Fair |
| Lichtenstein 1999 | 41 PTX+ / 146 PTX- | NP | 64.4 | CT, US | 3.5-MHz convex / Emergency physician | Consecutive / ICU | LS, CTA | US: 100 (89.3-100) | US: 98.4 (94.4-99.8) | Small sample size | Fair |
| Rowan 2002 | 11 PTX+ / 27 PTX- | 42 (17-83) | 92.6 | CT, US, CXR | 7 MHz linear / Radiologist | Convenience / Trauma | LS, CTA | CXR: 36.0 (15.0-65.0) US: 100 (74.0-100) |
CXR: 100 (81-100) US: 94.0 (72-99) |
Small sample size Possibility of selection bias | Fair |
| Kirkpatric 2004 | 52 PTX+ / 173 PTX- | NP | NP | CT, US, CXR | 5-10 MHz linear / Surgeon | Convenience / Trauma | LS, CTA | CXR: 20.9 (10.0-36.0) US: 48.8 (33.3-64.5) |
CXR: 99.6 (97.5-100) US: 98.7 (96.1-99.7) |
Possibility of selection bias | Fair |
| Blaivas 2005 | 53 PTX+ / 123 PTX- | NP | 57 | CT, US, CXR | 2 to 4 MHz convex / Emergency physician | Consecutive / Trauma | LS, CTA | CXR: 75.5 (61.7-86.2) US: 98.1 (89.9-99.9) |
CXR 100 (97.1-100) US: 99.2 (95.6-99.9) |
It selected patients who were more severely injured. | Good |
| Chung 2005 | 35 PTX+ / 72 PTX- | NP | NP | CT, US, CXR | 5-12 MHz linear / Radiologist | Convenience / Iatrogenic | LS, CTA | CXR: 47.1 (38.7-55.7) US: 80.0 (72.2-86.1) |
CXR: 93.9 (90.0-96.4) US: 93.9 (90.0-96.4) |
Possibility of selection bias | Fair |
| Rei Big 2005 | 4 PTX+ / 49 PTX- | 64 (NP) | 60.4 | CT, US, CXR | 7.5 MHz linear / Pneumologist | Consecutive / Iatrogenic | LS, CTA, LP | CXR: 75.0 (21.9-98.7) US: 100 (39.6-100) |
CXR:100 (90.1-100) US: 100 (90.1-100) |
Small sample size Small PTX cases |
Fair |
| Lichtenstein 2005 | 32 PTX+ / 146 PTX- | 44 (19) | NP | CT, US | 5 MHz convex / Intensivist | Consecutive / ICU | LS, CTA | US: 95.3 (82.9-99.2) | US: 94.7 (91.4-96.8) | Possibility of selection bias | Fair |
| Garofulo 2006 | 46 PTX+ / 138 PTX- | NP | 70.6 | CT, US | 2.5 MHz convex / Emergency physician | Convenience / Iatrogenic | LS, CTA | US: 95.6 (84.0-100) | US: 100 (96.6-100) | Possibility of selection bias | Fair |
| Soldati 2006 | 56 PTX+ / 130 PTX- | 52.4 (22.9) | 62.9 | CT, US, CXR | 5 MHz Convex / Emergency physician | Consecutive / Trauma | LS, CTA, LP | CXR: 53.6 (39.8-66.8) US: 98.2 (89.2-99.9) |
CXR 100 (96.4-100) US: 100 (96.4-100) |
Inclusion criteria may have introduced bias | Good |
| Zhang 2006 | 29 PTX+ / 106 PTX- | 45(15) | 84.4 | CT, US, CXR | 3.5 to 7.5 MHz linear / Emergency physician | Convenience / Trauma | LS, CTA, LP | CXR: 27.6 (11.3-43.9) US: 86.2 (73.7-98.8) |
CXR: 100 (100-100) US: 97.2 (94.0-100) |
Did not test reproducibility among operators | Good |
| Soldati 2008 | 25 PTX+ / 84 PTX- | 41.4 (20.5) | 62.9 | CT, US, CXR | 5.2 MHz linear / Emergency physician | Consecutive / Trauma | LS, CTA, LP | CXR: 52.0 (31.8-71.7) US: 91.7 (71.5-98.5) |
CXR: 100 (94.6-100) US: 98.8 (92.7-100) |
Inclusion criteria may have introduced bias | Good |
