Abstract
Objectives. We examined the longitudinal effect of obesity, major depression, and their combination on work performance impairment (WPI).
Methods. We collected longitudinal data (2004–2013) on 1726 paid employees from the Netherlands Study of Depression and Anxiety at baseline and 2-, 4-, and 6-year follow-up. We defined obesity with body mass index and waist circumference. We diagnosed major depression with the Composite International Diagnostic Interview 2.1. We assessed work performance impairment with a questionnaire for illness-associated costs. We used generalized estimating equations for modeling, and estimated interaction on the additive scale.
Results. Obesity, abdominal obesity, and major depression were longitudinally associated with increased risk of high WPI. The combinations of obesity and major depression, and of abdominal obesity and major depression were associated with increased risk of high WPI (odds ratios of 2.36 [95% confidence interval = 1.61, 3.44] and 1.88 [95% confidence interval = 1.40, 2.53], respectively), but the relative excess risks attributable to interaction were nonsignificant.
Conclusions. The longitudinal joint effect of obesity and major depression on high WPI implies that obesity intervention may be more beneficial for individuals with major depression than those without regarding risk of high WPI, if confirmed in a large, representative sample.
Obesity and major depression are major public health problems, posing enormous challenges in the decades to come.1,2 Both obesity and major depression increase the risk of adverse health outcomes, such as type 2 diabetes, cardiovascular diseases, premature death, and disability.1,2 By 2030, major depression is even expected to be one of the top leading causes of disability-adjusted life years in high-income countries.1 In the European Union area, the costs of depression were estimated at 92 billion euro in 2010, with lost productivity because of absenteeism (being off work because of sickness) and presenteeism (being present at work while ill) representing more than 50% of all costs related to depression.3 It has been shown that a broad range of occupational health problems including depression is strongly associated with obesity, making obesity a prevailing problem in the working population.4–6 Previous studies that examined obesity in working populations are mainly focused on absenteeism7,8; less is known about productivity loss at work attributable to obesity.
Both obesity and major depression can impair work performance. Work performance impairment (WPI) refers to productivity loss at work because of health problems. Work performance impairment is an increasing problem in aging workforces and has enormous cost implications for individuals, companies, and society as a whole.9,10 Earlier, cross-sectional studies showed that major depression is associated with high WPI.11,12 Higher body weight and an excess of visceral fat are also associated with productivity loss.5–7 However, it is not known whether obesity and major depression jointly affect high WPI and if the risk of major depression on high WPI further increases in obese individuals.
There are 3 main reasons to examine their interaction or joint effect on WPI. First, obesity and depression are bidirectionally related, and neither obesity nor major depression fully precedes the other regarding the effect of WPI (i.e., no sole mediation). Then, it would be interesting to examine the joint effect of these 2 risk factors on high WPI and to estimate to what extent their joint effect differs from the sum of their separate effects on high WPI. Second, obesity and major depression share around 12% to 20% pleiotropic genes, and it seems that they might have a common etiology that make them valuable to examine.13–17 Third, both obesity and depression are associated with a global burden of disease and disability.1,2 In terms of their effects on the risk of high WPI, obesity and major depression may interact thereby augmenting or reducing the effect of one another. If obesity and major depression exacerbate a common pathway, we expect to observe a substantially elevated risk of WPI in people with both exposures.
The interaction between 2 exposures of interest on a certain outcome can best be measured by statistical interaction on the additive scale by using measures such as the relative excess risk due to interaction (RERI) and attributable proportion (AP).18,19 A statistical interaction on the additive scale is more relevant to disease prevention and workplace health promotion programs in vulnerable workers than an interaction on the multiplicative scale, which is relevant in disease etiology.18 For example, if the joint effect of obesity and major depression surpasses the sum of their separate effects, then a reduction of either obesity or major depression would also reduce the risk of the other factor regarding high WPI. In terms of clinical decision-making, then someone with major depression can reduce his or her risk regarding high WPI even more by losing weight than someone without major depression.
The main objective of the present study was to examine the longitudinal separate and joint effects of obesity and major depression on WPI. We used the RERI and AP as measures to test the hypothesis that the joint effect of obesity and major depression on high WPI is larger than the sum of the separate effects of obesity and major depression on high WPI. To our knowledge, there is no study to date that has investigated this hypothesis.
METHODS
We derived data (2004–2013) from an ongoing longitudinal cohort study, the Netherlands Study of Depression and Anxiety (NESDA). This study examines the etiology, course, and consequences of depressive and anxiety disorders.20 A total of 2981 persons were included, aged 18 through 65 years, with a current depressive or anxiety disorder, with subthreshold symptoms, and controls without lifetime diagnoses of depressive or anxiety disorder. Recruitment took place in the community, primary care, and secondary care. Exclusion criteria were (1) a primary clinical diagnosis of a psychiatric disorder (i.e., psychotic disorder, obsessive–compulsive disorder, bipolar disorder, or severe addiction disorder), and (2) not being fluent in Dutch.
