Abstract
Objectives. We aimed to determine whether loneliness is associated with higher health care utilization among older adults in the United States.
Methods. We used panel data from the Health and Retirement Study (2008 and 2012) to examine the long-term impact of loneliness on health care use. The sample was limited to community-dwelling persons in the United States aged 60 years and older. We used negative binomial regression models to determine the impact of loneliness on physician visits and hospitalizations.
Results. Under 2 definitions of loneliness, we found that a sizable proportion of those aged 60 years and older in the United States reported loneliness. Regression results showed that chronic loneliness (those lonely both in 2008 and 4 years later) was significantly and positively associated with physician visits (β = 0.075, SE = 0.034). Loneliness was not significantly associated with hospitalizations.
Conclusions. Loneliness is a significant public health concern among elders. In addition to easing a potential source of suffering, the identification and targeting of interventions for lonely elders may significantly decrease physician visits and health care costs.
Social relationships are integral to human well-being, and research consistently documents that social integration and support have protective effects on morbidity and mortality outcomes.1–4 Yet loneliness and social isolation are often overlooked, despite being vital public health concerns, with mortality risk comparable to well-established risk factors such as cigarette smoking and even exceeding the influence of physical activity and obesity.5
Often described as the discrepancy between desired and perceived social relationships,6 loneliness can be particularly important among older adults, for whom decreases in economic resources, increases in impairments, and the deaths of contemporaries can heighten the risk of social isolation and loneliness.3 Prevalence statistics indicate that nearly 1 in 3 older adults report loneliness in the United States.7 Although loneliness is not a problem exclusively for elders, the oldest old (those aged 80 years and older) appear to have relatively high rates of loneliness—by some estimates, 40% to 50% report that they are often lonely.8
Research has consistently found that social relationships are associated with a variety of comorbid conditions, in addition to premature mortality. Negative health outcomes linked to loneliness include high blood pressure,9 cardiovascular disease,10 disability,11 cognitive decline,12 and depression.13 Such morbidities may, in turn, create higher need for health care and be linked to higher health care utilization,14 especially among older adults, who are more likely to suffer from multiple conditions.15
Some research suggests that there may also be a direct link between loneliness and health care utilization, regardless of health status. Although relatively limited, research has found that socially isolated persons are more likely to seek medical assistance to satisfy their need for interaction and interpersonal stimulation.16–18 In a study of older women in the San Francisco, California, area, Cheng found that loneliness–distress significantly explained higher physician utilization, independent of health factors.18 Similar findings have been reported in Europe. In Sweden, researchers found that frail elders who were lonely used more outpatient services than those who were not lonely. This included contacts with a physician and more visits to an emergency department as an outpatient.19 Among elders in Ireland, loneliness was independently associated with emergency hospitalization.20 And in Scotland, researchers found that among their sample of people aged 40 and 60 years, those who were lonely reported greater frequency of consultation with a general practitioner or family doctor.17 In essence, it is possible that lonely persons seek physician care less for medical needs than to have someone to talk to.
Despite the high prevalence of loneliness and its clear implications on health outcomes, relatively little attention has been paid by public health officials and other medical professionals to the importance of loneliness,5 especially in the United States. We examined the impact of loneliness on a tangible public health and public policy outcome: health care utilization.
METHODS
We used data from the 2008 and 2012 Health and Retirement Study (HRS). The HRS is a multistage national area probability study of a sample of households in the United States. The HRS has been widely used by researchers to study a large variety of issues in aging, including loneliness.21 In addition to an in-person interview, the HRS includes a self-administered questionnaire, which a subsample of participants are asked to return by mail. This “Leave Behind” (LB) questionnaire is intended to obtain information about the respondent’s psychosocial well-being, including loneliness. In 2008, the response rate for the LB questionnaire was 71%.
We linked data from respondents in the 2008 HRS wave to data from their interviews in the 2012 HRS wave. Although the HRS is conducted biannually, respondents receive the LB questionnaire only every other wave, so that those who completed the LB survey in 2008 were not reinterviewed on the in-depth psychosocial well-being questions until 2012.
