Abstract
Purpose
Despite the high prevalence and impact of distal radius fractures (DRFs) on older patients, the current available literature regarding DRFs in older adults lacks adequate comparative treatment data. The purpose of this prospective, controlled outcomes study is to compare outcomes using the volar locking plating system (VLPS) for DRFs in both older and younger adults.
Methods
Consecutive, eligible patients were enrolled into our prospective study over a two-year period on the basis of strict inclusion/exclusion criteria. Subjects were entered into two cohorts based on age: 20–40 years and ≥ 60 years. Patient outcomes and complication rates were evaluated at three, six and twelve months after surgery. Outcome measures included the Michigan Hand Outcomes Questionnaire (MHQ), grip strength, active wrist and forearm range of motion, the Jebsen-Taylor test, and radiographic parameters.
Results
55 patients (30 young and 25 older adults) with unilateral, inadequately reduced DRFs were enrolled and received surgical treatment with the VLPS. We observed no statistically significant difference in any of the outcomes for all three follow-up periods. While older age patients continued to improve throughout their twelve month postoperative visits, younger patients achieved their maximum recovery during the six month follow-up period, suggesting different recovery patterns. At the twelve-month assessment, older patients were able to achieve a higher mean MHQ score than their younger counterparts (normalized mean: 85% and 82%, respectively). Complication rates were similar between the two groups for all three time periods, with most occurring on or before the three month postoperative visit.
Conclusions
This study indicates that the VLPS is successful in managing DRFs in older patients and without increased complications compared to younger patients. For the older patients without prohibitive surgical risks, internal fixation using the VLPS yields comparable outcomes to younger patients.
Level of Evidence
Level II prospective comparative study
Keywords: Distal Radius Fracture, Elderly, the Michigan Hand Outcomes Questionnaire, Outcomes, Volar Locking Plating System
Introduction
Distal radius fractures (DRFs) represent the second most common type of fracture among patients over 60 years, incurring substantial functional and socioeconomic consequences.1–3 As the current baby-boom population matures, the incidence of geriatric DRFs is expected to escalate along with the aging population.4 Furthermore, it has been suggested that trends in the rising activity levels of people greater than 60 years have increased the frequency of DRFs among this population and also affected the expectations of older patients regarding functional treatment outcomes.5–7 However, despite the high prevalence and great impact of DRFs on older patients, the current available literature lacks adequate comparative data to guide treatment for this patient population. While current literature uniformly supports strict anatomic reduction in younger patients to enhance outcomes, evidence examining this relationship in older adults remains unproven.6,8–20 Thus, the optimal treatment for DRFs in older adults continues to be controversial.
Traditional management of DRFs in older patients has generally consisted of conservative, less invasive methods, such as closed reduction and casting or external fixation.19Such treatment is based on the historical paradigm that patients over the age of 60 years do not require precise anatomical reduction because of their decreased functional demands and concerns regarding the stability of internal fixation implants in the osteoporotic bone of older adults.18,21 Several recent studies from Scotland, Canada, and the US remain supportive of these conservative measures, arguing that the majority of older adults are not good surgical candidates and that older patients are able to achieve good outcomes despite marked radiographic deformity.13–16
However, recent advances of anatomically designed fixed-angle implants, including the volar locking plating system (VLPS), and the increased activity and independence of persons over the age of 60 have caused some physicians to propose a paradigm change regarding how DRFs in older adults should be treated.6,9,16–17,19–20 Instead of conservative, less stringent reduction methods, these surgeons advocate rigid internal fixation techniques to expedite recovery among older-age adults and return them to independent living. We found three retrospective case series analyzing the results of open reduction and internal fixation (ORIF) in older adults all with very promising results in favor of this approach.6,17,19 While the results of these studies are encouraging, they remain preliminary and relatively inconclusive; the validity of these studies were hampered by their retrospective study designs, small, uncontrolled sample sizes, and limited statistical analyses.
To date, hand surgeons still have insufficient knowledge regarding the effectiveness and safety of surgical techniques in older adults. The present study undertakes a prospective, controlled trial assessing DRF outcomes in an older sample to compare with a younger sample using the VLPS. The specific aims are: (1) to comparatively assess the radiographic changes, functional recovery, and patient-based outcomes in both older and young DRF patients; (2) to determine the complication rate in each sample and identify any significant differences; and, (3) to conduct a multivariable statistical analysis and evaluate the rate of recovery using VLPS in patients over 60 years and younger patients. We hypothesize that younger patients will experience better outcomes than older patients.
Materials and Methods
Eligible consecutive patients with inadequately reduced unilateral DRFs and persistent deformity after unsuccessful closed reduction were recruited as part of a larger study analyzing the VLPS in DRFs.9 Enrolled patients were assigned to one of two cohorts: (1) patients ≥ 60 years, and (2) patients 20–40 years. All patients underwent open reduction and internal fixation with the use of the Distal Volar Radius (DVR) system (Hand Innovations, Miami, Fl), according to the previously published technique by Orbay and Fernandez.6,20,22 Patient inclusion in our study required appropriate age (20–40years; ≥ 60 years), the ability to read and understand English, and one or more of the following surgical indication criteria for unacceptable closed reduction: dorsal/volar tilt angle greater than −10°, radial inclination angle less than 15°, radial height less than 10mm, and/or intra-articular step-off of ≥ 2mm. We excluded patients with open fractures as well as patients with confounding factors, such as concomitant wrist and/or upper-extremity injuries (i.e., injury to wrist ligaments or distal radio-ulnar joint instability), patients with systemic, multi-organ, or head injuries, patients treated more than 2 weeks after the initial injury, and patients with bilateral fractures.
