Abstract
Object
The authors analyzed headache relief after anterior cervical discectomy. Headache may be relieved after anterior cervical discectomy, but the mechanism is unknown. If headaches were directly referred from upper cervical pathology, more headache relief would be expected from surgery performed at higher cervical levels. If spinal kinesthetics were the mechanism, then headache relief may differ between arthroplasty and fusion. Headache relief after anterior cervical discectomy was quantified by the operated disc level and by the method of operation (arthroplasty vs arthrodesis).
Methods
The authors performed a post hoc analysis of an artificial disc trial. Data on headache pain were extracted from the Neck Disability Index (NDI) questionnaire.
Results
A total of 260 patients underwent single-level arthroplasty or arthodesis. Preoperatively, 52% reported NDI headache scores of 3 or greater, compared with only 13%–17% postoperatively. The model-based mean NDI headache score at baseline was 2.5 (95% CI 2.3–2.7) and was reduced by 1.3 points after surgery (95% CI 1.2–1.4, p < 0.001). Higher cervical levels were associated with a greater degree of preoperative headache, but there was no association with headache relief. There was no significant difference in headache relief between arthroplasty and arthrodesis.
Conclusions
Most patients with symptomatic cervical spondylosis have headache as a preoperative symptom (88%). Anterior cervical discectomy with both arthroplasty and arthrodesis is associated with a durable decrease in headache. Headache relief is not related to the level of operation. The mechanism for headache reduction remains unclear.
Keywords: headache, spine, cervicogenic, spondylosis, cervical
Headache is commonly associated with lower cervical spondylosis. Anterior neck surgery is associated with a significant reduction in headache. 10,14,19,20,22,25 Cervicogenic headache (International Headache Society [IHS] diagnosis 11.2.1) is defined according to strict criteria by the IHS and is thought to be referred from structures in the neck.5 The putative mechanism for cervicogenic headache involves afferent sensory input conveyed through the upper cervical nerves (C1–3) that converge on the spinal trigeminal nucleus, causing referred cranial pain.2 This mechanism fails to explain headache relief from anterior cervical discectomy at lower cervical levels. The trigeminocervical nucleus could theoretically extend farther down the cervical spinal cord than expected from anatomical studies. Therefore, lower cervical roots may project to the trigeminocervical nucleus. 4 Alternatively, kinesthetic impairment in the lower cervical spine could cause headache indirectly through structures innervated by C1–3.2,10,14,19,20,22,25
If spinal-mediated headache is a referred pain phenomenon, then operations on more rostral intervertebral discs might result in greater headache relief. Alternatively, if kinesthetic improvements after cervical spine surgery bring about headache relief, then cervical arthroplasty might result in greater symptomatic benefit for headaches. We determined the incidence of headache in patients undergoing anterior cervical discectomy for spondylosis-associated radiculopathy and/or myelopathy. We also determined the response of headache to anterior cervical discectomy. To preliminarily investigate the mechanism for headache, we analyzed headache based on the operated level, preoperative headache incidence, and postoperative headache reduction. We compared headache reduction in patients receiving an artificial disc versus those undergoing fusion.
Methods
Data were obtained from a multicenter randomized investigational device exemption (IDE) clinical trial to evaluate an artificial disc (Mobi-C, LDR Spine). The results of this study have been previously presented.6 The inclusion criteria consisted of adult patients (> 18 years) with symptoms of radiculopathy or myelopathy and cervical spondylosis at up to 2 levels and without significant facet disease. Patients were randomized on an allocation ratio of 2:1 for either anterior cervical discectomy and arthroplasty or anterior cervical discectomy and fusion. Subjects were administered the Neck Disability Index (NDI) questionnaire preoperatively and at 6 weeks and 3, 6, 12, 18, and 24 months. Data on headache pain (rated on a scale of 0–5) were extracted from the questionnaire at each time point and were analyzed. Our study included only those patients undergoing single-level surgery. The NDI headache scoring is as follows: 0, “I have no headaches at all.”; 1, “I have slight headaches that come infrequently.”; 2, “I have moderate headaches that come infrequently.”; 3, “I have moderate headaches that come frequently.”; 4, “I have severe headaches that come frequently.”; and 5, “I have headaches almost all the time.” This study was approved by the University of California, Davis, institutional review board and adheres to the principles set forth in the US Code of Federal Regulations and the World Medical Association Declaration of Helsinki.
