Abstract
Objectives. We studied if both observed and unobserved maternal health in African American women in hospitals or communities were associated with cesarean delivery of infants.
Methods. We examined the relationship between African American race and cesarean delivery among 493 433 women discharged from 255 Californian hospitals in 2010 using administrative data; we adjusted for patient comorbidities and maternal, fetal, and placental risk factors, as well as clustering of patients within hospitals.
Results. Cesarean rates were significantly higher overall for African American women than other women (unadjusted rate 36.8% vs 32.7%), as were both elective and emergency primary cesarean rates. Elevated risks persisted after risk adjustment (odds ratio generally > 1.27), but the prevalence of particular risk factors varied. Although African American women were clustered in some hospitals, the proportion of African Americans among all women delivering in a hospital was not related to its overall cesarean rate.
Conclusions. To address the higher likelihood of elective cesarean delivery, attention needs to be given to currently unmeasured patient-level health factors, to the quality of provider–physician interactions, as well as to patient preferences.
African American women are significantly more likely to have a cesarean delivery than other women. This has been documented in single-hospital studies,1–3 in large cities,4 in regional systems,5 and in large state-wide6 or national data sets.7 These findings extend from data gathered in the early 1990s6 to more recent periods, and the disparities in cesarean use show no sign of reduction.8
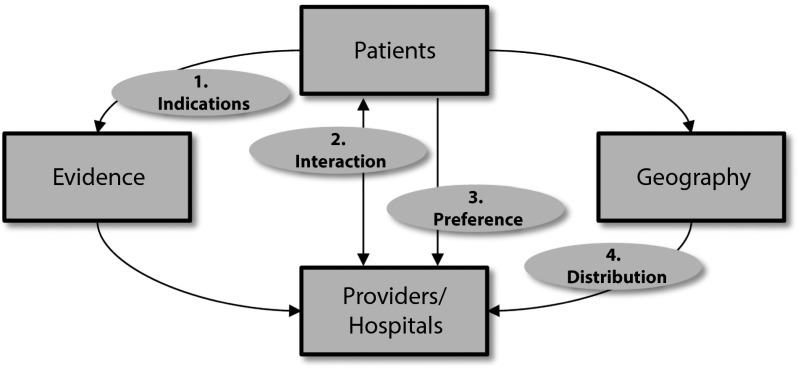
Many possible reasons could be responsible for racial disparities in care (Figure 1).9,10 First, African American women’s care may differ because of observed or unobserved cesarean indications; thus, observed differences in care reflect the evidence base. Maternal, fetal, and placental factors are associated with cesarean rates11; unobserved, unmeasured, or unrecorded indications (such as body mass index) may also vary by race and ethnicity.12 The adequacy of adjustment for preexisting indications is generally poorly understood.4 Adjustment is hampered in part by the use of administrative data that tends to omit important variables such as parity, obesity, and gestational age among many such clinically important variables.13
FIGURE 1—
Schematic diagram of potential causes of racial and ethnic disparities: California, 2010.
Note. Scheme is general and applicable to any care received by patients of any race/ethnicity and not intended to represent linear, ordered, or sequential effects. Cause 1 postulates that patients have different observed or unobserved health status and indications for treatment, and differences in observed care reflect the evidence base. Cause 2 supposes that differences in the interaction between patients and providers or hospitals leads to differences in care. Cause 3 conjectures that differences in patient preferences drive care differences. Finally, Cause 4 is based on clustering of patients of the same race within hospitals in which all patients receive a particular type of care.
Second, the care received by African American women may differ because of differences in the interaction between patients and providers or hospitals.4 In such a mechanism, African American women may face obstacles in communicating their preferences for maternity care to their providers, or those providers are less likely to act on communicated preferences. Third, patient preferences may play a role in producing observed differences in the care received by different racial/ethnic groups.4,6,14
Fourth, clustering of women by race/ethnicity within particular hospitals in which all patients receive a particular type of care may explain observed racial disparities in cesarean deliveries. Past national research documented extensive geographical and hospital-level variation in labor management and cesarean delivery.15,16 Variation in cesarean use across hospitals might be the result of financial incentives,17,18 hospital ownership type,19 labor and delivery practice patterns,20 the general nursing and organizational culture,21 or medicolegal experience.22 Such variations are thought to persist in the within-hospital environment.23
The existence and significance of clustering remains an important, unresolved question.4 One study that sought to control for patient clustering within hospitals did not demonstrate a significant impact on adjusted cesarean rates,24 and another study of military women with equitable access to the same medical care showed significantly higher cesarean risk among African American women.25
We examined hospital discharge data in 2010 in California and returned to the racial disparity in cesarean use. We rigorously tested 2 potential explanations related to observed indications for delivery mode and to geographical distribution of patients and hospitals.
To understand potential differences in indications for cesareans, we stratified all deliveries by whether the patient had a previous cesarean, which is a very well-known risk factor for a repeat cesarean. We also stratified deliveries by whether the women did or did not try to understand drivers of primary elective cesareans and primary emergency cesareans better. Prelabor primary cesareans might be an important quality measure.13 We also conducted sensitivity analyses among women at very low preexisting risk for a cesarean. Our main hypothesis was that African American women would have higher risk-adjusted rates of cesarean delivery (either elective or emergency) even without previous cesareans, suggesting either unobserved clinical risk or patient and provider factors that drive their overall cesarean risk.