Postoperatively, wrists were immobilized in volar plaster wrist splints. Patients were then fitted with removable Orthoplast splints to protect their injured wrists. The total splinting time was six weeks and no rigid casting was required. Within one week of surgery, all patients began a six-week structured hand therapy program with formal sessions two to three days per week plus a home exercise program. The program included active and passive finger range of motion, hand and wrist edema control, and active wrist motion exercises. One week after fixation with the VLPS, patients were allowed to return to their activities of daily living while wearing the splints. Strengthening exercises were initiated six weeks after the surgical procedure.
Outcomes Evaluations
All fractures were categorized according to the previously established AO classification system.23 Patient outcomes and complications were evaluated at three, six, and twelve months after surgery. At each postoperative visit, a comprehensive multi-modality outcomes assessment was performed, including both patient-rated and objective functional measures.
The primary outcome for our study was the overall score for the Michigan Hand Outcomes Questionnaire (MHQ), a validated method for measuring patient-rated hand performance.24–25 The MHQ assessment tool includes evaluation of overall function, activities of daily living, work, pain, aesthetics, and patient satisfaction. Additional functional outcomes included radiographic data (including articular step-off and gap), other well established tools for measuring hand function (Jebsen-Taylor test and grip strength), and postoperative active wrist and forearm range of motion (ROM) measurements (flexion + extension, pronation, and supination).26–27 The writing portion of the Jebsen-Taylor test was excluded from our assessment because of problems relating to hand dominance issues.26,28
All reported complications were recorded and categorized into three levels – mild (grade 1), moderate (grade 2), and severe (grade 3) – based on previously reported guidelines.27 Mild was defined as symptoms caused by DRF or its treatment that resolved with no specific treatment, moderate was defined as diagnoses that required a specific treatment such as therapy or splinting, and severe was defined as diagnoses that required surgical treatment. Any patients requiring additional intervention were identified, and their treatments were documented.
Statistical Analysis
Objective functional outcomes (wrist range of motion, grip strength, pronation, supination, and Jebsen-Taylor test) were normalized as a percentage of the value for the contralateral (untreated) wrist. Because a lower score for the Jebsen-Taylor test represents a better outcome, we subtracted the original percentage score from 100% to obtain a value consistent with other reported outcomes for which a higher score represents a better outcome. Regarding our grip strength calculations, we accounted for a 10% strength increase in the dominant hand if the right hand was dominant, but did not compensate if the left hand was dominant.28 MHQ data were reported as the overall score for the treated wrist and as the difference between injured and uninjured wrists (injured minus uninjured).
Demographic data were compared between young and old cohorts using the chi-square test. Means and standard deviations were reported for each outcome parameter at each follow-up time, and two-sample t-tests were used to determine statistically significant differences in outcomes between the old and young cohorts at 12 months. Predictors of hand outcomes after DRFs in patients of all ages have been previously explored in the literature for varying follow-up periods (3 months vs. 1 year).8 Based on these findings for the general population (all ages), we used multiple regression analysis, adjusting for age, gender, income, and fracture type (AO classification), to compare 12 month MHQ scores between the two age groups. In addition, linear mixed-effects models were used to model MHQ scores over the three predetermined follow-up times (3, 6, and 12 months). Prior to modeling, mean MHQ scores for each age group were plotted over time. Based on the results of the graphical analysis, MHQ scores were modeled either to linearly increase in time or to change from one level at 3 months to a different level during 6 to 12 months. Smaller values of Akaike Information Criteria (AIC) were used to choose between the two ways to model the outcome trend. AIC is a method used to select the most appropriate model for analyzing data with a small number of parameters.29 The linear mixed-effects models also included covariates of age, gender, income, and fracture type (AO classification). Given that previous works have also shown radiographic incongruity (articular step-off and gap) to be negatively associated with patient outcomes, we also chose to additionally assess the effect of this parameter on MHQ scores.8 Differences in complications at 3 months were compared using the chi-square test, and a generalized linear model (with logit link) and estimating equation were used to assess changes in complication rates over time. Statistical significance for all analyses was set at p ≤ 0.05.
Results
Over two years, fifty-nine eligible patients were recruited. One patient received surgical treatment at another institution and was eliminated. Three patients managed nonsurgically at outside institutions were also eliminated due to inadequate preoperative radiographic data. Objective outcomes (grip strength, Jebsen-Taylor test, and active range of motion) for both wrists of each patient were measured by a trained research assistant.
The demographic characteristics of the 55 enrolled patients are given in Table 1. The mean age was 30 years for the younger cohort (N = 30) and 69 years for the older cohort (N = 25). All fractures included in our study were classified as true Colles-type fractures. Among the older patients, there were 11 type A, 5 type B, and 14 type C fractures. In the younger cohort, there were 13 type A, 3 type B, and 9 type C fractures. Within both study groups, most patients were of Caucasian descent, had an income of at least $50,000, and had completed at least high school level education. No statistically significant differences in demographic variables between the two cohorts were found, but we observed a statistically significant difference in gender with females more common than males in the over 60 years subgroup (76% female), and the reverse relationship in younger subgroup (53% male; p = 0.03).
Table 1.
