Abstract
The extent to which deficits in specific cognitive domains contribute to older drivers’ safety risk in complex real-world driving tasks is not well understood. We selected 148 drivers older than 70 years of age both with and without neurodegenerative diseases (Alzheimer disease-AD and Parkinson disease-PD) from an existing driving database of older adults. Participant assessments included on-road driving safety and cognitive functioning in visuospatial construction, speed of processing, memory, and executive functioning. The standardized on-road drive test was designed to examine multiple facets of older driver safety including navigation performance (e.g. following a route, identifying landmarks), safety errors while concurrently performing secondary navigation tasks (“on-task” safety errors), and safety errors in the absence of any secondary navigation tasks (“baseline” safety errors). The inter-correlations of these outcome measures were fair to moderate supporting their distinctiveness. Participants with diseases performed worse than the healthy aging group on all driving measures, and differences between those with AD and PD were minimal. In multivariate analyses, different domains of cognitive functioning predicted distinct facets of driver safety on road. Memory and set-shifting predicted performance in navigation-related secondary tasks, speed of processing predicted on-task safety errors, and visuospatial construction predicted baseline safety errors. These findings support broad assessments of cognitive functioning to inform decisions regarding older driver safety on the road and suggest navigation performance may be useful in evaluating older driver fitness and restrictions in licensing.
Keywords: Driving safety, Cognitive function, On-road test, Aging, Alzheimer’s Disease, Parkinson’s Disease
1. Introduction
Epidemiological studies project an increase of 34% in crashes among all drivers compared to an increase of 178% among drivers 65 and older by 2030. Older drivers are also projected to account for 40% of the expected increases in crash involvement (Lyman et al., 2002; Evans, 2000). Cessation of driving restricts mobility, and is associated with subsequent depression and decreased well-being (Marottolli et al., 1997; Windsor et al., 2007). Empirical data are needed to distinguish between safe and unsafe older drivers so that decision-making in applied settings, including clinics and Department of Motor Vehicle offices (DMV), is better tailored to both preservation of mobility and public safety. To inform patients, clinicians and policy makers, empirical studies are needed to quantify drivers’ on-road safety risk in ways that capture the complexity of the driving task. To that end, we used our existing registry and database of healthy and diseased older drivers to quantify multiple facets of on-road driving performance and examined how different domains of cognitive function predicted each facet over and above disease status and age.
While controlling the vehicle and observing traffic rules, drivers engage in intrinsic secondary tasks, such as navigating to a destination based on directions or memory, and identifying landmarks such as restaurants or grocery stores. Difficulty on these key tasks, especially in familiar areas, may provide key clues to older drivers’ on-road safety risk. Older drivers tend to make more safety errors when navigating on their own than they do when following turn-by-turn directions of a driving instructor (Wood et al., 2009). Drivers who struggle with intrinsic tasks such as navigation may drive less safely overall.
This study examined driver performance in secondary navigation-related tasks of route-following and landmark/ sign identification. Drivers were asked 1) to memorize and execute a 4-turn route (Uc et al., 2004, 2007), and 2) to identify landmarks and traffic signs while driving on a commercial strip (Aksan et al., 2013, Uc et al., 2005, 2006). Their performance in these secondary navigation-related tasks, including number of correct turns, self-corrections, and number of restaurants and traffic signs identified, was evaluated separately from safety errors. Safety errors such as lane observance, lane change, speed control and others were measured during navigation-related tasks, or “on-task safety errors”. Safety errors were also measured during baseline driving (without secondary task demands) or “baseline safety errors”. Thus, the three driving outcomes were: 1) performance in navigation-related secondary tasks, 2) on-task safety errors, and 3) baseline safety errors.
The first goal of the study was to test whether performance in navigation-related secondary driving tasks was relevant to driver safety risk. Two pieces of evidence addressed this question. First, if error rates during secondary tasks (i.e., on-task safety errors) exceed baseline (no secondary task) safety error rates, this would indicate that navigation tasks intrinsic to driving affect concurrent safety, in line withWood et al. (2009). Second, if worse performance in navigation-related secondary tasks is associated with more baseline safety errors (when the driver is not performing secondary tasks, this correlation would indicate that older drivers who struggle with navigation also drive less safely overall.
The second goal was to examine whether cognitive functioning differentially predicted the three driving outcomes. Understanding which aspects of cognitive functioning predict specific facets of driving performance can inform design of off-road screening tests for driver licensure, clinician evaluations of driver fitness, and interventions for specific driving difficulties. Visual sensory function, motor, and cognitive functions including Useful Field of View (UFOV) predict driving safety outcomes (e.g., Aksan et al., 2012; Anstey et al., 2005; Anderson et al., 2012; Anstey & Woods, 2011; Ball et al., 1993; Ball et al., 2006; Dawson et al., 2010; Ross et al., 2009; Wood et al., 2008). Bivariate associations among predictors and driving safety measures range from fair to moderate. In multivariate analyses, UFOV and other cognitive functions often add to prediction of driver safety over and above the prediction provided by age and basic visual sensory function measures (Ball et al., 1993; Ball et al., 2006; Wood et al., 2008). This pattern is often found in drivers with healthy aging (Anstey et al., 2005; Wood et al., 2008) and age-related neurological disorders such as Parkinson’s (PD; Heikkila et al., 1998; Uc et al., 2011; Uc et al., 2009a; Wood et al., 2005) and Alzheimer’s disease (AD; Duchek et al., 2003; Fitten et al., 1995; Hunt et al., 1997; Iverson et al., 2010; Reger et al., 2004).
Driver assessment batteries often include tests of basic visual sensory function(e.g. acuity, contrast sensitivity) and UFOV, a measure of visual attention and processing speed (e.g., Aksan et al., 2012; Owsley et al., 1998; Sims et al., 2000; Ross et al., 2009; Wood et al., 2009). Tests of motor and cognitive functioning tend to vary across studies. Some investigators rely on reaction time tests that require coordination of motor and cognitive responses to driving related stimuli (Anstey & Woods, 2011; Wood et al., 2008). Others rely on widely used and standardized neuropsychological tests such as block construction, Trailmaking Test, and copying a complex figure (e.g. Anderson et al., 2012; Dawson et al., 2010; Uc et al., 2009). Lack of uniformity in test selection across studies makes it difficult to generate specific recommendations to clinicians who may lack access to expensive, specialized, or non-standard tests that are generally not found in neuropsychology clinics. This study relied on standard neuropsychological tests in four cognitive domains: visuospatial construction, memory, speed of processing, and set shifting (Anderson et al., 2012). We examined differential relevance of functioning in those cognitive domains in relation to three driving outcomes: a) navigation-related secondary task performance, b) on-task safety errors, and c) baseline safety errors.
Speed of processing declines during aging (Salthouse 1996). Many studies, including one based on the current sample (Anderson et al., 2012), have found that UFOV and other measures of cognitive functioning which heavily implicate speed of processing (e.g. Anstey & Wood, 2011; Ball et al., 1998; 2003, 2006; Clay et al., 2005) relate to driver safety errors. In this vein, we expect speed of processing to be associated with both on-task and baseline safety error rates.