Out of the NESDA population (n = 2981), we selected 1726 respondents who had a paid job for 8 or more hours per week at baseline. We took this cutoff because the employee should have been at work at least 1 day a week to be able to report the WPI information and to be consistent with previous NESDA studies.11,12 This constituted the final study sample. After the baseline measurement, we conducted extensive face-to-face and questionnaire-based assessments at 2-year, 4-year, and 6-year follow-up. The loss to follow-up regarding WPI measurements (availability of fewer than 2 measurements) was 27% and was associated with higher age, lower educational status, and depressive disorder, but not with gender, weight status, and anxiety disorder.
Measurements
General and abdominal obesity.
We assessed general obesity with body mass index (BMI; weight in kilograms divided by the square of height in meters). We calculated BMI from body weight and height measured at baseline (t0), and at 2-year (t1), 4-year (t2), and 6-year (t3) follow-up. We classified participants into 2 BMI categories according to the standard international classification of the World Health Organization (nonobese < 30 kg/m2, and obese ≥ 30.0 kg/m2). We defined abdominal obesity as having a waist circumference of 102 centimeters or greater for men and 88 centimeters or greater for women.21,22
Major depression.
We assessed major depression with the Composite International Diagnostic Interview (CIDI) 2.1, a highly reliable and valid instrument for assessing depressive and anxiety disorders. The CIDI is a structured clinical interview and diagnoses according to definitions and criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).23 The CIDI contains questions directly corresponding to the symptoms of axis I psychiatric disorders listed in the DSM-IV. It translates the criteria of DSM-IV into questions that can be readily and reliably answered by the general population. We diagnosed participants at baseline (t0), and at 2-year (t1), 4-year (t2), and 6-year (t3) follow-up. CIDI-trained interviewers (e.g., graduate students in psychology) conducted the interview under the supervision of clinicians. As remitted major depression was not associated with obesity,24 we dichotomized current major depression into individuals who were diagnosed positive and negative for the DSM-IV criteria of major depression in the past 6 months.25
Work performance impairment.
We measured work performance impairment with the Trimbos/Institute for Medical Technology Assessment Questionnaire for Costs Associated With Psychiatric Illness.26 We used the following questions and items to assess WPI: “On how many days in the last 6 months have you been working while hindered by health problems?” and “How efficient have you been working on the days that you were at work but were also hindered by health problems?”11 The scores ranged between 0 (inefficient) and 1 (efficient). We computed WPI with the following formula, in which a higher rate indicates more impairment:
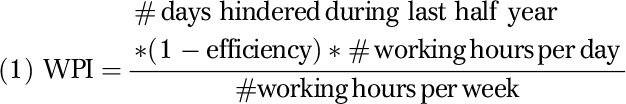 |
For example, the WPI rate of someone working 8 hours per day, 40 hours a week, who reported 25 days hindered, and a score of 0.8 at the efficiency scale, is 25 × (1-0.8) × 8/40 = 1. The variable ranged from 0 to 39 and did not meet normality assumptions. Therefore, we dichotomized WPI (low, high) by taking the highest quartile (> 1.60) as cutoff point.11
Covariates.
Covariates concerned sociodemographic characteristics (age, gender, educational status, and working hours). We used age as a continuous variable. We categorized educational level into low (primary and lower secondary education), middle (higher secondary education), and high (tertiary or higher education). We assessed anxiety disorders with the CIDI 2.1 and defined them as having a diagnosis of anxiety disorders at least once during their lifetime.
Statistical Analysis
We analyzed data in 3 steps. First, we described the characteristics of the cohort by using means and proportions by obesity and major depression status.
Second, we examined the separate effects of general obesity, abdominal obesity, and major depression on high WPI by using generalized estimating equations (GEEs), which allow correlated observations over time and missing values at different measurement points.27 We used an exchangeable correlation structure to take within-subject dependencies into account. In this structure we assumed the correlations between subsequent measurements to be the same, irrespective of the length of the time interval. We checked the goodness of fit by quasi likelihood under independence model criterion in time-lag models. In these models, the value of the outcome WPI at tx+1 (x = 0, 1,…) was longitudinally associated with obesity, major depression, or both at time-point tx over 6 years.28 The odds ratios (ORs) resulting from GEE logistic regression analyses can be interpreted as the longitudinal relationships between the predictors (obesity or depression or their combination) with high WPI.28 We adjusted all analyses for age, gender, and educational status. We adjusted for any potential relationship between age and the determinants and outcome by including age and age-squared in the models. We checked interactions between obesity and major depression × gender and obesity and major depression × time by entering the centered interaction terms in the gender or time-adjusted models for the outcome variable.