The sample was limited to persons aged 60 and older in 2008, living in the community (excluding respondents in nursing homes at either wave), and completing all 3 questions on the loneliness scale in both waves. The sample included 3530 respondents in 2008 who were followed up with the questionnaire in 2012, resulting in a balanced sample of 7060 total observations. The unit of analysis was individual year.
Measures
Health care utilization.
To examine the impact of loneliness on health care utilization, we examined hospitalization and physician visits. We measured hospitalization by self-reported number of different times the respondent was a patient in a hospital in the past 2 years. Because this variable had large outliers, we top coded it at the 99th percentile, with the final category counting 10 or more hospitalizations.
Respondents were also asked the number of times they had seen or talked to a medical doctor about their health (aside from hospital stays and outpatient surgery) in the last 2 years. This variable was also top coded at the 99th percentile, at 60 or more doctor visits.
Loneliness.
Our primary predictor variable was loneliness. We measured loneliness using the 3-item loneliness scale developed by Hughes et al. in 2004.21 The LB questionnaire included questions about how much of the time they felt that they (1) lacked companionship, (2) felt left out, and (3) felt isolated from others. Response options for each question were as follows: 1 = often, 2 = some of the time, 3 = hardly ever or never. Once items were reverse scored, we summed them to create an index of loneliness, with higher scores on the scale indicating higher loneliness (range = 3–9). The sample showed acceptable psychometrics, with an α of 0.81.
Following previous research,7 we also created a dichotomous measure of lonely versus not lonely to aid in the interpretation of the results. We coded persons who responded “some of the time” or “often” to any of these 3 measures as lonely. We did this for both 2008 and 2012, creating a dichotomous measure for each wave. We then used the dichotomous measure to determine loneliness across time, creating 4 options: (1) not lonely at either time, (2) lonely at both times, (3) lonely only in 2008, and (4) lonely only in 2012. Lonely at both times was considered “chronic loneliness.” We used “not lonely at either time” as the reference category in regression analyses. However, we also performed a sensitivity analysis using an alternative definition of loneliness from previous research.7 By this alternative definition, individuals were lonely only if they responded “some of the time” or “often” to at least 2 of the 3 items in the scale, and not lonely otherwise.
Additional control variables.
Additional variables entered into the models included demographics as well as variables associated with loneliness and the health outcomes. These included age (continuous), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic other), education (high school or general equivalency diploma [GED] vs more education), gender (male = reference), depressive symptoms (using the Center for Epidemiologic Studies Depression Scale [CES-D] continuous score, we created a dummy variable in which CES-D ≥ 3 was considered high depressive symptoms), health insurance (availability of at least 1 type of insurance), and marital status (married vs not married). Because income measures have a high rate of nonresponse, we used a subjective measure to control for financial situation, using the survey question that asked respondents how satisfied they were with their current financial situation: satisfied (completely, very, somewhat) or not satisfied (not very, not at all).
Because health care utilization is highly connected to health status, we included 2 measures of health, 1 objective and 1 subjective. The subjective measure was the respondent’s self-rated health, measured on a 5-point Likert scale ranging from poor to excellent. We recoded this into a dichotomous variable comparing “good, very good, or excellent health” with “fair or poor health.” Adapting previous research on loneliness,7,22 we used respondents’ self-report to capture the following objective health measures: high blood pressure, diabetes, cancer, lung disease, heart disease, stroke, or arthritis. We created a count variable for the number of chronic conditions reported.
We also included a disability measure, using the Activities of Daily Living (ADL) Scale.23 ADLs were measured by 6 items included in the LB survey, which asked respondents if they had difficulty with the following activities: bathing, eating, toileting, dressing, transferring to and from bed, and walking. We added the number of activities the respondent reported having difficulty with, which resulted in a variable ranging from 0 to 6. We also included a year dummy variable to control for time effects in the data.
Statistical Analyses
We present descriptive statistics of the sample by year (2008 vs 2012) and loneliness category (lonely vs not lonely). We conducted significance tests within each year, using the χ2 test to examine statistical significance in categorical variables and the t test for continuous variables.