Data Analysis
We summarized the frequencies and descriptive statistics (mean, SD, and range) at each of the 7 time points (baseline and 6 postoperative times). The primary analytical goals were 1) to determine whether there was postoperative relief of headache pain, 2) to determine whether this relief increased or decreased during the follow-up time, and 3) to determine whether there was a peak time of greatest improvement. We assessed this using mixed-models repeated measures regression,13 allowing for possible unequal spacing and numbers of follow-up measures and possible differences in starting levels, specifying a random effect for subject and unstructured covariance matrix. We also considered, in secondary analyses, generalized linear models with a logistic link and binomial error structure to address the nonnormality of the pain scores.26 For simplicity of reporting, we took the mixed models as the primary analysis. Effects of the surgical procedure (artificial disc vs fusion) and operated level were examined by adding both main effects and interaction terms (predictor with postoperative time) to the mixed models. All tests were 2-sided; p values < 0.05 were considered significant. Statistical analyses were carried out using SAS/STAT software (SAS Institute, Inc.).
Results
Table 1 shows the clinical data for the study. A total of 260 patients underwent single-level anterior cervical discectomy and arthroplasty (69%) or anterior cervical discectomy and fusion (5 patients at C3–4, 13 patients at C4–5, 146 patients at C5–6, and 96 patients at C6–7). Prior to surgery, 88% reported headache and 52% reported NDIs of 3 or greater. After surgery, 13%–17% of NDIs were 3 or greater (mean NDI 15.3 ± 1.2). Some patients who did not have headache at baseline later reported pain, and therefore we included all patients in this analysis to avoid bias due to regression to the mean.
TABLE 1.
Clinical data in patients who underwent either arthroplasty or fusion
| Parameter | Value |
|---|---|
| age in yrs | |
| median | 43 |
| range | 21–67 |
| no. of patients | 260 |
| % female sex | 54 |
| level of op (%) | |
| C3–4 | 5 (2) |
| C4–5 | 13 (5) |
| C5–6 | 146 (56) |
| C6–7 | 96 (37) |
| mean ± SD baseline headache score | 2.5 ± 1.5 |
| no. of patients w/ baseline headache (%) | 228 (88) |
| no. of patients w/ baseline headache ≥3 (%) | 135 (52) |
| surgical technique (%) | |
| fusion | 81 (31) |
| artificial disc | 179 (69) |
| no. of patients w/ 2-yr follow-up data (%) | 244 (94) |
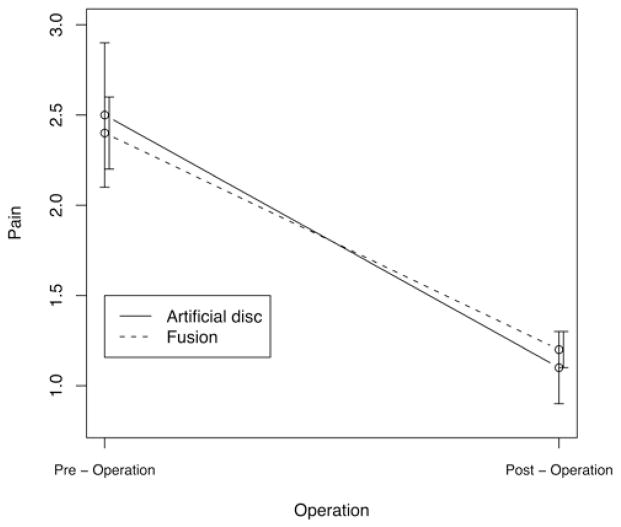
Repeated measures analyses of the headache trajectories supported the impression of substantial decline in headache pain following surgery. The model-based mean pain score at baseline (before surgery) was 2.5 (95% CI 2.3–2.7), and at postoperative visits the mean pain level was reduced by 1.3 points on average (95% CI 1.2–1.4 points lower than the preoperative level, p < 0.001 for test of no difference between pre- and postoperative pain). Eighty-one patients (31%) underwent fusion surgery, and the remaining 179 underwent artificial disc placement. We found no statistically significant difference between these groups at baseline (p = 0.56) in a mixed model with only a 0.11-point difference in estimated pain score (95% CI −0.25 to 0.47). During the postoperative period, the artificial disc group had a 0.19-point lower pain score than the fusion group (95% CI −0.45 to 0.07), but this modest difference was consistent with chance (p = 0.15) (Fig. 1).
