Abstract
Ependymomas are glial tumors derived from ependymal cells lining the ventricles and the central canal of the spinal cord. Two thirds of ependymomas arise in the infratentorial or intraventricles, whereas one-third are located in supratentorial space. But supratentorial “cortical” ependymomas are very rare. We report a case of a cortical ependymoma in a 17-year-old boy. The patient presented with transient recurrent right weakness and diplopia. This tumor was located in the left parieto-occipital region and he had gross total excision. Microscopy and immunohistochemistry showed grade III differentiation ependymoma.
Keywords: Brain tumor, ependymoma, supratentorial
INTRODUCTION
Ependymomas are rare neuroectodermal tumors arising from ependymal cells of the ventricular system, choroid plexus, filum terminale, or central canal of the spinal cord and most frequently affect children and young adults. Ependymomas constitute 1.2% to 7.8% of all intracranial neoplasms or 2% to 6% of all gliomas.[1,2,3] Ependymomas are frequently infratentorial, and a third of ependymomas are supratentorial. Supratentorial ependymomas outside the ventricular system as a distinct location are infrequent.[4] As reported in some articles, ectopic ependymoma can arise in the supratentorial parenchyma with no attachment to the ventricular system.[4] However, these are very rare and reported in only a few cases in the literature.[2] Ependymomas may manifest at any age with no gender predilection. Besides posterior fossa ependymoma arises most often in children (mean age, 6 years), supratentorial ependymoma generally manifests in an older age group (mean age, 18-24 years).[5] We present a case of an 17-year-old boy with a large supratentorial cortical ependymoma with prominent edema manifested as weakness and diplopia.
CASE REPORT
A 17-year-old right-handed boy was admitted to our unit with complaints of repetitive transient right leg weakness and diplopia lasting 2 weeks. The patient did not have any remarkable history, including no history of headache or seizure. His systemic examination was normal. The child did not show abnormalities in the neurologic examinations and the sensorimotor and gait assessments were also normal. Routine laboratory investigations were normal. Magnetic resonance imaging (MRI) showed a large mural nodule-enhanced in the left parieto-occipital region with a central cyst [Figures 1 and 2]. Spinal MRI was normal.
Figure 1.
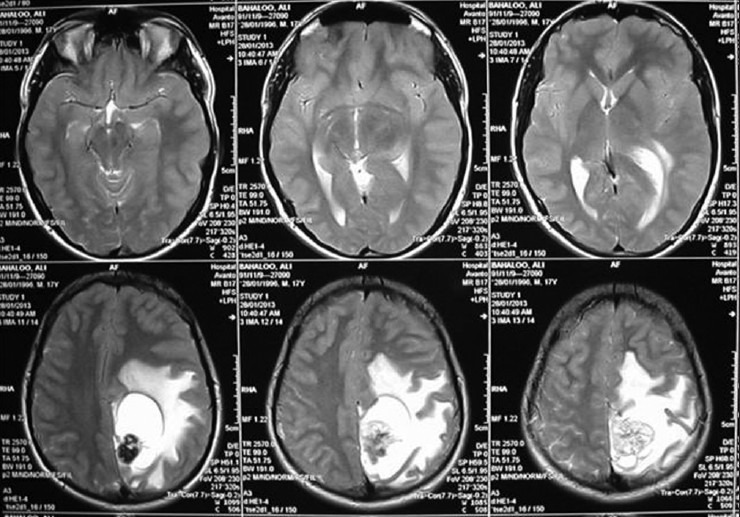
T2 MR images of the patient showing a cyst with mural nodule in the left parieto-occipital region with prominent edema
Figure 2.