Because observations were available for 2 time periods for the same individuals, we used panel data analysis.24 Therefore, to find the associations between loneliness and health care utilization (doctor visits and hospitalizations), we conducted a panel count data analysis using panel negative binomial regression method, since it helps to control overdispersion in the data.24 In addition to other covariates, we included time dummy indicators to implicitly control for possible time trends in the data. In both regression models, we analyzed the data using both population-averaged negative binomial estimator and negative binomial estimator with cluster-robust standard errors at the individual level, which produced similar results. We present the results from the population-averaged negative binomial estimators. In addition to results from our primary analyses, we present the results from the sensitivity analysis using the alternative definition of loneliness. We conducted all the analyses using Stata version 11.1 (StataCorp LP, College Station, TX).
RESULTS
Table 1 shows the prevalence of loneliness in each year by the primary and alternative definitions of loneliness. By our primary definition of loneliness (a response of “some of the time” or “often” to any of the 3 scale measures), more than half the population was lonely in both years. By a stricter (alternative) definition of loneliness (a response of “some of the time” or “often” to at least 2 of the 3 items), more than one third of the sample was lonely in both years. For both definitions, the prevalence of loneliness increased over the 4 years by several percentage points.
TABLE 1—
Prevalence of Loneliness Among Community-Dwelling Persons Aged 60 and Older, by 2 Definitions of Loneliness: Health and Retirement Study, United States, 2008 and 2012
| Primary Loneliness Definition |
Alternative Loneliness Definition |
|||
| Year | Lonely, % | Not Lonely, % | Lonely, % | Not Lonely, % |
| 2008 | 52.72 | 47.28 | 35.04 | 64.96 |
| 2012 | 56.63 | 43.37 | 37.08 | 62.92 |
Note. Alternative loneliness definition: individuals are categorized as lonely only if they responded “some of the time” or “often” to at least 2 of the 3 items in the scale. Primary loneliness definition: individuals are categorized as lonely if they responded “some of the time” or “often” to at least 1 of the 3 items in the scale.
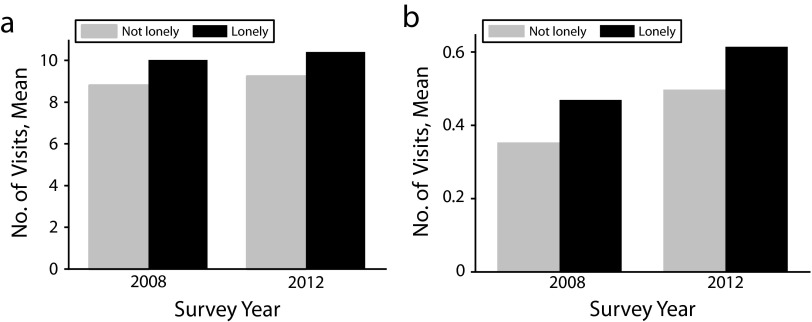
Table 2 provides sample descriptors by loneliness (lonely vs not lonely), with the primary definition of loneliness used for both years. The majority of the sample was female, with a mean age of 71 years at baseline. In both years, over half of respondents reported being lonely, 53% in 2008 and 57% in 2012. Respondents that were coded lonely in either year showed a significantly greater number of doctors’ and hospital visits (Figure 1). People who were lonely were more likely to be female, not married, and to have more health problems. Lonely respondents reported more ADL disability, had a greater numbers of depressive symptoms, were less likely to count their health as good, very good, or excellent, and reported a slightly greater average number of chronic conditions.
