Abstract
OBJECTIVE
To analyze the effects of acupressure at the SP6 point on labor duration and cesarean section rates in parturients served in a public maternity hospital.
METHODS
This controlled, randomized, double-blind, pragmatic clinical trial involved 156 participants with gestational age ≥ 37 weeks, cervical dilation ≥ 4 cm, and ≥ 2 contractions in 10 min. The women were randomly divided into an acupressure, placebo, or control group at a university hospital in an inland city in the state of Sao Paulo, Brazil, in 2013. Acupressure was applied to the SP6 point during contractions for 20 min.
RESULTS
The average labor duration was significantly different between the SP6 acupressure group [221.5 min (SD = 162.4)] versus placebo [397.9 min (SD = 265.6)] and versus control [381.9 min (SD = 358.3)] (p = 0.0047); however, the groups were similar regarding the cesarean section rates (p = 0.2526) and Apgar scores in the first minute (p = 0.9542) and the fifth minute (p = 0.7218) of life of the neonate.
CONCLUSIONS
The SP6 acupressure point proved to be a complementary measure to induce labor and may shorten the labor duration without causing adverse effects to the mother or the newborn. However, it did not affect the cesarean section rate.
Keywords: Acupressure, Complementary Therapies, Labor, Obstetric, Cesarean Section
INTRODUCTION
Historically, labor and childbirth are conducted in the home environment with the help of another woman, usually a midwife, bolstered by beliefs and empirical skills. The process of hospitalization for childbirth in the twentieth century was instrumental to the appropriation of knowledge in this area and for the development of medical knowledge, culminating in the establishment of the medicalization of the female body 17 and the dependency of women on others during childbirth.
In obstetric admissions, the use of uterotonic agents to induce labor, episiotomies, and cesarean sections have increased significantly in many countries. In the United States, 10.0%-15.0% of births occur electively (without a medical or obstetric justification) and before 39 weeks of gestation, which includes elective induction of labor and cesarean section. 6 , a Between 1996 and 2007, the number of cesarean sections increased 53.0%, reaching 32.0% of American births. b
Since 1985, the World Health Organization has recommended cesarean section rates between 5.0% and 15.0% in the general population. 21 However, these rates have increased steadily in various parts of the world. 3 In Brazil, a study conducted by the Ministry of Health found a significant increase in this rate from 32.0% in 1994 to 52.0% in 2010. c In 2014, this rate was still 52.0%, with 88.0% of the cesarean sections being performed in the private health network. d
At present, studies in obstetrics propose alternative health care strategies using noninvasive methods with the aim to recover humanized care and comfort for women during childbirth. Acupressure is a treatment based on traditional Chinese medicine and has the same principle as acupuncture: to maintain the balance of two opposing forces, the “negative” (yin) and the “positive” (yang) in the different channels that circulate throughout the body – the so-called meridians – which are linked to a target organ. 11 However, this procedure is performed without the use of needles. The stimuli are applied with hands and fingers at specific points, or in some circumstances, at combined points to achieve a greater effect in the proposed treatment. 20
Randomized controlled trials (RCT) conducted in some countries in Asia 4 , 5 , 11 , 12 and the Middle East 14 , 15 , 18 evaluated the effects of acupressure on the duration of the first stage of labor and on the mode of delivery. In these studies, three acupuncture points that are also targets for acupressure were identified: sanyinjiao (SP6), 4 , 11 , 12 , 14 , 18 hegu (LI4), 5 and zhiyin (B67). 5
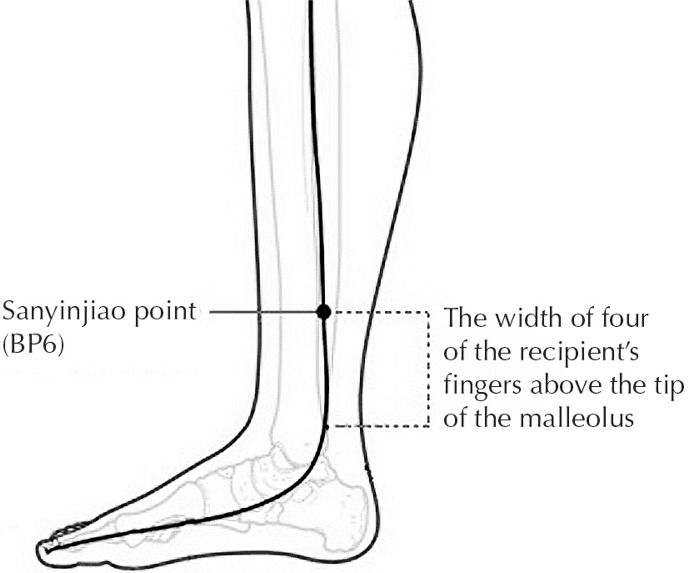
The SP6 point in particular has a strong influence on the reproductive organs, placental retention, and on dystocic and extended labor. The stimulation of this point is not indicated in preterm gestation because the concentration of yin energy can induce labor. 22 This point is located on the spleen-pancreas meridian, the width of four of the recipient’s fingers above the tip of the internal malleolus on the rear part facing the tibia (Figure 1). 21
Figure 1. Sanyinjiao point (SP6).
