Abstract
The use of reliable evidence to evaluate health care interventions has gained strong support within the medical community and in the field of plastic surgery in particular. Evidence-based medicine aims to improve health care and reduce costs through the use of sound clinical evidence in evaluating treatments, procedures and outcomes. The field is hardly new, however, and most trace its origins back to the work of Cochrane in the 1970s and Sackett in the 1990s. Though she wouldn’t know it, Florence Nightingale was applying the concepts of evidence-based reform to the medical profession more than a century before. She used medical statistics to reveal the nature of infection in hospitals and on the battlefield. Moreover, Nightingale marshaled data and evidence to establish guidelines for health care reform. Tracing the origins of evidence-based medicine back to Nightingale underscores how critical this movement is to improving the quality and effectiveness of patient care today.
Keywords: Florence Nightingale, Evidence-based medicine, medical statistics
There has been an increasing awareness amongst health care professionals that medical decision-making should be guided, if not determined, by sound evidence. This concept is particularly relevant today, as health care spending in America continues to increase without any measurable progress in outcome, access or quality of patient care. In plastic surgery, the emphasis on innovative techniques and procedures oftentimes leads to rising costs. Finding a way to assess these new techniques in terms of both cost and outcome is critical for efficient health care delivery.(1) The journal Plastic and Reconstructive Surgery is spearheading the effort to evaluate the latest treatments and procedures in Plastic Surgery through evidence-based measures. President Obama has also called attention to this growing need for evidence-guided reform by allocating $1.1 billion for what the administration calls “comparative effectiveness research”.(2, 3) Under this new legislation, the funds will be divided between the Agency for Healthcare Research and Quality, the National Institutes of Health and the Department of Health and Human Services, all with the purposes of comparing and finding the best diagnostic tools, drugs and treatments for any given medical condition. (4
Using evidence to support clinical decision-making is hardly a new concept. Throughout a physician’s education, training and professional career, he/she is continuously pushed to record data, interpret findings and draw conclusions. Evidence is culled from years in practice, research and personal experience, and thus called upon when making health-care decisions.(5) Although most attention is paid to the work of Sackett and Cochrane in tracing the origins of evidence-based medicine (EBM), Florence Nightingale was applying the concepts of evidence-based interventions to the medical profession more than a century before. Within the last two decades, EBM has become an apposite topic in all circles, amongst health care providers and public health professionals to politicians and the general public.(6, 7) Tracing its origins back to Nightingale and understanding her contributions to the history of evidence-based medicine will shed light on where the field can take us in the future.
Origins of Evidence-based Medicine
The concept of EBM was first introduced to the medical literature in 1992, but drew criticism from physicians and medical journal editors alike.(6, 8, 9) The universally-acknowledged pioneer of the field, David L. Sackett, defended evidenced-based medicine in response, describing it as “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients.”(10) Sackett maintained that providing this kind of medical care involves formulating a diagnosis in the most effective and efficient way, while incorporating the preferences and rights of the patient into the decisions that follow.
Looking back even farther, Archie Cochrane may be considered a forerunner of evidence-based medicine by advancing the use of randomized controlled trials (RCTs) in the 1970s. Cochrane rationalized that because health care resources are limited, they should only be allocated for those procedures proven most effective; effectiveness could be determined through the discriminating evidence provided by RCTs.(11) His promotion of randomized trials to provide evidence for health care decision-making proved instrumental to what would become the evidence-based medicine movement.
Although Sackett briefly attributes the “philosophical origins” of the movement to mid- 19th century Paris in his writings, Nightingale remains hitherto unrecognized for her integral role in laying the groundwork for what is now described by some as the “fourth revolution” in American medicine.(10, 12) Nightingale used evidence to reveal the nature of infection in hospitals and on the battlefield. She collected data, utilized statistics and, with the help of the British government, made vast improvements in health care delivery.
Nightingale as a Visionary for Evidence-based Medicine
Known best for her legacy as the Lady with the Lamp, Nightingale has been romanticized as one of the most compassionate and famous nurses in history, but few have considered her achievements in light of EBM. Although her work during the Crimean War (1854–1856) marked one of her greatest accomplishments, Nightingale’s post-war career in health care reform was her most significant contribution. She supervised the modernization of nursing, advised governments on Army health reform, marshaled sanitary improvements in Britain and India, and influenced hospital design. Gathering evidence to support the need for such reforms, Nightingale used careful observation, record-keeping and statistical analysis to validate her work in each of these developments.