Driving inherently involves the coordination of several subtasks and requires multi-tasking. Nevertheless in understanding and informing our predictions for sources of variation in on-task safety errors versus navigation-related secondary task performance, we find it useful to adopt the analogy that the measures obtained during the secondary task segments of the drive can be viewed as outcomes from a naturalistic dual-task paradigm. In laboratory based dual-task paradigms, Salthouse and colleagues (Salthouse & Miles, 2002; Salthouse et al., 2003) argued that general reduction in speed of processing may provide a better accounting for performance costs than executive functioning. Others have argued that executive function is more central to performance costs than speed of processing (Holtzer et al., 2005; Kramer et al., 1999). Recent meta-analyses indicate that age-related deficits in executive control play a small role in age-related declines in complex cognition (Verhaeghen, 2011). We examined this issue in driver performance costs in a naturalistic on-road test.
The secondary tasks in this study (identifying signs, landmarks, and following a route) are critical to navigation while driving and depend on both memory and visuospatial construction abilities. For example, dead reckoning is a critical cognitive mapping skill that allows navigation to a destination without getting lost, by relying on both internal and external cues to determine current location relative to a known starting point, permitting one to track and re-trace one’s path (Golledge, 1999). Cognitive mapping skills depend on visuospatial processing of information and memory, both of which decline with age. However, because local drivers were generally familiar with the area in which the on-road test was conducted, we expected memory to be particularly relevant to navigation-related performance. On familiar routes drivers can rely on long-term memory to reduce information processing and decision making demands. For example, in familiar areas major street names, restaurants and other landmarks as well as location of speed limit, traffic lights, and stop signs are stored as elements of cognitive maps. By relying on fixed attributes of cognitive maps in long-term memory in familiar routes, drivers can reduce processing demands and focus better on safety critical situational and dynamic task demands such as maintaining headway, changing lanes, and observing traffic signals. Thus, we would expect declines in memory to adversely impact performance in navigation-related tasks.
A key consideration for interpreting the literature of older driver safety concerns subject selection criteria. Studies to date have adopted various approaches including over-selecting from among aging drivers with a history of crashes (Ball et al., 1993; Owsley et al., 1991), selecting a representative, random sample of aging drivers free of neurological diseases (e.g., Wood et al., 2009), study a specific disease group such as PD or AD in relation to control participants (e.g., Reger et al., 2004; Uc et al., 2009). No study to date, however, has examined possible differences among those with AD and PD. In this study, we included both those with neurodegenerative disease and healthy aging adults. We expected to replicate the finding that those with neurodegenerative diseases would perform worse than healthy controls on all three outcome measures (Dawson et al., 2009; Reger et al., 2004; Uc et al., 2009; Wood et al., 2005). Small-sample studies to date do not suggest the presence of disease-specific differences in driving performance. Nevertheless, we explored mean differences in driving safety outcomes between those with AD and PD. We also considered the possibility that the associations of functioning in cognition (i.e. speed of processing, memory) with driving safety outcomes may be stronger in elderly with diseases compared to healthy elderly.
To summarize, we examined the effects of navigation-related secondary tasks intrinsic to driving on safety errors in naturalistic settings; and tested whether distinct aspects of cognitive functioning predicted multiple facets of driver performance over and above age, basic visual sensory functioning, and disease status; and explored whether the findings supported a disease-specific pattern of differences between those with AD and PD. The study fills several gaps in the literature. It examines the empirical utility of relatively simple modifications to design of on-road tests that can assess driving safety in advancing age more sensitively than DMV based tests. It is the first study to explore whether there are disease-specific markers of driving safety in AD and PD. It has the potential to inform decision making in applied settings such as clinics and DMV regarding the most relevant domains of cognitive functioning to driving safety.
2. Method
2.1 Sample
The participants were 148 (104 M, 44 F) active drivers between the ages of 70 and 89 (mean age = 75 years), including 77 with no neurologic disease, 32 with probable Alzheimer’s disease (AD), 39 with Parkinson’s disease (PD). Diagnosis of AD was based on the NINCDS-ADRDA criteria (McKhann et al., 1984)1. Diagnosis of PD was based on UK Parkinson's Disease Society Brain Bank clinical diagnostic criteria (Gibb & Lees, 1988; Hughes et al., 1992). All participants held a valid state driver’s license and were still driving. They were recruited from the general community by means of advertisements and from outpatient clinic to several studies of driving safety in advancing age. Data included in the current analyses were obtained from those participants who: 1) had completed the standard on-road driving evaluation, 2) those who completed the standard neuropsychological battery described below, 3) were 70 or older at the time of the assessment ensuring that the current sample is part of the subgroup that shows elevations in crash risk in epidemiological studies (Insurance Institute Highway Safety, March 2014). Exclusion criteria included alcohol or substance abuse, major psychiatric disease, use of sedating medication, and corrected visual acuity worse than 20/50. All participants provided informed consent according to the policies of the Institutional Review Board at the University of Iowa.
2.2 Overview of Procedures and Measures
Participants completed a battery of standardized neuropsychological tests lasting about 2 hours. These tests administered during the first visit yielded measures of basic visual sensory function and cognitive functioning which served as predictors. Generally on a separate day, participants took an 18-mile, 45-minute on-road driving test around Iowa City in an instrumented vehicle. Assessments conducted during the on-road drive test yielded the three outcome measures. Test descriptions, scoring, and data reduction are described next.
2.3 Basic Visual Sensory Function
Vision tests included contrast sensitivity with Pelli-Robson Chart, (Pelli et al., 1988), near and far acuity with Snellen and Early Treatment Diabetic Retinopathy Study charts (Ferris et al., 1982). Contrast sensitivity scores range from 0 to 2.25 with high scores indicating better performance, and acuity scores are expressed as logarithm of minimum angle of resolution with high scores indicating poorer performance. The raw test scores were z-transformed and were averaged to form the Visual Sensory Functioning composite (average r = .33) consistent with a recent confirmatory factor analytic study (Anderson et al., 2012).
2.4 Cognitive Functioning
2.4.1 Tests and Coding
The battery of standardized neuropsychological tests was selected on the basis of their conceptual relevance to driving and demonstrated sensitivity to brain dysfunction (for detailed test descriptions and scoring, see Lezak et al., 2004; Strauss et al., 2006). Brief descriptions and measures from each test are described next.
During the Complex Figure Test-Copy (CFT-Copy), participants are asked to reproduce a complex figure on a blank sheet of paper, and during the CFT-Recall they are asked to re-draw the same complex figure from memory 30 minutes after they completed CFT-Copy. Scoring in both tests reflects the number and seriousness of errors in reproducing the figure. During the Trail Making Test part-A (TMT-A) participants are asked to trace through 25 numbered dots as fast as possible without lifting their hand, and during part-B (TMT-B) they are asked to switch between numbered dots and letters as fast as possible (e.g. 1,a,2,b, etc.). Seconds to complete each part is recorded. The Judgment of Line Orientation involves matching the orientation and angle of lines in space to 11 lines arranged in a semicircle on a reference card. In WAIS-III Block Design, participants are asked to arrange blocks to match a specific pattern in a limited amount of time. The scoring scheme takes into account both accuracy and speed. For the Benton Visual Retention Test (BVRT), the participants are shown 10 individual designs, each for 10 seconds, and are asked to immediately reproduce each from memory on a plain sheet of paper. The reproductions are scored for number and types of errors made. For the Controlled Oral Word Association (COWA), the participants are asked to recall as many distinct words as possible in one minute that begin with the letters c, f, and s. Scoring takes into account the number of distinct words recalled. For the Rey Auditory Verbal Learning Test (AVLT), the participants hear a list of 15 words and are asked to recall as many as possible. This procedure is repeated five times on the same list of words. After a 30-minute delay the participant is asked to recall as many of the words on the list as possible. Number correct after the delay is used in scoring. For the Grooved Pegboard the participants are asked to place 25 pegs into randomly positioned slots on a board using only one hand at a time. The time it takes to complete the task is scored and average of left and right hand scores are used. For the Useful Field of View test the participants take four subtests that tap visual discrimination and processing speed (Ball et al., 1993; Edwards et al., 2005; Edwards et al., 2006). Subtest score represents the total duration in milliseconds (ms) at which the participant accurately performs on 75% of trials, ranging from 16.67 to 500ms. We used the sum of four subtests in this study.