| Brook 2009 | 43 PTX+ / 126 PTX- | 31 (13.2) | 85 | CT, US, CXR | 3.5 MHz linear / Radiologist | Consecutive / Trauma | LS, CTA | CXR: 16.3 (8.1-29.8) US: 46.5 (32.5-61) |
CXR: 100 (98.7-100) US: 99 (97.1-99.7) | Good | |
| Mashayekhian 2010 | 12 PTX+ / 48 PTX- | 36.5 (17.7) | 90 | CT, US | 7.5 MHz Linear / Emergency physician | Consecutive / Trauma | LS, CTA, LP | US: 91.7 (59.8-99.6) | US: 100 (90.8-100) | Small sample size Moderate quality of US set. |
Fair |
| Nagarsheth 2011 | 22 PTX+ / 57 PTX- | 44.5 (15.3) | 66. 4 | CT, US, CXR | 2.5 MHz convex / Surgeon | Convenience / Trauma | LS, CTA, LP | CXR: 31.8 (14.7-54.9) US: 81.8 (59.0-94.0) |
CXR: 100 (92.1-100] US: 100 (92.1-100) |
Possibility of selection bias | Fair |
| Nandipati 2011 | 21 PTX+ / 183 PTX- | 43 (19.5) | 74.5 | CT, US, CXR | 7.5 MHz linear / Emergency physician | Convenience / Trauma | LS, CTA | CXR: 78.9 (53.9-93.0) US: 95.2 (74.1-99.8) |
CXR: 99.4 (96.5-100) US: 99.4 (96.5-100) |
Possibility of selection bias | Fair |
| Xirouchaki 2011 | 8 PTX+ / 76 PTX- | 57.1 (21.5) | 90.5 | CT, US, CXR | 5 to 10 MHz Convex / Intensivist | Convenience / ICU | LS, CTA, LP | CXR: 0.0 (0.37) US: 75.0 (35.0-97.0) |
CXR: 99 (93-100) US: 93.0 (85-98) |
Possibility of selection bias. Small sample size. Time interval between lung ultrasound and CT could not be controlled. |
Fair |
| Donmez, 2012 | 33 PTX+ / 34 PTX- | NP | NP | CT, US, CXR | 5-MHz linear / Radiologist | Convenience / Trauma | LS, CTA | CXR: 82.6 (63.5-93.5) US: 91.4 (75.8-97.8) |
CXR: 100 (82.0-100) US: 97.0 (90.9-99.2) |
Small sample size Possibility of selection bias |
Fair |
| Hyacinthe 2012 | 53 PTX+ / 66 PTX- | 39 (22-51) | 82.0 | CT, US, CXR | 5.2 MHz Convex / Emergency physician | Consecutive / Trauma | LS, CTA, LP | CXR: 18.9 (9.9-32.4) US: 52.8 (38.8-66.5) |
CXR: 100 (93.1-100) US: 95.4 (86.4-98.8) |
Did not test reproducibility among operators. Diagnostic value of radiography was considered with physical examination as a whole |
Fair |
| Abbasi 2013 | 37 PTX+ / 109 PTX- | 37(14) | 87.6 | CT, US, CXR | 7.5 MHz linear / Emergency physician | Convenience / Trauma | LS, CTA | CXR: 48.64 (32.2-65.3) US: 86.4 (70.4-94.9) |
CXR: 100 (95.7-100) US: 100 (95.7-100) |
Possibility of selection bias | Fair |
| Jalli 2013 | 92 PTX+ / 105 PTX- | NP | NP | CT, US, CXR | 7.5 MHz linear / Radiologist | Consecutive / Respiratory problems | LS, CTA | CXR: 60.7 (50.1-70.7) US: 80.4 (70.6-87.7) |
CXR: 98.1 (92.6-99.7) US: 89.5 (81.6-94.4) |
The use of upright CXR in some patients. US exams were performed with in 48 h after the chest CT scan acquisition. |
Fair |
| Karimi 2013 | 72 PTX+ / 68 PTX- | 39.4 (15.8) | 62 | CT, US, CXR | 7.5 MHz linear / Emergency physician | Consecutive / Trauma | LS, CTA | CXR: 75.3 (63.6-84.4) US: 84.9 (74.2-91.9) |
CXR: 98.5 (90.1-99.9) US: 95.5 (86.6-98.9) |
The time interval between CT scan accusation and US was not clear. | Good |