Historical precedents: Education and Statistics
Nightingale was born into an upper-class family in 1820, and grew up in a household that placed a high premium on education. By 1840, Nightingale focused her studies on mathematics and during her 2-hour weekly tutoring sessions, she was introduced to statistics, a field she soon grew to love.(13) When Nightingale first expressed interest in a career in nursing, her family dismissed her. At the time, nurses traditionally came from the lower to lower-middle classes who were trained as little more than housemaids, cleaning and changing bedding in the hospital setting. Still, Nightingale recognized the growing need for trained nurses and during her travels in July of 1851, she visited the Institution for Deaconesses at Kaiserswerth on the Rhine.(14) She stayed on at Kaiserswerth to observe and train as a nurse for three months, marking this short sojourn as her only formal education in the field of nursing.
In April 1853, Nightingale left the strict confines of her family home and moved to London in order to become the Superintendent of the Institute for the Care of Sick Gentlewomen in Upper Harley Street, London.(15) During her first year in London, Nightingale began to hear reports of the War in Crimea where the British Army was suffering from poor conditions and lack of proper health care.(16) Sidney Herbert, a politician heading the War Office during the Crimean War, had heard of Nightingale and assigned her to lead a mission of nurses to Scutari, the Turkish barracks that served as the British Army’s military hospital.
Crimean War
Nightingale arrived in Constantinople on November 4, 1854 with 20 nurses, 8 Anglican sisters, 10 nuns and one other woman.(17) From there she surveyed the general hospital, then traveled across the Black Sea to the Barracks hospital in Scutari. The conditions at the hospitals were deplorable; supplies ordered never made it to their destinations and it was completely unclear who was managing the hospitals. Instead of passively recording her observations on the setbacks in Scutari, Nightingale sought to find the causes for each one. In a letter to Sidney Herbert dated 25 November 1854, she described the lack of sanitation in the hospital, and how there was no more than “a washing once in eighty days for 2300 men. The consequences of all of this are fever, cholera, gangrene, lice, bugs, fleas --& may be erisypelas –from the using of one sponge among many wounds.”(18) Like the majority of her contemporaries, Nightingale believed in the theory of miasma, which asserted that disease was caused by noxious vapors emanating from decomposing matter. Though Nightingale’s fundamental assumptions about how diseases spread were inaccurate, she still understood that diseases could be transferred amongst sick patients and sought to eliminate the mechanisms through which such preventable diseases were communicated.
In addition to the lack of supplies at Scutari, there were more fundamental problems contributing to poor health conditions. The hospital buildings were in a terrible state of disrepair, with contaminated water supplies and malfunctioning drainage systems. With time, it was eventually ascertained that Scutari was built upon an old Turkish burial ground. In March of 1855, a Sanitary Commission was sent to Crimea to address the terrible conditions reported by Nightingale. The Commission, headed by Dr. John Sutherland, went straight to work under her guidance. They unclogged drains and removed the debris from water pipes. They improved air circulation by installing windows and vents in the roof and washed the walls and floors of the hospital with lime. Waste management was instituted so that trash was removed from the hospital on a daily basis. The mortality rates dropped from 52% before the Commission’s arrival to 20% afterward.(19) Nightingale was certain that the Sanitary Commission was responsible for this drastic improvement in mortality rates.
Nightingale was most unimpressed with the poor record-keeping system at Scutari. She believed that in order to evaluate conditions and institute change, one must record data and provide compelling evidence for pursuing reforms. She was a proponent of data collection, but always with a greater purpose in mind; medical statistics were recorded in an effort to aid the objectives of disease prevention.(20) In a letter published in 1874, she wrote, “Do we look enough into the importance of keeping careful Notes of Lectures, of keeping notes of all types of cases, and of cases interesting from not being type cases: so as to improve our powers of observation: all essential, if we are in future to have change?”(17) Ultimately, it would not be until Nightingale left Scutari and returned to London before she would manage to fulfill her greatest potential in health care reform and actually see the changes she so actively sought.