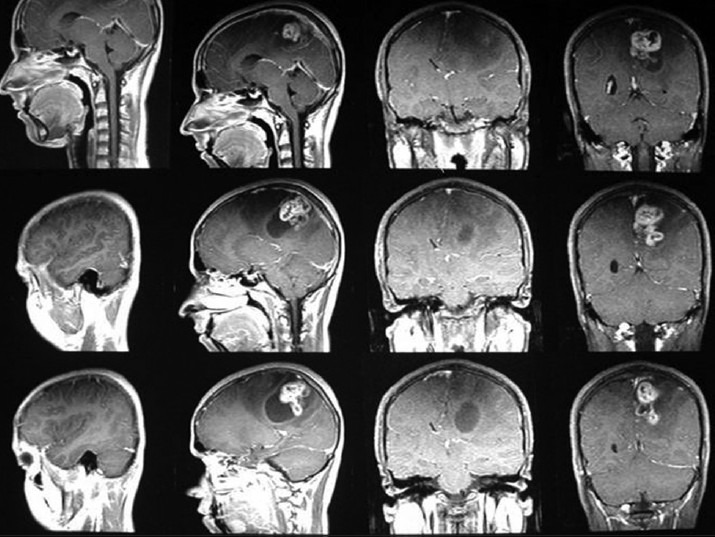
T1 contrast MR images of the patient showing a cyst with enhancing mural nodule in the left parieto-occipital region. Note that there is no communication of the ventricle
Surgical resection of the mass was planned, and the patient underwent total resection of the tumor, which was located in the parenchyma with no dural attachment. The tumor was clearly demarcated and dissected from the surrounding brain parenchyma. The surgical findings suggested no relationship with the lateral ventricular system. Histological examination of the tumor demonstrated perivascular pseudorosette formation, high mitosis index, massive calcification and clear cell, and immunocytochemical positive reactivity for glial fibrillary acidic protein (GFAP), vimentin and epithelial membrane antigen (EMA), but not synaptophysin [Figure 3].
Figure 3.
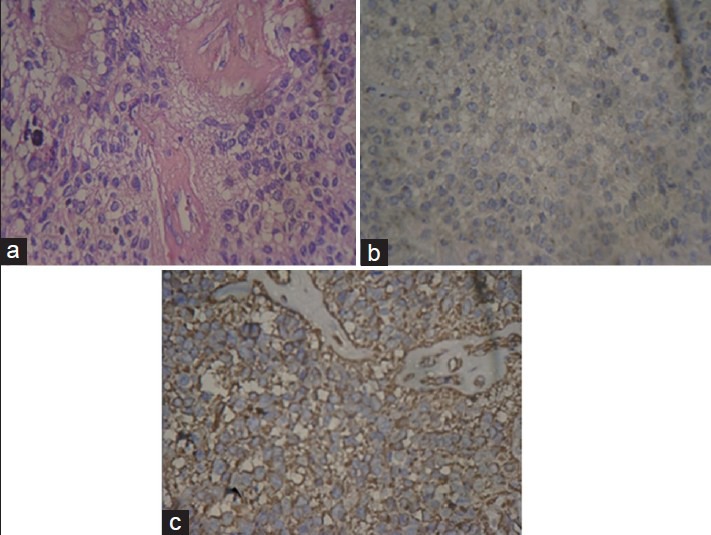
(a) Uniform cells with large nuclei and clear halo around the nuclei, (b) dot-like pattern for EMA and (c) positive reaction for vimentin
These findings were compatible with ependymoma, World Health Organization grade 3. The patient made a good recovery and had no neurologic deficiency. He did not have any seizure episodes after the surgery.
DISCUSSION
Although approximately half of the supratentorial ependymomas arise from ependymal cells of the ventricular system or choroid plexus and are purely intraventricular, the remaining has extension through adjacent cerebral tissue, representing extraventricular forms of ependymoma. Only few cases occur in distant places of the ventricular system, representing rare cases of ectopic lesions (Purely Cortical ependymoma).[6] Van Gompel et al.[7] report of 202 cases of ependymoma (Between 1997 and 2009 at the Mayo Clinic hospital). Among these, nine purely cortical ependymoma cases were retrospectively identified. The pure cortical ependymomas may arise from embryonic rests of ependymal tissue trapped in the developing cerebral hemispheres.[5] The supratentorial ependymoma tends to be larger in size at the time of diagnosis. Roncaroli et al.[6] found that 94% of supratentorial ependymomas manifest with a size larger than 4 cm and often contain a mixed solid and cystic component.[6,8] Despite their large size in the cerebral hemispheres, symptoms are relatively mild until a later stage of presentation.[5,9] Cortical ependymomas frequently, but not always, present with seizures, and despite their high association with epilepsy, are distinctly uncommon in the temporal lobe.[4,6,10,11,12,13,14] In nine purely cortical ependymoma cases of mayo clinic series, five cases arose from the frontal, three cases arose from the parietal, and one case arose from the occipital lobes. No tumor occurred in the temporal lobe, despite its reported association with seizures. The mean age at presentation was 27 years. The mean size of the lesion was 16 ± 14 cm≥.[7] Our patient did not have any seizure. The principal differential diagnosis of pure cortical ependymoma should include astrocytoma (both low grade and glioblastoma multiforme), supratentorial primitive neuroectodermal tumor (PNET), ganglioglioma, gangliocytoma, and oligodendroglioma.[1,6,15] Supratentorial ependymoma are iso- to slightly hypoattenuating to surrounding normal brain tissue at unenhanced CT.[6,8,9,16] They are iso- to hypointense relative to normal white matter on unenhanced T1-weighted MR images and hyperintense on T2- and proton-density-weighted MR images. Foci of signal heterogeneity within a solid neoplasm represent hemosiderin, necrosis, or calcification, that is very common in this tumor (40%-80% of cases).[1,5,8,16] Ependymomas can display a variable contrast enhancement pattern but generally enhance moderately intensely at both CT and MR imaging, with central areas of necrosis.