Fig. 1.
The effect of surgery type (artificial disc vs fusion) on headache relief. The pre- and postoperative NDI headache scores were 2.5 and 1.1, respectively, for the artificial disc group and 2.4 and 1.2, respectively, for the fusion group. There was no significant difference between the groups (p = 0.56).
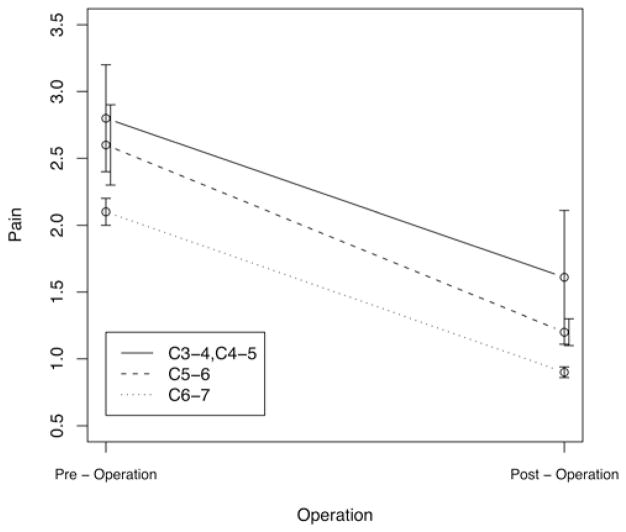
The most frequently treated level was C5–6 (56%, n = 146), followed by C6–7 (37%, n = 96), C4–5 (5%, n = 13), and C3–4 (2%, n = 5). Higher levels (levels more proximal to the head) were associated with significantly greater preoperative pain. There was no difference, however, in degree of postoperative pain relief as a function of surgical level (0.08 per level, 95% CI −0.12 to 0.28, p = 0.45 for quantitative approach, p = 0.38 overall for categorical approach). Because of the small numbers of surgeries at either C3–4 or C4–5, these levels were lumped together for the purposes of statistical analysis (Fig. 2).
Fig. 2.
The effect of the operated level on headache relief. The highest levels (C3–4 and C4–5) were combined for analysis, since the number of operations at these levels was low (5 and 13, respectively). The pre- and postoperative NDI headache scores, respectively, were 2.8 and 1.6 for levels C3–4/C4–5, 2.6 and 1.2 for C5–6, and 2.1 and 0.9 for C6–7. Higher levels (those more proximal to the head) were associated with greater preoperative pain. There was no difference, however, in degree of postoperative pain relief as a function of what level was surgically treated (p = 0.45 for quantitative approach, p = 0.38 overall for categorical approach).
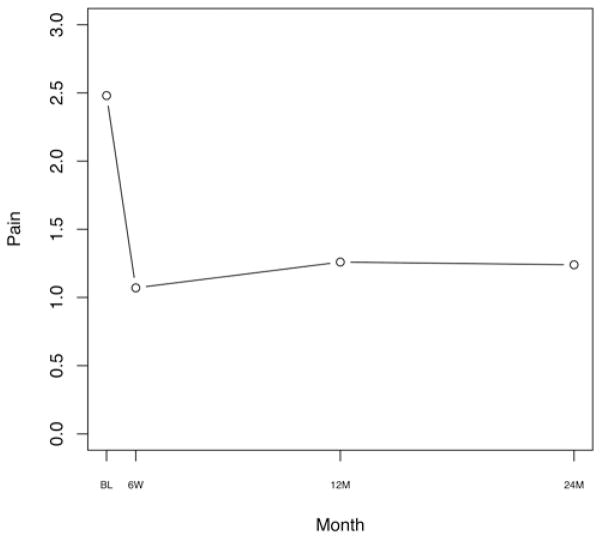
In secondary analyses, we looked both for trends in postoperative pain levels during the 2 years of follow-up (either increase or decrease), and for month-specific differences from the 6-week follow-up level. We found a very small but statistically significant worsening of pain level (0.002 points per week [p = 0.018]), amounting to a change of just one-tenth of a point worse per year, but the immediate postoperative pain relief was estimated in this model as 1.4 points (95% CI 1.3–1.5 points). This suggested the possibility of a nonlinear trajectory for the attenuation of pain relief. When we looked at differences from the short-term (6-week) pain report, pain relief continued without significant diminution through the third follow-up (6 months), but there was a significant rebound of 0.2 points on average by the 12-month visit (p = 0.02 [95% CI 0.0–0.4 points]). The 18-month and 2-year visits showed the same (after rounding) rebound compared with that at 6 weeks (0.2 points, p = 0.04). In this model, the pain relief at 6 weeks was estimated as a reduction of 1.4 points. Thus, the 2nd year showed an attenuation of a significant portion of the pain relief from the first 6 weeks to 6 months after surgery, but with most of the improvement retained (Fig. 3).
