Abstract
We formulated a conceptual framework that begins to answer the national call to improve health care access, delivery, and quality by explaining the processes through which community health workers (CHWs) facilitate patients’ adoption of healthy behaviors. In September 2011 to January 2012, we conducted a qualitative study that triangulated multiple data sources: 26 in-depth interviews, training documents, and patient charts. CHWs served as partners in health to immigrant Filipinos with hypertension, leveraging their cultural congruence with intervention participants, employing interpersonal communication techniques to build trust and rapport, providing social support, and assisting with health behavior change. To drive the field forward, this work can be expanded with framework testing that may influence future CHW training and interventions.
Community health workers (CHWs) are laypeople from within the communities where they work, who share common characteristics with their patients (e.g., ethnicity, culture, race, and language).1–4 CHWs have demonstrated effectiveness in an array of conditions, ranging from maternal and child health to chronic disease management.4–12 A systematic review of randomized controlled trials on CHW effectiveness determined that CHWs address health issues among various ethnic and racial groups, help improve use of early intervention services for children at risk for developmental delay, improve screening for breast and cervical cancer, and aid in improving dietary behaviors and blood pressure control.10
CHWs have specific training in providing basic nutrition and health promotion services; they aim to improve health care access through a set of core skills,13,14 advocacy, outreach, and education.2,15,16 They function in multiple roles: bridging communication between patients and providers, providing health education and counseling, and monitoring health status.7,12 Thus, CHWs have a tremendous potential to influence and improve health outcomes.
Although CHWs play integral roles in supporting patients’ individual health behaviors,17–23 the processes through which they are influential are poorly understood.21 Increasing use of this model in the United States, and recommendations in the Patient Protection and Affordable Care Act to integrate CHWs as part of health care teams,24 underscore the need to advance the knowledge base surrounding CHWs and to better understand mechanisms of this role. We developed a conceptual framework to explicate the processes through which CHWs facilitate the adoption of healthy behaviors among their patients.
PROPOSED MECHANISMS OF COMMUNITY HEALTH WORKER INFLUENCE
Suggested mechanisms underlying CHWs’ roles include empowerment, language concordance, peer modeling, cultural congruence, and trusting relationships between CHWs and patients.25–28 As experience-based experts,29,30 CHWs may appropriately support patients in moving toward improved health. CHWs’ intimate knowledge of their communities,26–28,31 and patients’ perceptions that they share a similar culture and values with their CHWs, promote trust and rapport, which in turn foster therapeutic relationships and lead to plans of care that are acceptable to patients.18,19,21,32 This cultural leverage is part of an interpersonal process consisting of (1) effective communication, (2) patient involvement in decision-making, and (3) providers’ positive and supportive interpersonal style, which characterizes high-quality health care.33
Recent work highlights the influence of provider–patient interpersonal communication processes on health outcomes.34 In particular, the current emphasis on patient-centered care is underscored by a shared power dynamic.33,35–37 The health communications literature explicates how shared power encourages a relational approach to health interactions,34 which in turn is associated with greater patient satisfaction, adherence, and more open discussion.38,39 Relational communication approaches include sharing power and decision-making, recognizing participants’ emotional needs, and demonstrating empathy, respect, and caring.40–42 Although the bulk of this work focuses on physician–patient interactions, further examination of interpersonal communication constructs may provide insight into effective strategies for optimizing health encounters with other providers, such as CHWs.
As a case study example, we qualitatively explored the role of CHWs in influencing hypertension-related behaviors among Filipino Americans in New York City. Hypertension is a significant risk factor for coronary artery disease, a leading cause of morbidity and mortality for Asian Americans.43,44 Compared with other Asian American ethnic groups, Filipino Americans have a high prevalence of coronary artery disease risk factors, such as hypertension,45–48 overweight and obesity,49,50 physical inactivity,51 metabolic syndrome,52 poor dietary patterns,53,54 and type 2 diabetes mellitus (for which their risk is also higher than among White Americans).53–59 The preponderance of these risk factors among Filipino Americans highlights the need to improve related health behaviors, and employing CHWs may be a suitable strategy.
Project AsPIRE (Asian American Partnerships in Research and Empowerment), a CHW intervention focused on improving hypertension-related outcomes (blood pressure control and reduction, appointment keeping, and medication adherence) addresses the cardiac health needs of Filipino immigrants with hypertension in New York City.60 The pilot intervention consisted of 4 monthly 90-minute group workshops delivered by CHWs. These sessions were held at the community collaborator’s office, community centers, local libraries, and apartment buildings. Between sessions, CHWs met individually with participants once a month and made 2 monthly phone calls. We conducted a qualitative study with a subset of AsPIRE pilot study participants.
METHODS
Methods for grounded theory guided the exploration of the processes through which CHWs influence the adoption of healthy behaviors. Because the design of Project AsPIRE drew from social cognitive theory and social support theory, a secondary aim examined the influence of their theoretical constructs (e.g., empowerment, self-efficacy, motivation, social modeling, skill building) and social support in these processes. All AsPIRE pilot participants, CHWs, and trainers were eligible to participate. The sampling frame (n = 113) consisted of 96 intervention participants, 4 CHWs, and 13 CHW trainers. Potential interviewees received 2 recruitment letters and up to 4 follow-up phone calls. We offered all 96 pilot study participants a $20 cash incentive to be interviewed. Of these participants, 78 did not respond, 1 refused to participate, and 4 cancelled interviews without rescheduling. One CHW declined to participate, and 3 trainers were unable to participate. We triangulated multiple data sources—patient records, CHW progress notes, CHW training material, and individual interviews (n = 26) with pilot study participants (n = 13), CHWs (n = 3), and CHW trainers (n = 10). In the parent study, 44% completed the intervention, 20% were partial completers, and the remainder dropped out. All but 1 of our qualitative study participants completed the pilot intervention.
Data
We collected basic demographic information from intervention participants and CHWs but not from CHW trainers, because our focus was CHW–patient interactions. We conducted quantitative analyses with SPSS version 22.0 (IBM, Armonk, NY). We analyzed descriptive statistics for sociodemographic variables to characterize the qualitative sample and determine how well they represented the pilot study population. We performed the independent sample t test to compare mean values for continuous measures and the χ2 test for categorical variables; in cases where minimum cell counts were less than 5, we performed the Fisher exact test. Significance was set at P = .05. We collected primary outcome data (blood pressure control and reduction, appointment keeping, and Hill–Bone compliance scale) from the pilot study60 and acculturation and social support data from the larger AsPIRE data set. Participants provided written, informed consent.