2.4.2 Data Reduction
The raw scores on the individual tests were transformed to z-scores. Guided by findings from a recent confirmatory factor analytic study (Anderson et al., 2012), the z-scores were first reversed when appropriate so that high scores represented better functioning, (indicated with (R) below) and then averaged to form the following composite scores: speed of processing (Grooved Peg Board (R), TMT-A (R), UFOV (R); average-r = .41), visuospatial construction (CFT-C, Judgment of Line Orientation, Blocks; average-r = .43), memory (BVRT-E (R), COWA, AVLT, CFT-R; average-r = .34). The reversed z-score of TMT-B time to completion was used to capture attentional set shifting, an aspect of executive functioning. Those four scores were used in all bivariate and multivariate analyses.
2.5 Road Test
2.5.1 Procedures and Design
On-road-driving test around Iowa City included both urban and rural routes and was conducted during non-rush hour traffic on days when weather did not lead to poor visibility or road conditions. The test began after a brief acclimation period to the vehicle, and a trained experimenter sat in the front passenger seat to give instructions and operate the dual controls, if needed. The instructions were typical of on-road tests, e.g. ‘turn left at the next lights,’ ‘take the next exit to interstate 380.’ The vehicle is a midsized car with automatic transmission and hidden instrumentation and sensors. Four miniature lipstick-size cameras captured driver behavior (two views) and anterior environment (two views). Participants were asked to complete two navigation-related secondary driving tasks during the road test: route-following and landmark/sign identification. In the route-following task, the participants were asked to memorize a 4-turn route (about 0.6 miles in total distance) while parked and navigated the route immediately after demonstrating successful recall. In the landmark/sign identification task, the participants were asked to identify (i.e. verbally name) the traffic signs on the right side and restaurants on either side of a 1.5 mile suburban commercial strip with speed limit ranging from 30 to 45 miles. The instructions for this task were also given while they were parked at the side of the road before entering this section of the drive. The order of these two navigation tasks was constant across participants. The route-following task took place at the beginning of the drive and landmark/sign identification task took place two thirds of the way through the drive. We refer to sections of the drive when participants were performing these two navigation tasks as ‘on-task’ segments. The remaining sections of the drive, together, constituted the baseline segments of the drive (a total of 13.9 miles) and were interspersed around the two navigation tasks. During the baseline segments of the drive, participants received turn-by-turn instructions typical in on-road tests.
2.5.2 Measures and Data Reduction
The on-task and baseline segments of the drive yielded the three outcome measures for the study: navigation-related secondary task performance, on-task safety errors, and baseline safety errors described next.
2.5.2.1 Navigation-Related Secondary Driving Task Performance
The route-following and landmark/ sign identification tasks each yielded two measures which were used to form a composite score of navigation-related secondary task performance. In route-following, the number of incorrect turns along with whether the participant got lost to the point that they could not take self-corrective action to get back on the route was tallied. The number of self-corrected incorrect turns and number of incorrect turns without self-correction (i.e., participant was lost) were transformed into proportions (each divided by 4) and averaged to form a composite score for route-following performance. Lower scores represented better performance. In landmark/sign identification, the number of restaurants and signs participants identified was divided by the total number of restaurants (13) and signs (16) in this segment of the drive (i.e. transformed into proportions) and averaged to form a composite score for landmark/sign identification performance. High scores represented better performance. Because we were interested in examining overall performance in navigation-related secondary tasks and because performance measures from the two tasks were also moderately intercorrelated, r(153) = −.33, p < .001, we standardized and then averaged both measures (after reversing route-following performance measures) into a composite score of secondary task performance. High scores represented better performance on the secondary tasks.
2.5.2.2 Safety Errors
A certified driving instructor reviewed the videotapes of the drive to score safety errors according to the standards of Iowa Department of Transportation (September 7, 2005 version). This instructor is a separate person from research assistants who administered the drive and evaluated driver performance in the navigation tasks. The driving instructor was not informed about study hypotheses or how we intended to utilize data from separate segments of the drive.
The scoring generated information on frequency and types of safety errors the participants committed. The taxonomy of 76 errors types (e.g., incomplete stop, straddles lane line) is organized into 15 categories (e.g., stop signs, lane observance). Majority of these errors would not be typically observed in brief DMV tests for licensure and only a subgroup would be grounds for failure. In this study only 7 error types were observed in both on-task and baseline segments of the drive for all three groups and were examined both pooling across categories and within categories (see Dawson et al., 2009 for further details on the coding system).
A single reviewer evaluated all drives in this study. To evaluate the reliability of this scoring system, a sample of 30 drives was re-reviewed by this instructor and was independently reviewed by a second driving instructor. For total number of errors per drive, the primary reviewer’s intra-rater correlation was .95, the inter-rater correlation was .73. Absolute agreement between two raters on the 7 common error categories (see Table 1) was excellent, Kappa = .79. In order to quantify driving safety errors during navigation-related secondary tasks, total number of errors committed in route-following and landmark/ sign identification segments were divided by the total of number of miles covered in those segments to form the on-task total safety errors per mile measure. Safety errors during remaining sections of the drive when the participant was not asked to perform any secondary tasks were compiled on a per mile basis to form baseline safety errors measure. The denominators for both of those safety measures were specific to each participant, correcting participant’s relative rank-order for the actual distance traversed (i.e. total miles covered during route-following would be larger for a participant who took incorrect turns and/ or got lost).
Table 1.
Descriptive statistics and p-values associated with mean comparisons among diseased and healthy older adults.
