Abstract
Objective
There is a lack of research on effects of occupational noise exposure in traditionally female-dominated workplaces. Therefore, the aim of this study was to assess risk of noise-induced hearing-related symptoms among obstetrics personnel.
Design
A cross-sectional study was performed at an obstetric ward in Sweden including a questionnaire among all employees and sound level measurements in 61 work shifts at the same ward.
Participants
115 female employees responded to a questionnaire (72% of all 160 employees invited).
Main outcome measures
Self-reported hearing-related symptoms in relation to calculated occupational noise exposure dose and measured sound levels.
Results
Sound levels exceeded the 80 dB LAeq limit for protection of hearing in 46% of the measured work shifts. One or more hearing-related symptoms were reported by 55% of the personnel. In logistic regression models, a significant association was found between occupational noise exposure dose and tinnitus (OR=1.04, 95% CI 1.00 to 1.09) and sound-induced auditory fatigue (OR=1.04, 95% CI 1.00 to 1.07). Work-related stress and noise annoyance at work were reported by almost half of the personnel. Sound-induced auditory fatigue was associated with work-related stress and noise annoyance at work, although stress slightly missed significance in a multivariable model. No significant interactions were found.
Conclusions
This study presents new results showing that obstetrics personnel are at risk of noise-induced hearing-related symptoms. Current exposure levels at the workplace are high and occupational noise exposure dose has significant effects on tinnitus and sound-induced auditory fatigue among the personnel. These results indicate that preventative action regarding noise exposure is required in obstetrics care and that risk assessments may be needed in previously unstudied non-industrial communication-intense sound environments.
Keywords: OCCUPATIONAL & INDUSTRIAL MEDICINE, OBSTETRICS
Strengths and limitations of this study.
The vast majority of previous research into noise-induced hearing disorders has been performed in industrial-like settings, whereas practically nothing is known of risks in non-industrial, traditionally female-dominated and communication-intense workplaces, such as hospitals. As such, this study presents novel results on occupational noise exposure and hearing among obstetrics personnel.
Both objective sound level measurements and analysis of subjective data indicate an increased risk of noise-induced hearing-related symptoms.
Owing to the study's cross-sectional design the influence of participants’ age cannot be disentangled.
The study sample size and the cross-sectional design without an unexposed control group limits the generalisation of the results and prevents us from drawing definite conclusions on causality.
Further studies are needed to confirm the results and assess the magnitude of the problem. However, we suggest that occupational healthcare services implement available preventative actions such as making hearing protective devices available for personnel as an act of precaution.
Introduction
Occupational noise exposure and effects on hearing are well described in industrial-like, traditionally male-dominated settings.1 In contrast, few studies have reported on traditionally female-dominated work environments. This has been acknowledged by the European Agency for Safety and Health at Work, who conclude that areas such as health and social services are largely overlooked concerning noise research,2 and that the noise in these types of workplaces may interfere with performance and well-being. High sound levels, regardless of their source, can cause hearing loss, tinnitus and sound sensitivity, and may also result in sound-induced auditory fatigue, the latter described by participants as avoidance of everyday sounds and a need for silence.1 3–7 The symptom ‘sound-induced auditory fatigue’ was first identified in pilot studies, interviewing preschool personnel, and later shown to be prevalent in questionnaire surveys.7 We hypothesise the symptom to be a result of constant or overloading stimulation of sounds during the day. The effect may possibly be due to the high information content, mainly of speech, such that overload is not merely a consequence of the sound energy as seen in auditory threshold shift, but as a result of an information-intense sound environment. Apart from hearing-related symptoms, noise exposure can also evoke non-auditory effects such as annoyance and stress.8 According to a recent meta-analysis, noise levels in hospitals have steadily increased since the mid-1960s.9 One heavily female-dominated workplace in the hospital is in the area of obstetrics care. According to data from Statistics Sweden in 2011, more than 99% of midwives are women. One peer-reviewed study reported on sound level measurements in a hospital in India, where the highest nighttime level (71.9 dB LAeq) was measured in the obstetrics and gynaecology ward, with slightly lower levels in the labour ward.10
In addition to potentially harmful noise levels in the obstetrics care area, midwives report a high degree of work-related stress and burnout,11 and, according to a recent report, burnout syndrome has doubled among midwives employed in the western region of Sweden during the last few years.12 The fact that obstetrics personnel are exposed to high levels of stress may be important when considering noise exposure at the workplace, since the combination of these exposures may interact in causing adverse health effects.13–15
There is a substantial lack of knowledge regarding occupational noise exposure, noise annoyance at work and hearing-related symptoms among obstetrics care personnel, as well as possible interaction effects between noise exposure, noise annoyance at work and work-related stress. Therefore, the aim of this study was to assess the risk of noise-induced hearing-related symptoms among obstetrics personnel by measuring sound levels in the labour ward of a general obstetrics ward and by analysing the effect of and interaction between occupational noise exposure, noise annoyance at work and work-related stress on hearing-related symptoms among obstetrics personnel.