| Ku 2013 | 47 PTX+ / 502 PTX- | NP | 75 | CT, US, CXR | 2 to 4 MHz linear / Emergency physician | Convenience / Trauma | LS, CTA | CXR: 40 (23-59) US: 57 (42-72) |
CXR: 100 (99-100) US: 99(98-100) |
Possibility of selection bias Possible misclassification bias | Fair |
| Shostak 2013 | 8 PTX+ / 177 PTX- | 67 (23-92) | 47.2 | CT, US | 5 to 10 MHz convex / Radiologist or clinical investigator | Convenience / Iatrogenic | LS, CTA | Radiologist: US: 75 (35-90) Clinical investigator: US: 88 (35-90) |
Radiologist: US: 97 (93-98) Clinical investigator: US: 97 (93-98) |
Possibility of selection bias Low prevalence of pneumothorax. |
Fair |
| Uz 2013 | 33 PTX+ / 74 PTX- | 36.7 (19.8) | 80.4 | CT, US | 5-10 MHz linear / radiologist | Consecutive / Trauma | LS, CTA, LP | US: 81.8 (68-95.5) | US: 100 (93.8-100) | Small sample size. | Fair |
| Ianniello 2014(1) | 87 PTX+ / 649 PTX- | 25(16-68) | 74.2 | CT, US | 7.5 MHz linear / Radiologist | Consecutive / Trauma | LS, CTA | US: 77.0 (66.5-85.1) | US: 98.5 (97.1-99.2) | ----- | Good |
| Ojaghi Haghighi 2014 | 52 PTX+ / 98 PTX- | NP | 82.7 | CT, LS, CXR | 6.5 to 9 MHz linear / Emergency physician | Convenience / Trauma | LS, CTA | CXR: 34.7 (27.2-42.9) US: 96.2 (85.7-99.3) |
CXR: 98 (92.1-99.6) US: 100 (95.3-100) |
Possibility of selection bias. | Fair |
| Vafaie 2014 | 48 PTX+ / 102 PTX- | 31.4 (13.8) | 77.6 | CT, US, CXR | 7.5 MHz linear / Emergency physician | Consecutive / Trauma | LS, CTA | CXR: 67.3 (53.26-78.9) US: 83.6 (70.7-91.8) |
CXR: 98 (92.1-99.6) US: 92.7 (85.1-96.8) |
CXR examinations were done in upright position. | Good |
Numbers are presented as mean (standard deviation or range); CI: Confidence interval; CT: Computed tomography; CTA: Comet-tail artifact; CXR: Chest radiography; ICU: Intensive care unit; L.P: Lung point; LS: Lung sliding; NP: Not presented; PTX: Pneumothorax; US: Ultrasound
Figure 1.
Flow chart of the study. Diagram represents the review process and selection of included studies
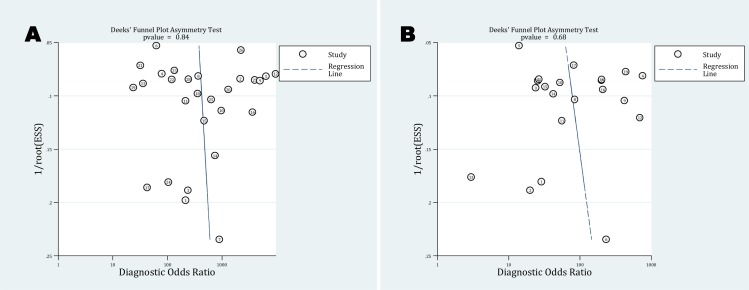
A bivariate mixed-effects binary regression model was used for performing analyses, because a significant statistical heterogeneity was found in diagnosis of pneumothorax. No publication bias was observed among included studies (P=0.84 for CUS, P=0.68 for CXR) (Figure 2).
Figure 2.
Deeks’ funnel plot for publication bias assessment of CUS (A) and CXR (B) for diagnosis of pneumothorax
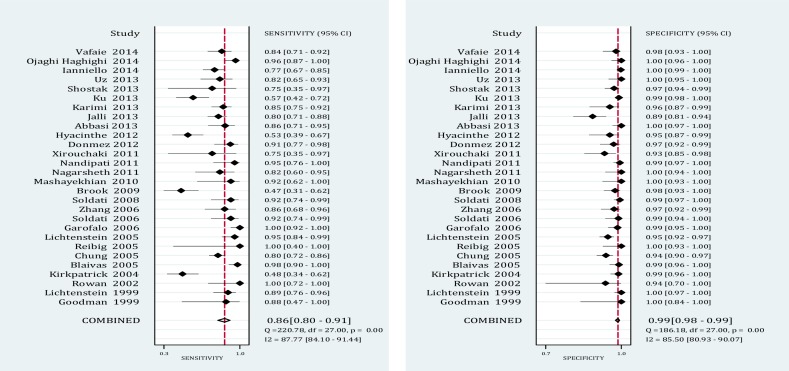
The analysis showed the pooled sensitivity and specificity of thoracic CUS were 0.87 (95% CI: 0.81-0.92; I2= 88.89, P<0.001) and 0.99 (95% CI: 0.98-0.99; I2= 86.46, P<0.001), respectively. The pooled sensitivity and specificity of CXR were 0.46 (95% CI: 0.36-0.56; I2= 85.34, P<0.001) and 1.0 (95% CI: 0.99-1.0; I2= 79.67, P<0.001), respectively (Figures 3 and 4).
Figure 3.
Forest plot for sensitivity and specificity of CUS for diagnosis of pneumothorax.