We conducted interviews from September 2011 to January 2012, an average of 14 months after the pilot study ended. A bilingual investigator conducted interviews in English (or Tagalog, as requested) with an in-depth, semistructured interview guide. Interviews explored CHWs’, trainers’, and pilot study participants’ views on CHWs’ roles in facilitating behavior change. Data collection and analysis were simultaneous. We digitally recorded all interviews. The interviewer integrated observations of nonverbal communication and reflective thoughts with the interview data. Interview data were professionally transcribed. Data saturation occurred at 26 participants, satisfying recommendations for sample sizes of 10 to 60 participants with grounded theory.61,62
Analysis
Analysis began with a preliminary reading of transcripts to obtain a general overview. Two established theories guiding the original intervention—Bandura’s social cognitive theory63 and House’s taxonomy of social support64—served as contextual referents for CHWs’ activities and gave us a provisional start list of 9 a priori codes derived from the literature.65 The preliminary coding list served as a structural tool, but we did not limit the analysis to a particular set of codes. We revised the codes (expanded and condensed) as we compared them with the raw data throughout the coding process and inductively generated additional codes to identify patterns in the data. Focused coding followed and finally identification of major themes. Coding involved constant comparison methods to identify similarities and differences in the data and to conceptually group codes.66
After finalizing a detailed codebook, a trained qualitative researcher entered these codes into qualitative analysis software, ATLAS.ti version 6.0 (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany). A research student familiar with the study independently coded a subset of 20% of the interviews to establish interrater reliability. This coding process yielded 48 initial codes, which we condensed to 32 codes and later grouped into 4 higher-level themes that informed the conceptual framework of processes underlying CHWs’ roles in facilitating the adoption of healthy behaviors. Strategies to ensure qualitative rigor involved reflective journaling, triangulating multiple data sources, keeping an audit trail, and completing member checks.
RESULTS
Our findings highlighted aspects of CHWs’ roles in facilitating intervention participants’ adoption of healthy behaviors that were most salient for participants, trainers, and CHWs themselves. These themes provided insight into the processes through which CHWs facilitate health behavior change for Filipino Americans with hypertension.
Patient and CHW characteristics are reported in Tables 1 and 2. Thirteen of the 96 eligible AsPIRE pilot study participants volunteered for our qualitative study. Pilot study outcomes are discussed in greater detail elsewhere.60 Our participants were similar to the pilot study population in most sociodemographic variables (Table 1) and had resided in the United States for about 13 years. The larger pilot population and our respondents had similar mean scores for acculturation (low) and social support (moderate). The qualitative study sample appeared to be more educated than the pilot population (84% and 66%, respectively, had a college degree or higher), but these differences were nonsignificant.
TABLE 1—
Descriptive Statistics for Qualitative Study Participants in Evaluation of Pilot Study on Role of Community Health Workers in Facilitating Adoption of Healthy Behaviors Among Immigrant Filipinos With Hypertension: Project AsPIRE, New York City, 2011–2012
| Characteristic | Qualitative Study Sample (n = 13), No. (%) or Mean ±SD | Pilot Study Sample (n = 83), No. (%) or Mean ±SD | Difference, Mean (95% CI) | Pa |
| Age, y | 55.69 ±14.27 | 55.62 ±10.98 | −0.07 (−6.89, 6.75) | .98 |
| Resided in United States, y | 12.92 ±9.86 | 12.77 ±9.63 | 0.15 (−5.60, 5.90) | .96 |
| Time since intervention completion, mo | 13.77 ±3.06 | 15.29 ±4.04 | 1.53 (−1.58, 4.63) | .33 |
| Acculturationb | 2.47 ±0.45 | 2.28 ±0.52 | −0.19 (−0.50, 0.13) | .24 |
| Social supportb | 3.46 ±0.42 | 3.50 ±0.57 | 0.04 (−0.29, 0.37) | .81 |
| Gender | .727 | |||
| Male | 2 (15.4) | 21 (25.3) | ||
| Female | 11 (84.6) | 62 (74.7) | ||
| Marital status | .317 | |||
| Married | 9 (69.2) | 47 (56.6) | ||
| Not married | 4 (30.8) | 36 (43.3) | ||
| Highest level of education | .496 | |||
| < high school | 0 | 4 (4.8) | ||
| High school | 0 | 8 (9.6) | ||
| Some college/technical | 2 (15.0) | 16 (19.3) | ||
| College degree | 9 (69.0) | 38 (45.8) | ||
| Graduate/professional degree | 2 (15.0) | 17 (20.5) | ||
| Residence | .76 | |||
| New Jersey | 5 (38.5) | 28 (33.7) | ||
| New York | 8 (61.5) | 55 (66.3) | ||
| Preferred language of communication | .739 | |||
| English | 1 (7.7) | 7 (8.9) | ||
| Tagalog | 3 (23.1) | 25 (31.6) | ||
| English, Tagalog, or both | 9 (69.2) | 38 (48.1) | ||
| Other | 0 | 8 (10.1) | ||
| Region of origin in the Philippines | .615 | |||
| Luzon | 10 (76.9) | 55 (68.8) | ||
| Visayas | 2 (15.4) | 10 (12.5) | ||
| Mindanao | 1 (7.7) | 15 (18.8) | ||
| Employment status | .578 | |||
| Full-time | 7 (53.8) | 45 (54.2) | ||
| Part-time | 2 (15.4) | 16 (19.3) | ||
| Not working | 4 (30.8) | 22 (26.5) | ||
| Type of work | .236 | |||
| Professional/managerial | 1 (7.7) | 6 (9.2) | ||
| Technical | 0 | 2 (3.1) | ||
| Administrative support | 3 (23.1) | 2 (3.1) | ||
| Service | 5 (38.4) | 41 (63.1) | ||
| Retired/unemployed other | 4 (30.8) | 14 (21.5) |
Note. CI = confidence interval.
Significance set to P < .05.
On a scale of 1–5, with 5 the greatest.