TABLE 2—
Characteristics of Sample of Community-Dwelling Persons Aged 60 and Older, by Loneliness: Health and Retirement Study, United States, 2008 and 2012
| 2008 |
2012 |
|||||
| Characteristic | Lonely, %, No. (%), or Mean ±SD | Not Lonely, %, No. (%), or Mean ±SD | P | Lonely, %, No. (%), or Mean ±SD | Not Lonely, %, No. (%), or Mean ±SD | P |
| No. of doctor visits (range = 0–60) | 10.02 ±10.41 | 8.80 ±8.61 | < .001 | 10.39 ±11.41 | 9.22 ±10.2 | < .001 |
| No. of hospital visits (range = 0–10) | 0.47 ±0.92 | 0.35 ±0.78 | < .001 | 0.61 ±1.21 | 0.50 ±1.1 | < .001 |
| Female | 61.52 | 56.60 | < .001 | 63.38 | 53.75 | < .001 |
| Age (range = 60–100) | 71.19 ±7.14 | 71.24 ±6.72 | .82 | 75.50 ±7.18 | 74.85 ±6.6 | < .001 |
| Married | 55.21 | 74.53 | < .001 | 48.42 | 71.56 | < .001 |
| Race/ethnicity | ||||||
| Hispanic | 6.77 | 6.47 | .72 | 5.9 | 7.57 | .05 |
| Non-Hispanic White | 79.95 | 84.12 | < .001 | 81.19 | 82.88 | .19 |
| Non-Hispanic Black | 12.03 | 8.21 | < .001 | 11.41 | 8.68 | .01 |
| Non-Hispanic other | 1.24 | 1.19 | .92 | 1.5 | 0.85 | .08 |
| Education | ||||||
| No formal degree | 20.58 | 15.51 | < .001 | 20.5 | 15.15 | < .001 |
| High school or GED | 57.06 | 55.36 | .31 | 56.38 | 56.11 | .87 |
| > high school | 22.35 | 29.11 | < .001 | 23.11 | 28.74 | < .001 |
| Satisfied with income | 80.08 | 91.77 | < .001 | 82.54 | 91.26 | < .001 |
| Insured | 97.95 | 98.38 | .35 | 98.7 | 98.82 | .74 |
| No. of ADL disabilities (range = 0–6) | 0.36 ±0.94 | 0.14 ±0.57 | < .001 | 0.51 ±1.17 | 0.25 ±0.81 | < .001 |
| No. of depressive symptoms (range = 0–8) | 1.6 ±2.06 | 0.59 ±1.10 | < .001 | 1.67 ±2.01 | 0.65 ±1.17 | < .001 |
| Self-rated good, very good, or excellent health | 70.75 | 83.63 | < .001 | 68.27 | 80.64 | < .001 |
| No. of chronic conditions (range = 0–7) | 2.23 ±1.27 | 2.02 ±1.25 | < .001 | 2.54 ±1.31 | 2.28 ±1.26 | < .001 |
| Sample | 1861 (53) | 1669 (47) | 1999 (57) | 1531 (43) | ||
Note. ADL = activity of daily living; GED = graduate equivalency diploma. Some variables have missing values, and the sample (number of respondents) for these may be smaller than the full sample.
FIGURE 1—
Number of visits, by year and loneliness status, to (a) the doctor and (b) the hospital: Health and Retirement Study, United States, 2008 and 2012.
Table 3 shows the results from the panel negative binomial regression analysis predicting the outcome of doctor visits. Loneliness was statistically significant and positively associated with the number of doctor visits only for persons lonely at both time points (b = 0.075, SE = 0.034), compared with persons not lonely at either time point. For persons reporting loneliness only in 2008 or only in 2012, there was no statistically significant relationship between loneliness and doctor visits. The significant effect of chronic loneliness (lonely at both time points) remained even after we controlled for sociodemographic variables, subjective and objective health measures, depressive symptoms, insurance status, financial situation, and time dummy variable. Results also indicated that depressive symptoms, being married, having higher ADL disability, having a higher number of chronic conditions, and being better educated (having at least a high school diploma) were also significantly and positively associated with the number of doctor visits, whereas being Hispanic and having good health conditions were negatively and significantly associated with doctor visits.