Third, we examined whether the joint effect of obesity and major depression on high WPI is larger than the sum of separate effects of obesity and major depression on high WPI. We created a 4-category variable, nonobese and nondepressed, obese, depressed, and both obese and depressed. If obesity is present, then i = 1; otherwise i = 0. If major depression is present, then j = 1; otherwise j = 0. Then, ORij represented the OR in both obese and depressed category i, j. We computed the 3 OR estimates (i.e., OR11, OR10, OR01, and OR00 [reference category]) from the GEE analyses. We assumed that obesity and major depression modify each other regarding the risk of high WPI, and that neither of them fully precedes the other. We also assumed that the effects of both exposures on high WPI were unconfounded. We assessed the presence of interactions on the additive scale by using the RERI and the AP. We defined RERI as RERI = OR11−OR10−OR01+1, and AP = RERI/OR11. We calculated 95% confidence intervals (CIs) for the RERI and AP by using the algorithm of Andersson et al. with covariances of parameter estimates from GEE models.18,19 A positive interaction of obesity and major depression with high WPI is reflected by a RERI or AP > 0, and an RERI or AP < 0, represents a negative interaction of obesity and major depression; RERI or AP = 0 indicates that there is no interaction (additivity) in the association of obesity and major depression with WPI. We assessed the presence of interaction on the multiplicative scale by including the product term (obesity × major depression) in the obesity and major depression adjusted model, and defined as OR11/(OR10 × OR01), which reflects whether the joint effect of obesity and major depression was larger than the product of the separate effects of obesity and major depression on high WPI.
We performed all statistical analyses with SPSS version 20.0 (IBM, Somers, NY). We considered effects significant when the 95% CI of OR and RERI did not contain 1 and 0, respectively.
RESULTS
Table 1 shows the baseline characteristics of the 1726 respondents by obesity and major depression status. At baseline, the prevalences of general obesity and abdominal obesity were 14% and 32%, respectively. A total of 555 employees (32%) were diagnosed with major depression in the past 6 months. The prevalences of general and abdominal obesity in participants with major depression were 18% and 34%, respectively. Out of those participants diagnosed with major depression, 72% were diagnosed with anxiety disorder at least once during their lifetime. Most workers (80%) were white collar (nonmanual) workers. High WPI at baseline was significantly correlated with WPI at 2-year (κ = 0.20), 4-year (κ = 0.18), and 6-year (κ = 0.13) follow-up (P < .001), indicating stability of WPI over time.
TABLE 1—
Baseline Characteristics of Sample by Obesity and Major Depression Status: Netherlands Study of Depression and Anxiety, 2004–2007
| Characteristics | Total Population (n = 1726), % or Mean (SD) | Nonobese and No Major Depression (n = 1024), % or Mean (SD) | Obese Without Major Depression (n = 147), % or Mean (SD) | Major Depression Without Obesity (n = 457), % or Mean (SD) | Both Obesity and Major Depression (n = 98), % or Mean (SD) | ANOVA/χ2 |
| Age, y | 41.0 (11.7) | 40.7 (11.9) | 46.5 (11.0) | 39.4 (11.3) | 43.3 (10.0) | P < .001 |
| Women | 64.6 | 64.6 | 59.2 | 68.1 | 57.1 | P < .05 |
| Educational status | ||||||
| Low | 4.2 | 2.6 | 7.5 | 5.5 | 10.2 | P < .001 |
| Middle | 53.1 | 47.8 | 62.6 | 57.8 | 73.5 | |
| High | 42.7 | 49.6 | 29.9 | 36.8 | 16.3 | |
| Working hours | 31.1 (10.7) | 30.8 (10.1) | 33.1 (13.5) | 30.8 (10.5) | 32.5 (12.9) | P < .05 |
| Abdominal obesitya | 31.7 | 21.7 | 95.2 | 20.1 | 95.9 | P < .001 |
| Anxiety disorder | 55.8 | 47.9 | 49.0 | 71.6 | 75.5 | P < .001 |
| High WPI | 24.7 | 14.9 | 24.5 | 42.2 | 44.9 | P < .001 |
Note. ANOVA = analysis of variance; WPI = work performance impairment.
Waist circumference ≥ 102 cm for men and ≥ 88 cm for women; obesity (body mass index ≥ 30 kg/m2).
We found longitudinal associations between general and abdominal obesity at tx and high WPI at tx+1 (OR = 1.45; 95% CI = 1.16, 1.80, and OR = 1.34; 95% CI = 1.12, 1.59, respectively). Adjustment for age, gender, and educational status slightly attenuated the estimates for the longitudinal association between general and abdominal obesity and high WPI (Table 2). We found no significant interactions between gender × obesity and time × obesity on high WPI.