[6,9,17] In pathologic examination, the tumor cells are characteristically organized in perivascular pseudorosettes and, less commonly, ependymal rosettes.[1,5] Although ependymomas are moderately cellular tumors with rare mitotic figures (World Health Organization (WHO) grade II lesions), our patient had a more aggressive tumor, classified as WHO grade III.[5] In adult patients, the majority of supratentorial ependymomas are classified as WHO grade III.[18] However, nearly 70% of all ependymomas diagnosed in the pediatric population are histologically benign and are classified as WHO grade II; less than 2% are considered WHO grade I or subependymoma, and the remainder are classified as WHO grade III or the anaplastic variant.[19] Age at the onset is also an important prognostic factor.[20,21,22] Children younger than 3 years have a significantly worse outcome than older children or adults.[1] The best treatment is surgical radical resection, because it appears that total tumor resection is the most important factor associated with recurrence.[5,9,22] Pure cortical ependymomas are approached easier than purely intraventricular ependymomas, having better outcome. Postoperative radiotherapy must be administered in every case of partially resected tumors or anaplastic tumors. Chemotherapy and prophylactic craniospinal irradiation are not indicated as adjuvant treatment.[1,15,20] Our patient was treated with radical surgery and postoperative radiation therapy, because of their anaplastic grade tumor. There was no evidence of residual tumor at postoperative imaging. Overall, cortical ependymomas appear to have a relatively favorable prognosis compared with other supratentorial ependymomas.[7]
CONCLUSION
In this article, we report a case of young patient with purely cortical ependymoma and its atypic clinical manifestation. To make a proper differential diagnosis on supratentorial cortical mass lesions in a young patient, ependymoma should be considered as a differential diagnosis because cortical ependymomas appear to have a relatively favorable prognosis compared with other supratentorial ependymomas.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Molina OM, Colina JL, Luzardo GD, Mendez OE, Cardozo D, Velasquez HS, et al. Extraventricular cerebral anaplastic ependymomas. Surg Neurol. 1999;51:630–5. doi: 10.1016/s0090-3019(98)00118-9. [DOI] [PubMed] [Google Scholar]
- 2.Yadav YR, Neha, Chandrakar SK. Pure cortical supratentorial extraventricular ependymoma. Neurol India. 2009;57:213–5. doi: 10.4103/0028-3886.51301. [DOI] [PubMed] [Google Scholar]
- 3.Lee SK, Lim DJ, Kim SD. Supratentorial cortical ependymoma in a 21-month-old boy. J Korean Neurosurg Soc. 2011;50:244–7. doi: 10.3340/jkns.2011.50.3.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miyazawa T, Hirose T, Nakanishi K, Uozumi Y, Tsuzuki N, Shima K. Supratentorial ectopic cortical ependymoma occurring with intratumoral hemorrhage. Brain Tumor Pathol. 2007;24:35–40. doi: 10.1007/s10014-007-0215-3. [DOI] [PubMed] [Google Scholar]
- 5.Ehtesham M, Kabos P, Yong WH, Schievink WI, Black KL, Yu JS. Development of an intracranial ependymoma at the site of a pre-existing cavernous malformation. Surg Neurol. 2003;60:80–3. doi: 10.1016/s0090-3019(03)00032-6. [DOI] [PubMed] [Google Scholar]
- 6.Roncaroli F, Consales A, Fioravanti A, Cenacchi G. Supratentorial cortical ependymoma: Report of three cases. Neurosurgery. 2005;57:E192. doi: 10.1227/01.neu.0000164171.29292.d6. [DOI] [PubMed] [Google Scholar]