Although some studies have associated acupressure point SP6 with decreased labor time 11 , 12 , 14 , 18 and lower cesarean rate, 4 , 14 it was not clear whether drugs were used to induce or augment labor or whether the amniotic membranes were artificially ruptured, which are factors that influence labor duration. In addition, no studies were found on the use of this technique in the Latin American population.
The objective of this study was to analyze the effects of acupressure at the SP6 point on labor and the cesarean section rate in parturient women served in a public maternity service.
METHODS
This randomized, controlled, pragmatic clinical trial 19 was conducted between January and August 2013. The subjects were pregnant women admitted to a tertiary public teaching hospital located in an inland city in the state of Sao Paulo, Brazil, for delivery. The following women were included: any age or parity, from 37 weeks of gestation in spontaneous, induced, and/or augmented labor with dilation ≥ 4 cm, 2-3 contractions every 10 min, with undamaged skin at the bilateral SP6 points, and whose fetus was alive in cephalic vertex position with good vital signs. The following cases were excluded: pre-eclampsia, placenta previa, two or more previous cesarean sections, or immediate indication for this mode of delivery.
The sample size was estimated considering the method to calculate sample size using the unpaired t-test, 16 , 23 and pretreatment and post-treatment data from three studies were used. 8 , 14 , 18 A significance level of 5% and a test power of 80.0% were assumed, except for the studies that also showed results after 60 min. In these cases, the Bonferroni correction was applied at a significance level of 2.5%. The calculation resulted in a sample containing 51 subjects per group, the largest sample size calculated among the studies, with a total of 153 pregnant women.
Participants were allocated using a selection list of random numbers and divided into three groups: acupressure group (SP6G); touch group (TG), the placebo; and control group (CG). The study used a double-blind method; neither the pregnant women in SP6G and TG nor the professionals who provided assistance in the obstetric unit knew which group each participant belonged to. For CG, there was no possibility of using a blind method because of the nature of the study.
The questionnaires were identified with a number and the respective groups were identified with a letter, maintaining the blind structure for statistical analysis.
The parturients in SP6G received medium-intensity pressure (5-15 kg) with the index finger, with brisk and rapid decompression; the TG subjects received only superficial touch with very low-intensity pressure (approximately 100 g). 2 In both groups, contact was made at the bilateral SP6 point during contractions for a period of 20 min.
Superficial touch is a common practice that involves palpating the points and energy paths through the body but can also stimulate the energy flow. 2 To discard the placebo effect and/or the influence of palpation by the researchers, we included a control group without the simulated technique.
The parturients in CG received the standard treatment in the obstetric unit and were followed during the same period. Induction, or pharmacological or mechanical augmentation of labor, is a routine practice. Cervical preparation in pregnant women with unfavorable cervix is done using prostaglandin or a Foley catheter (a balloon introduced above the internal orifice of the cervical canal and inflated with 30 ml to 50 ml of distilled water). Induction of labor is performed when the cervix is favorable and the Bishop index is ≥ 6. In women who start cervical ripening with prostaglandin and have a good response, this medication is maintained for the first 24h or until active labor is established: dose of 25 mcg every 6h (up to the maximum dose of 100 mcg, if necessary, for 24h). In cases where labor is induced with oxytocin, the protocol e establishes intravenous infusion of 2 mIU/min and the dose is doubled every 30 min until effective labor is established.
No uterotonic agents were used to induce or augment labor as a strategy to shorten the first stage of a group in relation to the other, because these practices were performed by professionals who were not aware of the distribution of the parturient women in the study groups.