Patient Demographics
| Young [20 – 40 yrs] | Old [≥60 yrs] | p-value§ | |
|---|---|---|---|
| Number of patients enrolled | 30 | 25 | N/A |
| Age (range) | 29.9 (20–40) | 68.9 (60–83) | |
| Male | 16 (53%) | 6 (24%) | 0.03 |
| Caucasian | 25 (86%) † | 23 (92%) | 0.43 |
| AO classification | 0.52 | ||
| Type A | 11 (37%) | 13 (52%) | |
| Type B | 5 (17%) | 3 (12%) | |
| Type C | 14 (47%) | 9 (36%) | |
| Income level | 0.54 | ||
| < $20,000 | 4 (14%)† | 1 (5%)‡ | |
| $20,000 – $50,000 | 5 (17%)† | 5 (25%)‡ | |
| > $50,000 | 20 (69%)† | 14 (70%)‡ | |
| Education level | 0.84 | ||
| Did not graduate high school | 2 (7%)† | 1 (4%) | |
| High school or some college | 11 (38%)† | 11 (44%) | |
| Finished college or graduate school | 16 (55%)† | 13 (52%) |
Some patients did not feel comfortable answering personal questions regarding income and education levels. Given that these data were not critical to our research we did not choose to make answering these questions mandatory. Thus, several data fields do not contain answers from all participants in our study.
Based on chi-square test from comparing demographics between young and old cohorts
Data reported for 29 patients in cohort (97%)
Data reported for 20 patients in cohort (80%)
Patient compliance with clinic follow-up visits decreased over time. However, these obstacles rarely applied to therapy treatment sessions due to the increased flexibility in location and available appointment times of the various therapy sites. At three months, 4 out of 30 young and 6 out of 25 older-age patients missed their follow-up assessment. For the six month follow-up visit, 14 young and 9 older-age patients failed to attend, and at 12 months, 15 young and 8 older-age patients were unable to keep their appointments. In an effort to increase compliance, patients who were unable to attend clinic visits were given the option to mail in their MHQ questionnaire, and local therapists were contacted and asked to obtain grip strength and ROM values for their patients. Given its complexity, the Jebsen-Taylor test was only administered in our clinic. Consequently, the overall number of patient records for each outcome measure is slightly varied. However, we did not find missing 6 month MHQ scores to be associated with the observed value of the 3 month MHQ score (p = 0.46), and similarly we did not find missing 12 month MHQ scores to be associated with the observed values of the 6 month MHQ score (p = 0.90). This suggested that both the missing data group and the observed data group are likely random samples of the same population and provided some assurance that our missing data did not depend on observed measurements such as poor outcome.
Patient-Rated Measures
The patient-rated outcome scores from the MHQ failed to demonstrate a statistically significant difference between cohorts at any of the follow-up times (Table 2). Given that the original design of work-related questions in the MHQ encompasses both professional and other daily living activities, we did not modify the questionnaire for older non-working patients. In addition, the work domain of the MHQ was not normalized with respect to the contralateral hand because this domain does not measure right and left hands independently, but rather, considers overall work performance. The difference between the older and younger cohort in MHQ score at 12 months was not significant (p = 0.40) even after adjusting for income, AO type, and gender. Given that income was missing for one member of the younger cohort and five members of the older cohort, we repeated our analysis after multiply imputing missing income values using iterative multivariable regression technique. However, the difference between cohorts in overall MHQ score at 12 months still remained insignificant (p = 0.79). Similarly, adjusting for radiographic incongruity did not result in a significant difference between the two age groups. The difference in MHQ scores between injured and uninjured hands at 12 months were marginally significant between the two age cohorts (p = 0.09), with the older cohort showing a smaller difference, but was not significant after adjusting for covariates, such as gender, income, and AO type (p = 0.43).
Table 2.
| Cohort | 3 Months | 6 Months | 12 Months¶ | |||
|---|---|---|---|---|---|---|
| Raw Score |
Difference§ | Raw Score |
Difference§ | Raw Score |
Difference§ | |
| Young | 77±16 (25) |
−17±12 (25) |
83±17 (20) |
−11±10 (20) |
82±18 (15) |
−12±11 (15) |
| Old | 77±15 (18) |
−16±12 (18) |
81±17 (16) |
−9±10 (16) |
85±18 (17) |
−6±10 (17) |
Michigan Hand Outcomes Questionnaire overall scores can range from 0 to 100; the higher the score, the better the subject’s hand performance.
Values are expressed as the mean ± standard deviation (number of patients)
The difference between the injured and uninjured sides (injured-uninjured); a large negative value corresponds to worse outcome in the injured hand compared with the uninjured hand.
Based on two-sided independent t-tests comparing outcomes at 12 months between the younger and older populations; unadjusted p-values are 0.62 for raw scores and 0.09 for difference scores.