- 7.Van Gompel JJ, Koeller KK, Meyer FB, Marsh WR, Burger PC, Roncaroli F, et al. Cortical ependymoma: An unusual epileptogenic lesion. J Neurosurg. 2011;114:1187–94. doi: 10.3171/2010.12.JNS10846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ono S, Ichikawa T, Ono Y, Date I. Large supratentorial ectopic ependymoma with massive calcification and cyst formation -Case report. Neurol Med Chir (Tokyo) 2004;44:424–8. doi: 10.2176/nmc.44.424. [DOI] [PubMed] [Google Scholar]
- 9.Davis MJ, Hasan F, Weinreb I, Wallace MC, Kiehl TR. Extraventricular anaplastic ependymoma with metastasis to scalp and neck. J Neurooncol. 2011;104:599–604. doi: 10.1007/s11060-010-0525-x. [DOI] [PubMed] [Google Scholar]
- 10.Lehman NL. Central nervous system tumors with ependymal features: A broadened spectrum of primarily ependymal differentiation? J Neuropathol Exp Neurol. 2008;67:177–88. doi: 10.1097/NEN.0b013e31816543a6. [DOI] [PubMed] [Google Scholar]
- 11.Lehman NL. Patterns of brain infiltration and secondary structure formation in supratentorial ependymal tumors. J Neuropathol Exp Neurol. 2008;67:900–10. doi: 10.1097/NEN.0b013e31818521cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lehman NL, Jorden MA, Huhn SL, Barnes PD, Nelson GB, Fisher PG, et al. Cortical ependymoma. A case report and review. Pediatr Neurosurg. 2003;39:50–4. doi: 10.1159/000070881. [DOI] [PubMed] [Google Scholar]
- 13.Lum DJ, Halliday W, Watson M, Smith A, Law A. Cortical ependymoma or monomorphous angiocentric glioma? Neuropathology. 2008;28:81–6. doi: 10.1111/j.1440-1789.2007.00831.x. [DOI] [PubMed] [Google Scholar]
- 14.Wang M, Tihan T, Rojiani AM, Bodhireddy SR, Prayson RA, Lacuone JJ, et al. Monomorphous angiocentric glioma: A distinctive epileptogenic neoplasm with features of infiltrating astrocytoma and ependymoma. J Neuropathol Exp Neurol. 2005;64:875–81. doi: 10.1097/01.jnen.0000182981.02355.10. [DOI] [PubMed] [Google Scholar]
- 15.Hamano E, Tsutsumi S, Nonaka Y, Abe Y, Yasumoto Y, Saeki H, et al. Huge supratentorial extraventricular anaplastic ependymoma presenting with massive calcification- Case report. Neurol Med Chir (Tokyo) 2010;50:150–3. doi: 10.2176/nmc.50.150. [DOI] [PubMed] [Google Scholar]
- 16.Alexiou GA, Panagopoulos D, Moschovi M, Stefanaki K, Sfakianos G, Prodromou N. Supratentorial extraventricular anaplastic ependymoma in a 10-year-old girl. Ped Neurosurg. 2011;46:480–1. doi: 10.1159/000325155. [DOI] [PubMed] [Google Scholar]
- 17.Afra D, Müller WM, Slowik F, Wilcke O, Budka H, Turoczy L. Supratentorial lobar ependymomas: Reports on the grading and survival periods in 80 cases, including 46 recurrences. Acta Neurochir (Wien) 1983;69:243–51. doi: 10.1007/BF01401811. [DOI] [PubMed] [Google Scholar]
- 18.Shuangshoti S, Rushing EJ, Mena H, Olsen C, Sandberg GD. Supratentorial extraventricular ependymal neoplasms: Aclinicopathologic study of 32 patients. Cancer. 2005;103:2598–605. doi: 10.1002/cncr.21111. [DOI] [PubMed] [Google Scholar]
- 19.Niazi TN, Jensen EM, Jensen RL. WHO Grade II and III supratentorial hemispheric ependymomas in adults: Case series and review of treatment options. J Neurooncol. 2009;91:323–8. doi: 10.1007/s11060-008-9717-z. [DOI] [PubMed] [Google Scholar]
- 20.Nakamizo S, Sasayama T, Kondoh T, Inoue S, Shiomi R, Tanaka H, et al. Supratentorial pure cortical ependymoma. J Clin Neurosci. 2012;19:1453–5. doi: 10.1016/j.jocn.2011.09.039. [DOI] [PubMed] [Google Scholar]
- 21.Ghani AR, Abdullah JM, Ghazali M, Ahmad F, Ahmad KA, Madhavan M. Recurrent paediatric supratentorial extraventricular ependymoma associated with genetic mutation at exon 4 of p53 gene. Singapore Med J. 2008;49:e192–4. [PubMed] [Google Scholar]
- 22.Ernestus RI, Schröder R, Stützer H, Klug N. Prognostic relevance of localization and grading in intracranial ependymomas of childhood. Child Nerv Syst. 1996;12:522–6. doi: 10.1007/BF00261604. [DOI] [PubMed] [Google Scholar]