| Control M (SD) |
AD M (SD) |
PD M (SD) |
AD vs. PD a |
Control vs. Diseased |
||
|---|---|---|---|---|---|---|
| Age | 75.4 (4.06) | 77.6 (4.28) | 74.58 (2.58) | .003 | .270 | |
| Educational level | 15.7 (2.8) | 15.25 (3.4) | 15 (2.9) | .936 | .249 | |
| Outcome measures | ||||||
| Secondary Task Performance ↑ | .43 (.73) | −.53 (.71) | −.42 (1.27) | .595 | < .001 | |
| Landmark/Sign identification ↑ | .27 (.76) | −.50 (.69) | −.13 (.62) | .092 | < .001 | |
| Route-following | .04 (.07) | .13 (.13) | .16 (.21) | .631 | < .001 | |
| Safety errors per mile | ||||||
| Baseline safety | 2.03 (.71) | 2.21 (.64) | 2.40 (.82) | .544 | .028 | |
| Lane change | .28 (.15) | .25 (.15) | .26 (.11) | .999 | .266 | |
| Lane observance | .69 (.50) | .96 (.58) | 1.02 (.62) | .927 | .002 | |
| Speed Control | .26 (.19) | .23 (.17) | .31 (.20) | .187 | .851 | |
| Traffic Signs | .10 (.09) | .12 (.10) | .09 (.08) | .286 | .464 | |
| Stop Sign | .26 (.13) | .22 (.11) | .31 (.14) | .012 | .788 | |
| Turns | .27 (.15) | .29 (.13) | .28 (.16) | .968 | .690 | |
| Start & Pull Away from Curb | .07 (.06) | .06 (.07) | .06 (.06) | .944 | .412 | |
| On task safety | 3.63 (1.57) | 4.30 (1.95) | 4.49 (1.81) | .900 | .011 | |
| Lane change | .82 (.80) | .85 (.69) | 1.04 (1.23) | .645 | .405 | |
| Lane observance | .71 (.78) | 1.22 (1.28) | .98 (1.01) | .566 | .017 | |
| Speed Control | .09 (.30) | .13 (.30) | .11(.19) | .970 | .567 | |
| Traffic Signs | .44 (.45) | .30 (.43) | .38 (.42) | .733 | .181 | |
| Stop Sign | .26 (.29) | .24 (.29) | .50 (.44) | .004 | .052 | |
| Turns | .84 (.64) | 1.12 (.76) | 1.49 (.95) | .100 | <.001 | |
| Start & Pull Away from Curb | .01 (.08) | .03 (.12) | .06 (.15) | .299 | .081 | |
| Predictor measures | ||||||
| Visual Sensory Fx ↑ | .26 (.64) | −.29 (.78) | −.27 (.75) | .991 | <.001 | |
| Visuospatial Construction ↑ | .29 (.67) | −.22 (.71) | −.44(.87) | .417 | <.001 | |
| Memory ↑ | .40 (.53) | −.57 (.51) | −.32 (.51) | .163 | <.001 | |
| Speed of processing ↑ | .44 (.47) | −.55 (.61) | −.51 (.87) | .958 | <.001 | |
| Executive Fx: TMT-B seconds | 94.9 (44.1) | 163.3 (67.6) | 162.1 (91.9) | .997 | <.001 | |
Abbrv. Fx= function; TMT-B = Trail Making Test (Part B); AD = Alzheimer’s Disease, PD = Parkinson’s Disease.
The p-values associated with the pairwise mean comparisons among the diseased groups are based on Tukey’s HSD. ↑ Indicates high scores represent better performance.
2.6 Statistical Analyses
The statistical analyses proceeded in four stages. In the first stage, we examined mean differences on demographic, predictor and the outcome measures among healthy elderly, AD and PD groups. In the second stage, we conducted 2X3 mixed design ANOVA to test: 1) whether performance in navigation-related secondary tasks was associated with concurrent increases in safety error rates, on-task safety, compared with safety error rates when participants were not asked to perform any secondary tasks, baseline safety and 2) whether those differences varied as a function of healthy aging, AD or PD status. In the third stage, we examined the bivariate associations of cognitive functioning and driving safety outcome measures. In the fourth stage, we conducted multiple regressions to examine whether different aspects of cognitive functioning predicted each of the three driving outcomes. Model fitting analyses carefully considered influential observations identified by Cook’s D statistics. The substantive inferences did not change when cases with large cook’s D values were removed from the regressions. Hence, the regression output provided in tables includes all cases.
3. Results
3.1 Preliminary Analyses
Table 1 presents descriptive statistics for demographic characteristics, predictor, and outcome measures, including the most common six categories of error types, and the associated p-values for the mean differences among the groups. Table 1 shows that the groups differed significantly on all 3 outcome measures, secondary task performance, baseline safety errors per mile, and on-task safety errors per mile. An examination of specific error types in the baseline and on-task segments of the drive also showed that with the exception of stop sign related errors, majority of differences were between healthy adults and diseased groups rather than between AD and PD participants. This pattern was also true for the specific measures of performance in the landmark/sign identification and route-following tasks. Not surprisingly, the groups also differed on all predictor measures. In all cases, the mean differences indicated that healthy adults performed better than diseased adults on driving measures, on cognitive functioning and visual sensory functioning.
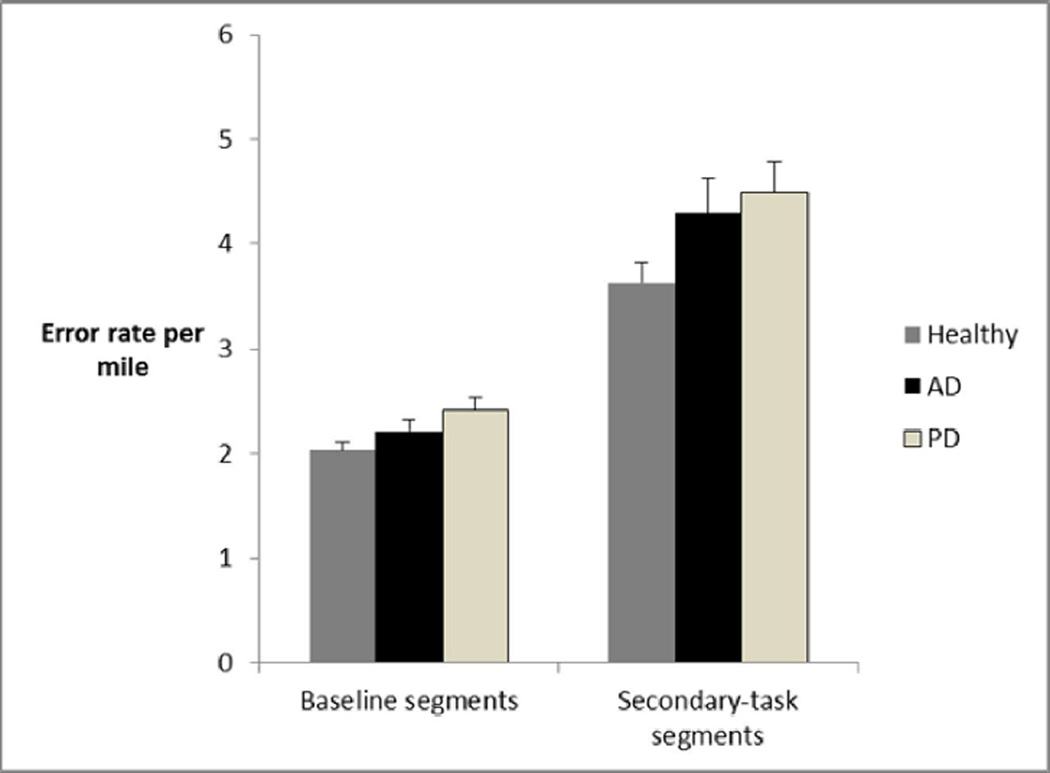
3.2 Navigation-related secondary task performance and its relevance to safety
We tested whether performance in navigation-related secondary tasks was associated with concurrent increases in safety error rates, on-task safety, compared with safety error rates when participants were not asked to perform any secondary tasks, baseline safety. We addressed this question with a 2×3 mixed design ANOVA on safety errors per mile, with segment of the drive (on-task vs. baseline) being the within-subject factor and three groups of drivers (AD, PD, and controls) being the between-subject factor. The results showed a main effect of task-status, F(1,132) = 180.06, p < .001, main effect of disease group, F(2, 132) = 4.49, p < .05, but no interaction effect between task-status and disease group, F(2,132) = 1.63, ns. There were no significant pairwise differences between the diseased groups suggesting the absence of a strong disease-specific pattern in driving performance measured in this study. Consistent with the means in shown in Table 1, those analyses indicate that the navigation-related tasks increase errors per mile compared to baseline sections of the drive for all three groups. This evidence supports our hypothesis that secondary navigation tasks affect concurrent safety for both healthy and diseased adults. Figure 1 depicts those means and associated standard errors.