Figure 4.
Forest plot for sensitivity and specificity of CUS for detection of pneumothorax.
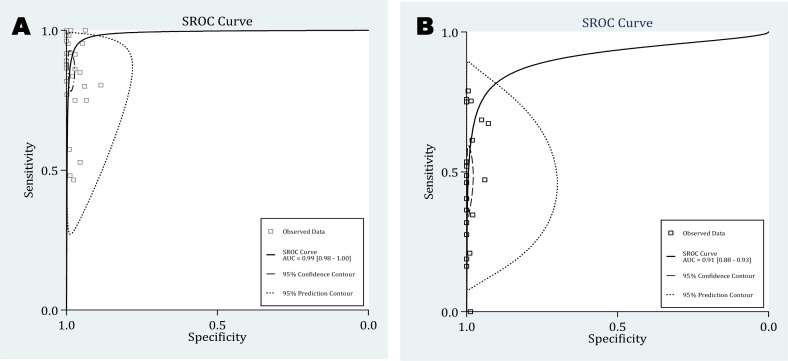
The pooled DOR for CUS was 465.52 (95% CI, 216.37 to 1001.56; I2= 100.0, P<0.001), whereas for CXR it was 179.75 (95% CI, 52.24 to 564.45; I2= 100.0, P<0.001) (Figure 5). The summary receiver operating characteristic (SROC) curves for CUS and CXR are presented in Figure 5. The AUC for CUS and CXR was 0.99 (95% CI: 0.98-1.0) and 0.91 (95% CI: 0.88-0.93), respectively (Figure 6).
Figure 5.
Forest plot for diagnostic odds ratio (DOR) of US (A) and CXR (B).
Figure 6.
Summary receiver operative curves for US (A) and CXR (B). AUC, Area under the curve
The subgroup analysis showed that ultrasound being performed by an emergency/non-emergency physician and the trauma/non trauma settings were the main possible sources of heterogeneity. The meta regression showed that the sensitivity (0.88; 95% CI: 0.82 - 0.94) and specificity (0.99; 95% CI: 0.98 - 1.0) of ultrasound were higher when it was performed by an emergency physician. In addition, non-trauma setting was associated with higher pooled sensitivity (0.90; 95% CI: 0.83 – 0.98) and lower specificity (0.97; 95% CI: 0.95 – 0.99). The possible source of heterogeneity in CXR findings was not specified in the analysis (Table 2).
Table 2.
Heterogeneity in the pooled sensitivity and specificity of chest radiography or ultrasound for detection of pneumothorax
| Covariate | Bivariate random-effect model | |||
|---|---|---|---|---|
|
|
||||
| Sensitivity | Specificity | I2 statistics | P value | |
| Thoracic ultrasonography | ||||
| Patient enrollment | ||||
| Consecutive | 0.87 (0.81-0.94) | 0.99 (0.98-1.0) | 0 | |
| Nonconsecutive | 0.85 (0.77-0.93) | 0.98 (0.97-1.0) | 0 | 0.66 |
| Patient type | ||||
| Trauma | 0.85 (0.78-0.91) | 0.99 (0.99-1.0) | 76 | <0.02 |
| Non trauma | 0.90 (0.83-0.98) | 0.97 (0.95-0.99) | 46 | |
| Operator | ||||
| Emergency physician | 0.88 (0.82-0.94) | 0.99 (0.98-0.1.0) | 86 | <0.001 |
| Non-emergency physician | 0.81 (0.73-0.90) | 0.98 (0.96-0.99) | 71 | |
| Probe type | ||||
| Linear | 0.85 (0.78-0.92) | 0.99 (0.98-1.0) | 0 | 0.74 |
| Nonlinear | 0.88 (0.81-0.95) | 0.98 (0.97-1.0) | 0 | |
| Frequency | ||||
| 2-5 Mhz | 0.87 (0.81-0.92) | 0.98 (0.97-0.99) | 0 | 0.4 |
| 5-10 Mhz | 0.86 (0.75-0.97) | 0.99 (0.98-1.0) | 0 | |
| Chest radiography | ||||
| Patient enrollment | ||||
| Consecutive | 0.46 (0.35-0.77) | 1.0 (0.99-1.0) | 6 | |
| Nonconsecutive | 0.44 (0.22-0.66) | 0.99 (0.96-1.0) | 0 | 0.35 |
| Patient type | ||||
| Trauma | 0.46 (0.35-0.57) | 0.99 (0.96-1.0) | 36 | 0.21 |
| Non trauma | 0.44 (0.22-0.66) | 1.0 (0.99-1.0) | 0 | |
DISCUSSION
The present meta-analysis declared that the diagnostic accuracy of CUS was higher than that of supine CXR for detection of pneumothorax. Overall, it seems that CUS is superior to CXR for detection of pneumothorax, even after adjusting for possible sources of heterogeneity (the lowest CUS subgroup sensitivity was 0.81). The odds of accurate diagnosis of pneumothorax by CUS (DOR= 465.52) were significantly higher than CXR (the pooled DOR was 179.75). The non-trauma setting and performing CUS by emergency physician were associated with higher sensitivity of ultrasound in diagnosis of pneumothorax. It may be explained by the fact that the emergency physician was aware of the patient's clinical condition, the injury site, and the mechanism of injury.