Post-War Health Care Reforms
On 24 February 1855, an engraving in the Illustrated London News depicted Florence Nightingale as the Lady with the Lamp (Fig. 1). The image became one of the most iconic images of the nursing profession, showing a benevolent woman tending to her wounded soldiers at night. In spite of this romantic painting of Nightingale as a war-time heroine, the woman herself was more interested in collecting evidence and putting it to use than in fostering a warm reception by her immediate audience and those abroad. Still, when she returned from Turkey, Nightingale was received with great acclaim.
Figure 1.
“Lady with the Lamp” engraving
Source: Illustrated London News 24 February 1855
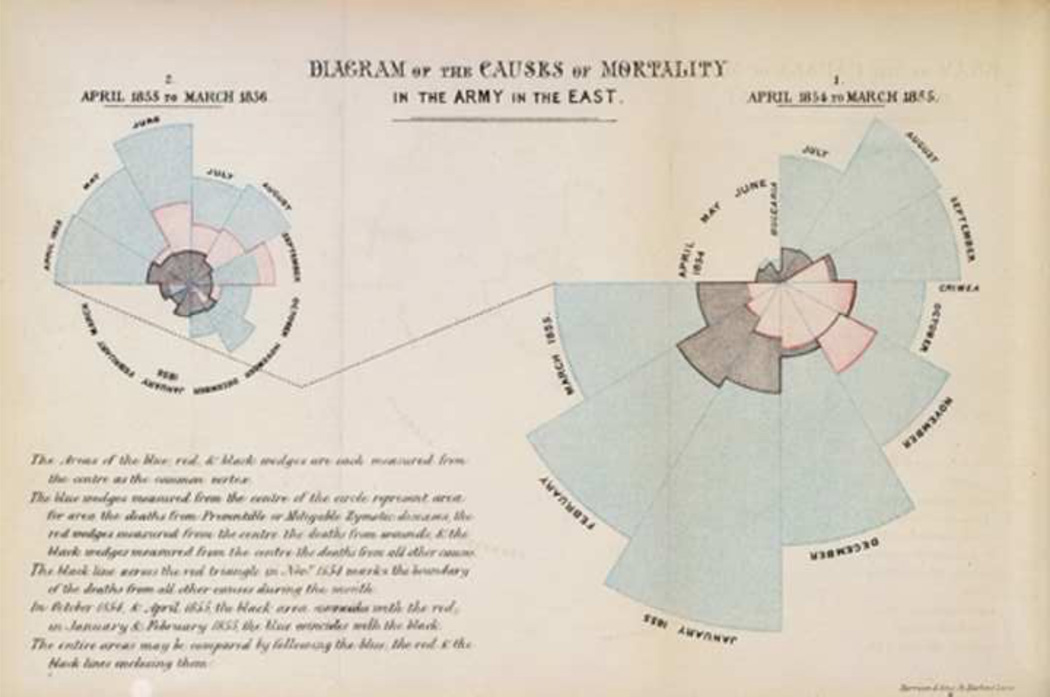
Despite her soaring reputation with the public, Nightingale remained withdrawn and isolated, diving into work preparing for upcoming meetings with the British government. In 1856 Nightingale was invited to meet with Queen Victoria and Lord Panmure in order to discuss the establishment of the Royal Commission to Enquire into the Sanitary Condition of the Army.(19) Panmure and the Queen assigned Nightingale the task of writing a précis or formal report on her experience at Scutari. Having worked tirelessly to produce comprehensive notes and recommendations, Nightingale augmented her findings with diagrams and tables. The most consistently reproduced figure in her writings was something she called a coxcomb, a primitive pie chart showing the mortality rate in Scutari (Fig. 2). Nightingale described her coxcomb as a means to “affect ‘thro the Eyes what we may fail to convey to the brains of the public through their word-proof ears.”(19) The evidence she produced was used to show the predominance of disease as the main cause of mortality in the British Army during the Crimean War, not actual war injuries. The diagram showed information from April 1854-March 1855, and April 1855- March 1856; in the annotation she noted, “The blue wedges…represent deaths from Preventible or Mitigable Zymotic Diseases, and the red wedges…the death from wounds and the black wedges…the deaths from all other causes.”
Figure 2.
Coxcomb
Source: Nightingale, F. Notes on matters affecting the health, efficiency, and hospital administration of the British army: founded chiefly on the experience of the late war. London: Harrison & Sons, 1858.