Figure 1.
Means and standard errors of safety errors per mile during baseline (baseline safety errors) and secondary-task segments (on-task safety errors) of the drive for each of the three groups.
Top portion of Table 2 shows the correlations among safety errors per mile during baseline and on-task sections of the drive, and navigation-related secondary task performance. As shown in Table 2, both measures of safety errors were significantly correlated. In addition, the correlation between navigation-related secondary task performance and baseline safety error rates was significant. The results also show that performance in these driving tasks essential to navigation is meaningfully but only modestly related to baseline driver safety.
Table 2.
Bivariate correlations with associated p-values (in parentheses) among the predictors and the outcomes.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Baseline safety errors | ||||||||
| 2. On-task safety errors | .454 (.000) |
|||||||
| 3. Secondary Task Performance | −.213 (.013) |
−.134 (.121) |
||||||
| 4. Age | .112 (.193) |
.057 (.511) |
−.192 (.020) |
|||||
| 5. Visual Sensory functioning | −.183 (.033) |
−.160 (.064) |
.488 (.000) |
−.246 (.003) |
||||
| 6. Speed of processing | −.262 (.002) |
−.278 (.001) |
.621 (.000) |
−.222 (.007) |
.511 (.000) |
|||
| 7. Memory | −.267 (.002) |
−.124 (.152) |
.577 (.000) |
−.043 (.602) |
.279 (.001) |
.578 (.000) |
||
| 8. Trail Making B (Set shifting) | .236 (.006) |
.107 (.221 |
−.671 (.000) |
.220 (.008) |
−.397 (.000) |
−.751 (.000) |
−.638 (.000) |
|
| 9. Visuospatial Construction | −.369 (.000) |
−.145 (.094) |
.488 (.000) |
−.046 (.581) |
.352 (.000) |
.510 (.000) |
.605 (.000) |
−.511 (.000) |
Note. N’s vary from 135 to 148.
3.4 Unique predictive associations among cognitive functioning and distinct facets of driving safety
Table 2 also presents the intercorrelations among composite cognitive measures and age with navigation-related secondary task performance, on-task safety errors, and baseline safety errors. Out of 12 correlations among outcome measures and cognitive functioning 11 were significant at p < .05 level or better. Furthermore, correlations among dimensions of cognitive functioning were generally strong. Basic visual sensory functioning and all dimensions of cognitive functioning showed fair to moderate associations with the outcomes. This pattern of bivariate correlations supports the importance of instituting statistical controls in examining the unique patterns of prediction from cognitive functioning to various driving safety outcomes.
In order to examine the unique predictive power of cognitive functioning in the four domains of focus to driving outcomes we examined a series of hierarchical regressions. Because all univariate analyses showed that most of the differences were between controls and diseased groups rather than among disease groups, diseased groups were pooled together in the regressions. All regressions controlled for age, visual sensory functioning and subject’s disease status (dummy variable contrasting diseased versus healthy (reference)) in the first step, before examining the unique predictive power cognitive functioning. Furthermore, in each regression we sought to isolate variability in the specific outcome measure by controlling for extraneous performance metrics in that regression framework. For example, in predicting on-task errors per mile, we controlled for navigation-related secondary task performance and safety errors per mile during baseline sections. In predicting navigation-related secondary task performance, we controlled for participant’s on-task safety errors per mile. Those controls permitted us to isolate variability associated with dual-task performance costs. Finally, we examined interaction of disease status with cognitive functioning outcomes. If some aspects of cognitive functioning are more predictive of driving safety than others in diseased populations compared to healthy aging adults, significant interactions would uncover that. Because no a priori expectations were set for these interactions and to preserve statistical power for tests of main effects, four two-way interaction terms were entered with forward selection algorithm in step-3 of regressions. In none of the regressions the interaction effects emerged as significant terms. The results of the three regressions are presented in Tables 3, 4, and 5.
Table 3.
Final regression equation predicting baseline safety errors per mile from demographic and cognitive variables.
| Predictors | Std Beta | p-value |
|---|---|---|
| Age | .097 | .258 |
| Disease status | −.010 | .935 |
| Visual Sensory functioning | .019 | .848 |
| Speed of processing | −.097 | .524 |
| Memory | −.049 | .708 |
| Visuospatial construction | −.311 | .005 |
| TMT-B (Set shifting) | −.055 | .693 |
The overall F for the regressions were as follows: for baseline safety errors F(7,126) = 3.34, p < .005. When the 7 cases that took on Cook’s D statistics >=.035 in the current sample were removed from the regressions above, the substantive inferences were not changed.
Table 4.
Final regression equation predicting on-task safety errors from demographic and cognitive variables
| Predictors | Std Beta | p-value |
|---|---|---|
| Baseline safety errors | .454 | .000 |
| Secondary Task Performance | −.006 | .959 |
| Age | −.031 | .702 |
| Disease status | .108 | .322 |
| Visual Sensory functioning | −.004 | .963 |
| Speed of processing | −.344 | .016 |
| Memory | .099 | .423 |
| Visuospatial construction | .091 | .390 |
| MT-B (Set shifting) | −.206 | .128 |
The overall F for the regressions were as follows: for baseline safety errors F(9,123) = 5.34, p < .001. When the 6 cases that took on Cook’s D statistics >.035 in the current sample were removed from the regressions above, the substantive inferences were not changed.
Table 5.
Final regression equation predicting secondary task performance from demographic and cognitive variables.
| Predictors | Std Beta | p-value |
|---|---|---|
| On-task errors | −.008 | .906 |
| Age | −.058 | .362 |
| Disease status | −.103 | .229 |
| Visual Sensory functioning | .194 | .008 |
| Speed of processing | −.036 | .754 |
| Memory | .208 | .031 |
| Visuospatial construction | .084 | .292 |
| TMT-B (Set shifting) | −.370 | .000 |
Note. The overall F for the regressions were as follows: for baseline safety errors F(8,124) = 19.14, p < 4 .001. When the 6 cases that took on Cook’s D statistics >.035 in the current sample were removed from the regressions above, the substantive inferences were not changed.
Table 3 shows that only visuospatial construction predicted baseline safety errors per mile. Higher functioning in visuospatial construction predicted fewer errors in the baseline segments of the drive controlling for other aspects of cognitive functioning and age. None of the two-way interactions of disease status with cognitive functioning were significant. The total r-square was .16.
Table 4 shows that only speed of processing predicted on-task safety errors after accounting for significant effects of secondary task performance and baseline safety error rates. Higher functioning in processing speed tests predicted lower error rates during the navigation or on-task segments of the drive controlling for other aspects of cognitive functioning, age, and disease status. None of the two-way interactions of disease status with cognitive functioning were significant. The total r-square was .23.
Table 5 shows the final regression equation for navigation-related secondary task performance controlling for concurrent on-task safety errors. Visual sensory functioning, memory and set shifting predicted performance in this outcome measure over and above age and disease status. None of the two-way interactions of disease status with cognitive functioning were significant. The total r-square was .55.
Although bivariate correlations had indicated significant associations among cognitive measures and all three driving outcomes, different dimensions of cognitive functioning emerged as significant predictors for the three outcomes in multivariate analyses. Specifically, visuospatial construction predicted baseline safety, speed of processing rather than set shifting predicted on-task errors per mile, and both memory and set-shifting predicted navigation-related secondary task performance. Findings showed that visual sensory functioning only remained a significant predictor of navigation-related secondary task performance. Furthermore, neither age nor disease status remained significant predictors of the outcome measures in the final regressions.