To understand the role of possible patient clustering, we separately examined the relationship between the proportion of African American women among all women delivering in a hospital and the rate of cesarean delivery in that hospital. We hypothesized that hospitals with larger proportions of African American women delivering would have higher rates of cesarean delivery among all women giving birth there. That is, the observed racial difference in delivery mode was confounded by clustering of African American women in hospitals with higher cesarean rates in general.
METHODS
We obtained Californian inpatient data from the Agency for Healthcare Research and Quality for California and included all 493 433 women discharged in 2010 with diagnostic codes for an outcome of delivery or diagnostic-related group codes of vaginal or cesarean delivery. These data contained patient demographic characteristics (age, self-reported race/ethnicity, insurance status, and median zip code income as a quartile of statewide income), previous cesarean delivery, whether the focal admission was scheduled (i.e., an emergent [in labor] or nonemergent admission, although the validity and reliability of this variable were not clear), and comorbid conditions.
These data also included intrapartum processes and outcomes that, together with well-known and validated algorithms, allowed us to code for the presence of labor26 (whether obstructed, prolonged, and abnormal forces) and procedures (use of instruments, medical and surgical induction), as well as delivery and postpartum outcomes (delivery mode, obstetric trauma, length of stay, and total billed charges). The data did not contain important variables, such as parity, actual gestational age, and body mass index.
We coded for the following maternal, placental, and fetal control covariates. These included 12 well-known indications for cesarean delivery (malpresentation, antepartum hemorrhage, herpes, severe hypertension, uterine scar, multiple gestation, macrosomia, unengaged fetal head, maternal soft tissue disorder, other hypertension, preterm gestation, or fetal congenital abnormality). Thirteen maternal comorbidities believed to be associated with increased pregnancy risk were also coded (diabetes, oligohydramnios, chorioamnionitis, rhesus disease, cerebrovascular disease, intrauterine growth disorder, disease of the kidney, thyroid, heart or liver, asthma, substance abuse disorder, and mental illness).27–29 We also coded the diagnosis of a nonreassuring fetal heart rate, which has been associated with cesarean delivery, as a control covariate.
We tested baseline differences in characteristics by whether the patient was African American versus women of all other races, including unreported race, not taking ethnicity into account. We used the χ2 test to test for difference in variables with categorical values of maternal, placental, and fetal characteristics, and for labor and delivery events and outcomes. We used the nonparametric Kruskal–Wallis test to assess variables with continuous values. We tested differences in unadjusted proportions of cesarean deliveries using the t test.
We determined the multivariable-adjusted odds ratio (OR) for cesarean delivery, for African American race in a logistic regression containing all the previously described patient and admission characteristics, and hospital annual deliveries because of the possibility of a volume–outcome relationship. This pooled regression also included indicators for each hospital. SEs were robust and clustered by hospital. For regressions with emergency cesarean as a dependent variable, we added dystocia, prolonged labor, abnormal forces, and nonreassuring fetal heart rate as variables. Because the latter variable is relatively subjective and could potentially be used as an ex–post-justification for proceeding to a cesarean delivery,12,30,31 we repeated these regressions without this variable to check for robustness.
We stratified these risk-adjusted analyses (Table 1) by whether the patient had or had not had a previous cesarean delivery and by whether they had or had not labored in the current admission, thus asking several important questions.
TABLE 1—
Potential Impact of African American Race on Likelihood of Cesarean Delivery: California, 2010
| Labored or Did Not Labor | Characteristic | Did Not Labor | Labored |
| 1a: Among all women without previous cesarean, were African Americans more likely to have a primary cesarean. | No previous cesarean | 1b: Among all women without previous cesarean, were African Americans more likely to have an elective primary cesarean. | 1c: Among all women without previous cesarean who labored, were African Americans more likely to have an emergency primary cesarean |
| 2a: Among all women with previous cesarean, were African Americans more likely to have a repeat cesarean. | Previous cesarean | 2b: Among all women with previous cesarean, were African Americans more likely to have an elective repeat cesarean. | 2c: Among all women with previous cesarean who labored, were African Americans more likely to have an emergency repeat cesarean. |
Note. All women who delivered without laboring had a cesarean delivery by default. “Elective” was not synonymous with a “scheduled cesarean”: elective delivery could occur through cesarean delivery or by the induction of labor, which might result in an emergent cesarean or a vaginal delivery.
In the sensitivity analyses, we also undertook analyses of women of particularly low preexisting risk (i.e., without previous cesarean; without preexisting maternal, fetal, or placental risk factors; and without intrapartum fetal heart rate abnormalities).
In separate analyses, we calculated the proportion of total deliveries in each hospital in African American women and reported the distribution of this proportion across hospitals, as well as its bivariate association with hospital cesarean rates. Raw administrative discharge data were managed using SAS version 9.2 (SAS Institute, Cary, NC), whereas all statistical analyses of patient data were performed using STATA/SE version 12.1 (StataCorp, College Station, TX). All P values were based on 2-tailed tests with a significance of .05, and no corrections for multiple comparisons were made.32
RESULTS
Of the total 493 443 women in our sample, 33.0% had a cesarean delivery (data available as a supplement to the online version of this article at http://www.ajph.org). Of the 410 916 women without previous cesarean delivery, 11.0% were delivered by elective and 10.2% by emergency primary cesarean delivery, for a total 21.2% primary cesarean rate. The emergency primary cesarean rate among the 365 916 women without a previous cesarean who labored was 11.5%.