The researcher responsible for applying the acupression technique underwent 32h of training. The control and consistency of the pressure using the index fingers were ensured with a cushioned electronic child anthropometric scale until the researcher could securely maintain the pressure and consistency desired for SP6G and TG.
The pregnant women in the three groups were directed and encouraged to take slow, thoracic breaths throughout labor (inhaling and exhaling slowly and deeply) during contractions; to relax all the body musculature associated with total breathing between contractions (slow thoracoabdominal breaths in a natural rhythm). 1
For collecting sociodemographic and clinical data, a questionnaire was prepared and submitted for validation of content by five judges with experience in the area of obstetrics and/or traditional Chinese medicine. Pretesting of the questionnaire in 15 pregnant women showed that further modifications were unnecessary.
The qualitative variables were described using the mean, median, and standard deviation, and the categorical variables were described using frequency and percentages.
The quantitative variables were compared between the groups using the Kruskal-Wallis test. In cases where significant differences were found, the Mann-Whitney test for multiple comparisons was used.
For associations between the groups and the variable categories, the Chi-square test was used. In the cases where at least 20.0% of the expected values were less than five, Fisher’s exact test was applied.
For the variables where comparisons were made between the groups and measurements were made for more than one period during the evaluation, Bonferroni’s correction was used, dividing the level of significance by the number of comparisons. When the variable was measured in three periods and the groups were compared in each period, the level of significance was 1.67%. For multiple comparisons, the level of significance was also corrected using the same criterion.
This study was approved by the Research Ethics Committee of the College of Medical Sciences at the Universidade Estadual de Campinas, Campinas, state of Sao Paulo, Brazil (Register 182.421). All patients participating in the study signed a term of free and informed consent.
RESULTS
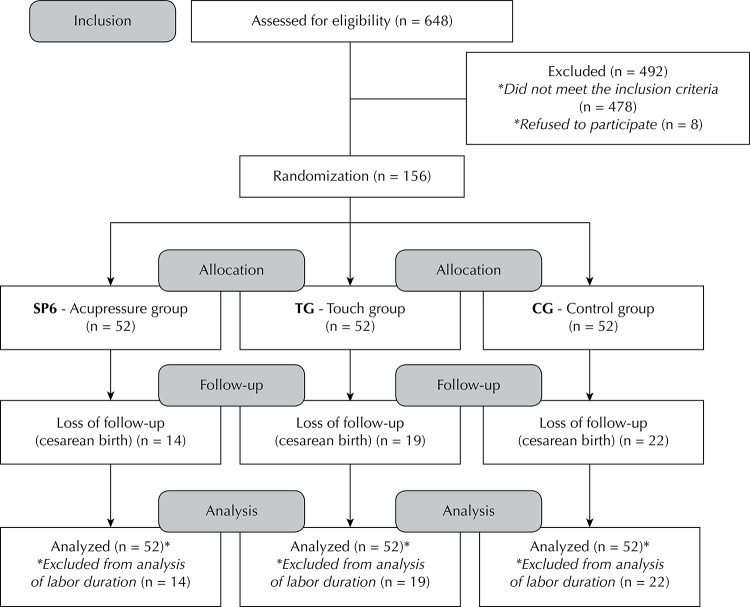
The study participants comprised 156 pregnant women equally distributed into three groups. There were no losses after randomization but the participants who had cesarean deliveries were excluded for the calculation of labor duration because of the surgical intervention during labor. Therefore, labor duration was analyzed in participants with vaginal deliveries, as described in the data collection process (Figure 2).
Figure 2. Diagram of data collection.
Table 1 shows the general characteristics of the parturients according to group location. The groups were similar with regard to age, level of education, and marital status. Most participants received education up to high school (96.0% in SP6G, 90.4% in TG, and 94.2% in CG). The remainder was still in school or had already completed higher education.