TABLE 2—
The Longitudinal Relation Between Obesity at tx and Major Depression at tx With High Work Performance Impairment at tx+1: Netherlands Study of Depression and Anxiety, 2004–2013
| High Work Performance Impairmenta |
||
| Predictors | OR (95% CI) | AORb (95% CI) |
| Obesity status | ||
| Nonobese (Ref) | 1.00 | 1.00 |
| Obesity (BMI ≥ 30 kg/m2) | 1.45* (1.16, 1.80) | 1.35* (1.08, 1.69) |
| Abdominal obesity status | ||
| No abdominal obesity (Ref) | 1.00 | 1.00 |
| Abdominal obesityc | 1.34* (1.12, 1.59) | 1.23* (1.03, 1.48) |
| Major depression status | ||
| No major depression (Ref) | 1.00 | 1.00 |
| Major depression | 1.66* (1.38, 2.00) | 1.63* (1.35, 1.96) |
Note. AOR = adjusted odds ratio; BMI = body mass index; CI = confidence interval; OR = odds ratio.
Reference: low work performance impairment.
Adjusted for age, gender, and educational status.
Waist circumference ≥ 102 cm for men and ≥ 88 cm for women.
*P < .05.
We found a longitudinal association between major depression at tx and high WPI at tx+1 (OR = 1.66; 95% CI = 1.38, 2.00). After we adjusted for age, gender, and educational status, the association attenuated but remained statistically significant (Table 2). We found no significant interactions between gender × major depression, and time × major depression on high WPI.
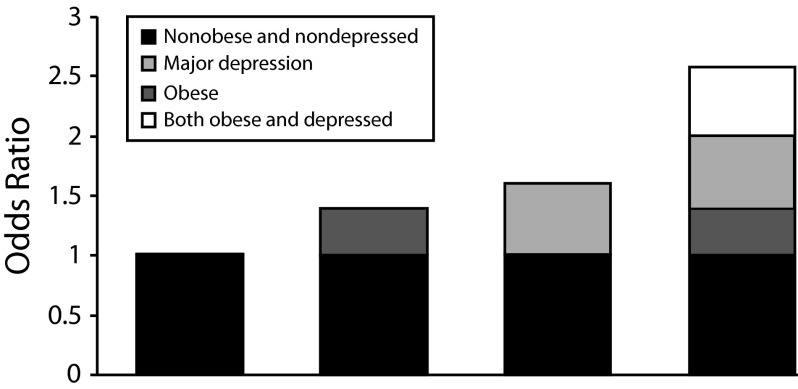
We found a longitudinal joint association of general obesity and major depression at tx and high WPI at tx+1 compared with nonobese and nondepressed counterparts (OR = 2.57; 95% CI = 1.77, 3.74; Table 3). After we adjusted for age, gender, and educational status, the association attenuated but remained statistically significant (OR = 2.36; 95% CI = 1.61, 3.44). The joint association of general obesity and major depression on high WPI was additive (RERI = 0.57 [95% CI = –0.46, 1.60] and AP = 0.22 [95% CI = –0.11, 0.55]). The interaction on the multiplicative scale was OR = 1.15 (95% CI = 0.71, 1.85; Table 3 and Figure 1). Similarly, the joint association of abdominal obesity and major depression on high WPI was additive (RERI = −0.09 [95% CI = –0.46, 0.61] and AP = −0.04 [95% CI = –0.39, 0.30]). The interaction on the multiplicative scale was OR = 0.84 (95% CI = 0.57, 1.24).
TABLE 3—
The Longitudinal Separate and Joint Associations of Obesity tx and Major Depression tx With High Work Performance Impairment tx+1: Netherlands Study of Depression and Anxiety, 2004-2013
| High Work Performance Impairmenta |
||||
| Predictors | OR (95% CI) | AORb (95% CI) | Additivity RERI (95% CI)c | Multiplicativity OR (95% CI)d |
| General obesity and major depression | ||||
| Nonobese and nondepressed | 1.00 (Ref) | 1.00 (Ref) | ||
| Obesity (BMI ≥ 30 kg/m2) | 1.39* (1.07, 1.80) | 1.31* (1.01, 1.70) | ||
| Major depression | 1.62* (1.31, 1.99) | 1.59* (1.29, 1.96) | ||
| Both obese and major depression | 2.57* (1.77, 3.74) | 2.36* (1.61, 3.44) | 0.57 (–0.46, 1.60) | 1.15 (0.71, 1.85) |
| Abdominal obesity and major depression | ||||
| Nonobese and nondepressed | 1.00 (Ref) | 1.00 (Ref) | ||
| Abdominal obesitye | 1.39* (1.14, 1.70) | 1.29* (1.05, 1.58) | ||
| Major depression | 1.77* (1.40, 2.24) | 1.74* (1.37, 2.20) | ||
| Both obese and major depression | 2.07* (1.55, 2.78) | 1.88* (1.40, 2.53) | −0.09 (–0.79, 0.61) | 0.84 (0.57, 1.24) |
Note. AOR = adjusted odds ratio; CI = confidence interval; OR = odds ratio; RERI = relative excess risk due to interaction.