Armed with figures and extensive notes, Sidney Herbert, Dr. Sutherland, and Nightingale prepared the witnesses to stand before the Commission, organized the evidence and calculated the statistics to be used for Nightingale’s report. In January 1858, she published her report and in her personal accounts of the situation in Crimea, Notes on Matters Affecting the Health, Efficiency and Hospital Administration of the British Army, Nightingale laid out a thorough proposal for the overhaul of the soldier’s living conditions during peacetime and at war. She enumerated the many ways in which to alleviate these problems and then recommended a new standard of hygiene in all hospitals. She emphasized that each hospital keep a patient records database detailing all medical information that may be pertinent to their care. Nightingale also published a pamphlet called the Mortality of the Army that compiled her diagrams and statistical data from the 1858 report, printed 2000 copies and circulated them to the royal family and other government officials. On account of this, the Army Sanitary Committee visited every barrack and army hospital in England from 1858–1861, reporting on the structural changes necessary for improved ventilation, sewage disposal, potable water supplies and adequate washing facilities.(19) The committee visited 108 barracks and 58 hospitals during that period.
In addition to establishing a medical records system and improving hygiene and sanitation, Nightingale laid out comprehensive plans for hospital reform. She recommended that entire hospital floors be redesigned to allow more efficient and improved square footage per patient bed. She included detailed notes on how to determine the correct amount of space surrounding each bed, accounting for ventilation, administration and clinical instruction.(21) She also suggested keeping windows open to allow for better ventilation and light, and the disinfection of soiled linens and disposal of all contaminated supplies.(22) Nightingale believed that the pavilion style hospital, with separate wings, would reduce the spread of infection. She also espoused the use of natural ventilation via windows on the wards, an idea inspired by what Nightingale saw at the Lariboisière Hospital in Paris, one of the many hospitals that she visited during her extensive travels before the Crimean War. (23
Though she would not know it, Nightingale’s recommendations for improved hospital design are topical even today. In the 18 May 2009 issue of The New York Times, an article described the prevalence of evidence-based hospital design.(24) To date, more than 1,500 studies have been performed to look at the way design influences health care. In addition to recommending the construction of single rooms to ensure adequate privacy and space for the patient, research by the Center for Health Design has shown that single rooms improve sleep and reduce stress of the patient, as well as reduce the spread of infection. Although Nightingale recommended the implementation of windows for natural light and improved ventilation, current research has also shown that natural light can reduce depression, pain and stress during hospital stays.(25) Nightingale did not have the means to conduct the kind of prospective research studies that would substantiate her recommendations, but she still exhibited great prescience in addressing areas for potential reform and using the limited resources she had in order to validate her own claims.
Nightingale’s use of Medical Statistics
Nightingale used statistical evidence to formulate recommendations for the renovation of the St. Thomas Hospital in England.(26) Nightingale first became involved with the hospital in 1859, when she was setting up her nursing school at the hospital. A few years later, the Charing Cross Railway Company offered to buy the hospital‘s land. The health care officials at St. Thomas had to choose between rebuilding the hospital de novo at a new and potentially better site and partially rebuilding it on the existing site. The government was wary of moving the hospital from the district it had served for centuries, but Nightingale “analyzed the origins of cases served by the hospital, tabulated the proportions of cases within certain radial distances, and showed the probable effect upon patients of the removal of the hospital to several possible sites suggested.”(27) In completing all of her calculations, Nightingale found that the majority of the hospital’s admissions came from outside of the district. It was upon her recommendations then that the new St. Thomas Hospital moved from its original site and was built on the pavilion plan at Lambeth.
Nightingale believed that using evidence from statistics would enable health care providers to achieve better care in a more efficient, economical manner. From her Notes on Hospitals, she wrote, “With fixed data…we can readily obtain the proportionate mortality, not only of the whole hospital, but of every ward of it, and also the proportionate mortality and duration of cases for each age, sex, and disease. These methods, if generally used, would enable us to ascertain the mortality in different hospitals, as well as from different diseases and injuries at the same time and at different ages, the relative frequency of different diseases and injuries among the classes which enter hospitals in different countries, and in different districts of the same country. They would enable us to ascertain how much each year of life is wasted by illness—what diseases and ages press most heavily on the resources of particular hospitals.”(21) She raised many points that are currently debated regarding the use of evidence-based medicine, such as quality of care as it relates to the use of hospital resources, the cost of treatment and costbenefit analyses, all from a nation-wide standpoint.(28)
Changing concepts at the end of Nightingale’s career
At the end of her productive working life, Nightingale had established the Nightingale Training School for nurses at St. Thomas’ Hospital, later to be known as the Florence Nightingale School of Nursing and Midwifery at King’s College London. In addition to training nurses, she continued to publish dozens of books and articles on public health at the end of her career. Recognized for her pioneering work in nursing, hospital and health care reform, Nightingale was awarded the Royal Red Cross in 1883 by Queen Victoria. A the urging of King Edward VII, she also became the first woman to receive the Order of Merit in 1907.