4. Discussion
To capture older drivers’ on-road safety risk, we quantified multiple facets of drivers’ on-road performance, including performance in secondary navigation tasks intrinsic to driving such as route-following and identifying signs and landmarks, as well as their baseline and on-task safety errors. We assessed the extent to which performance in those basic navigation tasks adversely affected concurrent driving safety, whether navigation ability per se predicted baseline safety, and whether distinct aspects of cognitive functioning predicted multiple facets of driver performance over and above disease status, age, and basic visual sensory function.
The findings showed that drivers with and without neurological diseases made more safety errors while concurrently performing secondary navigation tasks compared to baseline driving when they were not performing secondary tasks. It is possible the increase in errors during navigation task segments compared to baseline segments reflect differences in road cultures. While both segments of the drive included residential and city driving, baseline segments also included high-way driving. This is a limitation of our design and measures. Nevertheless, others have shown that drivers tend to make more errors while self-navigating compared to following turn-by-turn instructions of test administrators (Wood et al., 2009). Hence, we are relatively confident that the driving tasks such navigating a brief route immediately following instructions and identifying signs and landmarks along a familiar route, were challenging enough to adversely affect safety. Navigation performance itself was associated with baseline safety, albeit modestly, indicating these secondary tasks bear on drivers’ on-road safety risk.
Even though all four domains of cognitive functioning, speed of processing, set shifting, visuospatial construction, and memory showed moderately significant bivariate associations with navigation performance, only memory and set-shifting remained significant predictors in multivariate analyses. The positive prediction for memory provides empirical support to the clinical practice of recommending driving curtailment or cessation of driving when older drivers struggle with navigation in familiar areas. Overall, these findings suggest secondary navigation tasks that are essential to driving and perhaps why we drive at all, provide added value to on-road testing of older drivers.
Results in this study replicated and extended results from earlier reports that older adults with neurological diseases are generally less safe drivers than those without such diseases (Duchek, et al., 2003; Fitten, et al., 1995; Heikkila et al., 1998; Hunt et al., 1997; Iverson, et al., 2010; Reger et al., 2004; Uc, et al., 2011; Uc, et al., 2009; Wood, et al., 2005). Drivers with neurological diseases made more safety errors particularly during navigation, and tended to perform worse across the board on the outcome side. The only error type to show disease specificity was stop sign errors. PD patients committed more of these errors in both baseline and secondary task segments compared to AD patients. Although PD was initially considered predominantly as a motor disease, it is now well-understood that cognitive dysfunction affects a large proportion of patients with eventual progression to dementia (Uc et al., 2009b). Hence it is not surprising that comparisons on the predictor side also did not indicate that differences in composite measures of cognitive functioning between AD and PD patients. Collectively, those findings suggest deficits are not disease-specific early in the course of these neurodegenerative diseases (after all our participants had to be active drivers with valid driver’s licenses and hence relatively well-functioning). It is possible driving related deficits become more disease-specific as neurodegeneration advances, and with larger sample sizes disease-specificity in error patterns would become evident.
Importantly, multivariate analyses did not disclose disease status as a significant predictor of driving outcome measures once cognitive functioning was added to the models and it did not interact with cognitive functioning to predict the driving outcomes. This evidence provides empirical validation to the clinical experience that age and disease status alone fail to inform clinical decisions regarding a patient’s fitness to drive, and that cognitive functioning must be considered in evaluating patients’ driving risk (Rizzo, 2011). This is because considerable variability in cognitive functioning exists early in the course of these diseases and once that variability is taken into account disease status or age show limited utility in predicting safety risk.
The bivariate associations of basic visual sensory functioning and all four dimensions of cognitive functioning were generally fair to moderate in magnitude for baseline and on-task safety errors, while the correlations were consistently moderate for secondary task performance. In multivariate analyses, different dimensions of cognitive functioning emerged as significant predictors of multiple facets of older drivers’ on-road safety risk. Visuospatial construction predicted baseline safety, speed of processing predicted performance costs in on-task errors, and memory and set-shifting predicted navigation-related secondary task performance. Those findings provide empirical support to previous research practices in applied settings such as DMV or clinics that chose to broadly sample functioning in multiple domains of cognition rather than narrowly sampling a single domain (Anderson et al., 2012; Ball et al., 2006).
TMT-Part B, typically assumed to reflect set shifting, an aspect of executive functioning, did not predict on-task safety errors but predicted navigation performance. In contrast, speed of processing predicted safety errors but not navigation performance. This finding suggests that performance costs to the primary goal of safety are best explained by speed of processing rather than executive functioning. This interpretation would be consistent with the view of Salthouse and others (Salthouse & Miles, 2002; Salthouse et al., 2003; Verhaeghen, 2011). A weakness in our design was reliance on a single task, TMT-B, to measure executive function. Findings from recent confirmatory factor analytic studies suggest that TMT-Part B coheres with speed of processing tests more readily than with tests of executive function (Salthouse 2011a, 2011b). Future driving studies would benefit from more robust assessments of executive functioning to better understand its multifaceted role in driver performance and safety. Wisconsin card-sort and Stroop are possible additional executive function tests that are readily available at neuropsychological clinics for more robust assessments of cognitive function in this respect.
4.1 Conclusions and future directions
Our findings showed that AD and PD patients do not show highly distinct patterns of declines in driving safety early in the course of their disease but perform worse than healthy elderly across the board. More importantly, the findings showed that all four domains of cognitive functioning, including speed of processing, visuospatial construction, set shifting, and memory predicted different facets of older drivers’ on-road safety risk, over and above age, basic visual sensory functioning, and disease status. Current findings support recommendations from previous research that screening tests in applied settings such as DMV and clinics should broadly sample functioning in multiple domains of cognition rather than narrowly sampling a single domain (Anderson et al., 2012; Ball et al., 2006). The findings also inform design of future on-road tests which are generally designed with the fitness of novice drivers in mind. Including navigation-tasks common to driving in on-road tests may help increase the utility and sensitivity of these tests to distinguish safe from unsafe older drivers, and may inform graduated restrictions in licensing for those who do not appropriately self-regulate or self-restrict driving (Molnar, Eby, Charlton, Langford, Koppel, Marshall & Man-Son-Hing, 2013).
Acknowledgements
The authors would like to thank the entire Neuroergonomics research team and all participants in the study.
Conflict of interest: The work is a product of employment and affiliation for all authors. This study was supported by Awards AG 17717 and AG 15071 from the National Institute on Aging, Award NS 44930 from the National Institute of Neurological Disorders and Stroke. In addition, awards from Toyota Motor Company and Award HL 091917 from NHLBI provided salary support to the authors during the analysis and write-up of the manuscript.
Sponsor’s Role: This study was made possible by grants from NIH. Other than providing budget support for the conduct of this research, it had no role in design, methods, subject recruitment, data collection, analysis, or preparation of the paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The sample of 345 in the Anderson et al. (2012) study included all participants older than 50 years of age. The sample of 148 in the current study is based on the subsample of cases that were 70 years of age or older. The total number of errors from the entire drive constituted the only driving safety outcome measure in Anderson et al., 2012, which were not used in the current study.