Methods
Sound level measurements
Sound level measurements were carried out during 61 work shifts in the labour ward of a general obstetrics ward at the Sahlgrenska University Hospital in Gothenburg. Of the 61 shifts, 19 day shifts were measured between 7:00 and 15:30 (8.5 h), 12 evening shifts between 13:45 and 21:00 (7.25 h), and 30 nightshifts between 21:00 and 7:00 (10 h). The day and evening shifts were measured during separate weeks so as not to overlap. A convenient sample of 10 employees per shift each wore a personal dosimeter (Larson Davis 705+), with the microphone attached to the right shoulder, and kept a written log documenting work activities during the measured shift. A total of 610 separate measurements were collected, as 10 individuals each wore a dosimeter during the 61 shifts measured. However, due to technical errors, a few faulty measurements were excluded, leaving 529 (87%) to be included in the analysis. The dosimeters were set to measure A-weighted equivalent and maximum (fast) levels with a sampling interval of 30 s. All dosimeters were calibrated using the software Blaze V.5.06 before measurements began. The equivalent levels reported refer to the full-shift length and will hence vary between 7.25 and 10 h, hereinafter denoted as LAeq(7–10 h). Sound levels were analysed at group level as arithmetic mean and compared to Swedish Work Authorities’ exposure regulations. Sound levels exceeding the lower action level of 80 dB LAeq(8 h) indicate a risk for hearing damage and the employer is responsible to take preventative action, such as providing employees with hearing protection devices (HPDs). The exposure limits 85 dB LAeq(8 h) and 115 dB LAFmax are set as a maximum allowed level, above which the employer is required to take measures in order to reduce the noise exposure, and where the use of HPDs are mandatory. Employees must not be exposed to noise levels at or above the exposure limits (taking attenuation of HPDs into account).
Questionnaire survey
All personnel (n=160, all women) employed at the general obstetrics ward were included in a questionnaire survey. A total of 115 (72%) participated by responding either electronically (n=63) or in paper format (n=52), and these data were pooled together, as no statistical differences were seen on explanatory or outcome variables (p>0.05). The questionnaire was constructed using items specifically constructed for this study as well as items adapted from previous studies and international standards (ISO/TS 15666).7 16 Similar self-reported items assessing noise exposure as well as hearing loss and tinnitus have previously been subject for validation.17–20
The main explanatory variable occupational noise exposure dose was calculated as an exposure index derived from six questionnaire items including number of years worked in delivery care, number of years worked in alternative birth care, work allocation (delivery care, postpartum care or both), with two separate items on frequency of current work-related noise exposure (one assessing how often the sound levels are so high that the person has to speak with a raised voice and one assessing how often the person has trouble hearing what is said) and finally one item on frequency of hearing protection use. A higher occupational noise index indicates a higher occupational noise exposure dose. The scoring for each item's contribution to the index is presented in detail in online supplementary table S1. Each variable score was summed using mathematical addition to a total index score for each participant. In addition, the study group was categorised into four noise index groups based on calculation of quartiles, with each noise index category representing 25% of the study population. Work-related stress and noise annoyance at work were analysed as additional explanatory variables. Work-related stress was assessed using two separate questionnaire items asking responders to report how often they experience high degree of stress and how often they feel unwell due to stress at work. Participants were defined as having work-related stress if answering often or always/almost always on one or both of the items. These stress-related items have previously been used in noise-related research.21 Noise annoyance at work was assessed by the item ‘Are you annoyed by sounds/noise at your workplace?’, which is based on the International standard ISO/TS 15666, adapted for a workplace survey as opposed to community noise surveys. The hearing-related outcome variables included are hearing loss (yes), tinnitus, sound sensitivity (ie, hyperacusis) and sound-induced auditory fatigue (once a week or more often), general hearing status (poor or very poor) and difficulty perceiving speech (‘yes’ both at work and in leisure time). Variables considered as possible moderators for the association between exposure and outcome were smoking (previous or current) and leisure-time noise exposure (once a month or more often). Age (in years) was considered as a possible confounder. The questionnaire items are presented in full in the online supplementary table S2.
Statistical analyses
Hypothesis testing was performed using IBM SPSS Statistics V.20. Differences in arithmetic mean were analysed using one-way analysis of variance (ANOVA) or independent samples t test where applicable. Test for trend was analysed using linear regression with dummy coding for categorical predictors or Mantel-Haentzel linear-by-linear association where applicable. Binary logistic regression with Wald tests was used for analysis of associations and interaction. The significance level was set at 5% (p=0.05) for all tests. Based on a hypothesised order of importance of explanatory variables, manual sequential regression models were analysed. For each binary hearing-related outcome variable we used the following model testing procedure: In a first model, occupational noise index was analysed as a single continuous explanatory variable with the hearing-related symptom as a binary outcome variable. If occupational noise index was significant for the hearing-related symptom, then a second model was analysed, adjusting for moderators (leisure noise exposure and smoking), each one at a time. Age as a possible confounder was analysed separately due to initial hypothesised strong correlation to the noise index (due to its cumulative nature). If point estimates for noise index was comparable with and without adjustment, and the adjustment variable itself was non-significant, then it was not included in subsequent multivariable models. In the third model, work-related stress was analysed as an additional explanatory variable and in a fourth model noise annoyance at work instead of stress was included together with significant explanatory variables from model 2. The fifth model included explanatory variables found to be significant in any of the previous steps. Hypothesised interactions between explanatory variables were assessed in separate models by including an interaction term. Multicollinearity between explanatory variables was assessed using Pearson's correlation or Spearman's rank correlation, where applicable, and correlation below r=0.6 was deemed acceptable. Odds ratios (ORs) with 95% CIs were derived from the logistic regressions as a measure of association between exposure and outcome, and relative risk (RR) was calculated from predictive values derived from model 1. Goodness of fit for the regression models was assessed using the Hosmer-Lemeshow test and a non-significant p value (>0.05) was used to indicate adequate fit.