A meta-analysis done by Alrajab et al., who reviewed 13 studies, demonstrated a pooled sensitivity of 78.6% and specificity of 98.4% for CUS, while these rates were 39.8% and 99.3% for CXR, respectively (30). Their findings were lower in value than the two previous studies performed by Ding et al. and Alrajhi and colleagues (29, 31). Ding et al. included 15 articles in their analysis and showed that CUS had a pooled sensitivity and specificity of 88% and 99%, respectively (29). Alrajhi et al. included 8 studies in their analysis and declared 90.9% sensitivity and 98.2% specificity for CUS (31). The two latest meta-analyses were in concordance with the present meta-analysis. However, all three mentioned meta-analyses had some limitations. The first limitation was the small number of articles included in their analyses. The second one was lack of publication bias assessment. The third one was that they only considered English-language articles, which may lead to possible publication bias.
On the other hand, we performed an extensive search in several databases to include the maximum number of relevant studies. No language limitation was another advantage of our study. This search strategy led to finding 28 relevant articles. In addition, in the present meta-analysis there was no publication bias. However, our meta-analysis had a number of potential limitations. First, all the included studies were observational so that causal relationships could not be established. Moreover, residual confounders (confounders from unknown variables) might introduce some biases, as in any meta-analysis of observational studies. One of the residual confounders in the present meta-analysis is the operator-dependent nature of CUS accuracy. The quality of operator training is another possible confounding factor, which has not yet been paid attention in included studies. The direction of this bias is unpredictable. Moreover, the heterogeneity between studies was another issue. Therefore, it was decided to use a bivariate mixed random effects model to provide more conservative results.
CONCLUSION
The present meta-analysis showed that the diagnostic accuracy of CUS was higher than that of supine CXR for detection of pneumothorax. It seems that CUS is superior to CXR for detection of pneumothorax, even after adjusting for possible sources of heterogeneity.
REFERENCES
- 1.Hill A, Fowler R, Pinto R, Nathens A. Epidemiology of major trauma: a Canadian perspective. Canadian Journal of Surgery. 2011;54(3):S45. [Google Scholar]
- 2.Heron M. Deaths: leading causes for 2008. Natl Vital Stat Rep. 2012;60(6):1–94. [PubMed] [Google Scholar]
- 3.Danielsen M, Højgaard L, Kjær A, Fischer BM. Positron emission tomography in the follow-up of cutaneous malignant melanoma patients: a systematic review. Am J Nucl Med Mol Imaging. 2013;4(1):17–28. [PMC free article] [PubMed] [Google Scholar]
- 4.Schulze C, Hoppe H, Schweitzer W, Schwendener N, Grabherr S, Jackowski C. Rib fractures at postmortem computed tomography (PMCT) validated against the autopsy. Forensic Sci Int. 2013;233(1-3):90–8. doi: 10.1016/j.forsciint.2013.08.025. [DOI] [PubMed] [Google Scholar]
- 5.Esmailian M, Zargarbashi EH, Masoumi B, Karami M. Accuracy of Ultrasonography in Confirmation of Adequate Reduction of Distal Radius Fractures. Emergency. 2013;1(1):7–10. [PMC free article] [PubMed] [Google Scholar]
- 6.Brenner DJ. Medical imaging in the 21st century--getting the best bang for the rad. N Engl J Med. 2010;362(10):943–5. doi: 10.1056/NEJMe1000802. [DOI] [PubMed] [Google Scholar]
- 7.Lee J, Kirschner J, Pawa S, Wiener DE, Newman DH, Shah K. Computed tomography use in the adult emergency department of an academic urban hospital from 2001 to 2007. Ann Emerg Med. 2010;56(6):591–6. doi: 10.1016/j.annemergmed.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 8.Holmes JF, Wisner DH, McGahan JP, Mower WR, Kuppermann N. Clinical prediction rules for identifying adults at very low risk for intra-abdominal injuries after blunt trauma. Ann Emerg Med. 2009;54(4):575–84. doi: 10.1016/j.annemergmed.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010;17(1):11–7. doi: 10.1111/j.1553-2712.2009.00628.x. [DOI] [PubMed] [Google Scholar]