Reference: low work performance impairment.
Adjusted for age, gender, and educational status at baseline.
Waist circumference ≥ 102 cm for men and ≥ 88 cm for women.
Departure from additivity; RERI = OR11−OR10−OR01+1 = 2.57–1.39–1.62+1 = 0.57.
Departure from multiplicativity; OR11/(OR10 × OR01) = 2.57/(1.62 × 1.39) = 1.15.
*P < .05.
FIGURE 1—
Cumulative risk of high work performance impairment associated with the separate and joint exposures to obesity and major depression: Netherlands Study of Depression and Anxiety, 2004–2013.
DISCUSSION
To our best knowledge, this is the first study examining the longitudinal effects of general and abdominal obesity, major depression, and their combination on high WPI over 6-year follow-up. Obesity and major depression were independently associated with an increased risk of high WPI. Moreover, the combination of obesity and major depression was also associated with an increased risk of high WPI. The interactions between obesity and major depression on high WPI on the additive and the multiplicative scale were in the expected direction (i.e., positive interaction), but not statistically significant. This refutes the hypothesis that the joint effect of obesity and major depression on high WPI is larger than the sum of the separate effects of obesity and major depression on high WPI.
Our finding that obesity was longitudinally associated with an increased risk of high WPI is consistent with a nationwide prospective cohort study in the United States.29 That study found that obesity among employed women was associated with more self-reported work limitations compared with among normal-weight employed women.29 Dutch and Swedish studies also found associations of obesity with high productivity loss at work and work impairment.30–32 These findings across countries suggest that obesity is a global public and occupational health problem with a strong relationship with WPI.
The finding that major depression was longitudinally associated with an increased risk of high WPI confirms conclusions of a systematic review33 that showed a robust relationship between depressive disorders and work limitations. Several other studies have also reported consistent findings regarding the association of major depression and productivity loss at work.12,34–37 However, another Dutch study, the Netherlands Mental Health Survey and Incidence Study (NEMESIS), found no association between major depression or anxiety and impaired work performance.34 Possible explanations for this discrepancy are the differences in sampling and in assessment of major depression between the NEMESIS and NESDA cohort studies. NEMESIS comprised a representative sample of the general population, and NESDA included individuals with anxiety and depressive disorders from the community and primary and secondary health care.20 The prevalence of depression in the NEMESIS study was lower (5.2%) and concerned at average milder cases compared with NESDA.34 This might also be associated with the different DSM versions that were used to assess major depression. The NEMESIS study used DSM-III, whereas NESDA used the updated version, DSM-IV. In the DSM-IV, a clinical significance criterion for depression has been included that requires the depressive symptoms to cause clinically significant impairment in social activities, or occupational or other functioning.23
We found that the observed joint effect of obesity and major depression on high WPI was slightly larger than would have been expected on the additive scale. For the joint exposures obesity and major depression, the additional risk of high WPI was 157%, and the risk attributable to obesity and major depression was 101% (39% to obesity and 62% to major depression), leading to a RERI of 0.57. However, the RERI was not statistically significant. A possible explanation for the nonsignificant interaction between obesity and major depression on high WPI is that there is a tendency that patients with major depression or anxiety show clinical recovery over time even though residual symptoms of depression or anxiety often persist.38,39 This characteristic of major depression might influence the interaction effect on high WPI. It has also been shown that obesity is more strongly associated with more severe and chronic forms of major depression as opposed to a current and a broader diagnosis of major depression.25,40 Moreover, the interplay between obesity and major depression may need more time to lead to an actual interaction effect beyond additive effects. Another, more pragmatic explanation why the RERI is not significant is the rather small sample size for the subgroup analysis of obesity and major depression status categories with WPI.
It is possible that major depression shares genetic and complex biological, etiological substrates with obesity,13,41,42 which could explain the observed joint effect of obesity and major depression on high WPI (i.e., positive direction on the additive and multiplicative scale). For instance, gene–environment interactions may have activated the hypothalamic–pituitary–adrenal axis, which subsequently has led to depression and aggravation of obesity. Moreover, the alteration of neurotransmitters’ function and hormonal disturbances play an important role in the development and maintenance of both obesity and depressive disorders.41,42 Obesity and major depression are also independent risk factors for chronic conditions such as cardiovascular diseases, diabetes, and musculoskeletal disorders.1,2 These mechanisms and comorbidities could explain the observed joint effect of obesity and major depression on high WPI in our study population.