Results
Sound levels in the labour ward
Overall, the dosimeter measurements from the labour ward showed moderately high sound levels, as presented in table 1. The levels reached or exceeded the action and the limit levels. The lower action level 80 dB LAeq was exceeded in 30 different dosimeter measurements during 28 different work shifts, which corresponds to 46% of all measured shifts or 6% of all dosimeter measurements. The upper exposure action level and exposure limit 85 dB LAeq was reached or exceeded in three measurements from three different shifts, corresponding to 5% of all measured shifts or 0.6% of all measurements. The limit 115 dB LAFmax was reached or exceeded on 50 different occasions. However, of these, nine separate events could not be verified by the written logs and were therefore excluded. The remaining 41 events occurred in 17 different shifts corresponding to 28% of all measured shifts or 8% of all dosimeter measurements. There were no statistical differences in arithmetic mean, neither equivalent nor maximum levels were statistically different in different work shifts, or in measurements from dosimeters worn by midwives compared to assistant nurses. Owing to incomplete written logs, however, we were unable to categorise a third of the measurements into professional group. A segment sample from a dosimeter measurement is shown in figure 1, where high maximum levels (119 dB LAFmax) were recorded during a delivery, which, according to the written log, occurred between 22:30 and 23:05. The equivalent level in this particular measurement was 84 dB LAeq(10 h) for the measured shift length. As exposure limits should be regarded with HPDs taken into account, it is noteworthy that the majority of the respondents (92%) reported to never or almost never using hearing protective devices at work.
Table 1.
Sound level measurements at the labour ward showing arithmetic mean, SD and range of the measured equivalent, LAeq(7–10 h) and maximum, LAFmax sound levels in dB
| Sound level measurements |
|||
|---|---|---|---|
| dB LAeq(7–10 h) | dB LAFmax | n | |
| All measurements | |||
| Arithmetic mean (SD) | 70.3 (6.0) | 106.3 (6.0) | 529 |
| Range | 56.0–87.0 | 83.0–122.0 | |
| Measurements categorised by work shift (arithmetic mean, SD)* | |||
| Day shift | 70.8 (6.2) | 106.2 (5.9) | 139 |
| Evening shift | 70.8 (5.2) | 106.3 (5.6) | 127 |
| Night shift | 69.8 (6.3) | 106.4 (6.2) | 263 |
| Measurements categorised by professional group (arithmetic mean, SD) | |||
| Midwives | 71.3 (5.1) | 106.2 (5.9) | 289 |
| Assistant nurses | 72.2 (5.0) | 107.8 (5.2) | 114 |
| Uncategorised | 66.2 (7.0) | 103.9 (6.5) | 126 |
Also showing mean and SD of measurements categorised by work shift and by professional group as reported in written logs by the personnel carrying the dosimeter. Frequencies (n) in the table represent unique dosimeter measurements.
*Number of shifts categorised as day n=19, evening n=12 and night n=30.
Figure 1.
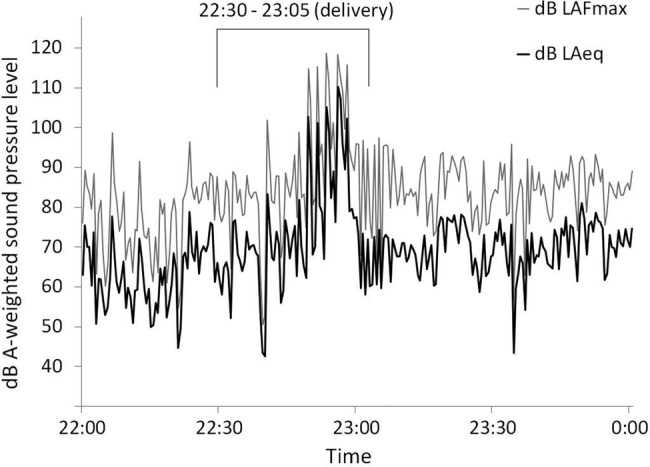
Two-hour section of a time history graph from sound level measurement with dosimeter carried by a midwife during a sample night shift in the obstetrics ward. Equivalent sound level during the entire shift was 84 dB LAeq (10 h) and 118.7 dB LAFmax was the highest recorded during the shift (shown in the selected section). According to the written log, the midwife attended a delivery during 22:30–23:05. Black curve showing the dB LAeq and grey curve showing dB LAFmax.
Association between noise exposure and hearing disorder
Table 2 shows occupational noise exposure dose (occupational noise index) and prevalence of hearing-related outcomes as well as demographics such as age, occurrence of explanatory/adjustment variables such as work-related stress and noise annoyance at work. Data is shown for the total study sample as well as categorised into four noise index groups calculated from quartiles of the occupational noise index. The first noise index group (1) represents the respondents with the lowest calculated noise exposure dose. Valid responses for the individual questionnaire items included in the analysis ranged from 108 to 115. A test for trend in the four noise index groups shows that age, number of years worked in obstetrics and prevalence of sound-induced auditory fatigue is significantly increasing with higher noise exposure group; p<0.001, <0.001 and 0.049, respectively.
Table 2.