Fig. 3.
The preservation of headache relief after surgery over time in all patients up to 2 years postoperatively. Postoperative headache NDI scores at baseline (BL), 6 weeks (6W), 12 months (12M), and 24 months (24M) were 2.48, 1.07, 1.26, and 1.24, respectively. We found a statistically significant trend for very gradual worsening of pain level of 0.002 NDI headache points per week (p = 0.018), amounting to a change of just a tenth of a point worse per year. The 2nd year showed an attenuation of a significant portion of the pain relief from the first 6 weeks to 6 months after surgery, but with most of the improvement retained.
Our findings did not change materially in secondary analyses using generalized linear models to allow for nonnormality of the pain scale residuals and possible nonlinearity.
Discussion
Headache associated with pathology in the neck, also known as cervicogenic headache, has a long history in the literature, tracing back to John Hinton’s remarks (ca 1860) that headache in the territory of the greater or lesser occipital nerve could be mediated by pathology between C-1 and C-2.17 Cervicogenic headache and its treatment are informed by 3 disciplines: surgery, neurology, and pain medicine.
Surgeons have long noted an association between cervical pathology and headaches and also have reported the relief of headache following operations on both the upper and lower cervical spine. A classic case series from 1946 described a 17-year-old girl with C-5 pathology and headaches, without other symptoms.11 In 1948 Raney and Raney published a series of 4 patients with headache and lower cervical disc pathology, and these authors subsequently proposed the theory that headache following traumatic brain injury might be referable to cervical structures.21 This theory was furthered by Braaf and Rosner in 1975.3 Importantly, lower cervical structures are often implicated in headache. Surgeons have reported headache relief following anterior neck surgery, mostly involving lower cervical disc levels.4,7–10,16,18,22,25 In the clinical study reported herein, we observed a very high incidence of headache in patients diagnosed with cervical disc disease, often at the lower cervical levels.
Our study was similar to a previously published report by Riina et al.22 that also used the headache score from the NDI, a nonspecific grading system that does not characterize the headache beyond the frequency and severity of symptoms. In the study by Riina et al., data from 2 separate IDE trials (randomized 1:1 arthroplasty to arthrodesis) were combined, whereas our study only included data from a single IDE trial (randomized 2:1). Furthermore, to shed light on the possible mechanism for headache relief, we additionally investigated the effect of level of operation on both the presence of preoperative headache and headache relief after surgery.
Our findings were similar to those previously reported. We found a preoperative incidence of headache and severe headache (NDI 3–5) of 88% and 52%, respectively, which is nearly identical to the previously reported incidences of 86.2% and 52.1%. We also similarly found significant improvement in headache scores for both the arthroplasty and arthrodesis groups that endured for the 24-month study period, and also similarly did not identify a statistically significant improvement in mean headache scores after surgery between the 2 groups. We report the novel findings that higher cervical levels were associated with greater preoperative headache pain, but that the level of operation did not predict the improvement in headache score.