References
- Aksan N, Anderson SW, Dawson J, Uc E, Johnson AJ, Rizzo M. Cognitive functioning predicts driver safety on road-tests one and two-years later. Journal of American Geriatric Society. 2012;60:99–105. doi: 10.1111/j.1532-5415.2011.03739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aksan N, Dawson JD, Emerson J, Yu, Lixi UcEY, Anderson S, Rizzo M. Naturalistic distraction during search for roadside targets and driving safety in older drivers. Human Factors. 2013;55:841–853. doi: 10.1177/0018720812465769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson S, Aksan N, Dawson J, Uc E, Johnson A, Rizzo M. Neuropsychological assessment of driving safety risk in older adults with and without neurologic disease. Journal of Clinical and Experimental Neuropsychology. 2012;34:895–905. doi: 10.1080/13803395.2011.630654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anstey KJ, Wood J, Lord S, Walker JG. Cognitive, sensory and physical factors enabling driver safety in older adults. Clinical Psychology Review. 2005;25:45–65. doi: 10.1016/j.cpr.2004.07.008. [DOI] [PubMed] [Google Scholar]
- Anstey KJ, Woods J. Chronological Age and Age-Related Cognitive Deficits Are Associated With an Increase in Multiple Types of Driving Errors in Late Life. Neurospychology. 2011;25:613–621. doi: 10.1037/a0023835. [DOI] [PubMed] [Google Scholar]
- Ball K, Roenker SL, Wadley VG, Edwards JD, Roth DL, McGwin G, Jr, Raleigh R, Joyce JJ, Cissell GM, Dube T. Can high-risk older drivers be identified through performance-based measures in a department of motor vehicles setting? Journal American Geriatric Society. 2006;54:77–84. doi: 10.1111/j.1532-5415.2005.00568.x. [DOI] [PubMed] [Google Scholar]
- Ball KK, Owsley C, Stalvey B, Roenker DL, Sloane ME, Graves M. Driving avoidance and functional impairment in older adults. Accident Analysis and Prevention. 1998;30:313–322. doi: 10.1016/s0001-4575(97)00102-4. [DOI] [PubMed] [Google Scholar]
- Ball K, Owsley C, Sloane ME, Roenker DL, Bruni JR. Visual attention problems as a predictor of vehicle crashes in older drivers. Investigations in Ophthalmology and Visual Sciences. 1993;34:3110–3123. [PubMed] [Google Scholar]
- Benton AL, Hamsher K, Varney NR, et al. Contributions to Neuropsychological Assessment. New York: Oxford University Press; 1983. [Google Scholar]
- Clay OJ, Wadley VG, Edwards JD, Roth DL, Roenker DL, Ball KK. Cumulative meta-analysis of the relationship between useful field of view and driving performance in older adults: Current and future implications. Optometry and Vision Science. 2005;82:724–731. doi: 10.1097/01.opx.0000175009.08626.65. [DOI] [PubMed] [Google Scholar]
- Dawson JD, Anderson SW, Uc EY, Dastrup E, Rizzo M. Predictors of driving safety in early Alzheimer disease. Neurology. 2009;72:521–527. doi: 10.1212/01.wnl.0000341931.35870.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson JD, Anderson SW, Uc EY, Dastrup E, Rizzo M. Ascertainment of on-road safety errors based on video review. Proceedings of the Fifth International Driving Symposium on Human Factors in Driver Assessment, Training, and Vehicle Design; 2009. pp. 419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson JD, Uc EY, Anderson SW, Johnson AM, Rizzo M. Neuropsychological predictors of driving errors in older adults. Journal American Geriatric Society. 2010;58:1090–1096. doi: 10.1111/j.1532-5415.2010.02872.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duchek JM, Carr DB, Hunt L, Roe CM, Xiong C, Shah K, Morris JC. Longitudinal driving performance in early-stage dementia of the Alzheimer type. Journal American Geriatric Society. 2003;51:1342–1347. doi: 10.1046/j.1532-5415.2003.51481.x. [DOI] [PubMed] [Google Scholar]
- Edwards JD, Vance DE, Wadley VG, Cissell GM, Roenker DL, Ball KK. The reliability and validity of the Useful Field of View as administered by personal computer. Journal of Clinical Experimental Neuropsychology. 2005;27:529–543. doi: 10.1080/13803390490515432. [DOI] [PubMed] [Google Scholar]
- Edwards JD, Myers C, Ross LA, Roenker DL, Cissell GM, McLaughlin AM, Ball KK. The longitudinal impact of cognitive speed of processing training on driving mobility. Gerontologist. 2009;49:485–494. doi: 10.1093/geront/gnp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards JD, Ross LA, Wadley VG, Clay OJ, Crowe M, Roenker DL, Ball KK. The useful field of view test: Normative data for older adults. Archives of Clinical Neuropsychology. 2006;21:275–286. doi: 10.1016/j.acn.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Evans L. Risks older drivers face themselves and threats they pose to other road users. International Journal of Epidemiology. 2000;29:315–322. doi: 10.1093/ije/29.2.315. [DOI] [PubMed] [Google Scholar]
- Ferris FL, III, Kassoff A, Bresnick GH, Baily I. New visual acuity charts for clinical research. American Journal of Ophthamology. 1982;94:91–96. [PubMed] [Google Scholar]
- Fitten LJ, Perryman KM, Wilkinson CJ, Little RJ, Burns MM, Pachana NA, Mervis JR, Malmgren R, Siembieda DW, Ganzell S. Alzheimer and vascular dementias and driving: a prospective road and laboratory study. Journal of American Medical Association. 1995;273:1360–1365. [PubMed] [Google Scholar]
- Gibb WR, Lees AJ. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. Journal of Neurology, Neurosurgery, Psychiatry. 1988;51:745–52. doi: 10.1136/jnnp.51.6.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golledge RG. Human wayfinding and cognitive maps. In: Golledge RG, editor. Wayfinding behaviour: Cognitive mapping and other spatial processes. Baltimore, MD: John Hopkins Press; 1999. pp. 5–45. [Google Scholar]
- Heikkila VM, Turkka J, Korpelainen J, Kallanranta T, Summala H. Decreased driving ability in people with Parkinson's disease. Journal of Neurology, Neurosurgery and Psychiatry. 1998;64:325–330. doi: 10.1136/jnnp.64.3.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzer R, Stern Y, Rakitin BC. Predicting age-related dual-task effects with individual differences on neuropsychological tests. Neuropsychology. 2005;19:18–27. doi: 10.1037/0894-4105.19.1.18. [DOI] [PubMed] [Google Scholar]
- Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. Journal of Neurology, Neurosurgery, Psychiatry. 1992;55:181–184. doi: 10.1136/jnnp.55.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt LA, Murphy CF, Carr D, Duchek JM, Buckles V, Morris JC. Reliability of the Washington University Road Test. A performance based assessment for drivers with dementia of the Alzheimer type. Archives of Neurology. 1997;54:707–712. doi: 10.1001/archneur.1997.00550180029008. [DOI] [PubMed] [Google Scholar]
- Insurance Institute Highway Safety. 2014 Mar; http://www.iihs.org/iihs/topics/t/older-drivers/qanda.