TABLE 3—
Results of Panel Negative Binomial Regression, With Outcome Variable the Number of Doctor Visits Among Community-Dwelling Persons Aged 60 and Older: Health and Retirement Study, United States, 2008 and 2012
| Variable | β (Bootstrap SE) | z Statistic | P |
| Years lonely | |||
| Both years | 0.075 (0.034) | 2.19 | .029 |
| Only 2008 | 0.063 (0.051) | 1.24 | .215 |
| Only 2012 | 0.015 (0.036) | 0.41 | .683 |
| High depressive symptoms | 0.100 (0.040) | 2.48 | .013 |
| Insured | 0.501 (0.144) | 3.49 | < .001 |
| ADL disabilities | 0.058 (0.015) | 3.94 | < .001 |
| No. of chronic conditions | 0.183 (0.012) | 15.59 | < .001 |
| Good health | −0.273 (0.034) | −8.06 | < .001 |
| Married | 0.098 (0.035) | 2.83 | .005 |
| Age | 0.002 (0.002) | 0.75 | .452 |
| Female | 0.025 (0.026) | 0.97 | .334 |
| Race/ethnicity | |||
| Hispanic | −0.206 (0.067) | −3.08 | .002 |
| Non-Hispanic Black | −0.028 (0.060) | −0.46 | .646 |
| Non-Hispanic other | −0.099 (0.133) | −0.75 | .455 |
| High school graduate | 0.166 (0.033) | 4.98 | < .001 |
| Satisfied with income | −0.039 (0.042) | −0.94 | .345 |
| Questionnaire, year 2008 | 0.040 (0.029) | 1.40 | .162 |
| Constant | 1.125 (0.241) | 4.66 | < .001 |
Note. ADL = activity of daily living. Number of observations = 6377. Wald χ2 = 874.96.
Table 4 presents the results from the panel negative binomial regression model, using the primary definition of loneliness whereby hospitalization was the outcome variable. Neither chronic loneliness (lonely in both years) nor being lonely only in 2012 was statistically significantly associated with hospitalizations, although being lonely only in 2008 was statistically significant and positively associated with hospitalizations. Logistic regressions (not shown here; available upon request) that examined any hospitalizations (vs none) provided the same nonsignificant results for the loneliness variables.
TABLE 4—
Results of Panel Negative Binomial Regression, With Outcome Variable the Number of Hospitalizations Among Community-Dwelling Persons Aged 60 Years and Older: Health and Retirement Study, United States, 2008 and 2012
| Variable | β (Bootstrap SE) | z Statistic | P |
| Years lonely | |||
| Both years | 0.048 (0.060) | 0.80 | .423 |
| Only 2008 | 0.218 (0.101) | 2.15 | .031 |
| Only 2012 | 0.136 (0.080) | 1.70 | .09 |
| High depressive symptoms | 0.065 (0.061) | 1.08 | .282 |
| Insured | 0.806 (0.389) | 2.07 | .038 |
| ADL disabilities | 0.160 (0.022) | 7.13 | < .001 |
| No. of chronic conditions | 0.332 (0.023) | 14.50 | < .001 |
| Good health | −0.581 (0.059) | −9.86 | < .001 |
| Married | 0.011 (0.057) | 0.19 | .846 |
| Age | 0.014 (0.004) | 3.67 | < .001 |
| Female | −0.146 (0.055) | −2.65 | .008 |
| Race/ethnicity | |||
| Hispanic | −0.385 (0.128) | −3.01 | .003 |
| Non-Hispanic Black | −0.267 (0.088) | −3.04 | .002 |
| Non-Hispanic other | −0.392 (0.296) | −1.32 | .187 |
| High school graduate | 0.025 (0.069) | 0.36 | .721 |
| Satisfied with income | −0.015 (0.075) | −0.20 | .84 |
| Questionnaire, year 2008 | −0.083 (0.048) | −1.73 | .083 |
| Constant | −3.081 (0.499) | −6.17 | < .001 |
Note. ADL = activity of daily living. Number of observations = 6746. Wald χ2 = 1420.69.
Table 5 presents the results from the sensitivity analyses of loneliness variables using the primary and alternative definitions of loneliness. Chronic loneliness seems to have had a positive and significant effect on doctor visits under both definitions of loneliness, whereas being lonely in either 2008 or 2012 was not significant. Although being lonely only in 2008 had a significant effect on hospitalizations under the primary definition of loneliness, it was not significant under the alternative (stricter) definition of loneliness. However, chronic loneliness and being lonely only in 2012 did not have any significant effects on hospitalizations under both definitions of loneliness.