Strengths and Limitations
The major strength of our study is its prospective design. We were able to examine longitudinal associations of obesity and major depression at 1 point in time with high WPI 2 years later over a 6-year follow-up period by using time-lag models (i.e., the temporal association was maintained). This supports assumptions on causality, though not conclusive ones. Moreover, we used psychiatric interviews to diagnose major depression instead of self-reports as often used before. We assessed obesity by using 2 anthropometric measurements (i.e., BMI and waist circumference) because many researchers have been criticizing the BMI for its inadequate reflection of body composition, which does not differentiate between fat mass and lean body mass, or between abdominal adiposity and general fatness. We have estimated interactions on additive and multiplicative scales.
We should also keep some limitations in mind. First, the NESDA study is a representative sample of a population with common mental disorders (i.e., depressive and anxiety disorders). Because of this, a rather large proportion of the participants had prevalent depressive or anxiety disorders, implying that nondepressed obese employees may be underrepresented. Nevertheless, we expect that the resulting study cohort is representative and generalizable to other settings in high-income countries because the prevalence of obesity in our study (14%) is comparable with that in the Dutch population (12%),43 and within the range of the World Health Organization European region prevalence (10%–30%).1 Furthermore, large-scale epidemiological studies have shown that the prevalence of both depression and anxiety disorders in the Netherlands is in the range of other high-income countries such as the United States, Germany, or Canada.44 The structure of the Dutch Health Care System is also comparable to that of several other European countries (e.g., United Kingdom, Germany) in which the general practitioner serves as the gatekeeper. In NESDA, 50% of the participants were recruited via general practices.
Another limitation with respect to the outcome might be that the WPI measure, which was based upon self-report and not on employer-reported data, may have been biased by depressive or anxiety symptoms. However, it has been shown that self-reported decreased work performance is highly correlated with employer payroll records.45 Finally, we used the number of days the respondent worked while hindered by health problems to compute WPI. It is not known explicitly whether the impairment was caused by depressive or anxiety disorders or by any other specific disease.
Implications and Conclusions
The findings demonstrate that obesity and major depression are important public and occupational health problems. Both obesity and major depression are separately and jointly associated with an increased risk of high WPI. Probably, more severe or recurrent forms of major depression might further increase the risk of high WPI in obese employees, as obesity is more strongly associated with recurrent or chronic depression than single or short episodes of major depression.40 If the RERI is confirmed in further studies, the joint effect of obesity and major depression on high WPI could have public and occupational health implications. Intervening on obesity may be more beneficial for individuals with major depression compared with those without major depression regarding the risk of high WPI. Hence, further research is needed to reexamine the joint effect of obesity and major depression in relation to high WPI in larger sample sizes and in the general population.
In conclusion, our study suggests that there is a longitudinal relationship of obesity, abdominal obesity, and major depression with an increased risk of high WPI. The longitudinal joint effect of obesity and major depression on high WPI implies that intervening on obesity may be more beneficial for individuals with major depression compared with those without major depression regarding the risk of high WPI, if confirmed in a large representative sample.
Acknowledgments
The infrastructure for the Netherlands Study of Depression and Anxiety (NESDA) (http://www.nesda.nl) is funded by the Netherlands Organization for Health Research and Development (Zon-Mw, grant 10-000-1002) and is supported by participating universities and mental health care organizations: VU University Medical Center, Geestelijke Gezondheidszorg (GGZ) in Geest, Arkin, Leiden University Medical Center, GGZ Rivierduinen, University Medical Center Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Scientific Institute for Quality of Healthcare, Netherlands Institute for Health Services Research, and Netherlands Institute of Mental Health and Addiction (Trimbos Institute).
Human Participant Protection
The NESDA study protocol was approved by the ethical review board of the VU University Medical Center and subsequently by local review boards of each participating center. After full verbal and written information about the study, written informed consent was obtained from all participants. The study was conducted in accordance with the Declaration of Helsinki.