Table 1. General and obstetric characteristics among the study groups. Campinas, SP, Southeastern Brazil, 2013.
| Variable | Study group | p | ||
|---|---|---|---|---|
|
| ||||
| SP6 | Touch | Control | ||
|
| ||||
| N = 52 | N = 52 | N = 52 | ||
| Mean age in years (SD) | 26.8 (7.1) | 26.4 (6.4) | 25.2 (7.3) | 0.4567a,ⱳ |
| Education in years of study, (SD) | 9.4 (2.6) | 9.8 (2.4) | 9.6 (3.0) | 0.8954a,ⱳ |
| Marital status, n (%) | ||||
| With partner | 49 (94.2) | 50 (96.2) | 49 (94.2) | – |
| Single | 3 (5.8) | 2 (3.9) | 3 (5.8) | – |
| Mean number of pregnancies (SD) | 2.6 (1.7) | 2.3 (1.5) | 1.8 ±1.2 | 0.0232 a,ⱳ |
| Parity, n (%) | ||||
| Nulliparous | 21 (40.4) | 28 (53.9) | 29 (55.8) | 0.2319a,Ԛ |
| Multiparous | 31 (59.7) | 24 (46.2) | 23 (44.2) | |
|
| ||||
| Before treatment | ||||
|
| ||||
| Amniotic membranes, n (%) | ||||
| Intact | 26 (50.0) | 38 (73.1) | 24 (46.2) | 0.0416b,Ԛ |
| Artificial rupture | 11 (21.2) | 4 (7.7) | 9 (17.3) | |
| Spontaneous rupture | 15 (28.9) | 10 (19.2) | 19 (36.5) | |
| Mean cervical dilation (cm) (SD) | 4.9 (0.8) | 4.65 (0.9) | 4.6 (0.9) | 0.1455a,ⱳ |
| Mean number of contractions (SD) | 3.3 (1.0) | 3.19 (1.1) | 3.4 (0.9) | 0.6212c,ⱳ |
| Intensity of contractions, n (%) | ||||
| Weak | 0 (0.0) | 4 (7.7) | 2 (3.9) | 0.1693b,ʄ |
| Moderate | 25 (48.1) | 30 (57.7) | 26 (50.0) | |
| Strong | 27 (51.9) | 18 (34.6) | 24 (46.2) | |
|
| ||||
| During treatment | ||||
|
| ||||
| Mean number of contractions in 20 min (SD) | 7.02 (1.8) | 6.3 (2.0) | 7.5 (2.2) | 0.0137 c,ⱳ |
|
| ||||
| After treatment | ||||
|
| ||||
| Mean number of contractions in 60 min (SD) | 3.6 (1.1) | 3.4 (1.2) | 3.6 (1.1) | 0.4484c,ⱳ |
| Intensity of contractions, n (%) | ||||
| Weak | 2 (4.3) | 3 (6.1) | 4 (8.3) | 0.7995b,ʄ |
| Moderate | 20 (42.6) | 18 (36.7) | 15 (31.3) | |
| Strong | 25 (53.2) | 28 (57.1) | 29 (60.4) | |
| Amniotic membranes, n (%) | ||||
| Artificial rupture | 10 (19.2) | 21 (40.4) | 14 (26.9) | 0.0518b,Ԛ |
| Spontaneous rupture | 7 (13.5) | 6 (11.5) | 2 (3.9) | |
| Others (cesarean section or previous rupture) | 35 (67.3) | 25 (48.1) | 36 (69.2) | |
a p < 0.05
b p < 0.025
c p < 0.0167
ⱳ Kruskal-Wallis test
Ԛ Chi-square test
ʄ Fisher’s exact test
Values with statistical significance are shown in bold.
The obstetric characteristics shown in Table 1 indicate the homogeneity of the groups for the variables that may influence the duration of the first stage of labor. With regard to the number and intensity of contractions within 60 min of treatment, the participants whose deliveries occurred within 60 min of admission into the study were excluded.
The De Lee’s plan assessed before treatment showed no difference between the groups, and the fetal station for most of the parturients was at -3 cm, except two women in TG and two in CG, with a value of -2 cm. The number of contractions reported by the participants during treatment was different between the groups, with a higher mean for CG, particularly when compared with those in the TG. When the medians were analyzed, SP6G and CG had seven contractions each versus six contractions in the TG.
Labor duration was calculated by dividing the labor duration into three categories (Table 2). The mean labor duration (from the beginning of rhythmic and painful contractions reported by the patients until treatment) was greater in CG but had no statistical difference at the established level of significance (p < 0.0167). Nevertheless, the mean labor duration in SP6G was 176.5 min less than that in TG, and 160.4 min less than that in CG, influencing the total labor duration in the three groups.