TABLE 5—
Sensitivity Analysis of Loneliness Among Community-Dwelling Persons Aged 60 Years and Older, Using 2 Definitions of Loneliness: Health and Retirement Study, United States, 2008 and 2012
| No. of Doctor Visits |
No. of Hospital Visits |
|||
| Variable | Primary Loneliness Definition, β (P) | Alternative Loneliness Definition, β (P) | Primary Loneliness Definition, β (P) | Alternative Loneliness Definition, β (P) |
| Lonely in both years | 0.075 (.029) | 0.073 (.046) | 0.048 (.423) | 0.059 (.426) |
| Lonely only in 2008 | 0.063 (.215) | 0.077 (.132) | 0.218 (.031) | 0.017 (.848) |
| Lonely only in 2012 | 0.015 (.683) | 0.092 (.089) | 0.136 (.09) | 0.065 (.421) |
| Constant | 1.125 (< .001) | 1.140 (< .001) | −3.081 (< .001) | −3.037 (< .001) |
Note. Alternative loneliness definition: individuals are categorized as lonely only if they responded “some of the time” or “often” to at least 2 of the 3 items in the scale. Primary loneliness definition: individuals are categorized as lonely if they responded “some of the time” or “often” to at least 1 of the 3 items in the scale.
DISCUSSION
This study supports previous research indicating that loneliness is a significant public health issue, especially among older adults. Under 2 definitions of loneliness, we found that a sizable proportion of those aged 60 years and older in the United States report loneliness. In addition to the potential quality-of-life implications, the results from this study show that chronic loneliness contributes to a cycle of illness and health care utilization. Although loneliness at only 1 time point did not predict health care utilization under either definition, chronic loneliness (defined here as reporting loneliness both at baseline and at 4-year follow-up) was significantly associated with increased number of doctor visits.
Although we hypothesized that chronic loneliness would also affect both physician visits and hospitalization, only physician visits were significant in our sample of community-dwelling elders under both definitions. Loneliness in 2008 was significantly associated with hospitalization under the primary definition, but this effect was not significant by the alternative definition of loneliness. This is contrary to findings by Molloy et al.,20 who found that among Irish elders, loneliness was significantly associated with emergency hospitalization. However, they did not find a significant link to planned inpatient hospital admissions.
Previous research has shown that loneliness is significantly linked with morbidity, which may explain some of the increase in physician visits found in the models. However, we controlled for a number of illnesses, as well as a global measure of subjective health, and chronic loneliness persisted as a significant predictor of physician visits. This suggests that there are other explanations for the link between loneliness and doctor visits.
We posit that for many, the doctor–patient relationship is one that provides social support rather than solely medical treatment, and that lonely elders seek social contact through these physician visits. This hypothesis is supported by the model that shows significantly increased use of physician services rather than hospitalizations. Generally, primary care physician appointments can be made and covered by insurance without prior diagnosis or referral, whereas hospitalization is only upon admittance by a physician. It is also possible that patients develop a more social relationship with a physician they are likely to see multiple times rather than with hospital staff, whose presence may be unpredictable.
This possible explanation is supported by research finding that socially isolated people may seek physician visits not for medical reasons but to meet their need for interaction and interpersonal stimulation. Recent survey data gathered by the Campaign to End Loneliness25 in the United Kingdom confirms this from a physician’s perspective. Three quarters of surveyed family doctors estimated that between 1 and 5 patients a day visited their practice primarily because they were lonely. The campaign estimated that as many as 1 in 10 patients visiting their family doctors in the United Kingdom were there not because of a medical need but because they were lonely.25
Limitations
Although use of the large sample of elders completing the HRS leave-behind questionnaire allowed us to gather self-reported data on a subjective variable, there are some limitations that should be considered when interpreting the findings. The LB questionnaires were returned only by a subset of the HRS respondents, and not all respondents completed all items on the scale for each wave. Therefore, the results may not be generalizable to the entire older population. Additionally, the self-report nature of the survey covering a 2-year time span exposes the outcome variables of health care utilization to recall bias. Although self-reported health care utilization has been applied in previous research using HRS data,26 some research has found that asking about health care utilization across long time spans likely results in bias toward underreporting at higher numbers of visits.27–29 Because data suggest that the tendency to underreport does not vary by demographics or health status,30 we do not have reason to think that any bias in reporting in our sample varied systematically by loneliness. However, there is no specific way to test this assumption, and results should be interpreted with caution. Additionally, to determine whether the respondent was lonely, we dichotomized loneliness from a 3-item scale. We based this on previous research,7 and it facilitated interpretation of the results. The collapsing of scale data, however, leads to loss of nuance. Finally, the HRS question in this study did not tease apart the type of hospitalization or reason for physician visits, and therefore we are not able to determine detailed health care outcomes. Because some researchers20 found a difference in the type of hospitalization examined, further investigation with more detailed outcomes of health care utilization is warranted.