TABLE 2—
Descriptive Statistics for Community Health Workers Encouraging Healthy Behaviors Among Immigrant Filipinos With Hypertension: Project AsPIRE, New York City, 2011–2012
| Characteristic | Sample, No. (%) or Mean ±SD |
| Age, y | 43 ±18.68 |
| Resided in United States, y | 12.67 ±6.51 |
| Gender | |
| Male | 2 (66.7) |
| Female | 1 (33.3) |
| Marital status | |
| Married | 1 (33.3) |
| Not married | 2 (66.7) |
| Highest level of education | |
| < high school | 1 (33.3) |
| High school | 1 (33.3) |
| Some college/technical | 1 (33.3) |
| College degree | |
| Graduate/professional degree | 2 (66.7) |
| Residence | 1 (33.3) |
| Region of origin in the Philippines | |
| Luzon | 1 (33.3) |
| Visayas | 2 (66.7) |
| Mindanao | 0 |
In information extracted from medical records of our respondents, we observed reductions in systolic blood pressure (mean reduction from baseline to 4 months = 10.3 mmHg; P < .1) and significant improvements in the proportion of participants with controlled blood pressure (baseline = 61.5%; 4 months = 92.3%; P < .05). As in the pilot study results, tobacco and alcohol use did not significantly improve, and improvements on appointment keeping and the Hill–Bone Compliance Scale were nonsignificant.
Partners in Health
The overarching theme that grounded this framework was that CHWs and patients are partners in health (Figure 1). Respondents described CHWs as guides, friends, teachers, and confidants on their journey toward becoming healthier. In their multiple roles, CHWs functioned as part of an open system influenced by intervention participant characteristics and contextual factors.
FIGURE 1—
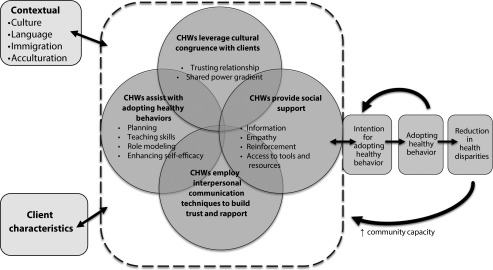
Conceptual framework of community health workers (CHWs) and patients as partners in health.
The dynamic interaction of 4 mutually reinforcing components characterized the process of CHWs facilitating healthy behaviors: (1) CHWs leveraged their cultural congruence with patients, (2) CHWs employed interpersonal communication techniques to build trust and rapport, (3) CHWs provided social support, and (4) CHWs assisted with adopting healthy behaviors. These components synergistically influenced patients’ intention to adopt healthy behaviors, which led to a reciprocal effect: successfully adopting healthy behaviors reinforced intention. Improving health behaviors could help reduce health disparities and lead to an enhanced community capacity, strengthening the CHW intervention itself.
Cultural Congruence
Cultural congruence, which included a shared set of common values, beliefs, language, and cultural identity, as well as a shared immigrant experience, aided in building trust and understanding between CHWs and patients. Cultural factors positively affected CHW–patient relations. Three subthemes represented this concept: (1) a common culture promoted participants’ comfort with CHWs (“We grew up from the same places, are familiar with the same places and territories in the Philippines, so we have a lot in common, so the trust is in there”—a CHW), (2) speaking the same language broke down barriers (“It makes me comfortable that we’re [speaking] in the same language and the same accent”—an intervention participant), and (3) CHWs and intervention participants related to each other through a shared immigrant experience (“You were talking with someone who could appreciate, maybe, what you were going through”—an intervention participant).
CHWs used their knowledge of the Filipino cultural values of pakikisama (belonging to the group), pakikipagkapwa-tao (caring for people), and hiya (shame or losing face) to influence health behaviors. CHWs considered the factors influencing intervention participants to place a lower priority on health (in particular, financial obligations to family abroad) and addressed this barrier by reorienting patients’ views on prevention and health promotion. One intervention participant’s CHW encouraged her to take an active role with her health, saying, “If you love your life, you have to do it . . . if you love your family, you have to do it.” CHWs reframed the traditional Filipino value of pakikipagkapwa-tao to include self-care and health maintenance. They encouraged patients to consider that the cultural imperative to financially provide for others should not take precedence over their own health. One respondent realized, “We are more focused on the job and sometimes forget our health . . . but you cannot work if you are not healthy anymore.”
Although most participants endorsed the intervention’s group approach, 2 respondents shared that although they positively viewed Filipino values of group centeredness, these aspects were “stifling” at times. They self-described as “conservative” and “not so fond of parties” or socializing, unlike others in their cohort. This contrasting view suggested that to appeal to the broadest variety of people, CHWs and CHW programs should anticipate such responses and offer diverse approaches to care.
A CHW described using hiya, a core Filipino value, to motivate patients to participate in self-care by being “more persistent than they [the patients] are of their own health.” He used this value as a platform to engage intervention participants in healthy behaviors: “I want them to be ashamed of themselves because of not going to the doctor. ‘If this guy [CHW] cares for me a lot, then why wouldn’t I care for myself?′” This strategy appeared to be inconsistent with CHWs’ grounding as trusted community members. All our respondents, however, held this CHW in high regard, describing him as “personable and easy to relate to,” with one noting, “When we talked with him, we talked freely . . . we were not ashamed.”
Communication Techniques
Although intervention participants recognized CHWs’ knowledge and professionalism, their down-to-earth qualities (e.g., friendliness, being respectful and nonjudgmental) were especially appealing, making them feel at ease. An equal power dynamic and mutual respect underscored this theme. These characteristics cultivated an environment for a trusting CHW–patient relationship that reduced barriers to engagement. Some CHW characteristics, though intangible, were very meaningful to intervention participants. One trainer noted that he trains CHWs from the perspective that CHWs meet patients “where they are, and [has] clients tell the CHWs where they want to go . . . and then they can work together.” Furthermore, a CHW trainer noted, “The footing might be perceived as being more equal,” leading, therefore, to a “more honest dialogue and better troubleshooting.”
Respondents believed that CHWs used respectful verbal and nonverbal communication:
The doctors don’t ask, they only prescribe. Our community health worker was very good in dealing with the warning, with the danger. We liked that. There is a diplomatic way of saying it that will be acceptable to you.