By the end of her professional career, Nightingale’s belief in the theory of miasma was dispelled, as several of her contemporaries were providing evidence for the germ theory of disease. John Snow used statistics to prove that a contaminated water supply was the source of the 1854 cholera outbreak. In 1867 Joseph Lister published On the Antiseptic Principle in the Practice of Surgery, showing that carbolic acid could be used to sterilize surgical instruments and prevent infection. Ultimately, it wasn’t until Robert Koch’s work in the 1870–80s that Nightingale showed evidence of having accepted the germ theory. In the late 1870s, she wrote a chapter in Quain’s Medical Dictionary urging the use of antiseptics in medicine and surgery.(19, 29)
Returning to Evidence-Based Medicine Today
Well over a century before the term “evidence-based medicine” was coined, Nightingale was using statistical evidence to achieve improvements in patient care and outcomes. Just as new attention has been paid to the use of EBM in surgery today, Nightingale was also looking at statistics for surgical operations from the viewpoint of hospital economics and surgical outcomes. She presented a paper on this topic at the Berlin meeting of the International Statistical Congress in 1863.(27) In conducting this work, Nightingale cast a critical eye to the problems inherent in the use of statistics, foreseeing three of the major problems clinicians face with an epidemiological approach to medical statistics as applied to surgical outcomes: insufficient control for the type of patient, data manipulation and the use of a single outcome measure such as mortality.(30)
With regards to evidence-based approaches to surgery, Nightingale believed that “improved statistics would tell us more of the relative value of particular operations and modes of treatment than we have any means of ascertaining at present…and the truth thus ascertained would enable us to save life and suffering, and to improve the treatment and management of the sick.”(31) Even though many critics of evidence-based medicine argue that it is a poor fit for surgery and reduces the “art of medicine” by jeopardizing the personal preferences of surgeon and patient, EBM still has relevance for the field of surgery and plastic surgery in particular.(32) The American Society of Plastic Surgeons and Plastic and Reconstructive Surgery are joining the effort to promote EBM by evaluating and publishing studies with higher levels of evidence, producing tutorial guides on how to practice and teach EBM, and publishing systematic reviews and meta-analyses that synthesize the most current evidence regarding the latest plastic surgery techniques and procedures.(1) Just as Nightingale marshaled evidence and data to establish guidelines for reform, the field of Plastic Surgery must also use rigorous evidence in order to evaluate the quality of new technologies in the field. It will only be through the judicious use of this data that we may actually determine which procedures are most effective at what cost in order to improve the quality of patient care.
Acknowledgments
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (to Dr. Kevin C. Chung).