Demographics, explanatory and adjustment variables and hearing-related outcomes from questionnaire survey among personnel at the general obstetrics ward
| Grouping by noise index quartiles |
Total | 95% CI of total | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| Number of participants | 28 | 29 | 29 | 29 | 115 | – |
| Demographics | ||||||
| Mean age in years (SD) | 39 (10) | 39 (7) | 45 (8) | 57 (5) | 45 (11) | 42.8 to 46.8 |
| Mean years worked (SD) | 3 (2) | 6 (2) | 14 (3) | 28 (6) | 12 (11) | 10.3 to 14.3 |
| Professional groups in %* | 54/36/11 | 69/24/7 | 69/21/10 | 76/21/3 | 68/25/7 | – |
| Explanatory/adjustment variables | ||||||
| Occupational noise index, range | 4.5–9.5 | 10–15 | 16–26 | 27–64 | 4.5–64 | 16.8 to 21.2 |
| Work-related stress, % | 43 | 52 | 31 | 41 | 42 | 32.9 to 51.1 |
| Noise annoyance at work, % | 50 | 45 | 55 | 45 | 49 | 39.8 to 58.2 |
| Ever smoker, % | 36 | 48 | 28 | 25 | 34 | 25.3 to 42.7 |
| Leisure noise exposure, % | 14 | 24 | 7 | 7 | 13 | 6.8 to 19.2 |
| Outcome variables (%) | ||||||
| Sound-induced auditory fatigue | 21 | 24 | 41 | 41 | 32 | 23.4 to 40.6 |
| Tinnitus | 7 | 11 | 10 | 24 | 13 | 6.8 to 19.2 |
| Sound sensitivity | 7 | 17 | 17 | 10 | 13 | 6.8 to 19.2 |
| Poor hearing | 11 | 21 | 17 | 14 | 16 | 9.3 to 22.7 |
| Hearing loss | 4 | 7 | 21 | 4 | 9 | 3.7 to 14.3 |
| Difficulty perceiving speech | 39 | 31 | 24 | 36 | 32 | 23.4 to 40.6 |
| Any symptom† | 54 | 48 | 55 | 63 | 55 | 45.9 to 64.1 |
Prevalence is presented categorised in four noise index groups based on quartiles of the index (1–4) and as total prevalence in the study sample. Percentages are given as column per cent in noise index quartile groups and per cent of total.
*Proportion of Midwife/Assistant nurse/Other. Other also includes missing.
†Any symptom was constructed as a binary variable including all those who reported either sound-induced auditory fatigue, tinnitus, sound sensitivity, poor hearing, hearing loss or difficulty perceiving speech.
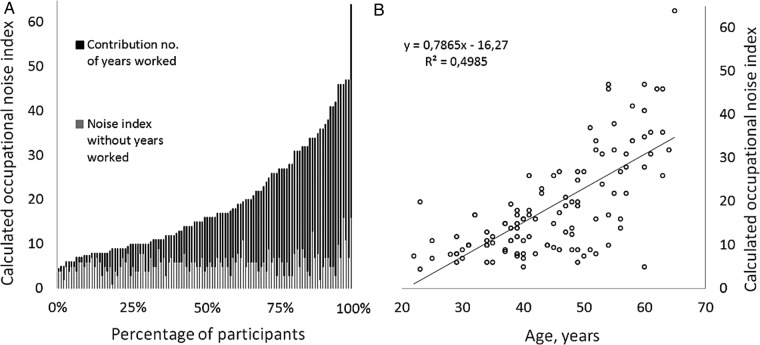
Associations between occupational noise exposure dose (continuous noise index), work-related stress, noise annoyance at work and hearing-related symptoms were evaluated in manual sequential binary logistic regression models, results of which are presented in table 3. The calculated noise index ranged from 4.5 to 64 in the study sample. The proportional contribution of years worked in obstetrics care to the index, as a proxy for cumulative exposure, is shown in figure 2A. The percentage of participants over the range of the occupational noise index also conveys the skewedness in the distribution of the index, for example, less than 25% of the participants have noise index values in the upper half of the range.
Table 3.
Point estimates of effect (B) and SE, ORs, 95% CIs of OR from binary logistic regression models for hearing-related symptom outcomes (binary dependent variables) among personnel in an obstetrics ward
| Dependent variables | Explanatory variables | B (SE) | OR (95% CI) | p Value |
|---|---|---|---|---|
| Sound-induced auditory fatigue | ||||
| Model 1 | Occupational noise index | 0.04 (0.02) | 1.04 (1.00 to 1.07) | 0.031 |
| Model 3 | Occupational noise index | 0.04 (0.02) | 1.04 (1.00 to 1.08) | 0.027 |
| Work-related stress | 0.96 (0.42) | 2.62 (1.15 to 5.98) | 0.022 | |
| Model 4 | Occupational noise index | 0.04 (0.02) | 1.04 (1.01 to 1.08) | 0.026 |
| Noise annoyance at work | 1.73 (0.47) | 5.67 (2.25 to 14.27) | <0.001 | |
| Model 5 | Occupational noise index | 0.04 (0.02) | 1.04 (1.01 to 1.08) | 0.025 |
| Work-related stress | 0.87 (0.45) | 2.39 (0.99 to 5.79) | 0.053 | |
| Noise annoyance at work | 1.66 (0.48) | 5.25 (2.05 to 13.42) | 0.001 | |
| Tinnitus | ||||
| Model 1 | Occupational noise index | 0.04 (0.02) | 1.04 (1.00 to 1.09) | 0.049 |
| Model 3 | Occupational noise index | 0.04 (0.02) | 1.04 (1.00 to 1.09) | 0.046 |
| Work-related stress | −0.43 (0.60) | 0.65 (0.20 to 2.10) | 0.470 | |
| Model 4 | Occupational noise index | 0.04 (0.02) | 1.05 (1.00 to 1.09) | 0.038 |
| Noise annoyance at work | 0.56 (0.58) | 1.85 (0.56 to 5.46) | 0.335 | |
| Sound sensitivity | Occupational noise index | 0.01 (0.02) | 1.03 (0.97 to 1.06) | 0.570 |
| Poor hearing | Occupational noise index | 0.00 (0.02) | 1.00 (0.96 to 1.04) | 0.985 |
| Hearing loss | Occupational noise index | 0.00 (0.03) | 1.00 (0.95 to 1.06) | 0.995 |
| Difficulty perceiving speech | Occupational noise index | 0.01 (0.02) | 1.01 (0.98 to 1.05) | 0.461 |
| Any symptom* | Occupational noise index | 0.02 (0.02) | 1.02 (0.99 to 1.05) | 0.273 |
All dependent variables were analysed in separate models. Manual sequential analysis was adopted, adding work-related stress and noise annoyance at work, and adding an interaction term if the initial model was statistically significant (p<0.05).