Table 2. Differences in the duration and induction of labor among parturients with vaginal delivery. Campinas, SP, Southeastern Brazil, 2013.
| Variable | Study group | p | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| SP6 | Touch | Control | |||||
|
| |||||||
| N = 38 | N = 33 | N = 30 | |||||
| Labor duration (min) | Mean | SD | Mean | SD | Mean | SD | |
| Until treatment | 444.8 | 351.7 | 492.7 | 352.9 | 534.8 | 378.5 | 0.5750a,ⱳ |
| From treatment until delivery | 221.5 | 162.4 | 397.9 | 265.6 | 381.9 | 358.3 | 0.0047 a,ⱳ |
| Total labor duration | 628.1 | 361.1 | 891.4 | 434.8 | 913.1 | 432.6 | 0.0039 aⱳ |
| Induction of labor | n | % | n | % | n | % | |
| Cervical catheter | 3 | 7.9 | 4 | 12.1 | 5 | 16.7 | 0.5490b,ʄ |
| Prostaglandin | 7 | 18.4 | 6 | 18.2 | 6 | 20.0 | 0.9801b,Ԛ |
| Oxytocin | 23 | 60.5 | 23 | 69.7 | 12 | 40.0 | 0.0521b,Ԛ |
a p < 0.0167
b p < 0.05
ⱳ Kruskal-Wallis test
ʄ Fisher’s exact test
Ԛ Chi-square test
Values with statistical significance are shown in bold.
The Mann-Whitney test indicated that total labor duration differed statistically between SP6G and TG (p = 0.0093) and between SP6G and CG (p = 0.0041); nevertheless, the time was similar between the TG and CG groups (p = 0.8802).
Noninduction or augmentation of labor using cervical preparation with a balloon catheter or pharmaceutical agents (prostaglandin or oxytocin) was different between the groups. In general, the pregnant women included in this outcome who did not receive these interventions were: 23.7% in SP6G, 15.2% in TG, and 50.0% in CG (p = 0.0065 using the Chi-square test). However, the differences were not significant when the balloon catheter and prostaglandin were used in isolation, and were borderline when compared with oxytocin (Table 2).
The type of delivery was similar between the groups. However, the cesarean section rate was greater in CG (42.3%), especially when compared with SP6G (Table 3).
Table 3. Type of delivery and Apgar score among the groups of parturients. Campinas, SP, Southeastern Brazil, 2013.
| Variable | Study group | p | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| SP6 | Touch | Control | |||||
|
| |||||||
| N = 52 | N = 52 | N = 52 | |||||
| Type of delivery | n | % | n | % | n | % | |
| Vaginal | 38 | 73.1 | 33 | 63.5 | 30 | 57.7 | 0.2526a,Ԛ |
| Cesarean section | 14 | 26.9 | 19 | 36.6 | 22 | 42.3 | |
| Apgar scores | Mean | SD | Mean | SD | Mean | SD | |
| 1st min | 8.5 | 1.2 | 8.17 | 1.8 | 8.3 | 2.1 | 0.9542a,ⱳ |
| 5th min | 9.6 | 0.6 | 9.54 | 0.7 | 9.3 | 1.5 | 0.7218a,ⱳ |
a p < 0.05
Ԛ Chi-square test
ⱳ Kruskal-Wallis test
The mean Apgar scores, the most commonly used method to immediately assess the condition of the newborn, were not significantly different between the first and fifth minutes of life, showing that the type of treatment for each group did not alter this indicator (Table 3).
DISCUSSION
The three groups in this study were homogenous before the designated treatment for some variables that may be considered to have an influence on the duration of the first stage of labor, including parity, stated labor duration before treatment, integrity of amniotic membranes, cervical dilation, and number and intensity of contractions. However, there was a difference in the number of contractions reported by the participants during treatment, with the median of one less contraction for TG, in addition to noninduction or augmentation of labor. The need for oxytocin was greater among the parturients in the SP6G and TG; however, there was no significant difference in the induction of labor with prostaglandin or cervical preparation with a cervical catheter.
Labor duration for the parturients receiving acupressure at the SP6 point was smaller than that for the women receiving the simulated technique (TG) or the standard treatment (CG). This difference was greater when compared with TG, even though SP6G received induction or augmentation of labor with pharmaceuticals at levels equivalent to those received by the TG group. The study of the placebo effect can be disregarded when considering the use of uterotonic agents and the labor duration among the three groups.