Of the 82 527 women with previous cesareans, 88.0% were delivered by elective and 3.8% by emergency repeat cesarean delivery for a total 91.8% repeat cesarean rate. The emergency repeat cesarean rate among 9915 laboring women was 31.8%.
In our data, 6.02% of all women reported African American race, which aligned with the birth certificate data for 2010 that showed 5.4% African American live births.33 African American women were slightly more likely to have had a previous cesarean (17.6% vs 16.7%; P < .001) and substantially less likely to labor during the current admission (73.1% vs 76.4%; P < .001), compared with others.
In terms of the questions in Table 1, but without adjusting for risk, African American women were significantly more likely to have a cesarean overall, compared with women of another race/ethnicity (36.8% vs 32.7%). They were significantly more likely to have a primary cesarean delivery (25.2% vs 20.9%), an elective primary cesarean (14.0% vs 10.8%), and if they labored, an emergency primary cesarean (13.0% vs 11.4%) compared with other women (all P < .001).
Among all women with previous cesarean deliveries, African Americans were not significantly more likely to have a repeat cesarean (91.6% vs 91.8%; P = .74), to have an elective repeat cesarean (87.4.0% vs 88.0%; P = .87), or to have an emergency repeat cesarean (32.6% vs 31.7%; P = .32) compared with women of another race/ethnicity. The overall 4.1% unadjusted excess in all cesareans among African American women appeared to be driven mostly by a higher rate of elective primary cesareans.
Table 2 shows the observed maternal, fetal, and placental characteristics so that the possible differences in risk factors that drove the elective primary procedures can be understood.
TABLE 2—
Maternal, Placental, and Fetal Characteristics of Deliveries, by Race: California, 2010
| Characteristic | African American | Other | P |
| Medi-Cal FFS, % | 22.8 | 33.3 | < .001 |
| Private MC, % | 7.4 | 16.9 | |
| Medi-Cal MC, % | 38.3 | 14.7 | |
| Private FFS, % | 1.4 | 2.8 | |
| Private HMO, % | 25.6 | 28.4 | |
| Self-pay, % | 1.5 | 1.8 | |
| Other pay, % | 2.0 | 1.8 | |
| Medicare, % | 1.1 | 0.2 | |
| Zip code income quartile,a % | < .001 | ||
| 1 | 47.1 | 28.8 | |
| 2 | 23.1 | 26.8 | |
| 3 | 18.9 | 23.6 | |
| 4 | 10.8 | 20.8 | |
| Scheduled admission, % | 21.8 | 29.4 | < .001 |
| Cesarean risk indications,b % | < .001 | ||
| 0 | 69.4 | 76.1 | |
| 1 | 22.0 | 18.4 | |
| 2 | 6.4 | 4.2 | |
| > 2 | 2.1 | 1.2 | |
| Pregnancy risk factors,b % | < .001 | ||
| 0 | 75.5 | 79.1 | |
| 1 | 20.1 | 17.9 | |
| 2 | 3.7 | 2.7 | |
| > 2 | 0.7 | 0.4 | |
| Fetal heart rate abnormality, % | 19.0 | 13.2 | < .001 |
| Hospital deliveries, median | 2695 | 3144 | .001 |
Note. FFS = fee for service; HMO = health maintenance organization; MC = managed care. Total of 493 443 women delivering in 255 Californian hospitals in 2010. P values from χ2 tests for categorical values and Kruskal-Wallis tests for continuous values. Effects are not independent and additive.
Patient zip code household income, as quartile of state values for all zip codes. Higher values correspond to more affluent zip codes.
Coded from 12 maternal, fetal, and placental indications associated with cesarean, and 13 other maternal comorbidities associated with pregnancy risk, as explained in text.
Insurance mix and local socioeconomic differences showed significant differences, and African American women were significantly more likely to deliver in a hospital with fewer annual deliveries than women of other ethnicity or race. We found substantially lower rates of scheduled admission among African American women, although the validity and reliability of this variable in obstetrical admissions was not clear. African American women (30.6%) had at least 1 of 12 known indications for cesarean, and 24.5% had at least 1 comorbidity associated with a higher risk pregnancy (vs 23.9% and 20.9%, respectively; both P < .001). Intrapartum fetal heart rate abnormalities were also diagnosed significantly more often in African American women than other women (19.0% vs 13.2%; P < .001).
In risk-adjusted regressions, we found that the previously described unadjusted relative risks were robust to risk-adjustment. Table 3 summarizes the adjusted ORs and 95% confidence intervals (CIs) for the impact of African American race on the different cesarean delivery events in the different questions explored. Estimates of the association between African American race and cesarean delivery remained significantly higher than 1 (except for emergency repeat cesarean) in well-fitting models, with R2 generally in excess of 0.28, regardless of subset and event type. Results were robust to the exclusion of fetal heart rate abnormalities as control variables (estimated OR on African American race increased because this intrapartum diagnosis is substantially more common among African Americans).