Similarly, another respondent shared that her CHW “really discussed things. She explained clearly, you know . . . in our level really like . . . no knowledge at all, medical or whatever. So we were able really to understand.” One CHW described the art of communicating with Filipinos: “You cannot just talk straight to them. You go around the bush a lot of time in order to be sensitive and for them to buy into your idea.”
Intervention participants were also motivated by CHWs’ persistence, flexibility, and encouragement. CHWs’ relationships with patients enabled them to interact in ways that meaningfully influenced the process of adopting healthy behaviors. A respondent who missed scheduled group sessions because of work conflicts described how her CHW “called up, [asking] when, when, when . . . she really went out of her way to come to our place.” This respondent appreciated her CHW’s persistence, interpreting the frequent contact and reminders as great motivators to stay on track with her own health goals:
What is special there is that [the CHW] is very much concerned. She’s very friendly. It’s like you developed a relationship. So that is how you are reminded of what you need to do. It’s not like you’re going to remember everything—you know these things already, but if you have a reminder, you become more aware again of what you’re supposed to be doing. Perhaps if she wasn’t very personalized, it would not make a difference. She really reached out—she calls, if you invite her she goes, and we sort of developed an identity for her that she is the “cholesterol girl”! She established an identity within our own group. So I think her work had an impact on us. . . . It’s still with us.
Social Support
CHWs facilitated adoption of healthy behaviors through 4 supportive actions: (1) sharing accurate information to increase patients’ health awareness, (2) offering empathy, (3) connecting patients with tools and resources for achieving change, and (4) providing feedback and advice that helped patients construct an understanding of their progress. Most importantly, CHWs considered the contextual barriers to healthy behaviors and strategized with patients to effect future change. For instance, CHWs recognized knowledge deficits, teaching patients “a lot that [they did] not know, and to understand things that [they] did not understand before, like failure to take your medication.” More pragmatically, CHWs increased exercise opportunities by purchasing jump ropes for some intervention participants and inviting individuals or small groups for walks to the park.
For new immigrants in particular, CHWs provided emotional support, offering genuine care and concern that showed intervention participants that their CHW was there to assist. Participants’ experiences were validated, and they believed that they were not alone, as one respondent reflected, “He became not only a friend, but a part of our family—someone like a brother, that you can say anything [to].” By reinforcing skills, and offering encouragement, CHWs worked with patients to enhance their self-efficacy for making healthy behavior changes. One respondent told us that her CHW “encouraged changes in lifestyle, in diet, in exercise. I would probably call it a gentle push.”
Adoption of Healthy Behaviors
CHWs assisted with creating realistic and achievable plans for health behavior change, taught skills for achieving these goals, served as role models for change, and encouraged improvements in self-efficacy. The shared power dynamic, mutual respect, and empathy minimized the social distance traditionally found between providers and their patients. CHWs and patients “develop a relationship . . . and [patients] are reminded of what [they] need to do,” said one of our patient respondents. Intervention participants described “writing down goals . . . and revisiting what was happening with those goals.” They saw their CHWs as knowledgeable peers and looked to them as role models for behaviors ranging from maintaining an ideal body weight to quitting smoking. Finally, through frequent contact and feedback, CHWs enhanced participants’ self-efficacy for skills. For instance, many participants reported greater confidence with choosing appropriate food portions and selecting and preparing foods that were nutrient dense or that varied in color.
CHWs directly influenced patients’ intentions to adopt healthy behaviors. Intervention participants learned that they could take measures to improve their health status, and they incrementally approached their health goals. One respondent described CHWs’ influence as “a big impact . . . opening [our] eyes to the reality, and the rest [adopting healthy behaviors] is up to you.” CHWs supportively presented culturally competent, accurate health information and worked with patients to develop the skills and confidence required for making changes.
One outcome of the CHW role was that health disparities declined as intervention participants individually adopted healthy behaviors that mitigated risks for disease progression and transmitted their knowledge to others. Several respondents spoke of “sharing what they learned through [their CHW]” with family and friends. The contagious nature of the intervention—whereby a ripple effect occurred and individuals shared the skills and lessons learned with those in their social networks—has the potential to affect overall community health.
DISCUSSION
CHWs as patients’ partners in health surfaced as the overarching theme explaining the processes through which CHWs facilitate the adoption of healthy behaviors. We identified influential aspects of CHWs’ roles that were congruent with the literature. We expanded on these descriptions by forming an integrated conceptual framework that may lead to future testing and development of outcome measures.
Our finding that CHWs and patients identified with each other through sharing the immigrant experience aligns with other CHW studies with ethnic minority groups in North America.67–69 Newer immigrants (those in the country < 5 years) more frequently reported looking to their CHW as a role model, noting that their CHW understood the challenges of migration and was better versed in the “ways of living in the US.” CHWs’ multifaceted roles with new immigrants ranged from listening to stories to actively connecting people to support networks. CHWs’ nuanced understanding of the context of intervention participants’ lives allowed them to help participants identify goals and develop meaningful strategies.
As in previous studies,19,22,25–28,70–72 we found that shared sociocultural characteristics (e.g., culture, language, and immigrant experience) were critical in building trusting CHW–patient relationships. Hiya was an important divergent cultural theme that illustrated the bidirectionality of CHWs’ cultural approaches. Hiya underlies and regulates social behavior, resulting in positive or negative effects.73–76 Emphasizing the shame aspect of hiya, however, highlights its potential to function as a negative cultural construct that is inconsistent with the value system of CHWs. Participants described the CHW who employed hiya as respectful, diplomatic, and humorous, and they did not perceive him as intimidating. These favorable responses suggest that hiya can become a positive value when it is employed to encourage change toward healthy behaviors.
Cultural values that prioritize work over self-care were primary barriers to participation in the intervention. To influence behavioral change, CHWs reframed the value of caring for others to include self-care and health maintenance. Intervention participants’ intentions to adopt healthy behaviors were linked to realizing that preserving their health would allow them to financially support relatives abroad—a primary driver of immigration for many respondents. To support this, CHWs creatively accommodated intervention participants’ work schedules, from meeting at local coffee shops and parks to bringing information sessions into participants’ homes.