Ottar Sjasstad, a Norwegian migrainologist, coined the term “cervicogenic headache” in 1983, and out of the European school of neurology emerged fairly strict clinical diagnostic criteria for cervicogenic headache.24 The Cervicogenic Headache International Study Group, led by Dr. Sjaastad, outlined initial (1990) and revised (1998) diagnostic criteria for cervicogenic headache, which include symptoms and signs of neck involvement, precipitation of headache by neck movement or awkward neck position, and also unilaterality without side-shift.23 A centerpiece of the Cervicogenic Headache International Study Group diagnostic criteria is the requirement for a relief of headache after anesthetic blockade of offending structures, such as major or minor occipital nerves, the C-2 root, the third occipital nerve, facet joints, or the lower cervical roots and branches on the symptomatic side. Autonomic symptoms, such as photo- and phonophobia, nausea, and vomiting, are considered to be of lesser significance. Patients with relief of headache after surgery but without prior evaluation may not qualify for a cervicogenic headache diagnosis. The IHS streamlined the diagnostic criteria, which include: A) pain in the head or face referred from a source in the neck, B) imaging or other evidence of a lesion in the neck “known to be … a valid cause of headache,” C) demonstration of clinical signs or diagnostic blockade that implicate the neck as a cause of the pain, and D) the pain resolves within 3 months after treatment of the neck lesion. Anterior neck surgery with headache relief would therefore fulfill Criterion D of the IHS classification system for cervicogenic headache.5
Clinical evidence supports the notion that cervicogenic headache can originate from muscular, articular, osseous, neurological, or vascular structures in the neck. The precise neurological mechanism that refers neck pathology to various parts of the head and face is not known. Nikolai Bogduk, a physician and anatomist in Australia, has championed the trigeminocervical nucleus as a neuroanatomical basis for cervicogenic headache.1 Convergence of trigeminal and cervical afferents within the gray matter of this nucleus leads to referred pain in the head and face. Therefore, pathology or irritation caused by structures innervated by C1–3, including muscles, joints, ligaments, and spinal and posterior fossa dura, have the potential to cause referred head or face pain. The limitation of this theory is that it does not provide a mechanism for headache induced by lower cervical pathology. Our data indicate that the level of cervical pathology does not predict headache relief after surgery. Patients with lower cervical disc operations experienced headache relief after discectomy to the same extent as patients with higherlevel disc pathology (Fig. 3). Sjaastad et al. acknowledged that discrepancy in the offending cervical level among various clinical studies of cervicogenic headache “is not readily explainable.”24 With regard to the ability of lower cervical spinal levels to produce headache, Bogduk and Govind argued that since there is no neuroanatomical link between the lower cervical nerves and the trigeminocervical nucleus, “Intermediate mechanisms, such as muscle tension and secondary kinematic abnormalities that affect upper cervical joints might be involved.”2 If this were true, one might predict that total cervical disc replacement would favorably affect headache relief by improving spinal kinesthetics at higher levels. Our data demonstrate that both arthroplasty and arthrodesis result in favorable relief of headache (Fig. 2). Thus, improvement in spinal kinesthetics after cervical disc surgery is less likely to be important in mediating headache relief.
Alternative mechanisms for headache generation in cervical spondylosis must be sought. Innervation of the spinal dura through meningeal rami can extend caudally over 1–2 segments,12 so that, theoretically, dorsal rami from C-3 could receive afferent input from lower levels resulting in referred pain from the spinal trigeminal tract in the upper cord. Alternatively, CSF obstruction may play a role. Cerebrospinal fluid hydrodynamics have been implicated in headaches related to CSF outflow obstruction at the foramen magnum in Chiari malformation Type I. McGirt et al.15 prospectively measured cine phase contrast MRI of the foramen magnum in 33 patients undergoing Chiari decompression. Occipital but not generalized headaches were significantly associated with obstructed CSF outflow at the foramen magnum. Notably, all patients with obstructed CSF outflow did well after decompressive surgery, regardless of headache location.15 Cervical spondylotic disease, especially when combined with congenital cervical canal stenosis, creates an obstruction to pulsatile CSF flow across the foramen magnum and upper spinal canal into the large spinal CSF capacitance system during systole. Outflow obstruction within the cervical spinal canal could potentially cause an increased CSF pulse pressure that could be transmitted to both the posterior fossa and spinal canal dura and nerve root sleeves rostral to the obstruction, thus resulting in cervicogenic headache according to the trigeminocervical mechanism outlined above. Indeed, not only anterior neck surgery but posterior decompression also relieves headache. Jansen reported a series of 8 patients with cervicogenic headache; 7 were relieved of headache following laminoplasty.7 The authors remarked that fewer innervated structures are encountered with the posterior approach, and they speculate that the spinal dura is a triggering factor. The dorsal spinal dura is, however, relatively sparsely innervated compared with the ventral dura,12 and headache generation and relief by an alternative mechanism is more likely.
This study used a crude headache measure—the NDI headache score—and the headaches were not further characterized in terms of quality, location, laterality, and duration. Also, the patients did not undergo diagnostic injections of cervical structures to evaluate potential pain generators. Therefore, it is not possible to determine whether the headaches met the standard diagnostic criteria for cervicogenic headache.