Implications
Although public health and public policy officials place high priority on smoking, diet, and physical activity, less attention has been paid to social engagement factors such as loneliness.5 However, identifying a vulnerable group such as lonely elders can aid in early interventions, which could potentially decrease some health care utilization. In a time of limited resources, interventions that reduce high-cost health care needs are a priority.
The types of public health interventions can vary in scope and cost, ranging from increasing social support through community activities, organizing buddy programs, increasing transportation options for homebound elders, increasing social groups targeting older adults, and changing the built environment to encourage social interaction. On the basis of our data, it may also be worthwhile to consider requiring insurance companies to reimburse physicians for tending to the social as well as medical needs of patients.
Although studies proving the effectiveness of interventions are rare, one European randomized control trial showed the effectiveness of group interventions on health care utilization.31 Researchers found that their intervention, which included art and group therapy, provided significant improvements in subjective health and lowered health care costs by an estimated 943 euros per person per year,31 which exceeded the total cost of the intervention. Although specific interventions will vary by community, these results suggest that group therapy interventions can not only improve quality of life but also decrease health care utilization and costs. No study to date has examined the impact of a loneliness intervention on health care costs in the United States.
According to US census estimates, the population aged 65 years and older will increase from 35 million in 2000 to 72 million in 2030,32 when it will constitute nearly 20% of the total US population. With such a dramatic projected increase in the number of older Americans, identifying and intervening among those who are lonely should be a public health priority. Some researchers7 have suggested that loneliness may be more treatable than other determinants of functional decline among elders, such as chronic conditions. Currently, however, health care workers are not trained to consider loneliness as a coexisting issue along with other illness or complaints. Our research suggests that those that are chronically lonely are likely to turn to physicians for social contact, and health care workers should be aware of, and take into consideration, loneliness as a factor when seeing patients in their practice.
Human Participant Protection
This study has been exempted by the University of Georgia institutional review board because data were obtained from publicly available secondary data sources.
References
- 1.Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seeman T. How do others get under our skin? Social relationships and health. In: Ryff CD, Singe BH, editors. Emotion, Social Relationships, and Health. New York, NY: Oxford University Press; 2001. pp. 189–209. [Google Scholar]
- 3.Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci U S A. 2013;110(15):5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 5.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peplau LA, Perlman D. Perspectives on loneliness. In: Peblau LA, Perlman D, editors. Loneliness: A Sourcebook of Current Theory, Research and Therapy. New York, NY: Wiley; 1982. pp. 1–18. [Google Scholar]
- 7.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172(14):1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dykstra PA. Older adult loneliness: myths and realities. Eur J Ageing. 2009;6(2):91–100. doi: 10.1007/s10433-009-0110-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25(1):132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knox SS, Uvnas-Moberg K. Social isolation and cardiovascular disease: an atherosclerotic pathway? Psychoneuroendocrinology. 1998;23(8):877–890. doi: 10.1016/s0306-4530(98)00061-4. [DOI] [PubMed] [Google Scholar]