References
- 1.Kessler RC, Berglund P, Demler O et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.Kelly T, Yang W, Chen CS et al. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 2008;32(9):1431–1437. doi: 10.1038/ijo.2008.102. [DOI] [PubMed] [Google Scholar]
- 3.Olesen J, Gustavsson A, Svensson M et al. The economic cost of brain disorders in Europe. Eur J Neurol. 2012;19(1):155–162. doi: 10.1111/j.1468-1331.2011.03590.x. [DOI] [PubMed] [Google Scholar]
- 4.Proper KI, Hildebrandt VH. Overweight and obesity among Dutch workers: differences between occupational groups and sectors. Int Arch Occup Environ Health. 2010;83(1):61–68. doi: 10.1007/s00420-009-0438-1. [DOI] [PubMed] [Google Scholar]
- 5.Pandalai SP, Schulte PA, Miller DB. Conceptual heuristic models of the interrelationships between obesity and the occupational environment. Scand J Work Environ Health. 2013;39(3):221–232. doi: 10.5271/sjweh.3363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schulte PA, Wagner GR, Ostry A et al. Work, obesity, and occupational safety and health. Am J Public Health. 2007;97(3):428–436. doi: 10.2105/AJPH.2006.086900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neovius K, Johansson K, Kark M et al. Obesity status and sick leave: a systematic review. Obes Rev. 2009;10(1):17–27. doi: 10.1111/j.1467-789X.2008.00521.x. [DOI] [PubMed] [Google Scholar]
- 8.Neovius K, Neovius M, Kark M et al. Association between obesity status and sick-leave in Swedish men: nationwide cohort study. Eur J Public Health. 2012;22(1):112–116. doi: 10.1093/eurpub/ckq183. [DOI] [PubMed] [Google Scholar]
- 9.Gilmour H, Patten SB. Depression and work impairment. Health Rep. 2007;18(1):9–22. [PubMed] [Google Scholar]
- 10.Sanderson K, Cocker F. Presenteeism—implications and health risks. Aust Fam Physician. 2013;42(4):172–175. [PubMed] [Google Scholar]
- 11.Plaisier I, de Graaf R, de Bruijn J et al. Depressive and anxiety disorders on-the-job: the importance of job characteristics for good work functioning in persons with depressive and anxiety disorders. Psychiatry Res. 2012;200(2-3):382–388. doi: 10.1016/j.psychres.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Plaisier I, Beekman AT, de Graaf R, Smit JH, van Dyck R, Penninx BW. Work functioning in persons with depressive and anxiety disorders: the role of specific psychopathological characteristics. J Affect Disord. 2010;125(1-3):198–206. doi: 10.1016/j.jad.2010.01.072. [DOI] [PubMed] [Google Scholar]
- 13.Afari N, Noonan C, Goldberg J et al. Depression and obesity: do shared genes explain the relationship? Depress Anxiety. 2010;27(9):799–806. doi: 10.1002/da.20704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Markowitz S, Friedman MA, Arent SM. Understanding the relation between obesity and depression: causal mechanisms and implications for treatment. Clin Psychol Sci Pract. 2008;15:1–20. [Google Scholar]
- 15.Kivimäki M, Lawlor DA, Singh-Manoux A et al. Common mental disorder and obesity: insight from four repeat measures over 19 years: prospective Whitehall II cohort study. BMJ. 2009;339:b3765. doi: 10.1136/bmj.b3765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luppino FS, de Wit LM, Bouvy PF et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 17.Needham BL, Epel ES, Adler NE, Kiefe C. Trajectories of change in obesity and symptoms of depression: the CARDIA study. Am J Public Health. 2010;100(6):1040–1046. doi: 10.2105/AJPH.2009.172809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41(2):514–520. doi: 10.1093/ije/dyr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andersson T, Alfredsson L, Kallberg H et al. Calculating measures of biological interaction. Eur J Epidemiol. 2005;20(7):575–579. doi: 10.1007/s10654-005-7835-x. [DOI] [PubMed] [Google Scholar]
- 20.Penninx BW, Beekman AT, Smit JH et al. The Netherlands Study of Depression and Anxiety (NESDA): rationale, objectives and methods. Int J Methods Psychiatr Res. 2008;17(3):121–140. doi: 10.1002/mpr.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. World Health Organization. Obesity. 2014. Available at: http://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity. Accessed December 20, 2014.
- 22. Waist circumference and waist–hip ratio: report of a WHO expert consultation. Geneva, Switzerland: World Health Organization; 2008.