Although we failed to find a significant association between headache relief and the level of surgery, the original study was not powered to detect such a difference, and the conclusions drawn are at risk for a Type II error. A relatively small number of patients underwent surgery at the C3–4 and C4–5 levels. Estimated differences were very small and confidence intervals were relatively narrow, however, suggesting that any differences we failed to detect are likely to be modest at best. This study should be interpreted with caution in that it is a post hoc analysis of prospectively collected data, and further prospective study would be necessary to confirm our findings.
We add the very important caveat that this study investigated the effect of anterior neck surgery on headache in a cohort of patients with cervical myelopathy and/or radiculopathy. Headache was not an indication for enrollment in the trial. If headache had been prospectively evaluated in greater detail as an independent outcome measure, the results might have been different. Therefore, our study should not be interpreted as justifying headache as a primary indication for anterior cervical decompression. It was outside the scope of this study to associate headache relief with the relief of other symptoms.
Conclusions
A majority of patients who undergo surgery for myeloradiculopathy present with headaches. Anterior neck surgery, either arthroplasty or arthrodesis, often results in lasting headache relief, irrespective of the operated level. This study does not provide sufficient evidence to support headache as an independent indication for anterior cervical discectomy.
Acknowledgments
This work was supported by the UC Davis Department of Neurological Surgery and the UC Davis Spine Center. Statistical consultation was provided through Grant No. UL1RR024146 from the National Center for Research Resources, a component of the NIH, and NIH Roadmap for Medical Research. The LDR company provided access to data but no financial support and had no influence on what material is reported in the manuscript. Kee D. Kim and Hyun W. Bae each receive royalties and serve as consultants for LDR Spine. Dr. Kim is also a consultant for Stryker and Globus.
Abbreviations used in this paper
- IDE
investigational device exemption
- IHS
International Headache Society
- NDI
Neck Disability Index
Footnotes
Some of the data were presented in the Poster Forum at the 2010 CNS Annual Meeting, October 18, 2010, in San Francisco, California.
Disclosure
Author contributions to the study and manuscript preparation include the following. Conception and design: Schrot. Acquisition of data: Kim, Schrot, Bae. Analysis and interpretation of data: Schrot, Li, Beckett. Drafting the article: Schrot, Mathew. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Kim. Statistical analysis: Li, Beckett. Administrative/technical/material support: Kim, Schrot. Study supervision: Kim, Schrot. Provided preliminary background research: Mathew.
References
- 1.Bogduk N. The anatomical basis for cervicogenic headache. J Manipulative Physiol Ther. 1992;15:67–70. [PubMed] [Google Scholar]
- 2.Bogduk N, Govind J. Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol. 2009;8:959–968. doi: 10.1016/S1474-4422(09)70209-1. [DOI] [PubMed] [Google Scholar]
- 3.Braaf MM, Rosner RS. Trauma of cervical spine as cause of chronic headache. J Trauma. 1975;15:441–446. doi: 10.1097/00005373-197505000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Diener HC, Kaminski M, Stappert G, Stolke D, Schoch B. Lower cervical disc prolapse may cause cervicogenic headache: prospective study in patients undergoing surgery. Cephalalgia. 2007;27:1050–1054. doi: 10.1111/j.1468-2982.2007.01385.x. [DOI] [PubMed] [Google Scholar]