TABLE 3—
Risk-Adjusted Impact of African American Race on Likelihood of Cesarean Delivery: California, 2010
| Patient Subset and Outcome of Interest | African American Race, AOR (95% CI) |
| All without prior cesarean | |
| Primary cesarean | 1.27 (1.21, 1.33) |
| Elective primary cesarean | 1.31 (1.23, 1.39) |
| Only those who labored | |
| Emergency primary cesarean | 1.22 (1.14, 1.32) |
| All with prior cesarean | |
| Repeat cesarean | 1.23 (1.09, 1.40) |
| Elective repeat cesarean | 1.24 (1.13, 1.37) |
| Only those who labored | |
| Emergency repeat cesarean | 1.09 (0.85, 1.40) |
Note. AOR = adjusted odds ratio; CI = confidence interval. Logistic regression with robust SEs clustered on hospital, contains unreported patient demographic and maternal, fetal, and placental controls, as well as hospital delivery volume and indicators for each hospital.
Because of the large contribution to the overall excess cesarean rate that elective primary cesareans make, we separately examined the prevalence of risk factors by African American race or not in this subset of women. Table 4 shows the 11 risk factors that had both the highest impact on the event, based on size of the OR (significantly > 1.05) in the logistic regression on the event, and in which the difference in the prevalence of the risk factor between African American and other women was significant (P < .01).
TABLE 4—
Prevalence of Selected Risk Factors for Elective Primary Cesareans, by Race: California, 2010
| Prevalence of Risk Factors, % |
|||
| Risk Factor | African American | Other Race/Ethnicity | P |
| Malpresentation | 21.5 | 32.9 | < .001 |
| Macrosomia | 5.3 | 8.5 | < .001 |
| Severe hypertension | 6.4 | 5.3 | .006 |
| Unengaged fetal head | 2.8 | 3.8 | .002 |
| Maternal soft tissue disorder | 12.2 | 8.9 | < .001 |
| Herpes | 5.2 | 3.2 | < .001 |
| Preterm gestation | 20.6 | 17.4 | < .001 |
| Other hypertension | 16.3 | 10.7 | < .001 |
| Diabetes | 8.9 | 12.9 | < .001 |
| Thyroid disease | 1.8 | 3.2 | < .001 |
| Mental illness diagnosis | 5.8 | 3.6 | < .001 |
Note. P value from χ2 test for categorical values. Selected risk factors based on significant (P < .01) prevalence difference, and significant risk factor adjusted odds ratio (> 1.05; P < .01) in multivariable logistic regression on elective primary cesarean among all women without previous cesarean delivery.
Table 4 also summarizes the findings for the subset of such risk factors. In general, differences were slight, except for hypertensive diagnoses and preterm gestation, which were markedly more common, and malpresentation, which was markedly less common among African Americans. We noted that despite the essentially similar degree of risk between the 2 racial categories within this subset of women, scheduled admissions were still much more common among women of other races/ethnicity (37.8% vs 23.9%; P < .001).
Apart from these more plausibly preexisting conditions, we examined the difference in prevalence for immediately prepartum or intrapartum factors. Fetal heart rate abnormality was significantly more prevalent among African American women who had a primary elective cesarean than women of another race/ethnicity (46.1% vs 30.3%; P < .001), as were medical (8.3% vs 6.6%; P < .001) and surgical induction procedures (7.6% vs 6.4%; P < .001).
In sensitivity analyses, we examined the subset of those women at lowest risk for cesareans: no previous cesarean; no maternal, fetal, or placental indications for cesarean; no maternal comorbidities associated with higher risk pregnancy; and no intrapartum fetal heart rate abnormalities. The impact of African American race remained large and significant in analogous logistic regressions; there was an adjusted OR of 1.22 (95% CI = 1.12, 1.34) for primary cesarean delivery, an OR of 1.41 (95% CI = 1.15, 1.74) for elective primary cesarean, and an OR of 1.17 (95% CI = 1.07, 1.28) for emergency primary section among those who labored.
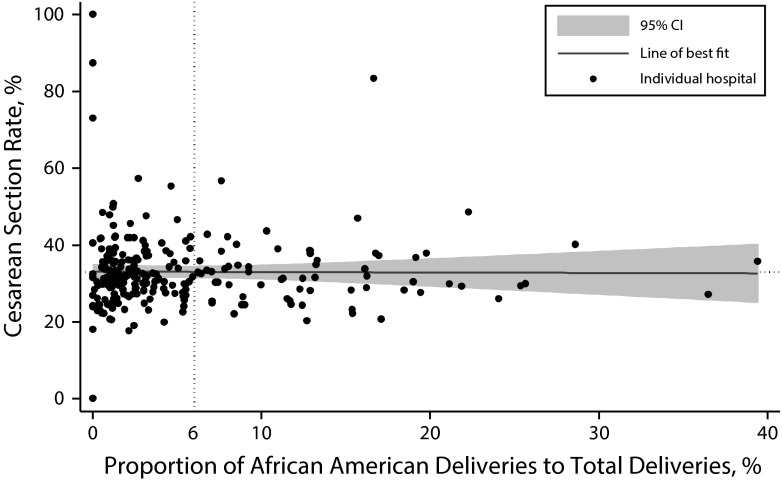
Our second research question concerned patient clustering within particular hospitals that provided a particular type of delivery care (e.g., highly interventional) to all their patients, not just their African American patients. Although the overall population proportion of African American deliveries was 6%, there were 186 hospitals whose proportion of deliveries by African American women was less than 6% of their total deliveries. Of the total of 255 hospitals, 54 hospitals had fewer than 1%, 24 hospitals had fewer than 0.5%, and 15 hospitals had no deliveries at all by African American women.