In this study, the difference found in labor duration between the SP6G and TG was similar to that of an RCT conducted in Iran 14 and that evaluated similar groups. The parturients who received acupressure at the SP6 point for 30 min showed a mean reduction in labor duration of 189.0 min compared with that in TG, even though fewer parturients received oxytocin in SP6G (41.7% in SP6G versus 63.3% in TG, p = 0.017). 14
Similarly, two South Korean RCTs 11 , 12 showed reduced labor duration in parturients who received acupressure at the SP6 point. Another study 10 showed shorter labor time compared with participants who received standard treatment. The mean decrease in labor in SP6G considering a cervical dilation of 3 cm was 52.4, 11 52.6, 12 and 54.0 10 min. With regard to the use of oxytocin, there was no difference between the groups in an RCT, 11 although the total volume in TG was higher than that in SP6G. Other studies 10 , 12 did not report the use of oxytocin or any method to augment labor.
Two other RCTs 15 , 18 assessed the effects of acupressure on the LI4 and SP6 points compared with a third group of pregnant women without intervention; however, these trials did not clarify the use of uterotonics. A study by Salehian et al 18 showed reduced labor time in SP6 patients and LI4 patients compared with control patients (p = 0.001). Similarly, Kim et al 15 showed a 127.9 min and 149.6 min reduction in labor time for SP6 patients and LI4 patients, respectively, compared with control patients. No significant difference was observed between SP6 and LI4 patients.
The precise mechanisms by which acupressure on the SP6 point induces labor are unclear. During labor, obstruction of the meridians that cross the body is common, blocking the flow of these channels; consequently, this stimulus helps to unblock the meridians and restore equilibrium, thereby bringing relief to the women in labor. 7 Acupressure may also stimulate oxytocin release from the pituitary gland, which in turn regulates uterine contractions to improve the progress of labor. 5 However, no previous studies have measured the level of oxytocin or any endogenous hormone that may induce uterine contractions and treating the sample exclusively with acupressure instead. For this reason, future studies are needed to elucidate the physiological mechanisms that underlie acupressure in the body of the mother.
SP6G showed a lower cesarean section rate among the groups in this study. In contrast, the CG group had 15.4% more cesarean sections than SP6G, reaching the rate recorded in the last annual report of the institution where the study was conducted (44.5% cesarean sections in 2013); f however, no statistically significant difference was observed. By contrast, two RCTs showed a significant reduction of 10.0% 18 and 12.8% 7 in the number of cesarean sections. However, these studies included only women who were nulliparous or who had not had previous cesarean section.
Some authors 13 suggest that cesarean section may contribute to elevated risk of maternal death. The progressive increase in the cesarean section rate in Brazil c has become a disturbing indicator for public health and related policies. Brazil is among the countries that most use this type of delivery, as shown in a global survey conducted in 2007. 3 Alternative methods that promote improved progress of labor and consequently, of vaginal birth, can significantly decrease the number of cesarean sections, as proposed in this study.
No changes in the Apgar scores were observed among newborns born to women who received acupressure when compared with those born to women in the other groups, indicating that there is no adverse effect for those born to mothers receiving this intervention, corroborating the results of the RCTs that assessed this variable. 9 , 18
Despite the lack of detail on the total dose of oxytocin and prostaglandin administered (due mainly to the absence of the exact dosage in the medical history), the administration of these drugs as well as the number of participants receiving these drugs in the three groups was detailed in the present study.
Another limitation is related to the fact that the study was conducted in a university hospital, which is a referral center for high-risk pregnancies, which may have contributed to the high rates of medical interventions.
The results of this study indicated that 20 min of acupressure on the SP6 point may be a complementary strategy for augmenting labor and/or shortening the first stage of labor without causing adverse effects to the mother or the newborn.
The cesarean section rate did not significantly differ between the groups, although it was lower in SP6G. The fact that the university hospital served women with high-risk pregnancies may have influenced the present results, including those related to induction and augmentation of labor, which suggests that better results can be achieved in the use of this technique in natural childbirth centers.
In conclusion, acupressure can be easily implemented in clinical practice because it does not require prolonged training, and therefore can be offered to women who prefer less invasive methods performed by nurses or trained professionals.
ACKNOWLEDGMENTS
The authors are grateful to Henrique Oliveira Ceretta of the Nursing School at the Universidade Estadual de Campinas for his contributions to the statistical analysis.