Our results align with Reinschmidt’s findings that CHWs’ sociocultural and personal characteristics contribute to patients’ confidence, comfort, and security with them.23 Strategies were implemented at the individual level (e.g., buying jump ropes for intervention participants and accompanying them for walks in the park). The wider impact of CHWs’ influence may be realized, however, by scaling up these interventions to a systemic level. For instance, Balcazar et al. employ an ecological approach to preventing cardiovascular disease among Hispanics living along the US–Mexican border.77 Their program uses CHWs and targets individual, interpersonal, organizational, community, and policy levels. Such community-based participatory research approaches may be applied to achieve “environmental restructuring”77(p2) within Filipino communities.
Intervention participants developed a repertoire of skills that enhanced their self-confidence and prepared them to adopt healthy behaviors. These skills included reading and understanding nutrition labels, interpreting the meaning of their blood pressure readings, and developing creative ways to include non–work-related physical activity in their daily routine, such as getting off the subway at an earlier stop and walking the rest of way or taking the stairs instead of the escalator or elevator. Previous work emphasized that CHWs’ value lies in “teaching how, not what”18; similarly, participants’ acquisition and incorporation of these new skills illustrated CHWs’ roles in providing anticipatory guidance. CHWs do not just prescribe change; they work with patients to ensure understanding, development of skill mastery, and increased self-efficacy.
Intervention participants individually shared information and skills learned through the program with others, and the intervention increased community capacity. Following the pilot study, the primary community partner for this project established a storefront community center space staffed by CHWs. The group has great visibility and continues to serve as a resource for addressing the health needs of the Filipino American community in New York City.
Limitations
The small sample size limits transferability of the framework to Filipino immigrants elsewhere. Participants completed the AsPIRE program an average of 14 months before the qualitative interviews. This lag time posed a potential for recall bias and may account for the low enrollment of pilot study participants into our qualitative study. Interestingly, of the 13 intervention participants interviewed, all but 1 completed the entire program. By contrast, the pilot study had a completion rate of 44%,60 indicating potential selection bias. Perhaps some predisposing characteristic among completers increased the likelihood of enrolling in our study. Nearly one third of our respondents chose professional–managerial to describe their primary area of work in the Philippines, which is not typical of most CHW program participants and may have introduced bias to the study. However, fewer than 10% of our respondents reported working in professional or managerial roles in the United States. It is not known whether the experience of immigrating and transitioning to different fields of work minimizes this bias.
Although our coding approach considered the theoretical basis of the AsPIRE program, our use of Bandura's social cognitive theory and social support theory constructs may have constrained the emergence of theory; however, we detailed the methodological strategies employed to minimize this limitation. Finally, we focused on CHWs’ individual-level impact and did not examine their roles at broader levels.
Future Research
To our knowledge, ours is the first conceptual framework that articulates the processes underlying CHWs’ roles in facilitating health behavior change. This signifies a starting point for more nuanced examinations of the mechanisms through which CHWs influence health. Future studies with larger sample sizes and diverse ethnic groups may broaden the framework’s transferability. Efforts should also focus on recruiting program dropouts. These perspectives may identify areas for program improvement and offer insight about areas for targeted CHW training.
CHWs’ interpersonal and relational communication skills enable them to reach those who infrequently access care by health professionals. In addition to further elucidating how CHWs establish connections with patients to improve health outcomes, future research should explore CHWs’ roles within interdisciplinary teams. It may be helpful to determine what combination of skills (e.g., those inherent to CHWs and delegated tasks from other health professionals) is optimal. Finally, it would be timely to augment this framework to examine CHWs’ roles beyond individual-level interactions.
The Patient Protection and Affordable Care Act presents opportunities for integrating and sustaining CHWs within new models of care delivery.78–80 CHWs can play integral roles in engaging communities in programs created by the new law and in coordinating and delivering care. CHWs may also play broader roles in addressing the shortcomings of the US health care system through ensuring quality, accessible, comprehensive care. Acknowledging the potential contributions of CHWs to systems change may lead to better approximations of their widespread impact; this challenges us to consider the ways that CHWs influence social determinants of health.
Conclusions
Our framework conceptually aligns with previous descriptions of CHWs’ roles in the United States and adds greater insight to the processes through which CHWs facilitate the adoption of healthy behaviors. Our study validates many empirical assumptions regarding CHWs’ roles and provides information on the CHW intervention with Filipino Americans, an immigrant group at risk for coronary artery disease that is traditionally underrepresented in the literature.
CHWs facilitate the adoption of healthy behaviors by leveraging their shared culture, language, and life experiences; using interpersonal communication approaches that promote trust; providing social support; and guiding patients toward behavior change. The capacity of CHWs to translate and tailor positive health behaviors and health promotion strategies in the daily and social context of their patients’ lives is essential to increasing those patients’ self-efficacy and adoption of such behaviors. As CHWs become more widely incorporated members of health care teams in the United States, our framework may be used in further work to guide and structure CHW intervention training and evaluation.
Acknowledgments
This work was supported by the National Institutes of Health (NIH) National Institute on Minority Health and Health Disparities (grants P60MD000538 and R24001786); the National Center for the Advancement of Translational Science (grant UL1 TR000038); the Centers for Disease Control and Prevention (CDC; grant U48DP001904 and grant U58DP005621); and the Sigma Theta Tau International Honor Society of Nursing, Doris Bloch Research Award.
We acknowledge D. Chyun and E. Ea for their constructive critique during the study; R. Ursua, D. Aguilar, L. Gamboa, and L. Wyatt for facilitating access to the study population; research assistants, K. Escondo, and S. Bender; and finally S. Gennaro and M. K. Hutchinson for their insightful editorial comments. The critiques provided by the 3 anonymous reviewers are greatly appreciated. We especially thank Kalusugan Coalition Project AsPIRE staff, CHWs, and community participants for their support in conducting this study.
Note. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH and CDC.
Human Participant Protection
Approval and oversight of the study was provided by New York University School of Medicine’s institutional review board.