Despite this skewed distribution, we found no meaningful hospital-level association between the rate of overall cesarean deliveries in a hospital and the proportion of deliveries by African American women (Pearson correlation = −0.01; P = .92; Figure 2). In an unreported analysis, we also found no significant relationship between a hospital’s cesarean delivery rates among African American women and the proportion of deliveries by African American women (−0.03; P = .69). This absence of association persisted when we restricted analysis to only those hospitals with a lower or a higher than average proportion of African American women delivering.
FIGURE 2—
Relationship between hospital cesarean rates and hospital proportion of African American women among all women delivering in that hospital: California, 2010.
Note. Scatterplot with superimposed local regression smoothed estimate (horizontal line) and 95% confidence interval (shaded area). Each marker represents 1 of 255 hospitals. Pearson correlation = –0.01 (P = .92).
DISCUSSION
In this large retrospective Californian cohort study, our main finding is that African American women without previous cesarean were significantly more likely to deliver by primary cesarean (both by elective primary cesarean without labor, and by emergent primary cesarean after labor) than women of other race/ethnicity and that this risk drives the overall difference in cesarean delivery utilization. The data and results support the conclusion that there may be clinical reasons for this difference in primary cesarean birth. We found no significant differences for repeat cesarean birth.
Although observed indications for cesarean and pregnancy risk factors were significantly more prevalent among African Americans, there were no risk factors, except for hypertensive disorders and preterm gestation, that were both more prevalent among African Americans and strongly associated with elective primary cesareans, whereas the pronounced risk factor of malpresentation was substantially more prevalent among non-African American women. Our main hypothesis was that African American women would have higher risk-adjusted rates of cesarean delivery (either elective or emergency) even without previous cesareans, and this was confirmed.
Separately, we found that clustering of African American women in particular hospitals was pronounced. However, there was no significant relationship between the proportion of African American women among all women delivering in a hospital, and that hospital’s rate of cesarean deliveries. This made the African American risk for cesareans based on clustering less plausible and, therefore, did not support or confirm our other hypothesis that clustering of African American women occurred within hospitals where all women were more likely to receive a cesarean. Our study was nevertheless consistent with past studies and showed that African American racial disparities in cesarean use were pronounced in California. However, our work suggested that broad geographical or general hospital-specific factors were not large drivers of the variation in cesarean likelihood at the patient level.
A number of possible factors could explicate our main results and have importance for policy and practice. The most likely explanation was that both observed and unobserved clinical risk drove these results. Higher parity, lower or higher gestational age, and higher body mass index are all known to drive increased cesarean rates, yet all these factors were missing from this data set. Another strong potential explanation was unmeasured health status or social determinants of health,34,35 which might differ between patients of different races and ethnicity.
Nutrition, access to antenatal care, smoking, and previous obstetric complications were variables that were not coded in the administrative data we examined. To the extent that these unmeasured health factors were associated with different races and with cesarean delivery, they present a practical focus for data collection, for measurement of preexisting risk, and incorporation into prevention activities.
Other more speculative reasons for our findings could be that preferences differed systematically along racial/ethnic lines. For example, despite little evidence in the literature for differences in preferences among the races, it is well-known that some women have a more intervention-prone philosophy, and meeting preferences for cesareans on maternal request is accepted in the field.36
Cesareans have important negative effects for mothers37 and infants,38 but some patients might not be sufficiently well informed to know about their delivery options, or not confident enough to assert their preferences. Still others might be “present-biased,”39 discounting the well-known potential for future harm to subsequent children.40,41 Rates of cesarean delivery on maternal request were estimated as being low, in the single digits42; however, this might be a preventable cause of racial/ethnic disparities in cesarean use. Because of the current lack of data, this needs to be investigated further.
More worrying was an explanation based on poor provider–patient interaction or mistaken beliefs by a provider about some patients.43,44 Although no evidence existed for differences in such phenomena by race, anecdotal reports suggested it should not be ruled out. In this explanation, some African American women might acquiesce to a cesarean that a provider recommends for non–evidence-based reasons. Alternatively, some women might have a cesarean recommended on the basis of their physician’s misunderstanding their patient’s pain threshold, articulated preferences, etc.
Our study did not rule out such an explanation among physicians within hospitals, although it did suggest that such difficulties were not systematic across hospitals. It was not clearly known how such psychological, communication, and provider interactions differed between African American women and women of other ethnicities/races. Studies incorporating provider race as a variable are necessary to understand this cause of disparity better.