- 10.Xirouchaki N, Magkanas E, Vaporidi K, Kondili E, Plataki M, Patrianakos A, et al. Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensive Care Med. 2011;37(9):1488–93. doi: 10.1007/s00134-011-2317-y. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez RM, Hendey GW, Marek G, Dery RA, Bjoring A. A pilot study to derive clinical variables for selective chest radiography in blunt trauma patients. Ann Emerg Med. 2006;47(5):415–8. doi: 10.1016/j.annemergmed.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Sears BW, Luchette FA, Esposito TJ, Dickson EL, Grant M, Santaniello JM, et al. Old fashion clinical judgment in the era of protocols: is mandatory chest X-ray necessary in injured patients? J Trauma. 2005;59(2):324–30. doi: 10.1097/01.ta.0000179450.01434.90. discussion 330-2. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez RM, Anglin D, Langdorf MI, Baumann BM, Hendey GW, Bradley RN, et al. NEXUS chest: validation of a decision instrument for selective chest imaging in blunt trauma. JAMA Surg. 2013;148(10):940–6. doi: 10.1001/jamasurg.2013.2757. [DOI] [PubMed] [Google Scholar]
- 14.Forouzanfar MM, Safari S, Niazazari M, Baratloo A, Hashemi B, Hatamabadi HR, et al. Clinical decision rule to prevent unnecessary chest X-ray in patients with blunt multiple traumas. Emerg Med Australas. 2014;26(6):561–6. doi: 10.1111/1742-6723.12302. [DOI] [PubMed] [Google Scholar]
- 15.Poletti PA, Kinkel K, Vermeulen B, Irmay F, Unger PF, Terrier F. Blunt abdominal trauma: should US be used to detect both free fluid and organ injuries? Radiology. 2003;227(1):95–103. doi: 10.1148/radiol.2271020139. [DOI] [PubMed] [Google Scholar]
- 16.Ojaghi Haghighi SH, Morteza Begi HR, Sorkhabi R, et al. Diagnostic Accuracy of Ultrasound in Detection of Traumatic Lens Dislocation. Emergency. 2014;2(3):121–4. [PMC free article] [PubMed] [Google Scholar]
- 17.Heydari F, Esmailian M, Dehghanniri M. Diagnostic Accuracy of Ultrasonography in the Initial Evaluation of Patients with Penetrating Chest Trauma. Emergency. 2014;2(2):81–4. [PMC free article] [PubMed] [Google Scholar]
- 18.Zarain Obrador L, Al-Lal YM, de Tomás Palacios J, Amunategui Prats I, Turégano Fuentes F. Transmediastinal and transcardiac gunshot wound with hemodynamic stability. Case Rep Surg. 2014;2014:985097. doi: 10.1155/2014/985097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xirouchaki N, Kondili E, Prinianakis G, Malliotakis P, Georgopoulos D. Impact of lung ultrasound on clinical decision making in critically ill patients. Intensive Care Med. 2014;40(1):57–65. doi: 10.1007/s00134-013-3133-3. [DOI] [PubMed] [Google Scholar]
- 20.Williams SR, Perera P, Gharahbaghian L. The FAST and E-FAST in 2013: trauma ultrasonography: overview, practical techniques, controversies, and new frontiers. Crit Care Clin. 2014;30(1):119–50, vi. doi: 10.1016/j.ccc.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 21.Wagner MS, Garcia K, Martin DS. Point-of-care ultrasound in aerospace medicine: known and potential applications. Aviat Space Environ Med. 2014;85(7):730–9. doi: 10.3357/asem.3754.2014. [DOI] [PubMed] [Google Scholar]
- 22.Volpicelli G. Point-of-care lung ultrasound. Praxis (Bern 1994) 2014;103(12):711–6. doi: 10.1024/1661-8157/a001690. [DOI] [PubMed] [Google Scholar]
- 23.See KC, Ong V, Teoh CM, Ooi OC, Widjaja LS, Mujumdar S, et al. Bedside pleural procedures by pulmonologists and non-pulmonologists: a 3-year safety audit. Respirology. 2014;19(3):396–402. doi: 10.1111/resp.12244. [DOI] [PubMed] [Google Scholar]
- 24.Barbara DW. Bedside Lung Ultrasonography: A Tool for Rapid Assessment of Pneumothorax. Anesthesiology. 2014 doi: 10.1097/ALN.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 25.Aspler A, Pivetta E, Stone MB. Double-lung point sign in traumatic pneumothorax. Am J Emerg Med. 2014;32(7):e1–2. doi: 10.1016/j.ajem.2013.12.059. 819. [DOI] [PubMed] [Google Scholar]