References
- 1.Chung K, Swanson J, Schmitz D, et al. Introducing evidence-based medicine to plastic and reconstructive surgery. Plast Reconstr Surg. 2009;123:1385–1389. doi: 10.1097/PRS.0b013e31819f25ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Japsen B, McCormick J, Levey N. Los Angeles Times. Los Angeles: 2009. Obama gives doctors his healthcare prescription; p. 14. [Google Scholar]
- 3.Pear R. The New York Times. Late Edition Ed. New York: 2009. U.S. to Study Effectiveness of Treatments; p. 1. [Google Scholar]
- 4.Sipkoff M. Comparative Effectiveness: An Idea Whose Time Has Finally Come. Manag Care. 2009;18:14–21. [PubMed] [Google Scholar]
- 5.McCarthy CM, Collins ED, Pusic AL. Where Do We Find the Best Evidence? Plast Reconstr Surg. 2008;122:1942–1947. doi: 10.1097/PRS.0b013e31818d2098. [DOI] [PubMed] [Google Scholar]
- 6.Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992;268:2420–2425. doi: 10.1001/jama.1992.03490170092032. [DOI] [PubMed] [Google Scholar]
- 7.Montori VM. Progress in evidence-based medicine. JAMA. 2008;300:1814. doi: 10.1001/jama.300.15.1814. [DOI] [PubMed] [Google Scholar]
- 8.Evidence-based medicine, in its place. Lancet. 1995;346:785. [PubMed] [Google Scholar]
- 9.Naylor C. Grey zones of clinical practice: some limits to evidence-based medicine. Lancet. 1995;345:840–842. doi: 10.1016/s0140-6736(95)92969-x. [DOI] [PubMed] [Google Scholar]
- 10.Sackett DL. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312:71. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung K, Shah H. Archie Cochrane and his vision for evidence-based medicine. Plast Reconstr Surg. doi: 10.1097/PRS.0b013e3181b03928. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chung KC, Ram AN. Evidence-Based Medicine: The Fourth Revolution in American Medicine? Plast Reconstr Surg. 2009;123:389. doi: 10.1097/PRS.0b013e3181934742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kudzma EC. Florence Nightingale and healthcare reform. Nurs Sci Q. 2006;19:61–64. doi: 10.1177/0894318405283556. [DOI] [PubMed] [Google Scholar]
- 14.Seymer LR. Florence Nightingale at Kaiserwerth. Am J Nurs. 1951;51:424–426. [PubMed] [Google Scholar]
- 15.Diamond M. Nightingale on Quetelet. J R Statist Soc. 1981;144:66–79. [Google Scholar]
- 16.Allen D. Florence Nightingale: Toward a Psychohistorical Interpretation. J Interdiscip Hist. 1975;6:23–54. [Google Scholar]
- 17.Dossey BM, Selanders LC, Beck DM, et al. Florence Nightingale today: Healing, leadership, global action. Silver Spring, MD: American Nurses Association; 2005. [Google Scholar]
- 18.Goldie SM. I have done my duty: Florence Nightingale in the Crimean War, 1854-56. Manchester: Manchester University Press; 1987. [Google Scholar]
- 19.Bostridge M. Florence Nightingale: the Woman and her Legend. London, New York: Viking; 2008. [Google Scholar]
- 20.Newell DJ. Present Position and Potential Developments: Some Personal Views: Medical Statistics. J R Statist Soc. 1984;147:186–197. [Google Scholar]
- 21.Nightingale F. Notes on hospitals. London: Longmans, Green & Co; 1863. [Google Scholar]
- 22.Miracle VA. The life and impact of Florence Nightingale. Dimens Crit Care Nurs. 2008;27:21–23. doi: 10.1097/01.DCC.0000304670.76251.2e. [DOI] [PubMed] [Google Scholar]
- 23.Furst LR. Between doctors and patients: the changing balance of power. Charlottesville: University of Virginia Press; 1998. [Google Scholar]
- 24.Campbell CA. The New York Times. New York: 2009. Health Outcomes Driving New Hospital Design; p. 5. [Google Scholar]
- 25.Walch JM. The effect of sunlight on postoperative analgesic medication use: a prospective study of patients undergoing spinal surgery. Psychosom Med. 2005;67:156–163. doi: 10.1097/01.psy.0000149258.42508.70. [DOI] [PubMed] [Google Scholar]
- 26.Huxley EJG. Florence Nightingale. London: Weidenfield and Nicholson; 1975. [Google Scholar]
- 27.Kopf E. Florence Nightingale as Statistician. Pub Am Stat Assoc. 1916;15:388–404. [Google Scholar]
- 28.Thompson JD. Epidemiology and Health Services Administration: Future Relationships in Practice and Education. Milbank Mem Fund Quart. 1978;56:253–273. [PubMed] [Google Scholar]
- 29.Freedman DA. From association to causation: Some remarks on the history of statistics. Stat Sci. 1999;14:243–258. [Google Scholar]
- 30.Spiegelhalter DJ. Surgical audit: statistical lessons from Nightingale and Codman. J R Statist Soc. 1999;162:45–58. [Google Scholar]
- 31.Nightingale F. Florence Nightingale on Hospital Reform. New York: Garland Publishers; 1988. [Google Scholar]
- 32.Black N. Evidence-based surgery: a passing fad? World J Surg. 1999;23:789–793. doi: 10.1007/s002689900581. [DOI] [PubMed] [Google Scholar]