*Any symptom was constructed as a binary variable including all those who reported either sound-induced auditory fatigue, tinnitus, sound sensitivity, poor hearing, hearing loss or difficulty perceiving speech. Bold typeface indicates statistical significance at p<0.05.
Figure 2.
Calculated occupational noise index for obstetrics personnel. (A) The contribution of the variable number of years worked in obstetrics (in black) to the noise index for each participant, each bar representing one participant. The light grey bars represent the index with the variable years worked in obstetrics omitted. The percentages of participants are shown on the x axis and the calculated noise index value on the y axis. (B) The correlation between occupational noise index and age of participants.
Occupational noise index as a single explanatory variable was significantly associated with tinnitus and sound-induced auditory fatigue, but not to the other hearing-related symptoms. Work-related stress and noise annoyance at work were both significantly associated with sound-induced auditory fatigue in separate models, but not with tinnitus. Sound-induced auditory fatigue, including all three significant explanatory variables (noise index, stress and annoyance) in model 5 resulted in marginal changes in point estimates for noise index and noise annoyance at work. It did, however, affect the estimates for work-related stress, which slightly missed statistical significance (p=0.053). No significant statistical interactions were found between explanatory variables. Neither work-related stress nor noise annoyance at work were significantly correlated to noise index. There was, however, a weak yet significant correlation between stress and noise annoyance (r=0.249, p=0.008). The point estimates for noise index were comparable with or without adjustment for smoking and leisure-time noise exposure in model 2, and neither one of the adjustment variables were themselves significant. Hence, they were not included in the subsequent multivariable models. All reported models had an acceptable goodness of fit.
As prevalence of sound-induced auditory fatigue was much higher than 10%, assessing ORs only may overestimate the risk. The calculated RR for sound-induced auditory fatigue from model 1, in comparable 1 unit steps of the noise index, however, showed that the difference between OR and RR was minor (at the most 0.02 difference).
Owing to the cumulative property of the noise index, the index was assumed to be correlated to age, which was also confirmed in the analysis (r=0.706, p<0.001) with R2=0.498, as shown in figure 2B. Multicollinearity issues, therefore, precluded the assessment of both variables in one regression model. Notably and importantly though, age was not significantly associated with any of the hearing-related symptoms when assessed as a single explanatory variable in separate regression models.
Discussion
The effect of noise exposure on hearing
In order to assess the effect of occupational noise exposure on hearing-related symptoms among obstetrics personnel, sound level measurements were carried out at the labour ward at a general obstetrics ward and associations between calculated occupational noise exposure dose and hearing-related symptoms were analysed in binary logistic regression models based on self-reported data from personnel at the same ward.
Prevalence of hearing-related symptoms among the personnel showed that tinnitus and sound-induced auditory fatigue were most common among personnel with the highest occupational noise exposure dose. Accordingly, we were also able to detect statistically significant associations between occupational noise index and both tinnitus and sound-induced auditory fatigue in logistic regression models. Sound-induced auditory fatigue is a new concept that has previously been reported among preschool personnel and is hypothesised as a consequence of a constant noise load during the work day.7 16 As with pre-school personnel, obstetric personnel are mainly exposed to intermittent sounds from voices and screams, but additionally, they are also exposed to sound from alarms and medical equipment. It is possible that the demands and needs of attending to meaningful sounds with a high element of irregularity contribute to a mental fatigue that some individuals with sound-induced auditory fatigue describe. As for sound-induced auditory fatigue, we could also show a significant association between tinnitus and noise exposure. Although it is well established that noise may contribute to tinnitus,4 22 23 it has, to the best of our knowledge, not been reported previously among obstetrics personnel; hence this result is highly interesting, as it supports the concerns that noise levels in non-industrial and previously less studied work environments, mainly female dominated, may be harmful.2 As the prevalence especially for sound-induced auditory fatigue was high, it is important to note that ORs may not directly be translated into a measure of relative risk.24 We did, however, not detect major divergences between the two measures.
In addition to increased risk of hearing-related symptoms of cumulative occupational noise exposure, we also found high current sound level exposure, above regulated limits, in the labour ward. The sound level measurements further heighten the concern that obstetrics personnel may risk acquiring hearing-related disorders as personnel carrying the dosimeters were exposed to levels exceeding the lower action level of 80 dB LAeq during as much as 46% of the measured work shifts. While the average noise levels were in accordance with an earlier study reporting noise levels from an obstetrics and labour ward at a general hospital,10 our study further showed that the exposure limit 115 dB LAFmax may be exceeded in as many as one-third of the work shifts in a labour ward. The data are also in accordance with results from a workplace inspection performed in 2010 by the occupational healthcare unit at a small obstetrics ward in Sweden, which showed that personnel were at times exposed to sound levels above the regulated action and limit levels adopted by the Swedish work environment authority.25 This result is especially alarming as very few personnel report use of hearing protection, which certainly may be impractical in this type of work setting. Although caution is required in establishing the source of high maximum levels recorded in unsupervised measurements, the results are indeed important, since such high sound levels have been described as a mechanism responsible for acquired hearing loss, tinnitus and sound sensitivity.3 These results highlight the need to initiate preventive action regarding noise exposure in the obstetrics care area, which includes but is not limited to information to all employees, access to suitable hearing protection devices, and cooperation between the employer and an occupational healthcare unit for assessment of noise exposure and hearing-related symptoms. Hearing tests and anamnesis regarding hearing-related symptoms may also be considered for new employees.