- 26.Kline JP, Dionisio D, Sullivan K, Early T, Wolf J, Kline D. Detection of pneumothorax with ultrasound. AANA J. 2013;81(4):265–71. [PubMed] [Google Scholar]
- 27.Fankhauser GT, Fowl RJ, Stone WM, Money SR. Elimination of pneumothorax and hemothorax during placement of implantable venous access ports using ultrasound and fluoroscopic guidance. Vascular. 2013 doi: 10.1177/1708538112472279. [DOI] [PubMed] [Google Scholar]
- 28.Tang H, Pan T, Qin X, Xue L, Wu B, Zhao X, et al. A portable thoracic closed drainage instrument for hemopneumothorax. J Trauma Acute Care Surg. 2012;72(3):671–5. doi: 10.1097/TA.0b013e3182277857. [DOI] [PubMed] [Google Scholar]
- 29.Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest. 2011;140(4):859–66. doi: 10.1378/chest.10-2946. [DOI] [PubMed] [Google Scholar]
- 30.Alrajab S, Youssef AM, Akkus NI, Caldito G. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care. 2013;17(5):R208. doi: 10.1186/cc13016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alrajhi K, Woo MY, Vaillancourt C. Test characteristics of ultrasonography for the detection of pneumothorax: a systematic review and meta-analysis. Chest. 2012;141(3):703–8. doi: 10.1378/chest.11-0131. [DOI] [PubMed] [Google Scholar]
- 32.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 33.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 34.Sistrom CL, Mergo PJ. A simple method for obtaining original data from published graphs and plots. AJR Am J Roentgenol. 2000;174(5):1241–4. doi: 10.2214/ajr.174.5.1741241. [DOI] [PubMed] [Google Scholar]
- 35.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58(9):882–93. doi: 10.1016/j.jclinepi.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 37.Goodman TR, Traill ZC, Phillips AJ, Berger J, Gleeson FV. Ultrasound detection of pneumothorax. Clin Radiol. 1999;54(11):736–9. doi: 10.1016/s0009-9260(99)91175-3. [DOI] [PubMed] [Google Scholar]
- 38.Lichtenstein D, Mezière G, Biderman P, Gepner A. The comet-tail artifact: an ultrasound sign ruling out pneumothorax. Intensive Care Med. 1999;25(4):383–8. doi: 10.1007/s001340050862. [DOI] [PubMed] [Google Scholar]
- 39.Rowan KR, Kirkpatrick AW, Liu D, Forkheim KE, Mayo JR, Nicolaou S. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT--initial experience. Radiology. 2002;225(1):210–4. doi: 10.1148/radiol.2251011102. [DOI] [PubMed] [Google Scholar]
- 40.Kirkpatrick AW, Sirois M, Laupland KB, Liu D, Rowan K, Ball CG, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST) J Trauma. 2004;57(2):288–95. doi: 10.1097/01.ta.0000133565.88871.e4. [DOI] [PubMed] [Google Scholar]
- 41.Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12(9):844–9. doi: 10.1197/j.aem.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 42.Chung MJ, Goo JM, Im JG, Cho JM, Cho SB, Kim SJ. Value of high-resolution ultrasound in detecting a pneumothorax. Eur Radiol. 2005;15(5):930–5. doi: 10.1007/s00330-004-2518-7. [DOI] [PubMed] [Google Scholar]
- 43.Reissig A, Kroegel C. Accuracy of transthoracic sonography in excluding post-interventional pneumothorax and hydropneumothorax. Comparison to chest radiography. Eur J Radiol. 2005;53(3):463–70. doi: 10.1016/j.ejrad.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 44.Lichtenstein DA, Mezière G, Lascols N, Biderman P, Courret JP, Gepner A, et al. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005 Jun;33(6):1231–8. doi: 10.1097/01.ccm.0000164542.86954.b4. [DOI] [PubMed] [Google Scholar]
- 45.Garofalo G, Busso M, Perotto F, De Pascale A, Fava C. Ultrasound diagnosis of pneumothorax. Radiol Med. 2006;111(4):516–25. doi: 10.1007/s11547-006-0047-y. [DOI] [PubMed] [Google Scholar]
- 46.Soldati G, Testa A, Pignataro G, Portale G, Biasucci DG, Leone A, et al. The ultrasonographic deep sulcus sign in traumatic pneumothorax. Ultrasound Med Biol. 2006;32(8):1157–63. doi: 10.1016/j.ultrasmedbio.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 47.Zhang M, Liu ZH, Yang JX, Gan JX, Xu SW, You XD, et al. Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Crit Care. 2006;10(4):R112. doi: 10.1186/cc5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Soldati G, Testa A, Sher S, Pignataro G, La Sala M, Silveri NG. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest. 2008;133(1):204–11. doi: 10.1378/chest.07-1595. [DOI] [PubMed] [Google Scholar]