- 23.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 24.de Wit LM, Fokkema M, van Straten A et al. Depressive and anxiety disorders and the association with obesity, physical, and social activities. Depress Anxiety. 2010;27(11):1057–1065. doi: 10.1002/da.20738. [DOI] [PubMed] [Google Scholar]
- 25.van Reedt Dortland AK, Giltay EJ, van Veen T et al. Longitudinal relationship of depressive and anxiety symptoms with dyslipidemia and abdominal obesity. Psychosom Med. 2013;75(1):83–89. doi: 10.1097/PSY.0b013e318274d30f. [DOI] [PubMed] [Google Scholar]
- 26.Hakkaart-van Roijen L. Rotterdam, The Netherlands: Institute for Medical Technology Assessment; 2002. Trimbos/iMTA Questionnaire for Costs Associated With Psychiatric Illness (TIC-P) [Google Scholar]
- 27.Shek DT, Ma CM. Longitudinal data analyses using linear mixed models in SPSS: concepts, procedures and illustrations. ScientificWorldJournal. 2011;11:42–76. doi: 10.1100/tsw.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Twisk JW. Applied Longitudinal Data Analysis for Epidemiology: A Practical Guide. Cambridge, UK: Cambridge University Press; 2003. pp. 102–144. [Google Scholar]
- 29.Tunceli K, Li K, Williams LK. Long-term effects of obesity on employment and work limitations among U.S. Adults, 1986 to 1999. Obesity (Silver Spring) 2006;14(9):1637–1646. doi: 10.1038/oby.2006.188. [DOI] [PubMed] [Google Scholar]
- 30.Neovius K, Rehnberg C, Rasmussen F et al. Lifetime productivity losses associated with obesity status in early adulthood: a population-based study of Swedish men. Appl Health Econ Health Policy. 2012;10(5):309–317. doi: 10.1007/BF03261865. [DOI] [PubMed] [Google Scholar]
- 31.Robroek SJ, van den Berg TI, Plat JF et al. The role of obesity and lifestyle behaviours in a productive workforce. Occup Environ Med. 2011;68(2):134–139. doi: 10.1136/oem.2010.055962. [DOI] [PubMed] [Google Scholar]
- 32.Striegel RH, Bedrosian R, Wang C. Comparing work productivity in obesity and binge eating. Int J Eat Disord. 2012;45(8):995–998. doi: 10.1002/eat.22069. [DOI] [PubMed] [Google Scholar]
- 33.Lagerveld SE, Bultmann U, Franche RL et al. Factors associated with work participation and work functioning in depressed workers: a systematic review. J Occup Rehabil. 2010;20(3):275–292. doi: 10.1007/s10926-009-9224-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Michon HW, ten Have M, Kroon H et al. Mental disorders and personality traits as determinants of impaired work functioning. Psychol Med. 2008;38(11):1627–1637. doi: 10.1017/S0033291707002449. [DOI] [PubMed] [Google Scholar]
- 35.Rytsälä HJ, Melartin TK, Leskela US et al. Functional and work disability in major depressive disorder. J Nerv Ment Dis. 2005;193(3):189–195. doi: 10.1097/01.nmd.0000154837.49247.96. [DOI] [PubMed] [Google Scholar]
- 36.Lerner D, Adler DA, Rogers WH et al. Work performance of employees with depression: the impact of work stressors. Am J Health Promot. 2010;24(3):205–213. doi: 10.4278/ajhp.090313-QUAN-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Spijker J, Graaf R, Bijl RV et al. Functional disability and depression in the general population. Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Acta Psychiatr Scand. 2004;110(3):208–214. doi: 10.1111/j.1600-0447.2004.00335.x. [DOI] [PubMed] [Google Scholar]
- 38.Bothwell R, Scott J. The influence of cognitive variables on recovery in depressed inpatients. J Affect Disord. 1997;43(3):207–212. doi: 10.1016/s0165-0327(97)01431-6. [DOI] [PubMed] [Google Scholar]
- 39.van Reedt Dortland AK, Giltay EJ, van Veen T et al. Associations between serum lipids and major depressive disorder: results from the Netherlands Study of Depression and Anxiety (NESDA) J Clin Psychiatry. 2010;71(6):729–736. doi: 10.4088/JCP.08m04865blu. [DOI] [PubMed] [Google Scholar]
- 40.Nigatu Y, Bültmann U, Reijneveld S. The prospective association between obesity and major depression: a longitudinal cohort study in the general population. Eur J Public Health. 2013;23(suppl 1):62–63. [Google Scholar]
- 41.Penninx BW, Milaneschi Y, Lamers F, Vogelzangs N. Understanding the somatic consequences of depression: biological mechanisms and the role of depression symptom profile. BMC Med. 2013;11:129. doi: 10.1186/1741-7015-11-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thormann J, Chittka T, Minkwitz J et al. Obesity and depression: an overview on the complex interactions of two diseases [in German] Fortschr Neurol Psychiatr. 2013;81(3):145–153. doi: 10.1055/s-0032-1330351. [DOI] [PubMed] [Google Scholar]
- 43. Statistics Netherlands. Statline. 2014. Available at: http://statline.cbs.nl/StatWeb/publication/?VW=T&DM=SLEN&PA=37852eng&LA=EN. Accessed December 15, 2014.
- 44.Andrade L, Caraveo-Anduaga JJ, Berglund P et al. The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res. 2003;12(1):3–21. doi: 10.1002/mpr.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kessler RC, Barber C, Beck A et al. The World Health Organization Health and Work Performance Questionnaire (HPQ) J Occup Environ Med. 2003;45(2):156–174. doi: 10.1097/01.jom.0000052967.43131.51. [DOI] [PubMed] [Google Scholar]