- 5.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders. Cephalgia. (2) 2004;24 (Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 6.Hisey M, Bae HW, Davis R, Gaede S, Hoffman G, Kim K, et al. Multi-center, prospective, randomized, controlled investigational device exemption study comparing Mobi-C© Cervical Artificial Disc to anterior discectomy and fusion in the treatment of symptomatic degenerative disc disease in the cervical spine. Presented at the 11 annual conference of the International Society for the Advancement of Spine Surgery; Las Vegas. 2011; [Accessed April 29, 2014]. Abstract ( http://www.isass.org/pdf/sas11/2-Wednesday/Cervical-TDR/583.pdf) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jansen J. Laminoplasty—a possible treatment for cervicogenic headache? Some ideas on the trigger mechanism of CeH. Funct Neurol. 1999;14:163–165. [PubMed] [Google Scholar]
- 8.Jansen J. Surgical treatment of cervicogenic headache. Cephalalgia. 2008;28 (Suppl 1):41–44. doi: 10.1111/j.1468-2982.2008.01620.x. [DOI] [PubMed] [Google Scholar]
- 9.Jansen J. Surgical treatment of non-responsive cervicogenic headache. Clin Exp Rheumatol. 2000;18 (2 Suppl 19):S67–S70. [PubMed] [Google Scholar]
- 10.Jansen J, Sjaastad O. Cervicogenic headache: long-term prognosis after neck surgery. Acta Neurol Scand. 2007;115:185–191. doi: 10.1111/j.1600-0404.2006.00771.x. [DOI] [PubMed] [Google Scholar]
- 11.Keegan JJ. Dermatome hypalgesia with posterolateral herniation of lower cervical intervertebral disc. J Neurosurg. 1946;4:115– 139. doi: 10.3171/jns.1947.4.2.0115. [DOI] [PubMed] [Google Scholar]
- 12.Kimmel DL. Innervation of spinal dura mater and dura mater of the posterior cranial fossa. Neurology. 1961;11:800–809. doi: 10.1212/wnl.11.9.800. [DOI] [PubMed] [Google Scholar]
- 13.Laird NMN, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–974. [PubMed] [Google Scholar]
- 14.Lied B, Roenning PA, Sundseth J, Helseth E. Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage) BMC Surg. 2010;10:10. doi: 10.1186/1471-2482-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGirt MJ, Nimjee SM, Floyd J, Bulsara KR, George TM. Correlation of cerebrospinal fluid flow dynamics and headache in Chiari I malformation. Neurosurgery. 2005;56:716–721. doi: 10.1227/01.neu.0000156203.20659.14. [DOI] [PubMed] [Google Scholar]
- 16.Michler RP, Bovim G, Sjaastad O. Disorders in the lower cervical spine. A cause of unilateral headache? A case report. Headache. 1991;31:550–551. doi: 10.1111/j.1526-4610.1991.hed3108550.x. [DOI] [PubMed] [Google Scholar]
- 17.Pearce JM. Cervicogenic headache: an early description. J Neurol Neurosurg Psychiatry. 1995;58:698. doi: 10.1136/jnnp.58.6.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Persson LCG, Carlsson JY. Headache in patients with neckshoulder- arm pain of cervical radicular origin. Headache. 1999;39:218–224. doi: 10.1046/j.1526-4610.1999.3903218.x. [DOI] [PubMed] [Google Scholar]
- 19.Persson LCG, Carlsson JY, Anderberg L. Headache in patients with cervical radiculopathy: a prospective study with selective nerve root blocks in 275 patients. Eur Spine J. 2007;16:953–959. doi: 10.1007/s00586-006-0268-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raney AA, Raney RB. Headache; a common symptom of cervical disk lesions; report of cases. Arch Neurol Psychiatry. 1948;59:603–621. doi: 10.1001/archneurpsyc.1948.02300400039002. [DOI] [PubMed] [Google Scholar]
- 21.Raney AA, Raney RB, Hunter CR. Chronic posttraumatic headache and the syndrome of cervical disc lesion following head trauma. J Neurosurg. 1949;6:458–465. doi: 10.3171/jns.1949.6.6.0458. [DOI] [PubMed] [Google Scholar]
- 22.Riina J, Anderson PA, Holly LT, Flint K, Davis KE, Riew KD. The effect of an anterior cervical operation for cervical radiculopathy or myelopathy on associated headaches. J Bone Joint Surg Am. 2009;91:1919–1923. doi: 10.2106/JBJS.H.00500. [DOI] [PubMed] [Google Scholar]
- 23.Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. Headache. 1998;38:442–445. doi: 10.1046/j.1526-4610.1998.3806442.x. [DOI] [PubMed] [Google Scholar]
- 24.Sjaastad O, Saunte C, Hovdahl H, Breivik H, Grønbaek E. “Cervicogenic” headache. An hypothesis. Cephalalgia. 1983;3:249–256. doi: 10.1046/j.1468-2982.1983.0304249.x. [DOI] [PubMed] [Google Scholar]
- 25.Torbjørn AF, Stolt-Nielsen A, Skaanes KO, Sjaastad O. Headache and the lower cervical spine: long-term, postoperative follow-up after decompressive neck surgery. Funct Neurol. 2003;18:17–28. [PubMed] [Google Scholar]
- 26.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]