- 11.Lund R, Nilsson CJ, Avlund K. Can the higher risk of disability onset among older people who live alone be alleviated by strong social relations? A longitudinal study of non-disabled men and women. Age Ageing. 2010;39(3):319–326. doi: 10.1093/ageing/afq020. [DOI] [PubMed] [Google Scholar]
- 12.James BD, Wilson RS, Barnes LL, Bennett DA. Late-life social activity and cognitive decline in old age. J Int Neuropsychol Soc. 2011;17(6):998–1005. doi: 10.1017/S1355617711000531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21(1):140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- 14.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 2005;83(4):1–28. [PubMed] [Google Scholar]
- 15.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 16.Barsky AJ. Hidden reasons some patients visit doctors. Ann Intern Med. 1981;94(4 pt 1):492–498. doi: 10.7326/0003-4819-94-4-492. [DOI] [PubMed] [Google Scholar]
- 17.Ellaway A, Wood S, Macintyre S. Someone to talk to? The role of loneliness as a factor in the frequency of GP consultations. Br J Gen Pract. 1999;49(442):363–367. [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng S-T. Loneliness-distress and physician utilization in well-elderly females. J Community Psychol. 1992;20(1):43–56. [Google Scholar]
- 19.Taube E, Kristensson J, Sandberg M, Midlov P, Jakobsson U. Loneliness and health care consumption among older people. Scand J Caring Sci. 2014 doi: 10.1111/scs.12147. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Molloy GJ, McGee HM, O’Neill D, Conroy RM. Loneliness and emergency and planned hospitalizations in a community sample of older adults. J Am Geriatr Soc. 2010;58(8):1538–1541. doi: 10.1111/j.1532-5415.2010.02960.x. [DOI] [PubMed] [Google Scholar]
- 21.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Theeke LA. Predictors of loneliness in US adults over age sixty-five. Arch Psychiatr Nurs. 2009;23(5):387–396. doi: 10.1016/j.apnu.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The Index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 24.Cameron AC, Trivedi PK. Microeconometrics Using Stata. Revised ed. College Station, TX: Stata Press Publication; 2010. [Google Scholar]
- 25.Neill-Hall J. Family doctors ill-equipped for loneliness epidemic. Campaign to End Loneliness, 2013. Available at: http://www.campaigntoendloneliness.org/wp-content/uploads/downloads/2013/11/FINAL-GP-Polling-PR-15.11.13.pdf. Accessed June 13, 2014.
- 26.Manski RJ, Moeller JF, Chen H, Schimmel J, St Clair PA, Pepper JV. Patterns of older Americans’ health care utilization over time. Am J Public Health. 2013;103(7):1314–1324. doi: 10.2105/AJPH.2012.301124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wallihan DB, Stump TE, Callahan CM. Accuracy of self-reported health services use and patterns of care among urban older adults. Med Care. 1999;37(7):662–670. doi: 10.1097/00005650-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Norrish A, North D, Kirkman P, Jackson R. Validity of self-reported hospital admission in a prospective study. Am J Epidemiol. 1994;140(10):938–942. doi: 10.1093/oxfordjournals.aje.a117182. [DOI] [PubMed] [Google Scholar]
- 29.Roberts RO, Bergstralh EJ, Schmidt L, Jacobsen SJ. Comparison of self-reported and medical record health care utilization measures. J Clin Epidemiol. 1996;49(9):989–995. doi: 10.1016/0895-4356(96)00143-6. [DOI] [PubMed] [Google Scholar]
- 30.Ritter PL, Stewart AL, Kaymaz H, Sobel DS, Block DA, Lorig KR. Self-reports of health care utilization compared to provider records. J Clin Epidemiol. 2001;54(2):136–141. doi: 10.1016/s0895-4356(00)00261-4. [DOI] [PubMed] [Google Scholar]
- 31.Pitkala KH, Routasalo P, Kautiainen H, Tilvis RS. Effects of psychosocial group rehabilitation on health, use of health care services, and mortality of older persons suffering from loneliness: a randomized, controlled trial. J Gerontol A Biol Sci Med Sci. 2009;64(7):792–800. doi: 10.1093/gerona/glp011. [DOI] [PubMed] [Google Scholar]
- 32.Older Americans 2012: Key Indicators of Well-Being. Washington, DC: Federal Interagency Forum on Aging-Related Statistics; 2012. [Google Scholar]