No significant associations between occupational noise index and the other hearing-related symptoms were detected in this study. This may be explained partly by the fact that hearing loss is developed over a long period of time, usually becoming apparent after the age of retirement, and that mild deterioration in hearing may not be easily detected via self-assessment. As the study was cross-sectional, the fact that hearing loss was most prevalent in the third noise index group and had lower prevalence in the fourth noise index group may have influenced the analysis. This in turn is possibly due to a healthy worker effect as individuals with hearing loss may not be able to continue working in obstetrics care. Similarly, but in the opposite direction, as difficulty perceiving speech was reported by many young individuals, which to a larger extent were classified in the lowest noise index quartile owing to fewer years of work in obstetrics care, it may have influenced the analysis of the effect of occupational noise exposure dose such that no significant effect was seen. Such a high prevalence of difficulty perceiving speech is in any case alarming. Compared to prevalence data from the Swedish National Board of Health and Welfare from 2000 to 2005, using a similar survey item as in this study,26 our data indicate higher age and gender-matched prevalence. Between the ages 25 and 64 years the prevalence in our sample ranged from 26% to 35%, while the prevalence in the same age range among women in the reference material was 5% to 15%. Sound sensitivity is less researched, but one previous study from Sweden reports prevalence in the general population of 8% to 9%.27 No gender-specific prevalence was reported, making direct comparisons to our data somewhat problematic; yet our data indicate slightly higher prevalence. In addition to the significant association between occupational noise exposure dose, and tinnitus and sound-induced auditory fatigue, our data also show that having one or more hearing-related symptoms is most common among those with highest occupational noise exposure dose as seen in table 2. However, having any hearing-related symptom was not significantly associated to noise exposure in the regression model, probably due to the variable difficulty perceiving speech as having a large influence with the high prevalence in the lower noise index group. Again, it is staggering to find that more than half of the participating personnel group reported one or more hearing-related symptoms.
The risks of acquiring hearing-related symptoms in this work environment should also be considered in the light of recent animal studies, which show that noise contributes to neurodegenerative effects and acute loss of afferent nerve terminals—the effects of which are believed to be of importance to auditory processing and subsequently may result in hearing injuries emerging only later in life.28–30 If applicable to humans, an implication would hence be that hearing functions of importance for auditory processing in adverse listening conditions may be impaired even though subjects have apparent normal hearing31 and, importantly, that risk of auditory injury from noise exposure is greater than previously assumed. Studies such as ours, investigating risks for hearing injury within occupational groups exposed to levels at or just below the stipulated risk levels, are therefore of high relevance.
Work-related stress and noise annoyance at work
Work-related stress was common among the obstetrics personnel surveyed, which is in line with previous research.11 12 A new finding, though, was that noise annoyance at work is also highly prevalent in this occupational group and that stress and noise annoyance were both positively associated with sound-induced auditory fatigue; however, the estimated effect for stress was reduced when stress and noise annoyance were both included in the same model. This may be due to lack of power in the analysis and possibly also multicollinearity, as there was a weak yet significant correlation between stress and annoyance. The associations were hypothesised based on models of pathways previously suggested by Babish,13 and in a recent model by Heinonen-Guzejev et al.32 In contrast to previous results of an association between stress and tinnitus,33 34 our results do not support this association among noise exposed personnel despite the fact that work-related stress was very common in our sample. It is possible that our measure of work-related stress did not capture the association, that the relationship is far more complex or that tinnitus is instead more strongly associated with psychological distress, as is also suggested by studies on tinnitus, and depression and anxiety,35 36 rather than physiological or psychosocial stress.
Methodological consideration
We are aware of methodological issues in retrospectively assessing exposure dose.37 38 In this study, an estimate of occupational noise exposure dose (noise index) was calculated by using years worked as a proxy for the accumulated exposure. In order to increase the sensitivity of this estimate, we also included years worked with the alternative birth care method (ABC-method, predominantly used during the 1980s and hypothesised to have given rise to higher sound levels in the labour ward due to the non-use of anaesthetics), and an assessment of current noise exposure as well as considered the protective effect of personal hearing protective devices. A common problem in studies where cumulative exposure is estimated is that age will naturally be incorporated in the exposure assessment, possibly confounding the results. In our data, there was a strong correlation between calculated occupational noise index and age, which is illustrated in figure 2B. It is, therefore, difficult to distinguish between effects of age and noise exposure dose, which would be the case independent of how the index was constructed as an accumulated exposure dose would naturally always correlate to increased age. As such, the possible confounding effect of age could not be properly adjusted for in the statistical model for the association between occupational noise index and hearing-related outcomes. When both were included in the logistic regression model, neither noise index nor age showed a statistically significant effect on any of the hearing-related outcomes. Interestingly though, we could show that the noise exposure index was significantly associated to the hearing-related outcomes tinnitus and sound-induced auditory fatigue, while this was not the case for age alone as a predictor in a separate bivariable model. Pathological changes in the inner ear resulting in hearing loss as an effect of increasing age alone is debated in the research community.39 Results are even less solid when considering increasing age as a sole cause of tinnitus.40 Instead, the effect of noise exposure is hypothesised to largely contribute to the increased prevalence of hearing-related disorder seen in increased age.30 39 40
Finally, being an initial study in this area, we were not able to include a large study sample, which affects the reliability of the analyses and the generalisation of the results. Also, though the cross-sectional design prevents drawing definite conclusions on causal relationships, we argue, based on previous research and our study results, that it is reasonable to assume a causal pathway from noise exposure to hearing-related symptoms; the hypothesised casual pathway involving work-related stress and noise annoyance at work, however, being less certain.