Limitations
Our study clearly had a number of important limitations. Foremost of these limitations was our use of administrative discharge data instead of clinical, chart, or registry data.45 In particular, our data had very high proportions of unknown, undeclared, unentered, or unclassified race categories (a total of 118 232 patient records). We maintained the untestable assumption that missing race categories were not differential across the different ethnicities/races. Although our aggregate results were similar to past research,1–8,11 and although the aggregate proportion of African American women in our data (6%) was similar to the birth certificate-based proportion (5.4% for 2010),33 the reliability of the race variables was not guaranteed in this data set.
A related limitation hinged on the validity of risk adjustment for cesarean delivery. Our use of well-known conditions from the specialist maternity care literature was still not a completely satisfactory approach. The lack of clinical data on indications for cesarean (for example, the lack of data on obesity or morbid obesity) and the lack of data on patient-initiated requests (for example, cesarean delivery on maternal request) made risk adjustment incomplete. It was not clear whether such risk adjustors were similarly prevalent across the different races/ethnicities.
Finally, because of the large proportion of Hispanic Americans and Latinas in California, our comparison group of non-African American women was substantially different from that in other states. Maternal preferences, and observed and unobserved health statuses might also differ systematically from those in other states, threatening external validity.
Conclusions
National rates of cesarean delivery are too high15 and should be reduced through a national agenda46 focused on measuring and monitoring quality metrics,47 and directly educating practitioners.48–51 Clinical partnerships between key payors, such as Medicaid, with a particular focus on quality improvement are an especially important piece of the puzzle.52
Despite many decades of consensus published in specialty obstetric journals and similar efforts by natural childbirth advocates, current interventions have not controlled the rise of cesareans, let alone reduced it to rates deemed more acceptable. In California, the overall cesarean rate rose by half from an initial rate of 22% in 1990,23 to 33% in our data in 2010.
Whether on maternal request,36,53,54 because of physician incentives and convenience and hospital decisions on labor and delivery management, the result of poor communication, or because of maternal health, there are clearly many opportunities to understand the causes and reduce the mean and variance of this delivery mode.42 Reducing cesareans in general while enhancing our focus on the pronounced excess of cesareans among African American women are clearly both public health imperatives.
Acknowledgments
We gratefully acknowledge funding support from the Agency for Healthcare Research and Quality (grant R21 HS21868; PI: M. H.).
Human Participant Protection
Institutional review board approval was received from the University of Southern California.
References
- 1.Ehrenthal DB, Jiang X, Strobino DM. Labor induction and the risk of a cesarean delivery among nulliparous women at term. Obstet Gynecol. 2010;116(1):35–42. doi: 10.1097/AOG.0b013e3181e10c5c. [DOI] [PubMed] [Google Scholar]
- 2.Bryant AS, Washington S, Kuppermann M, Cheng YW, Caughey AB. Quality and equality in obstetric care: racial and ethnic differences in caesarean section delivery rates. Paediatr Perinat Epidemiol. 2009;23(5):454–462. doi: 10.1111/j.1365-3016.2009.01059.x. [DOI] [PubMed] [Google Scholar]
- 3.Washington S, Caughey AB, Cheng YW, Bryant AS. Racial and ethnic differences in indication for primary cesarean delivery at term: experience at one US institution. Birth. 2012;39(2):128–134. doi: 10.1111/j.1523-536X.2012.00530.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Janevic T, Loftfield E, Savitz DA, Bradley E, Illuzzi J, Lipkind H. Disparities in cesarean delivery by ethnicity and nativity in New York City. Matern Child Health J. 2014;18(1):250–257. doi: 10.1007/s10995-013-1261-6. [DOI] [PubMed] [Google Scholar]
- 5.Getahun D, Strickland D, Lawrence JM, Fassett MJ, Koebnick C, Jacobsen SJ. Racial and ethnic disparities in the trends in primary cesarean delivery based on indications. Am J Obstet Gynecol. 2009;201(4):422.e1–422.e7. doi: 10.1016/j.ajog.2009.07.062. [DOI] [PubMed] [Google Scholar]
- 6.Braveman P, Egerter S, Edmonston F, Verdon M. Racial/ethnic differences in the likelihood of cesarean delivery, California. Am J Public Health. 1995;85(5):625–630. doi: 10.2105/ajph.85.5.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kabir AA, Pridjian G, Steinmann WC, Herrera EA, Khan MM. Racial differences in cesareans: an analysis of US 2001 national inpatient sample data. Obstet Gynecol. 2005;105(4):710–718. doi: 10.1097/01.AOG.0000154154.02581.ce. [DOI] [PubMed] [Google Scholar]
- 8.Howell EA, Zeitlin J, Hebert P, Balbierz A, Egorova N. Paradoxical trends and racial differences in obstetric quality and neonatal and maternal mortality. Obstet Gynecol. 2013;121(6):1201–1208. doi: 10.1097/AOG.0b013e3182932238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smedley BD, Stith AY. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 10. Hebert P, Ross J, Goldstein N, Howell E. Should statistical models of hospital quality include patient’s race as a covariate? Presented at: VA Equity Research Conference; September 13–14, 2010; Boston, MA.