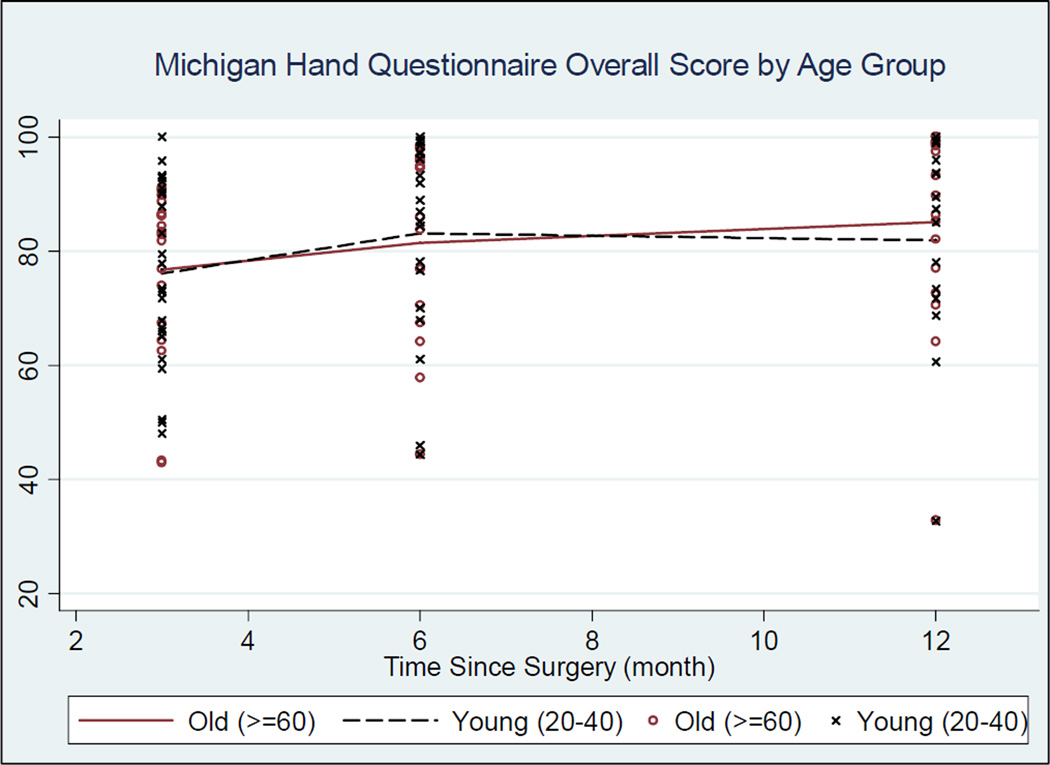
Another interesting finding was the dissimilarity in recovery trends between the two cohorts. Both young and old patients achieved similarly high levels of function by their 3 month postoperative visit. However, using Akaike’s Information Criterion (AIC), we found two distinct trends in MHQ scores over time between cohorts. While the older cohort continued to improve throughout their 6 and 12 month postoperative visits, the younger cohort peaked in their improvement during the 6 month visit and only maintained outcomes for the 12 month visit (Figure 1). We therefore fit a separate mixed-effect model for each age cohort (Table 3).
Figure 1. Michigan Hand Outcomes Questionnaire over Time by Two Age Cohorts This figure demonstrates the overall score for the Michigan Hand Outcomes Questionnaire for each cohort over time.
Connecting lines are based on locally weighted smoothing to illustrate patterns over time. The red line represents the older cohort (>=60) and the black dashed line represents the younger cohort (20–40). The black “x” marks represent individual patient outcomes for the older cohort and the red “o” marks represent individual patient outcomes for the younger cohort for each follow-up period (3,6, and 12 months).
Table 3.
Multivariable Predictors of Overall MHQ Score
| Predictor | Old | Young | ||||
|---|---|---|---|---|---|---|
| Coefficient£ | p-value | 95% CI | Coefficient£ | p-value | 95% CI | |
| Follow-up time† | 1.1 | 0.001 | 0.5, 1.8 | 5.7 | 0.036 | 0.4, 10.9 |
| Male | −6.9 | 0.369 | −22.0, 8.2 | 2.2 | 0.723 | −9.9, 14.3 |
| Income‡§ | 8.8 | 0.081 | −1.1, 18.8 | 9.2 | 0.033 | 0.8, 17.7 |
| AO type B* | 20.6 | 0.010 | 4.9, 36.3 | 3.8 | 0.637 | −12.1, 19.7 |
| AO type C* | 17.5 | 0.006 | 5.0, 30.0 | 1.4 | 0.835 | −11.5, 14.2 |
| Radial incongruityαβ | −2.8 | 0.719 | −18.3, 12.6 | −20.2 | 0.013 | −36.1, −4.2 |
| Ulnar variance | −1.1 | 0.555 | −5.0, 2.6 | −1.0 | 0.501 | −3.8, 1.9 |
This chart demonstrates the relationship between each predictor term and MHQ outcomes for both the older and younger cohorts. A positive coefficient represents a positive relationship between predictor term increase and MHQ value and a negative coefficient represents an inverse relationship. The magnitude of the coefficient term corresponds with the magnitude of the relationship between predictor term and MHQ score.
Follow-up time was modeled differently for each cohort based on the distinct recovery patterns displayed in Figure 1. For older patients, follow-up time is real time (in month) post-surgery, whereas for younger patients follow-up time is an indicator for 6 or 12 months with reference category of 3 month.
Income data were missing for 6 patients
Income was divided into 3 ordinal categories: 0 = < $20,000; 1 = $20,000-$50,000; 2 = ≥ $50,000
AO type A served as the reference group
Radial incongruity data were missing for 7 patients
Radial incongruity = (articular step-off + gap) ≥ 1mm
Our model showed that for the older cohort, the MHQ score increased linearly at a rate of 1.1 point each month (p = 0.001). Alternatively, for the younger cohort, the MHQ increased 5.7 points (p = 0.036) from 3 to 6 months and remained at that level. For both groups, income was positively associated with MHQ score, but only statistically significant in the younger cohort (p = 0.081 for the older cohort; p = 0.033 for the younger cohort). Interestingly, radiographic incongruity was associated with worse outcomes for the younger cohort only (p = 0.01); incongruity was observed in 9.8% and 7.1% of the measurements of the older and the younger cohort, respectively, and was not different between the two cohorts (p = 0.723).