References
- 1.American Public Health Association. Community health workers. Available at: http://www.apha.org/apha-communities/member-sections/community-health-workers. Accessed August 6, 2014. [DOI] [PubMed]
- 2.Eng E, Young R. Lay health advisors as community change agents. Fam Community Health. 1992;15(1):24–40. [Google Scholar]
- 3.Nemcek MA, Sabatier R. State of evaluation: community health workers. Public Health Nurs. 2003;20(4):260–270. doi: 10.1046/j.1525-1446.2003.20403.x. [DOI] [PubMed] [Google Scholar]
- 4.Viswanathan M, Kraschnewski J, Nishikawa B . Outcomes of Community Health Worker Interventions. Rockville, MD: Agency for Healthcare Research and Quality; 2009. Evidence Report/Technology Assessment 181. AHRQ publication 09-E014. Available at: http://www.ahrq.gov/research/findings/evidence-based-reports/comhwork-evidence-report.pdf. Accessed June 19, 2014. [Google Scholar]
- 5.American Association of Diabetes Educators. AADE position statement: community health workers in diabetes management and prevention. Diabetes Educ. 2009;35(3 suppl):48S–52S. [Google Scholar]
- 6.Andrews JO, Felton G, Wewers ME, Heath J. Use of community health workers in research with ethnic minority women. J Nurs Scholarsh. 2004;36(4):358–365. doi: 10.1111/j.1547-5069.2004.04064.x. [DOI] [PubMed] [Google Scholar]
- 7.Brownstein JN, Bone LR, Dennison CR, Hill MN, Kim MT, Levine DM. Community health workers as interventionists in the prevention and control of heart disease and stroke. Am J Prev Med. 2005;29(5 suppl 1):128–133. doi: 10.1016/j.amepre.2005.07.024. [DOI] [PubMed] [Google Scholar]
- 8.Brownstein JN, Chowdhury FM, Norris SL et al. Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med. 2007;32(5):435–447. doi: 10.1016/j.amepre.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Findley SE, Sanchez M, Mejia M et al. Effective strategies for integrating immunization promotion into community programs. Health Promot Pract. 2009;10(2 suppl):128S–137S. doi: 10.1177/1524839909331544. [DOI] [PubMed] [Google Scholar]
- 10.Gibbons MC, Tyus NC. Systematic review of U.S.-based randomized controlled trials using community health workers. Prog Community Health Partnersh. 2007;1(4):371–381. doi: 10.1353/cpr.2007.0035. [DOI] [PubMed] [Google Scholar]
- 11.Krieger JW, Takaro TK, Song L, Weaver M. The Seattle-King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–659. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Viswanathan M, Kraschnewski J, Nishikawa B et al. Outcomes and costs of community health worker interventions: a systematic review. Med Care. 2010;48(9):792–808. doi: 10.1097/MLR.0b013e3181e35b51. [DOI] [PubMed] [Google Scholar]
- 13.University of Arizona. A Summary of the National Community Health Advisor Study. Baltimore, MD: Annie E. Casey Foundation; 1998. Available at: http://crh.arizona.edu/sites/crh.arizona.edu/files/pdf/publications/CAHsummaryALL.pdf. Accessed June 4, 2014. [Google Scholar]
- 14.O’Brien MJ, Squires AP, Bixby RA, Larson SC. Role development of community health workers: an examination of selection and training processes in the intervention literature. Am J Prev Med. 2009;37(6 suppl 1):S262–S269. doi: 10.1016/j.amepre.2009.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Health Resources and Services Administration. Community Health Workers National Workforce Study. Washington, DC: US Dept of Health and Human Services; 2007. Available at: http://bhpr.hrsa.gov/healthworkforce/reports/chwstudy2007.pdf. Accessed January 5, 2014. [Google Scholar]
- 16.Ingram M, Reinschmidt KM, Schachter KA et al. Establishing a professional profile of community health workers: results from a national study of roles, activities and training. J Community Health. 2012;37(2):529–537. doi: 10.1007/s10900-011-9475-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balcazar HG, Wise S, Redelfs A et al. Perceptions of community health workers (CHWs/PS) in the U.S.-Mexico Border HEART CVD Study. Int J Environ Res Public Health. 2014;11(2):1873–1884. doi: 10.3390/ijerph110201873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis KL, O’Toole ML, Brownson CA, Llanos P, Fisher EB. Teaching how, not what: the contributions of community health workers to diabetes self-management. Diabetes Educ. 2007;33(suppl 6):208S–215S. doi: 10.1177/0145721707304133. [DOI] [PubMed] [Google Scholar]
- 19.Deitrick LM, Paxton HD, Rivera A et al. Understanding the role of the promotora in a Latino diabetes education program. Qual Health Res. 2010;20(3):386–399. doi: 10.1177/1049732309354281. [DOI] [PubMed] [Google Scholar]
- 20.Gimpel N, Marcee A, Kennedy K, Walton J, Lee S, DeHaven MJ. Patient perceptions of a community-based care coordination system. Health Promot Pract. 2010;11(2):173–181. doi: 10.1177/1524839908320360. [DOI] [PubMed] [Google Scholar]
- 21.Heisler M, Spencer M, Forman J et al. Participants’ assessments of the effects of a community health worker intervention on their diabetes self-management and interactions with healthcare providers. Am J Prev Med. 2009;37(6 suppl 1):S270–S279. doi: 10.1016/j.amepre.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCloskey J, Flenniken D. Overcoming cultural barriers to diabetes control: a qualitative study of southwestern New Mexico Hispanics. J Cult Divers. 2010;17(3):110–115. [PubMed] [Google Scholar]
- 23.Reinschmidt KM, Hunter JB, Fernández ML, Lacy-Martinez CR, Guernsey de Zapien J, Meister J. Understanding the success of promotoras in increasing chronic disease screening. J Health Care Poor Underserved. 2006;17(2):256–264. doi: 10.1353/hpu.2006.0066. [DOI] [PubMed] [Google Scholar]
- 24. Patient Protection and Affordable Care Act. Pub L No. 111–148, 124 Stat 119 (2010) HR 3590; Title V, Subtitle B. § 5101, 5102, 5313, 5403, and 3509.