Conclusion
This study presents new results regarding risk of noise-induced hearing-related symptoms among obstetrics personnel, which, to the best of our knowledge, has not been described before. The results show that obstetrics personnel are at times exposed to sound levels above regulated limits and that more than half of the participants report one or more hearing-related symptoms. Furthermore, a statistically significant association was found between occupational noise exposure dose and the hearing-related symptoms tinnitus and sound-induced auditory fatigue. Noise annoyance at work was a common complaint and, in addition to occupational noise exposure, also an important factor for sound-induced auditory fatigue. These results indicate that preventative action regarding noise exposure is required in obstetrics care and that risk-assessments may be needed in previously unstudied non-industrial communication-intense sound environments.
Acknowledgments
The authors would like to thank Lars Larsson for performing the dosimeter measurements, Christofer Andersson for assistance with the web-survey and Agneta Agge for survey data entry, as well as all the participating personnel at the obstetrics care unit at the Sahlgrenska University Hospital.
Footnotes
Contributors: KPW and KT obtained funding. KPW, SF and AT contributed to the study concept and design. SF collected the data with the help of KPW. OH, SF, KPW and KT designed the plan of analysis. SF performed the final analyses. SF, KPW, OH and KT drafted the manuscript and interpreted the results. All authors made substantive editorial contributions at all stages of manuscript preparation.
Funding: This study was funded by grants from the Swedish research council for Health, Working Life and Welfare (Forte, grant no. 2009-1741) as well as the Swedish funder AFA insurance (grant no. 090161). The researchers are independent from funders.
Competing interests: None.
Ethics approval: The study was approved by the ethics committee in Gothenburg Sweden, No. 788-11.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statements: No additional data are available.
References
- 1.Nelson DI, Nelson RY, Concha-Barrientos M et al. . The global burden of occupational noise-induced hearing loss. Am J Ind Med 2005;48:446–58. 10.1002/ajim.20223 [DOI] [PubMed] [Google Scholar]
- 2. European Agency for Safety and Health at Work. New risks and trends in the safety and health of women at work, 2013. https://osha.europa.eu/en/publications/reports/new-risks-and-trends-in-the-safety-and-health-of-women-at-work.
- 3.Axelsson A, Hamernik RP. Acute acoustic trauma. Acta Otolaryngol 1987;104:225–33. 10.3109/00016488709107322 [DOI] [PubMed] [Google Scholar]
- 4.Henry JA, Dennis KC, Schechter MA. General review of tinnitus: prevalence, mechanisms, effects, and management. J Speech Lang Hear Res 2005;48:1204–35. 10.1044/1092-4388(2005/084) [DOI] [PubMed] [Google Scholar]
- 5.Kähäri K, Zachau G, Eklöf M et al. . Assessment of hearing and hearing disorders in rock/jazz musicians: Evaluación de la audición y de los problemas auditivos en músicos de rock y jazz. Int J Audiol 2003;42:279–88. 10.3109/14992020309078347 [DOI] [PubMed] [Google Scholar]
- 6.Palmer K, Griffin M, Syddall H et al. . Occupational exposure to noise and the attributable burden of hearing difficulties in Great Britain. Occup Environ Med 2002;59:634–9. 10.1136/oem.59.9.634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Persson Waye K, Ryherd E, Hsu T et al. . Personnel response in intensive care units. Internoise; 13–16 June 2010; Lisbon, Portugal. [Google Scholar]
- 8.Kjellberg A. Subjective, behavioral and psychophysiological effects of noise. Scand J Work Environ Health 1990:29–38. 10.5271/sjweh.1825 [DOI] [PubMed] [Google Scholar]
- 9.Busch-Vishniac IJ, West JE, Barnhill C et al. . Noise levels in Johns Hopkins Hospital. J Acoust Soc Am 2005;118:3629 10.1121/1.2118327 [DOI] [PubMed] [Google Scholar]
- 10.Vinodhkumaradithyaa A, Kumar D, Ananthalakshmi I et al. . Noise levels in a tertiary care hospital. Noise Health 2008;10:11–3. 10.4103/1463-1741.39003 [DOI] [PubMed] [Google Scholar]
- 11.Hildingsson I, Westlund K, Wiklkund I. Burnout in Swedish midwives. Sex Reprod Healthc 2013;4:87–91. 10.1016/j.srhc.2013.07.001 [DOI] [PubMed] [Google Scholar]
- 12.Hultberg A, Hadžibajramović E, Pettersson S et al. . KART-studien. Arbetsmiljö, stress och hälsa bland anställda vid Västra Götalandsregionen. Delrapport 5: Uppföljning utifrån organisations-, yrkesgrupps- och individperspektiv 2008–2010 [In Swedish] Ahlborg G, ed. Västra Götaland, Sweden:Institute of Stress Medicine, 2011:1–95. http://www.vgregion.se/upload/Regionkanslierna/ISM%20Institutet%20f%c3%b6r%20stressmedicin/Publikationer/ISM-rapporter/ISM-rapport%2010.pdf [Google Scholar]
- 13.Babisch W. The noise/stress concept, risk assessment and research needs. Noise Health 2002;4:1–11. [PubMed] [Google Scholar]
- 14.Leather P, Beale D, Sullivan L. Noise, psychosocial stress and their interaction in the workplace. J Environ Psychol 2003;23:213–22. 10.1016/S0272-4944(02)00082-8 [DOI] [Google Scholar]