Footnotes
Berns SD, Kott A, editores. Toward improving the outcome of pregnancy III: enhancing perinatal health through quality, safety and performance initiatives. White Plain: March of Dimes National Foundation; 2010 [cited 2013 Aug 19]. Available from: http://www.marchofdimes.com/glue/files/TIOPIII_FinalManuscript.pdf
Menacker F, Hamilton BE. Recent trends in cesarean delivery in the United States. Atlanta; 2010 [cited 2013 Aug 25]. Available from: http://www.cdc.gov/nchs/data/databriefs/db35.pdf
Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise de Situação de Saúde. Saúde Brasil 2011: uma análise da situação de saúde e a vigilância da saúde da mulher. Brasília (DF); 2012 [cited 2013 Oct 14]. Available from: http://bvsms.saude.gov.br/bvs/ publicacoes/saude_brasil_2011.pdf
Fundação Oswaldo Cruz. Nascer no Brasil: pesquisa revela número excessivo de cesarianas. Agência Fiocruz de Notícias. Rio de Janeiro (RJ); 2014 [cited 2014 Oct 20]. Available from: http://portal.fiocruz.br/pt-br/content/pesquisa-revela-numero-excessivo-de-cesarianas-no-pais
Universidade Estadual de Campinas. Centro de Assistência Integral à Saúde da Mulher. Divisão de Obstetrícia. Preparo cervical e indução do parto: protocolo. Campinas (SP); 2008 [cited 2013 Nov 14].
Universidade Estadual de Campinas. Centro de Atenção Integral à Saúde da Mulher. Hospital da Mulher Prof. Dr. José Aristodemo Pinotti. Relatório anual do Conselho Técnico Administrativo – CTA/CAISM. Campinas; 2013 [cited 2014 Oct 23]. Available from: http://www.caism.unicamp.br/templates/shaper_pheonix/PDF/RelatorioAnualAtividades2013.pdf
Based on the master’s thesis of Mafetoni RR, titled: “Acupressão para alívio da dor no trabalho de parto: ensaio clínico randomizado,” presented to the Postgraduate Program in Nursing at the Nursing College at Universidade Estadual de Campinas, in 2014.
REFERENCES
- 1.Almeida NAM, Sousa JT, Bachion MM, Silveira NA. Utilização da técnica de respiração e relaxamento para alivio de dor e ansiedade no processo de parturição. 10.1590/S0104-11692005000100009Rev Latino-Am Enfermagem. 2005;13(1):52–58. doi: 10.1590/s0104-11692005000100009. [DOI] [PubMed] [Google Scholar]
- 2.Bastos SRC. Shiatsu tradicional: fundamentos, prática e clínica shiatsuterapia. Rio de Janeiro: Sohaku-in; 2000. [Google Scholar]
- 3.Bétran AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, Van Look P, et al. Rates of caesarean section: analysis of global, regional and national estimates. Pediatr Perinat Epidemiol. 2007;21(2):98–113. doi: 10.1111/j.1365-3016.2007.00786.x. http://www.ncbi.nlm.nih.gov/pubmed/17302638 [DOI] [PubMed] [Google Scholar]
- 4.Chang SB, Park YW, Cho JS, Lee MK, Lee BC, Lee SJ. Differences of cesarean section rates according to San-Yin-Jiao(SP6) acupressure for women in labor. Taehan Kanho Hakhoe Chi. 2004;34(2):324–332. doi: 10.4040/jkan.2004.34.2.324. [DOI] [PubMed] [Google Scholar]
- 5.Chung U, Hung L, Nancy O, Kuo S. Effects of LI4 and BL 67 Acupressure on Labor Pain and Uterine Contractions in the First Stage of Labor. 10.1097/01.JNR.0000347644.35251.c1J Nurs Res. 2003;11(4):251–260. doi: 10.1097/01.jnr.0000347644.35251.c1. [DOI] [PubMed] [Google Scholar]
- 6.Clark SL, Miller DD, Belfort MA, Dildy GA, Frye DK, Meyers JA. Neonatal and maternal outcomes associated with elective term delivery. 10.1016/j.ajog.2008.08.068Am J Obstet Gynecol. 2009;200(2):156–157. doi: 10.1016/j.ajog.2008.08.068. [DOI] [PubMed] [Google Scholar]
- 7.Cook A, Wilcox E. Pressuring pain: alternative therapies for labor pain management. 10.1111/j.1552-6356.1997.tb00929.xAWHONN Lifelines. 1997;1(2):36–41. doi: 10.1111/j.1552-6356.1997.tb00929.x. [DOI] [PubMed] [Google Scholar]