Objective Measures
Functional outcomes (Jebsen-Taylor test and grip strength) and active wrist and forearm range of motion are presented in Table 4. Overall, most measurements demonstrated continued improvement between both the three-to-six month period and the six-to-twelve month time periods. The highest scores (percentage value of the contralateral, uninjured wrist) were achieved by the Jebsen-Taylor test and range of motion tests (flexion + extension, pronation, supination), while grip strength consistently maintained the lowest score and largest degree of variation (standard deviation) for both cohorts. No objective measures showed a statistically significant difference between the younger and older cohorts at twelve months, except the Jebsen-Taylor test that showed a trend toward a worse outcome in the older-age cohort. Similarly, no significant difference was observed between radiographic outcomes at the twelve month follow-up period, except for ulnar variance, which was significantly different between the two groups (younger mean ulnar variance at 12 months = −0.8 + 1.6; older mean ulnar variance at 12 months = 0.3 + 1.4; p = 0.04) (Table 5).
Table 4.
Postoperative Objective Measurements†
| Measurement | Cohort | 3 Months | 6 Months | 12 Months | p-value§ |
|---|---|---|---|---|---|
|
Jebsen Taylor Test‡ |
Young | 91±14 (26) | 94±13 (16) | 97±14 (15) | 0.09 |
| Old | 82±22 (19) | 90±18 (16) | 87±18 (17) | ||
|
Wrist Range of Motionαβ |
Young | 86±12 (25) | 89±12 (16) | 92±11 (14) | 0.60 |
| Old | 81±10 (19) | 84±17 (17) | 95±17 (17) | ||
|
Grip Strength᧠|
Young | 66±19 (26) | 78±22 (18) | 80±22 (15) | 0.73 |
| Old | 44±28 (19) | 67±35 (17) | 77±31 (17) | ||
| Pronation | Young | 93±8 (25) | 97±9 (16) | 97±6 (14) | 0.80 |
| Old | 95±8 (19) | 97±7 (17) | 98±8 (17) | ||
| Supination | Young | 90±10 (25) | 95±7 (16) | 96±5 (14) | 0.25 |
| Old | 95±8 (19) | 97±18 (16) | 100±10 (17) |
Data reported as mean percent ± standard deviation (number of patients evaluated)
Normalized percent values were calculated as [(1-(injured-normal)/normal)*100] so that higher scores represent a better outcome
Wrist range of motion is based on active flexion + extension
Higher range of motion and grip strength scores represent better outcome; normalized percent values were calculated as (injured-normal)/normal*100
Based on two-sided independent t-tests comparing outcomes at 12 months between the young and old patient groups
Grip strength is adjusted for hand dominance using the 10% rule
Table 5.
Radiographic Outcomes
| Measurement | Cohort | 3 Months | 6 Months | 12 Months | p-value§ |
|---|---|---|---|---|---|
|
Radial Inclination† |
Young | 25±3.4 (24) | 25±2.1 (17) | 25±1.7 (15) | 0.52 |
| Old | 25±4.1 (18) | 24±5.0 (16) | 24±4.5 (17) | ||
|
Palmar Tilt† |
Young | 9±6.9 (24) | 9±5.6 (17) | 9±3.8 (15) | 0.84 |
| Old | 9±8.2 (18) | 8±7.7 (16) | 10±5.8 (17) | ||
|
Radial Height† |
Young | 13±2.1 (24) | 12±1.0 (17) | 13±1.8 (15) | 0.29 |
| Old | 13±3.0 (18) | 12±3.1 (16) | 12±2.8 (17) | ||
|
Ulnar Variance† |
Young | −0.5±1.7 (24) | −0.8±1.6 (17) | −0.8±1.6 (15) | 0.04 |
| Old | 0.6±1.2 (18) | 0.2±1.1 (16) | 0.3±1.4 (17) | ||
|
Articular Step-Off‡* |
Young | 13% (24) | 0% (17) | 7% (15) | 0.37 |
| Old | 0% (18) | 13% (16) | 6% (17) | ||
|
Articular Gap‡* |
Young | 8% (24) | 0% (17) | 6% (15) | 0.93 |
| Old | 6% (18) | 0% (16) | 6% (17) |
Data reported as mean ± standard deviation (number of patients evaluated)
Data reported as % of patients with step or gap ≥ 1mm (number of patients evaluated)
93% of articular step-off measurements and 95% of articular gap measurements were 0mm, which severely skewed the distribution of results for these parameters. Thus, a calculation of the mean was not a suitable summary statistic, and it is more appropriate and meaningful to dichotomize at an appropriate cutoff value and report the percent of patients that fall within each category.
Based on two-sided independent t-tests comparing outcomes at 12 months between the younger and older patient groups
Complications
A list of complications (mild = 1, moderate = 2, and severe = 3) observed in both patient groups is presented in Table 6. Overall, we did not observe any tendon ruptures, plate removals, or deep infections. Ten patients, five young and five older, experienced 11 complications. Nine of these complications occurred on or before the three-month postoperative visit. No statistical difference was found in complication rates between the two cohorts for all follow-up measurement times, and the likelihood of experiencing a complication decreased significantly over time (p = 0.01) (Table 7).
Table 6.