- 25.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am J Prev Med. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 26.Giblin PT. Effective utilization of indigenous health care workers. Public Health Rep. 1989;104(4):361–368. [PMC free article] [PubMed] [Google Scholar]
- 27.Islam NS, Zanowiak JM, Wyatt LC et al. A randomized-controlled, pilot intervention on diabetes prevention and healthy lifestyles in the New York City Korean community. J Community Health. 2013;38(6):1030–1041. doi: 10.1007/s10900-013-9711-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Islam NS, Wyatt LC, Patel SC et al. Evaluation of a community health worker pilot intervention to improve diabetes management in Bangladeshi immigrants with type 2 diabetes in New York City. Diabetes Educ. 2013;39(4):478–493. doi: 10.1177/0145721713491438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilkey M, Garcia CC, Rush C. Professionalization and the experience-based expert: strengthening partnerships between health educators and community health workers. Health Promot Pract. 2011;12(2):178–182. doi: 10.1177/1524839910394175. [DOI] [PubMed] [Google Scholar]
- 30.Sabo S, Ingram M, Reinschmidt KM et al. Predictors and framework for fostering community advocacy as a community health worker core function to eliminate health disparities. Am J Public Health. 2013;103(7):e67–e73. doi: 10.2105/AJPH.2012.301108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Islam NS, Zanowiak JM, Wyatt LC et al. Diabetes prevention in the New York City Sikh Asian Indian community: a pilot study. Int J Environ Res Public Health. 2014;11(5):5462–5486. doi: 10.3390/ijerph110505462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kangovi S, Grande D, Carter T et al. The use of participatory action research to design a patient-centered community health worker care transitions intervention. Healthcare. 2014;2(2):136–144. doi: 10.1016/j.hjdsi.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 33.Stewart AL, Napoles-Springer A, Pérez-Stable EJ. Interpersonal processes of care in diverse populations. Milbank Q. 1999;77(3):305–339. doi: 10.1111/1468-0009.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Duggan A. Understanding interpersonal communication processes across health contexts: advances in the last decade and challenges for the next decade. J Health Commun. 2006;11(1):93–108. doi: 10.1080/10810730500461125. [DOI] [PubMed] [Google Scholar]
- 35.Dubbin LA, Chang JS, Shim JK. Cultural health capital and the interactional dynamics of patient-centered care. Soc Sci Med. 2013;93:113–120. doi: 10.1016/j.socscimed.2013.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sharf BF, Street RL., Jr The patient as a central construct: shifting the emphasis. Health Commun. 1997;9(1):1–11. [Google Scholar]
- 37.Stewart M. Towards a global definition of patient centered care: the patient should be the judge of patient centered care. BMJ. 2001;322(7284):444–445. doi: 10.1136/bmj.322.7284.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cousin G, Schmid Mast M, Roter DL, Hall JA. Concordance between physician communication style and patient attitudes predicts patient satisfaction. Patient Educ Couns. 2012;87(2):193–197. doi: 10.1016/j.pec.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 39.Janssen SM, Lagro-Janssen ALM. Physician’s gender, communication style, patient preferences and patient satisfaction in gynecology and obstetrics: a systematic review. Patient Educ Couns. 2012;89(2):221–226. doi: 10.1016/j.pec.2012.06.034. [DOI] [PubMed] [Google Scholar]
- 40.Hanyok LA, Hellmann DB, Rand C, Ziegelstein RC. Practicing patient-centered care: the questions clinically excellent physicians use to get to know their patients as individuals. Patient. 2012;5(3):141–145. doi: 10.2165/11599530-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 41.Epstein RM, Franks P, Fiscella K et al. Measuring patient-centered communication in patient–physician consultations: theoretical and practical issues. Soc Sci Med. 2005;61(7):1516–1528. doi: 10.1016/j.socscimed.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 42.Rao JK, Anderson LA, Inui TS, Frankel RM. Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med Care. 2007;45(4):340–349. doi: 10.1097/01.mlr.0000254516.04961.d5. [DOI] [PubMed] [Google Scholar]
- 43. National Center for Health Statistics. Health, United States, 2010: with special feature on death and dying. DHHS publication 2011-1232. Available at: http://www.cdc.gov/nchs/data/hus/hus10.pdf 2011. Accessed July 27, 2014.
- 44.Heron M. Deaths: leading causes for 2010. Natl Vital Stat Rep. 2013;62(6):1–96. [PubMed] [Google Scholar]
- 45.Araneta MR, Barrett-Connor E. Subclinical coronary atherosclerosis in asymptomatic Filipino and White women. Circulation. 2004;110(18):2817–2823. doi: 10.1161/01.CIR.0000146377.15057.CC. [DOI] [PubMed] [Google Scholar]
- 46.Brown DE, James GD. Physiological stress responses in Filipino-American immigrant nurses: the effects of residence time, life-style, and job strain. Psychosom Med. 2000;62(3):394–400. doi: 10.1097/00006842-200005000-00013. [DOI] [PubMed] [Google Scholar]
- 47.Ryan C, Shaw R, Pliam M et al. Coronary heart disease in Filipino and Filipino-American patients: prevalence of risk factors and outcomes of treatment. J Invasive Cardiol. 2000;12(3):134–139. [PubMed] [Google Scholar]
- 48.Wu TY, Hsieh HF, Wang J, Yao L, Oakley D. Ethnicity and cardiovascular risk factors among Asian Americans residing in Michigan. J Community Health. 2011;36(5):811–818. doi: 10.1007/s10900-011-9379-1. [DOI] [PubMed] [Google Scholar]
- 49.Ye J, Rust G, Baltrus P, Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann Epidemiol. 2009;19(10):718–723. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Narayan KMV, Aviles-Santa L, Oza-Frank R et al. Report of a National Heart, Lung, and Blood Institute Workshop: heterogeneity in cardiometabolic risk in Asian Americans in the US: opportunities for research. J Am Coll Cardiol. 2010;55(10):966–973. doi: 10.1016/j.jacc.2009.07.075. [DOI] [PubMed] [Google Scholar]