- Iverson DJ, Gronseth G, Reger MA, Classen S, Dubinsky RM, Rizzo M. Practice Parameter update: Evaluation and management of driving risk in aging and in dementia evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74:1–10. doi: 10.1212/WNL.0b013e3181da3b0f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer AF, Hahn S, Gopher D. Task coordination and aging: explorations of executive control processes in the task switching paradigm. Acta Psychologica. 1999;101:339–378. doi: 10.1016/s0001-6918(99)00011-6. [DOI] [PubMed] [Google Scholar]
- Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4th ed. New York: Oxford University Press; 2004. [Google Scholar]
- Lyman S, Ferguson SA, Braver ER, Williams AF. Older driver involvements in police reported crashes and fatal crashes: Trends and projections. Injury Prevention. 2002;8:116–120. doi: 10.1136/ip.8.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marottolli RA, Mendes LCF, Glass TA, Williams CS, Cooney LM, Berkman LF, Tinetti ME. Driving cessation and increased depressive symptoms: prospective evidence from the New Haven EPESE. Established Populations for Epidemiologic Studies of the Elderly. Journal of American Geriatric Society. 1997;45:202–206. doi: 10.1111/j.1532-5415.1997.tb04508.x. [DOI] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- Molnar LJ, Eby DW, Charlton JL, Langford J, Koppel S, Marshall S, Man-Son-Hing M. Reprint of “Driving avoidance by older adults: Is it always self-regulation?”. Accident Analysis and Prevention. 2013;61:272–280. doi: 10.1016/j.aap.2013.07.004. [DOI] [PubMed] [Google Scholar]
- Owsley C, Ball K, McGwin G, Jr, Sloane ME, Roenker DL, White MF, Overley ET. Visual processing impairment and risk of motor vehicle crash among older adults. Journal of the American Medical Association. 1998;279:1083–1088. doi: 10.1001/jama.279.14.1083. [DOI] [PubMed] [Google Scholar]
- Pelli DG, Robson JG, Wilkins AJ. The design of a new letter chart for measuring contrast sensitivity. Clinical Vision Sciences. 1988;2:187–199. [Google Scholar]
- Reger MA, Welsh RK, Watson GS, Cholerton B, Baker LD, Craft S. The relationship between neuropsychological functioning and driving ability in dementia: A metaanalysis. Neuropsychology. 2004;18:85–93. doi: 10.1037/0894-4105.18.1.85. [DOI] [PubMed] [Google Scholar]
- Rizzo M. Impaired driving from medical conditions: A 70-year-old man trying to decide he should continue driving. Journal of the American Medical Association. 2011;305:1018–1026. doi: 10.1001/jama.2011.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LA, Clay O, Edwards JD, Ball K, Wadley V, Vance D, et al. Do older drivers at-risk for crashes modify their driving over time? Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64B:163–170. doi: 10.1093/geronb/gbn034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse TA. The processing-speed theory of adult age differences in cognition. Psychological Review. 1996;103:403–428. doi: 10.1037/0033-295x.103.3.403. [DOI] [PubMed] [Google Scholar]
- Salthouse TA. Cognitive correlates of cross-sectional differences and longitudinal changes in trail making performance. Journal of Clinical and Experimental Neuropsychology. 2011a;33:242–248. doi: 10.1080/13803395.2010.509922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse TA. What cognitive abilities are involved in trial-making performance? Intelligence. 2011b;39:222–232. doi: 10.1016/j.intell.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salthouse TA, Miles JD. Aging and time-sharing aspects of executive control. Memory & Cognition. 2002;30:572–582. doi: 10.3758/bf03194958. [DOI] [PubMed] [Google Scholar]
- Salthouse TA, Atkinson TM, Berish DE. Executive functioning as a potential mediator of age-related cognitive decline in normal adults. Journal of Experimental Psychology: General. 2003;132:566–594. doi: 10.1037/0096-3445.132.4.566. [DOI] [PubMed] [Google Scholar]
- Sims RV, McGwin G, Allman RM, Ball KK, Owsley C. Exploratory study of incident vehicle crashes among older drivers. Journal of Gerontological Society-A: Biological Sciences and Medical Sciences. 2000;55:M22–M27. doi: 10.1093/gerona/55.1.m22. [DOI] [PubMed] [Google Scholar]
- Strauss E, Sherman EMS, Spreen OA. Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. 3rd Ed. New York: Oxford University Press; 2006. [Google Scholar]
- Uc EY, Rizzo M, Johnson AM, Emerson JL, Liu D, Mills ED, Anderson SW, Dawson JD. Real-life driving outcomes in Parkinson Disease. Neurology. 2011;76:1894–1902. doi: 10.1212/WNL.0b013e31821d74fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uc EY, Rizzo M, Johnson AM, Dastrup E, Anderson SW, Dawson JD. Road safety in drivers with Parkinson disease. Neurology. 2009a;73:2112–2119. doi: 10.1212/WNL.0b013e3181c67b77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uc E, McDermott M, Marder K, Anderson S, Litvan I, Como P, Auinger P, Chou K, Growdon P. Incidence of and risk factors for cognitive impairment in an early Parkinson disease clinical trial cohort. Neurology. 2009b;73:1469–1477. doi: 10.1212/WNL.0b013e3181bf992f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uc EY, Rizzo M, Anderson SW, Shi Q, Dawson JD. Driver route-following and safety errors in early Alzheimer s Disease. Neurology. 2004;73:832–837. doi: 10.1212/01.wnl.0000139301.01177.35. [DOI] [PubMed] [Google Scholar]
- Uc EY, Rizzo M, Anderson SW, Shi Q, Dawson JD. Driver landmark and traffic sign identification in early Alzheimer’s disease. Journal of Neurology, Neurosurgery, and Psychiatry. 2005;76:764–768. doi: 10.1136/jnnp.2004.049338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uc EY, Rizzo M, Anderson SW, Sparks JD, Rodnitzky RL, Dawson JD. Impaired visual search in drivers with Parkinson’s disease. Annals of Neurology. 2006;60:407–413. doi: 10.1002/ana.20958. [DOI] [PubMed] [Google Scholar]
- Uc EY, Rizzo M, Anderson SW, Sparks JD, Rodnitzky RL, Dawson JD. Impaired navigation in drivers with Parkinson’s disease. Brain. 2007;130:2433–2440. doi: 10.1093/brain/awm178. [DOI] [PubMed] [Google Scholar]
- Verhaeghen P. Aging and executive control: Reports of a demise greatly exaggerated. Current Directions in Psychological Science. 2011;20:174–180. doi: 10.1177/0963721411408772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windsor TD, Anstey KJ, Butterworth P, Luszcz MA, Andrews GA. The role perceived control in explaining depressive symptoms associated with driving cessation in longitudinal study. The Gerontologist. 2007;47:215–223. doi: 10.1093/geront/47.2.215. [DOI] [PubMed] [Google Scholar]
- Wood JM, Worringham C, Kerr G, Mallon K, Silburn P. Quantitative assessment of driving performance in Parkinson’s disease. Journal of Neurology, Neurosurgery, Psychiatry. 2005;76:176–180. doi: 10.1136/jnnp.2004.047118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JM, Anstey KJ, Kerr GK, Lacherez PF, Lord S. A multidomain for predicting older driver safety under in-traffic road conditions. Journal of the American Geriatrics Society. 2008;56:986–993. doi: 10.1111/j.1532-5415.2008.01709.x. [DOI] [PubMed] [Google Scholar]
- Wood JM, Anstey KJ, Lacherez PF, Kerr GK, Mallon K, Lord SR. on-road difficulties of older drivers and their relationship with self-reported motor crashes. Journal of the American Geriatric Society. 2009;57:2062–2069. doi: 10.1111/j.1532-5415.2009.02498.x. [DOI] [PubMed] [Google Scholar]