Summary of Complications
| Cohort | Complication | Severity† | Follow-up time‡ |
|---|---|---|---|
| Young | Tendonitis (second dorsal compartment)§ | 1 | 3 months |
| Cellulitis | 1 | ||
| Skin blisters | 1 | ||
| Suture abscess | 1 | ||
| Median nerve damage (thenar motor branch) | 3 | ||
| Intersection syndrome§ | 2 | 6 months | |
| Old | Scar adherence | 1 | 3 months |
| Forearm blister with edema | 1 | ||
| Left wrist hematoma | 3 | ||
| Hardware loosening; removal of plate | 3 | ||
| Minimal collapse of distal radius fracture (ulnar plus variance) |
1 | 6 months |
Complication severity was graded on scale from 1 to 3: 1 = mild, 2 = moderate, 3 = severe
No complications were experienced at the 12 month for either cohort
These complications were experienced by the same patient
Table 7.
Observed Complication Rates*
| Cohort | Time Since Operation | ||
|---|---|---|---|
| 3 Month | 6 Month | 12 Month | |
| 20–40 | 19% (5/26) | 5% (1/20) | 0% (0/15) |
| ≥60 | 21% (4/19) | 6% (1/17) | 0% (0/17) |
Data reported as percentage (# of patients experiencing complications/total number of patients)
Three patients had severe complications (grade 3), all of which occurred within the three month postoperative period. One younger patient suffered from transient dysfunction of the thenar branch of the median nerve that resolved after carpal tunnel release. A second older patient suffered from a wrist hematoma that required evacuation, and a third older patient experienced hardware loosening and required subsequent plate removal. The remaining six complications were all considered minor (Table 6).
Power Analysis
Because our findings indicated no statistically significant difference in MHQ score between the older and younger cohorts, we conducted a post-hoc power analysis to evaluate the detectable size of the difference in overall MHQ score between the two subgroups in this study. At the three month follow-up period, assuming a common standard deviation of 16 in the overall MHQ score and based on a sample size of 25 patients in the younger cohort and 18 patients in the older cohort, our study had 80% power to detect a difference in mean MHQ scores of 14 or greater using an independent two-sided two-sample t-test (p = 0.05). Then, using repeated measurements at each of the three assessment time periods with conservatively assumed sample sizes of 20 and 17 in each group (the observed sample size at each time varied) and assuming the observed correlation across repeated measurements of 0.7, this study had 80% power to detect a between group difference in mean MHQ of 15 or greater.
Discussion
Since Colles’ observation of distal radius fractures almost 200 years ago, many physicians continue to perceive older patients as a group with low functional demand and thus manage the vast majority of DRFs in older adults with conservative measures irrespective of activity level.21 Proponents of the traditional treatment approach have not found a benefit of anatomic reduction in older patients due to a lack of correlation between radiographic and functional outcomes in this patient population.13–16 However, the conclusions of these studies should be interpreted with caution for several reasons. First, several of these studies only included sicker, less-active older adults and thus their conclusions may only be considered valid for a small subset of today’s older population.13–14 Second, although the study performed by Anzurat, et al included more active older adults, the authors based their conclusions on a single radiographic parameter (dorsal/volar tilt) previously tested exclusively in younger patients.15Moreover, only 59% of patients reported being satisfied or very satisfied with their functional status at 6 months. The authors of the study were unable to explain the observed dissatisfaction from their patient-rated outcomes (SF-12 PCS, SF-12 MCS, and DASH), which may suggest that the SF-12 and DASH surveys are not sensitive enough to evaluate patient-rated DRF outcomes in older patients. Thus, although outcomes were consistent between unacceptably reduced and acceptably reduced subjects, general satisfaction with closed reduction and casting was poor among older-age patients.
In contrast to the above philosophy, other recent studies have emphasized the importance of radiographic outcomes and anatomic re-alignment in older patients.17–20 A recent retrospective study evaluating outcomes of close reduction and external fixation for unstable intra-articular distal radius fractures in women over 55 years of age found significant secondary displacement occurring in 11 out of 16 patients, and 6 out of 16 (38%) patients reported fair or poor outcomes.16 Furthermore, of the four reported poor outcomes, one patient suffered from a malunion, another from significant loss of reduction, and the other two from radial incongruity ≥ 1mm. The observed degree of secondary displacement and positive relationship of displacement with functional outcomes suggest that external fixation methods alone are not able to sufficiently reduce older-age osteoporotic bone and may affect overall outcomes, particularly in fractures with an intra-articular component.
As a response to these findings, several authors have shown that predictable anatomic reduction with internal fixation methods in older adults is possible and the corresponding functional outcomes are very encouraging.6,17,19 In 2002, Jupiter et al conducted a retrospective case series of 20 inadequately-reduced DRF patients over the age of 60 with active lifestyles.17While outcomes at 38 months were found to be good or excellent in 18 out of 20 patients, the authors reported a significant number of complications with 6 patients requiring surgical removal of the plate.17 In a similar study (2004) with 18 patients over the age 60, Beharrie et al obtained equally promising functional outcomes with only 4 minor complications.19 However, neither of these studies controlled for the type of plating approach and included dorsal and volar plating systems. Orbay and Fernandez specifically assessed the volar fixed-angle approach in 23 patients between 75–94 years (mean age = 82 years) with 24 DRFs.6 At 63 weeks follow-up, the authors noted good outcomes and a very low complication rate. Thus, they concluded that the new VLPS is successfully able to handle osteoporotic bone in older patients, providing stable internal fixation and allowing for early functional restoration.6 The conclusions drawn from the above studies suggest that predictable anatomic reduction in older-age adults is both possible and successful despite the presence of osteoporosis and other comorbid conditions. However, these findings are preliminary and relatively inconclusive due to their small sample sizes, lack of comparison or control group, use of multiple internal fixation techniques, and/or limited statistical analysis.