- 11.Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huesch MD. Association between type of health insurance and elective cesarean deliveries: New Jersey, 2004–2007. Am J Public Health. 2011;101(11):e1–e7. doi: 10.2105/AJPH.2011.300333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huesch MD, Currid-Halkett E, Doctor JN. Measurement and risk adjustment of prelabor cesarean rates in a large sample of California hospitals. Am J Obstet Gynecol. 2014;210(5):443.e1–443.e17. doi: 10.1016/j.ajog.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Wagner M. Choosing caesarean section. Lancet. 2000;356(9242):1677–1680. doi: 10.1016/S0140-6736(00)03169-X. [DOI] [PubMed] [Google Scholar]
- 15.Baicker K, Buckles KS, Chandra A. Geographic variation in the appropriate use of cesarean delivery. Health Aff (Millwood) 2006;25(5):w355–w367. doi: 10.1377/hlthaff.25.w355. [DOI] [PubMed] [Google Scholar]
- 16.Kozhimannil KB, Law MR, Virnig BA. Cesarean and delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood) 2013;32(3):527–535. doi: 10.1377/hlthaff.2012.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keeler EB, Brodie M. Economic incentives in the choice between vaginal delivery and cesarean section. Milbank Q. 1993;71(3):365–404. [PubMed] [Google Scholar]
- 18.Spetz J, Smith MW, Ennis SF. Physician incentives and the timing of cesarean sections: evidence from California. Med Care. 2001;39(6):536–550. doi: 10.1097/00005650-200106000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Johnson N. For-profit hospitals performing more C-sections. California Watch. September 11, 2010. Available at: http://californiawatch.org/health-and-welfare/profit-hospitals-performing-more-c-sections-4069. Accessed April 8, 2013.
- 20.Brennan DJ, Robson MS, Murphy M, O’Herlihy C. Comparative analysis of international cesarean delivery rates using 10-group classification identifies significant variation in spontaneous labor. Am J Obstet Gynecol. 2009;201(3):308.e1–8. doi: 10.1016/j.ajog.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 21.Main E. Reducing Labor (Primary) Cesarean Section Rates. Stanford, CA: California Maternal Quality Care Collaborative; 2011. [Google Scholar]
- 22.Brown HS., III Lawsuit activity, defensive medicine, and small area variation: the case of cesarean sections revisited. Health Econ Policy Law. 2007;2(pt 3):285–296. doi: 10.1017/S1744133107004136. [DOI] [PubMed] [Google Scholar]
- 23.Main EK, Morton CH, Hopkins D, Giuliani G, Melsop K, Gould JB. Cesarean deliveries, outcomes, and opportunities for change in California: toward a public agenda for maternity care safety and quality. CMQCC White Paper 2011. Available at: https://www.cmqcc.org/resources/2079. Accessed January 1, 2015. [DOI] [PubMed]
- 24.Chung JH, Garite TJ, Kirk AM, Hollard AL, Wing DA, Lagrew DC. Intrinsic racial differences in the risk of cesarean delivery are not explained by differences in caregivers or hospital site of delivery. Am J Obstet Gynecol. 2006;194(5):1323–1328. doi: 10.1016/j.ajog.2005.11.043. [DOI] [PubMed] [Google Scholar]
- 25.Irwin DE, Savitz DA, Bowes WA, St Andre KA. Race, age, and cesarean delivery in a military population. Obstet Gynecol. 1996;88(4 pt 1):530–533. doi: 10.1016/0029-7844(96)00263-3. [DOI] [PubMed] [Google Scholar]
- 26.Gregory KD, Korst LM, Gornbein JA, Platt LD. Using administrative data to identify indications for elective primary cesarean delivery. Health Serv Res. 2002;37(5):1387–1401. doi: 10.1111/1475-6773.10762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henry OA, Gregory KD, Hobel CJ, Platt LD. Using ICD-9 codes to identify indications for primary and repeat cesarean sections: agreement with clinical records. Am J Public Health. 1995;85(8 pt 1):1143–1146. doi: 10.2105/ajph.85.8_pt_1.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gregory KD, Korst LM, Fridman M et al. Vaginal birth after cesarean: clinical risk factors associated with adverse outcome. Am J Obstet Gynecol. 2008;198(4):452.e1–452.e12. doi: 10.1016/j.ajog.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 29.Gregory KD, Korst LM. Age and racial/ethnic differences in maternal, fetal, and placental conditions in laboring patients. Am J Obstet Gynecol. 2003;188(6):1602–1606. doi: 10.1067/mob.2003.391. [DOI] [PubMed] [Google Scholar]
- 30.Minkoff H, Chervenak FA. Elective primary cesarean delivery. N Engl J Med. 2003;348(10):946–950. doi: 10.1056/NEJMsb022734. [DOI] [PubMed] [Google Scholar]
- 31.Meikle SF, Steiner CA, Zhang J, Lawrence WL. A national estimate of the elective primary cesarean delivery rate. Obstet Gynecol. 2005;105(4):751–756. doi: 10.1097/01.AOG.0000157435.67138.78. [DOI] [PubMed] [Google Scholar]
- 32.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46. [PubMed] [Google Scholar]
- 33.California Department of Public Health. Birth statistical data tables. 2010. Available at: http://www.cdph.ca.gov/data/statistics/Documents/VSC-2010-0206.pdf. Accessed May 27, 2014.