- 15.Lercher P, Hörtnagl J, Kofler WW. Work noise annoyance and blood pressure: combined effects with stressful working conditions. Int Arch Occup Environ Health 1993;65:23–8. 10.1007/BF00586054 [DOI] [PubMed] [Google Scholar]
- 16.Persson Waye K, Agge A, Hillström J et al. . Being in a pre-school sound environment—annoyance and subjective symptoms among personnel and children . Internoise; 13–16 June 2010; Lisbon, Portugal. [Google Scholar]
- 17.Neitzel R, Daniell W, Sheppard L et al. . Comparison of perceived and quantitative measures of occupational noise exposure. Ann Occup Hyg 2009;53:41–54. 10.1093/annhyg/men071 [DOI] [PubMed] [Google Scholar]
- 18.Nondahl DM, Cruickshanks KJ, Wiley TL et al. . Accuracy of self-reported hearing loss. Int J Audiol 1998;37:295–301. 10.3109/00206099809072983 [DOI] [PubMed] [Google Scholar]
- 19.Schlaefer K, Schlehofer B, Schüz J. Validity of self-reported occupational noise exposure. Eur J Epidemiol 2009;24:469–75. 10.1007/s10654-009-9357-4 [DOI] [PubMed] [Google Scholar]
- 20.Sindhusake D, Mitchell P, Smith W et al. . Validation of self-reported hearing loss. The Blue Mountains hearing study. Int J Epidemiol 2001;30:1371–8. [DOI] [PubMed] [Google Scholar]
- 21.Ryberg JB, Agge A, Persson Waye K. Low frequency noise in a paper mill control room. J Low Freq Noise Vibration Active Control 2007;26:165–76. 10.1260/026309207783700420 [DOI] [Google Scholar]
- 22.Axelsson A, Prasher D. Tinnitus induced by occupational and leisure noise. Noise Health 2000;2:47–54. [PubMed] [Google Scholar]
- 23.Nouvian R, Eybalin M, Puel J-L. The Cochlea and the Auditory Nerve as a Primary Source of Tinnitus. In: Eggermont JJ, Zeng F-G, Popper AN, eds. Tinnitus. New York: Springer Science and Business Media, 2012:83–85. [Google Scholar]
- 24.Schmidt CO, Kohlmann T. When to use the odds ratio or the relative risk? Int J Public Health 2008;53:165–7. 10.1007/s00038-008-7068-3 [DOI] [PubMed] [Google Scholar]
- 25.Tenenbaum A, Hendriksson A, Larsson L. Bullernivåer och hörselundersökning på förlossningsavdelning. Läkarstämman. Stockholm, Sweden, 2010. [In Swedish]. [Google Scholar]
- 26.Danermark B, Hanning M. Hearing and vision: health in Sweden: the National Public Health Report 2012. Chapter 17. Scand J Public Health 2012;40(9 Suppl):287–92. 10.1177/1403494812459621 [DOI] [PubMed] [Google Scholar]
- 27.Andersson G, Lindvall N, Hursti T et al. . Hypersensitivity to sound (hyperacusis): a prevalence study conducted via the internet and post. Int J Audiol 2002;41:545–54. 10.3109/14992020209056075 [DOI] [PubMed] [Google Scholar]
- 28.Kujawa SG, Liberman MC. Adding insult to injury: cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci 2009;29:14077–85. 10.1523/JNEUROSCI.2845-09.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin HW, Furman AC, Kujawa SG et al. . Primary neural degeneration in the Guinea pig cochlea after reversible noise-induced threshold shift. J Assoc Res Otolaryngol 2011;12:605–16. 10.1007/s10162-011-0277-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kujawa SG, Liberman MC. Acceleration of age-related hearing loss by early noise exposure: evidence of a misspent youth. J Neurosci 2006;26:2115–23. 10.1523/JNEUROSCI.4985-05.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ruggles D, Bharadwaj H, Shinn-Cunningham BG. Normal hearing is not enough to guarantee robust encoding of suprathreshold features important in everyday communication. Proc Natl Acad Sci USA 2011;108:15516–21. 10.1073/pnas.1108912108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heinonen-Guzejev M, Koskenvuo M, Silventoinen K et al. . Noise sensitivity and disability retirement: a longitudinal twin study. J Occup Environ Med 2013;55:365–70. 10.1097/JOM.0b013e318285f433 [DOI] [PubMed] [Google Scholar]
- 33.Alpini D, Cesarani A. Tinnitus as an alarm bell: stress reaction tinnitus model. ORL 2006;68:31–7. 10.1159/000090488 [DOI] [PubMed] [Google Scholar]
- 34.Hébert S, Lupien SJ. The sound of stress: blunted cortisol reactivity to psychosocial stress in tinnitus sufferers. Neurosci Lett 2007;411:138–42. 10.1016/j.neulet.2006.10.028 [DOI] [PubMed] [Google Scholar]
- 35.Holgers K-M, Erlandsson SI, Barrenäs M-L. Predictive factors for the severity of tinnitus: factores predictivos de la severidad del tinnitus. Int J Audiol 2000;39:284–91. 10.3109/00206090009073093 [DOI] [PubMed] [Google Scholar]
- 36.Robinson SK, Viirre ES, Stein MB. Antidepressant therapy in tinnitus. Hear Res 2007;226:221–31. 10.1016/j.heares.2006.08.004 [DOI] [PubMed] [Google Scholar]
- 37.Davies HW, Teschke K, Kennedy SM et al. . Occupational exposure to noise and mortality from acute myocardial infarction. Epidemiology 2005;16:25–32. 10.1097/01.ede.0000147121.13399.bf [DOI] [PubMed] [Google Scholar]
- 38.Nilsson T, Burström L, Hagberg M. Risk assessment of vibration exposure and white fingers among platers. Int Arch Occup Environ Health 1989;61:473–81. 10.1007/BF00386482 [DOI] [PubMed] [Google Scholar]
- 39.Van Eyken E, Van Camp G, Van Laer L. The complexity of age-related hearing impairment: contributing environmental and genetic factors. Audiol Neurotol 2007;12:345–58. 10.1159/000106478 [DOI] [PubMed] [Google Scholar]
- 40.Sanchez L. The epidemiology of tinnitus. Audiol Med 2004;2:8–17. 10.1080/16513860410027781 [DOI] [Google Scholar]