In this study, we present an analysis of two parallel prospective cohorts aimed at comparing outcomes and complication rates of DRF treatment with the VLPS in both young and older patients. Our findings are consistent with the conclusions of Orbay et al, suggesting that the VLPS is successful in treatment of DRFs in patients over 60 years of age. More specifically, we observed no significant difference between cohorts for both functional and patient-rated outcomes (MHQ score). Nevertheless, we did notice a marginal difference in the results of our Jebsen-Taylor test, in which patients over 60 years of age experienced worse outcomes than the younger cohort (p = 0.09). Although a difference in ulnar variance was observed between the two groups at the three month postoperative evaluation, the stability of reduction was maintained over the follow-up period. Taken together, these results suggest that no loss of reduction was observed in the older cohort due to the presence of osteopenia. The presence of a measurement error is unlikely because all measurements were performed by a single blinded evaluator using a computer program that systematically assessed all X-ray images in a standardized fashion.
The results of our multivariable analysis identified income as a significant positive predictor (p = 0.033) and articular incongruity as a significant negative predictor (p = 0.013) of MHQ score in younger patients. Although the older adults demonstrated the same associated trends, these relationships were not statistically significant. In particular, better radiographic results appeared to have less of an impact on VLPS outcomes in older patients than in younger patients.
The most significant conclusion drawn from our study can be observed in the different recovery trends (based on MHQ score) for each cohort. Although both groups achieved similarly high levels of functional restoration at the 3 month follow-up period, the older-age cohort continued to improve linearly over the 6 and 12 month follow-up period while the younger cohort improved to a higher level at the 6 month period and remained at the level through the 12 month follow up time (Figure 1). Ultimately, at 12 months, older patient outcomes slightly exceeded those of their younger counterparts. These results suggest that compared to younger patients who recovered quickly and reached their maximum recovery by the 6[th] month, older patients took longer to recover, but ultimately attained better outcomes than the younger cohort one year after surgery. Thus, physicians and researchers should consider the different recovery pattern of older patients when analyzing outcomes, structuring future clinical trials, and performing economic analyses regarding the VLPS for older adults.
Study Limitations
The findings of our study are limited by several factors. As with any clinical trial involving outpatient subjects, we were unable to maintain 100% patient recruitment throughout the 12 month follow-up period. Despite the concern that our patient participation was less than optimal, the findings of this study are important given the paucity of literature available on this topic and the potential impact our findings may have on future clinical trial design. We also recognize that the shortened 12 month duration of our follow-up period presents an additional study limitation. However, the close approximation of the observed outcome plateaus for both cohorts between the 6 and 12 month recovery dates to the ceiling of our MHQ scales suggest that further follow-up time would not affect our study results. In consideration of these results as well as the additional patient burden associated with continued clinic visits, we chose to end our follow-up evaluation at 12 months. Our study did not include a comparative analysis of patients who received non-operative treatment. However, given the rather minimal displacement of the fractures treated non-operatively, we felt that this subgroup of patients would not be comparable to the studied patient group in our trial. The purpose of the present study is not to recommend internal fixation for all DRFs in older patients, but rather to assert the eligibility of this patient group for surgical management with the VLPS.
Other potential limitations of our research include our lack of patient demographic data, such as pre-operative activity levels and a measure of osteoporosis. Given the difference in appearance between older and younger patients, apparent indications for surgery, and visibility of post-surgical scarring, it was impossible to completely blind patients and outcome assessors in this study. In addition, all patients were surgically treated at the same tertiary care center by surgeons very experienced with the VLPS technique, which may bias our outcomes. Furthermore, the definition of our older cohort as greater than or equal to 60 years may also present another study limitation. After performing a sensitivity analysis comparing outcomes of patients ≥70 years of age to other older and younger patients, we found no significant difference between all three cohorts for each follow-up period (3 months p = 0.99; 6 months p = 0.77; 12 months p = 0.83). Thus, it is reasonable to believe that by including patients between 60 and 70 years of age, we did not bias our outcomes in favor of producing similar results to the younger cohort. Finally, it is possible that the older patients presented in our study represent a subset of healthier, more active patients given our exclusion of patients with systemic conditions or multi-organ failure. Despite the above mentioned limitations, we feel that the VLPS is successful in managing older-age DRFs and without increased complications compared to younger patients.
Future Recommendations
To date, no current studies in the literature have tested the effects of pre-operative activity levels or osteopenia severity on DRF outcomes and complication rates in older patients. We recommend the investigation of older-age DRFs in a prospective, randomized-controlled, multi-center study comparing the VLPS with other treatment methods to determine the optimal strategy for managing DRFs in the older patient population. Standardized patient demographic information should incorporate pre-operative activity levels and the severity of osteoporosis (as measured by bone mineral density) in addition to age, gender, fracture severity, income, race, and education levels (as a measure of socioeconomic status). Outcome measures should be determined a priori and include objective functional measures (grip strength, ROM), radiographic results, and patient-rated outcomes. As life expectancies increase, adults greater than 60 years will become more stratified within their age group, and physicians may no longer rely solely on age to base their treatment decisions. Older adults must be considered for surgical management of DRFs based on appropriate predictors, rather than based on age alone.
References
- 1.Weinstein JN, Birkmeyer JD, editors. The Dartmouth Atlas of Musculoskeletal Health Care. Chicago, IL: American Hospital Publishing; 2000. [PubMed] [Google Scholar]
- 2.Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149:2445–2448. [PubMed] [Google Scholar]
- 3.Ray NF, Chan JK, Thamer M, Melton LJ., III Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res. 1997;12:24–35. doi: 10.1359/jbmr.1997.12.1.24. [DOI] [PubMed] [Google Scholar]
- 4.Federal Interagency Forum on Aging-Related Statistics. [Accessed 2006 Aug 31];Older Americans 2000: Key Indicators of Well-Being [Web Page] Available at: http://www.agingstats.gov/chartbook2000/population.html.