- 34.Marmot M, Wilkinson RG. Social Determinants of Health. 1999. Oxford, UK: Oxford University Press; 1999. [Google Scholar]
- 35.Wilensky GR, Satcher D. Don’t forget about the social determinants of health. Health Aff (Millwood) 2009;28(2):w194–w198. doi: 10.1377/hlthaff.28.2.w194. [DOI] [PubMed] [Google Scholar]
- 36.Ecker J. Elective cesarean delivery on maternal request. JAMA. 2013;309(18):1930–1936. doi: 10.1001/jama.2013.3982. [DOI] [PubMed] [Google Scholar]
- 37.Liu S, Liston RM, Joseph KS, Heaman M, Sauve R, Kramer MS. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. CMAJ. 2007;176(4):455–460. doi: 10.1503/cmaj.060870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gould JB, Danielson B, Korst L et al. Cesarean delivery rate and neonatal morbidity in a low-risk population. Obstet Gynecol. 2004;104(1):11–19. doi: 10.1097/01.AOG.0000127035.64602.97. [DOI] [PubMed] [Google Scholar]
- 39.Loewenstein GF, Prelec D. Preferences for sequences of outcomes. Psychol Rev. 1993;100(1):91–108. [Google Scholar]
- 40.Kennare R, Tucker G, Heard A, Chan A. Risks of adverse outcomes in the next birth after a first cesarean delivery. Obstet Gynecol. 2007;109(2 pt 1):270–276. doi: 10.1097/01.AOG.0000250469.23047.73. [DOI] [PubMed] [Google Scholar]
- 41.Gray R, Quigley M, Hockley C, Kurinczuk J, Goldacre M, Brocklehurst P. Caesarean delivery and risk of stillbirth in subsequent pregnancy: a retrospective cohort study in an English population. BJOG. 2007;114(3):264–270. doi: 10.1111/j.1471-0528.2006.01249.x. [DOI] [PubMed] [Google Scholar]
- 42.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal–Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol. 2012;120(5):1181–1193. doi: 10.1097/aog.0b013e3182704880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Balsa AI, McGuire TG. Statistical discrimination in healthcare. J Health Econ. 2001;20(6):881–907. doi: 10.1016/s0167-6296(01)00101-1. [DOI] [PubMed] [Google Scholar]
- 44.Balsa AI, McGuire TG, Meredith LS. Testing for statistical discrimination in healthcare. Health Serv Res. 2005;40(1):227–252. doi: 10.1111/j.1475-6773.2005.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gossman GL, Joesch JM, Tanfer K. Trends in maternal request cesarean delivery from 1991 to 2004. Obstet Gynecol. 2006;108(6):1506–1516. doi: 10.1097/01.AOG.0000242564.79349.b7. [DOI] [PubMed] [Google Scholar]
- 46.Main EK, Morton CH, Melsop K, Hopkins D, Giuliani G, Gould JB. Creating a public agenda for maternity safety and quality in cesarean delivery. Obstet Gynecol. 2012;120(5):1194–1198. doi: 10.1097/aog.0b013e31826fc13d. [DOI] [PubMed] [Google Scholar]
- 47.Janakiraman V, Ecker J. Quality in obstetric care: measuring what matters. Obstet Gynecol. 2010;116(3):728–732. doi: 10.1097/AOG.0b013e3181ea4d4f. [DOI] [PubMed] [Google Scholar]
- 48.Oshiro BT, Henry E, Wilson J, Branch DW, Varner MW. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113(4):804–811. doi: 10.1097/AOG.0b013e31819b5c8c. [DOI] [PubMed] [Google Scholar]
- 49.Clark SL, Frye DR, Meyers JA, Belfort MA, Dildy GA, Kofford S et al. Reduction in elective delivery at <39 weeks of gestation: comparative effectiveness of 3 approaches to change and the impact on neonatal intensive care admission and stillbirth. Am J Obstet Gynecol. 2010;203(5):449.e1–449.e6. doi: 10.1016/j.ajog.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 50.Young GJ. Multistakeholder regional collaboratives have been key drivers of public reporting, but now face challenges. Health Aff (Millwood) 2012;31(3):578–584. doi: 10.1377/hlthaff.2011.1201. [DOI] [PubMed] [Google Scholar]
- 51.Miller ES, Hahn K, Grobman WA. Consequences of a primary elective cesarean delivery across the reproductive life. Obstet Gynecol. 2013;121(4):789–797. doi: 10.1097/AOG.0b013e3182878b43. [DOI] [PubMed] [Google Scholar]
- 52.Green D, Gee RE, Conway PH. Medicare and Medicaid quality programs. Obstet Gynecol. 2013;121(4):705–708. doi: 10.1097/AOG.0b013e3182883cdc. [DOI] [PubMed] [Google Scholar]
- 53.Huesch MD, Doctor JN. Cesarean request on maternal demand. JAMA. 2013;310(9):978. doi: 10.1001/jama.2013.194756. [DOI] [PubMed] [Google Scholar]
- 54.National Institutes of Health. State-of-the-science conference statement: cesarean delivery on maternal request March 27–29, 2006. Obstet Gynecol. 2006;107(6):1386–1397. [PubMed] [Google Scholar]