- 8.Hamidzadeh A, Shahpourian F, Orak RJ, Montazeri AS, Khosravi A. Effects of LI4 acupressure on labor pain in the first stage of labor. 10.1111/j.1542-2011.2011.00138.xJ Midwifery Womens Health. 2011;57(2):133–138. doi: 10.1111/j.1542-2011.2011.00138.x. [DOI] [PubMed] [Google Scholar]
- 9.Hjelmstedt A, Shenoy ST, Stener-Victorin E, Lekander M, Bhat M, Balakumaran L, et al. Acupressure to reduce labor pain: a randomized controlled trial. 10.3109/00016349.2010.514323Acta Obstet Gynecol Scand. 2010;89(11):1453–1459. doi: 10.3109/00016349.2010.514323. [DOI] [PubMed] [Google Scholar]
- 10.Lee MK, Chang SB, Lee HS, Kim HS. Effects of treatment with San-Yin-Jian (SP-6) acupressure for labor women on labor pain, length time for delivery and anxiety: A clinical trial pilot study. Korean J Women Health Nurs. 2002;8(4):559–569. [Google Scholar]
- 11.Lee MK. Effects of San-Yin-Jiao (SP6) acupressure on labor pain, delivery time in women during labor. Taehan Kanho Hakhoe Chi. 2003;33(6):753–761. doi: 10.4040/jkan.2003.33.6.753. [DOI] [PubMed] [Google Scholar]
- 12.Lee MK, Chang SB, Kang D. Effects of San-Yin-Jiao(SP6) acupressure on labor pain, delivery time in women during labor. 10.1089/acm.2004.10.959J Altern Complement Med. 2004;10(6):959–965. doi: 10.1089/acm.2004.10.959. [DOI] [PubMed] [Google Scholar]
- 13.Leite RMB, Araújo TVB, Albuquerque RM, Andrade ARS, Duarte Nt JP. Fatores de risco para mortalidade materna em área urbana do Nordeste do Brasil. 10.1590/S0102-311X2011001000011Cad Saude Publica. 2011;27(10):1977–1985. doi: 10.1590/s0102-311x2011001000011. [DOI] [PubMed] [Google Scholar]
- 14.Kashanian M, Shahali S. Effects of acupressure at the Sanyinjiao point (SP6) on the process of active phase of labor in nulliparas women. 10.3109/14767050903277662J Matern Fetal Neonatal Med. 2010;23(7):638–641. doi: 10.1080/14767050903277662. [DOI] [PubMed] [Google Scholar]
- 15.Kim YR, Chang SB, Lee MK, Maeng WJ. Effects on Labor Pain and Length of Delivery Time for Primipara Women treated by San-Yin-Jian (SP-6) Acupressure and Hob-Gog (LI-4) Acupressure. Korean J Women Health Nurs. 2002;8(2):244–256. [Google Scholar]
- 16.Machin D, Campbell M, Fayers P, Pinol A. Sample Size Tables for Clinical Studies. 2. Malden: Blackwell Science; 1997. [Google Scholar]
- 17.Nagahama EEI, Santiago SM. A institucionalização médica do parto no Brasil. 10.1590/S1413-81232005Cienc Saude Coletiva. 2005;10(3):651–657. [Google Scholar]
- 18.Salehian T, Dehcheshmaei FS, Pirak A, Kazemian A, Atarodi Z, Righi SDN. Comparison of the effect of Hoku Point (LI4) acupressure with that of San-Yin-Jiao (SP6) acupressure on labor pain and the length of delivery time in primiparous women. SJKU. 2011;16(1):64–72. [Google Scholar]
- 19.Schawartz D, Lellouch J. Explanatory and pragmatic attitudes in therapeutical trials. 10.1016/j.jclinepi.2009.01.012J Clin Epidemiol. 2009;62(5):499–505. doi: 10.1016/j.jclinepi.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 20.Smith CA, Collins CT, Crowther CA, Levett KM. Acupuncture or acupressure for pain management in labour. CD00923210.1002/14651858.CD009232Cochrane Database of Syst Rev. 2011;7 doi: 10.1002/14651858.CD009232. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization Appropriate technology for birth. Lancet. 1985;2(8452):436–437. [PubMed] [Google Scholar]
- 22.Yamamura Y. Acupuntura tradicional: a arte de inserir. 2. São Paulo: Roca; 1998. [Google Scholar]
- 23.Zar JH. Bioestatistical Analysis. 2. Englewood Cliffs: Prentice-Hall; 1984. [Google Scholar]