- 5.Smith DW, Henry MH. Volar fixed-angle plating of the distal radius. J Am Acad Orthop Surg. 2005;13:28–36. doi: 10.5435/00124635-200501000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fracture in the elderly patient. J Hand Surg. 2004;29A:96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 7.Schoeni RF, Freedman VA, Wallace RB. Persistent, consistent, widespread, and robust? Another look at recent trends in old age disability. J Gerontol B Psychol Sci Soc. 2001;56:206–218. doi: 10.1093/geronb/56.4.s206. [DOI] [PubMed] [Google Scholar]
- 8.Chung KC, Kotsis SV, Kim M. Predictors of functional outcomes after surgical treatment of distal radius fractures. J Hand Surg. 2007;32:76–83. doi: 10.1016/j.jhsa.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radius fractures with the volar locking plating system. J Bone Joint Surg. 2006;88A:2687–2694. doi: 10.2106/JBJS.E.01298. [DOI] [PubMed] [Google Scholar]
- 10.Rozental TD, Beredjiklian PK, Bozentka DJ. Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of the radius. J Bone Joint Surg. 2003;85A:1956–1960. doi: 10.2106/00004623-200310000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Carter PR, Frederick HA, Laseter GF. Open reduction and internal fixation of unstable distal radius fractures with a low-profile plate: a multicenter study of 73 fractures. J Hand Surg. 1998;23A:300–307. doi: 10.1016/S0363-5023(98)80131-7. [DOI] [PubMed] [Google Scholar]
- 12.Campbell DA. Open reduction and internal fixation of intra articular and unstable fractures of the distal radius using the AO distal radius plate. J Hand Surg. 2000;25[B]:528–534. doi: 10.1054/jhsb.2000.0485. [DOI] [PubMed] [Google Scholar]
- 13.Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg. 2000;25A:19–28. doi: 10.1053/jhsu.2000.jhsu025a0019. [DOI] [PubMed] [Google Scholar]
- 14.Beumer A, McQueen MM. Fractures of distal radius in low-demand elderly patients: closed reduction of no value in 53 of 60 wrists. Acta Orthop Scand. 2003;74:98–100. doi: 10.1080/00016470310013743. [DOI] [PubMed] [Google Scholar]
- 15.Anzarut A, Johnson JA, Rowe BH, Lambert RGW, Blitz S, Majumdar SR. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated fractures. J Hand Surg. 2004;29A:1121–1127. doi: 10.1016/j.jhsa.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Hegeman JH, Oskam J, Vierhout PAM, ten Duis HJ. External fixation for unstable intra-articular distal radial fractures in women older than 55 years. Acceptable functional end results in the majority of the patients despite significant secondary displacement. Injury, Int J Care Injured. 2005;36:339–344. doi: 10.1016/j.injury.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 17.Jupiter JB, Ring D, Weitzel PP. Surgical treatment of redisplaced fractures of the distal radius in patients older than 60 years. J Hand Surg. 2002;27A:714–723. doi: 10.1053/jhsu.2002.34007. [DOI] [PubMed] [Google Scholar]
- 18.Ring D, Jupiter JB. Treatment of osteoporotic distal radius fractures. Osteoporos Int. 2005;16:S80–S84. doi: 10.1007/s00198-004-1808-x. [DOI] [PubMed] [Google Scholar]
- 19.Beharrie AW, Beredjiklian PK, Bozentka DJ. Functional outcomes after open reduction and internal fixation for treatment of displaced distal radius fractures in patients over 60 years of age. J Orthop Trauma. 2004;18:680–686. doi: 10.1097/00005131-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg. 2002;27A:205–215. doi: 10.1053/jhsu.2002.32081. [DOI] [PubMed] [Google Scholar]
- 21.Colles A. On the fracture of carpal extremity of the radius. Edinb Med Surg J. 1814;10:182–186. [PMC free article] [PubMed] [Google Scholar]
- 22.Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000;5(2):103–12. doi: 10.1142/s0218810400000223. [DOI] [PubMed] [Google Scholar]
- 23.Graff S, Jupiter J. Fracture of the distal radius: classification of treatment and indications for external fixation. Injury. 1994;25(Suppl 4) doi: 10.1016/0020-1383(95)90125-6. S-D14-25. [DOI] [PubMed] [Google Scholar]
- 24.Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of and responsiveness to clinical change. Ann Plastic Surg. 1999;42:619–622. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg [Am] 1998;23:575–587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 26.Jebsen RH, Taylor N, Trieschmann RB, Trotter MJ, Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil. 1969;50:311–319. [PubMed] [Google Scholar]
- 27.McKay SD, MacDermid JC, Roth JH, Richards RS. Assessment of complications of distal radius fractures and development of a complication checklist. J Hand Surg. 2001;26A:916–922. doi: 10.1053/jhsu.2001.26662. [DOI] [PubMed] [Google Scholar]
- 28.Sharma S, Schumacher HR, Jr, McLellan AT. Evaluation of the Jebsen hand function test for the use in patients with rheumatoid arthritis [corrected] Arthritis Care Res. 1994;7:16–19. doi: 10.1002/art.1790070105. [DOI] [PubMed] [Google Scholar]
- 29.Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;AC-19(6):716–723. [Google Scholar]