- 51.Mampilly CM, Yore MM, Maddock JE, Nigg CR, Buchner D, Heath GW. Prevalence of physical activity levels by ethnicity among adults in Hawaii, BRFSS 2001. Hawaii Med J. 2005;64(10) 270-272–273. [PubMed] [Google Scholar]
- 52.Palaniappan LP, Wong EC, Shin JJ, Fortmann SP, Lauderdale DS. Asian Americans have a greater prevalence of metabolic syndrome despite lower body mass index. Int J Obes (Lond) 2011;35(3):393–400. doi: 10.1038/ijo.2010.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Araneta MRG, Barrett-Connor E. Ethnic differences in visceral adipose tissue and type 2 diabetes: Filipino, African-American, and White women. Obes Res. 2005;13(8):1458–1465. doi: 10.1038/oby.2005.176. [DOI] [PubMed] [Google Scholar]
- 54.Magno CP, Araneta MRG, Macera CA, Anderson GW. Cardiovascular disease prevalence, associated risk factors, and plasma adiponectin levels among Filipino American women. Ethn Dis. 2008;18(4):458–463. [PubMed] [Google Scholar]
- 55.Araneta MRG, Wingard DL, Barrett-Connor E. Type 2 diabetes and metabolic syndrome in Filipina-American women: a high-risk nonobese population. Diabetes Care. 2002;25(3):494–499. doi: 10.2337/diacare.25.3.494. [DOI] [PubMed] [Google Scholar]
- 56.Araneta MRG, Barrett-Connor E. Adiponectin and ghrelin levels and body size in normoglycemic Filipino, African-American, and White women. Obesity (Silver Spring) 2007;15(10):2454–2462. doi: 10.1038/oby.2007.291. [DOI] [PubMed] [Google Scholar]
- 57.Cuasay LC, Lee ES, Orlander PP, Steffen-Batey L, Hanis CL. Prevalence and determinants of type 2 diabetes among Filipino-Americans in the Houston, Texas metropolitan statistical area. Diabetes Care. 2001;24(12):2054–2058. doi: 10.2337/diacare.24.12.2054. [DOI] [PubMed] [Google Scholar]
- 58.Gomez SL, Kelsey JL, Glaser SL, Lee MM, Sidney S. Immigration and acculturation in relation to health and health-related risk factors among specific Asian subgroups in a health maintenance organization. Am J Public Health. 2004;94(11):1977–1984. doi: 10.2105/ajph.94.11.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Javier JR, Huffman LC, Mendoza FS. Filipino child health in the United States: do health and health care disparities exist. Prev Chronic Dis. 2007;4(2):A36. [PMC free article] [PubMed] [Google Scholar]
- 60.Ursua RA, Aguilar DE, Wyatt LC et al. A community health worker intervention to improve management of hypertension among Filipino Americans in New York and New Jersey: a pilot study. Ethn Dis. 2014;24(1):67–76. [PMC free article] [PubMed] [Google Scholar]
- 61.Morse JM. Determining sample size. Qual Health Res. 2000;10(1):3–5. [Google Scholar]
- 62.Starks H, Trinidad SB. Choose your method: a comparison of phenomenology, discourse analysis, and grounded theory. Qual Health Res. 2007;17(10):1372–1380. doi: 10.1177/1049732307307031. [DOI] [PubMed] [Google Scholar]
- 63.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 64.House JS. Work Stress and Social Support. Reading, MA: Addison-Wesley; 1981. [Google Scholar]
- 65.Miles MB, Huberman AM. Qualitative Data Analysis. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 66.Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 3rd ed. Thousand Oaks, CA: Sage; 2008. [Google Scholar]
- 67.Ngo-Metzger Q, Sorkin DH, Phillips RS et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007;22(suppl 2):324–330. doi: 10.1007/s11606-007-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fowler N. Providing primary health care to immigrants and refugees: the North Hamilton experience. CMAJ. 1998;159(4):388–391. [PMC free article] [PubMed] [Google Scholar]
- 69.McElmurry BJ, Park CG, Buseh AG. The nurse-community health advocate team for urban immigrant primary health care. J Nurs Scholarsh. 2003;35(3):275. doi: 10.1111/j.1547-5069.2003.00275.x. [DOI] [PubMed] [Google Scholar]
- 70.Becker J, Kovach AC, Gronseth DL. Individual empowerment: how community health workers operationalize self-determination, self-sufficiency, and decision-making abilities of low-income mothers. J Community Psychol. 2004;32(3):327–342. [Google Scholar]
- 71.Fuller J. Challenging old notions of professionalism: how can nurses work with paraprofessional ethnic health workers? J Adv Nurs. 1995;22(3):465–472. doi: 10.1046/j.1365-2648.1995.22030465.x. [DOI] [PubMed] [Google Scholar]
- 72.Vissman AT, Eng E, Aronson RE et al. What do men who serve as lay health advisers really do?: immigrant Latino men share their experiences as Navegantes to prevent HIV. AIDS Educ Prev. 2009;21(3):220–232. doi: 10.1521/aeap.2009.21.3.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bulatao JC. Hiya. Philipp Stud. 1964;12(3):424–438. [Google Scholar]
- 74.Gong F, Gage SJL, Tacata LA. Help seeking behavior among Filipino-Americans: a cultural analysis of face and language. J Community Psychol. 2003;31(5):469–488. [Google Scholar]
- 75.Nadal K. Filipino American Psychology. New York, NY: Wiley; 2011. [Google Scholar]
- 76.Pe-Pua R, Protacio-Marcelino EA. Sikolohiyang Pilipino (Filipino psychology): a legacy of Virgilio G. Enriquez. Asian J Soc Psychol. 2000;3(1):49–71. [Google Scholar]
- 77.Balcázar H, Wise S, Rosenthal EL et al. An ecological model using promotores de salud to prevent cardiovascular disease on the US-Mexico border: the HEART Project. Prev Chronic Dis. 2012;9:110100–110109. doi: 10.5888/pcd9.110100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Balcazar H, Rosenthal EL, Brownstein JN, Rush CH, Matos S, Hernandez L. Community health workers can be a public health force for change in the United States: three actions for a new paradigm. Am J Public Health. 2011;101(12):2199–2203. doi: 10.2105/AJPH.2011.300386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Islam N, Nadkarni SK, Zahn D, Skillman M, Kwon SC, Trinh-Shevrin C. Integrating community health workers within Patient Protection and Affordable Care Act implementation. J Public Health Manag Pract. 2015;21(1):42–50. doi: 10.1097/PHH.0000000000000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rosenthal EL, Brownstein JN, Rush CH et al. Community health workers: part of the solution. Health Aff (Millwood) 2010;29(7):1338–1342. doi: 10.1377/hlthaff.2010.0081. [DOI] [PubMed] [Google Scholar]