- 49.Brook OR, Beck-Razi N, Abadi S, Filatov J, Ilivitzki A, Litmanovich D, et al. Sonographic detection of pneumothorax by radiology residents as part of extended focused assessment with sonography for trauma. J Ultrasound Med. 2009;28(6):749–55. doi: 10.7863/jum.2009.28.6.749. [DOI] [PubMed] [Google Scholar]
- 50.Mashayekhian M, Abbasi S, Farsi D, et al. Evaluation Of The Accuracy Of Bedside Ultrasonography In The Diagnosis Of Pneumothorax In Suspicious Cases Admitted In Hazrate-Rasool Akram Hospital During 2008. Razi J Med Sci. 2010;17(77):67–73. In Persian. [Google Scholar]
- 51.Nagarsheth K, Kurek S. Ultrasound detection of pneumothorax compared with chest X-ray and computed tomography scan. Am Surg. 2011;77(4):480–4. [PubMed] [Google Scholar]
- 52.Nandipati KC, Allamaneni S, Kakarla R, Wong A, Richards N, Satterfield J, et al. Extended focused assessment with sonography for trauma (EFAST) in the diagnosis of pneumothorax: experience at a community based level I trauma center. Injury. 2011;42(5):511–4. doi: 10.1016/j.injury.2010.01.105. [DOI] [PubMed] [Google Scholar]
- 53.Donmez H, Tokmak TT, Yildirim A, Buyukoglan H, Ozturk M, Yaşar Ayaz U, et al. Should bedside sonography be used first to diagnose pneumothorax secondary to blunt trauma? J Clin Ultrasound. 2012;40(3):142–6. doi: 10.1002/jcu.21884. [DOI] [PubMed] [Google Scholar]
- 54.Hyacinthe AC, Broux C, Francony G, Genty C, Bouzat P, Jacquot C, et al. Diagnostic accuracy of ultrasonography in the acute assessment of common thoracic lesions after trauma. Chest. 2012;141(5):1177–83. doi: 10.1378/chest.11-0208. [DOI] [PubMed] [Google Scholar]
- 55.Abbasi S, Farsi D, Hafezimoghadam P, Fathi M, Zare MA. Accuracy of emergency physician-performed ultrasound in detecting traumatic pneumothorax after a 2-h training course. Eur J Emerg Med. 2013;20(3):173–7. doi: 10.1097/MEJ.0b013e328356f754. [DOI] [PubMed] [Google Scholar]
- 56.Jalli R, Sefidbakht S, Jafari SH. Value of ultrasound in diagnosis of pneumothorax: a prospective study. Emerg Radiol. 2013;20(2):131–4. doi: 10.1007/s10140-012-1091-7. [DOI] [PubMed] [Google Scholar]
- 57.Karimi E, Safari S, Shekarchi B. Evaluation of the accuracy of portable ultrasound (eFAST) for detection of pneumothorax. J Army Univ Med Sci. 2013;11(3):225–30. in persian. [Google Scholar]
- 58.Ku BS, Fields JM, Carr B, Everett WW, Gracias VH, Dean AJ. Clinician-performed Beside Ultrasound for the Diagnosis of Traumatic Pneumothorax. West J Emerg Med. 2013;14(2):103–8. doi: 10.5811/westjem.2012.12.12663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shostak E, Brylka D, Krepp J, Pua B, Sanders A. Bedside sonography for detection of postprocedure pneumothorax. J Ultrasound Med. 2013;32(6):1003–9. doi: 10.7863/ultra.32.6.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Uz I, Yürüktümen A, Boydak B, Bayraktaroğlu S, Ozçete E, Cevrim O, et al. Impact of the practice of “Extended Focused Assessment with Sonography for Trauma” (e-FAST) on clinical decision in the emergency department. Ulus Travma Acil Cerrahi Derg. 2013;19(4):327–32. doi: 10.5505/tjtes.2013.23326. [DOI] [PubMed] [Google Scholar]
- 61.Ianniello S, Di Giacomo V, Sessa B, Miele V. First-line sonographic diagnosis of pneumothorax in major trauma: accuracy of e-FAST and comparison with multidetector computed tomography. Radiol Med. 2014;119(9):674–80. doi: 10.1007/s11547-014-0384-1. [DOI] [PubMed] [Google Scholar]
- 62.Ojaghi Haghighi SH, Adimi I, Shams Vahdati S, Sarkhoshi Khiavi R. Ultrasonographic diagnosis of suspected hemopneumothorax in trauma patients. Trauma Mon. 2014;19(4):e17498. doi: 10.5812/traumamon.17498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vafaei A, Hatamabadi HR, Heidary K, Tarbiyat M. Diagnostic Accuracy of Ultrasound and Radiography in Comparison to Computer Tomography Scan in Initial Evaluation of Patients with Chest Traumas; 2014. [Unpublished data] [Google Scholar]