Abstract
Objective. To evaluate the impact of health literacy (HL) activities incorporated into a required, first professional year (P1), patient-centered communication course on pharmacy students’ knowledge, abilities, confidence, and attitudes related to HL.
Design. Integrated, active-learning HL activities were incorporated into the course. Students’ knowledge and abilities were assessed with course evaluations. Students’ knowledge, confidence levels, and attitudes were evaluated by a precourse and postcourse survey. Third professional year (P3) students who did not complete HL activities were also surveyed.
Assessment. Almost all students “met” or “exceeded” expectations (the top 2 levels of achievement on the objective structured clinical examination (OSCE) grading rubrics) on HL course evaluations. Survey results showed significant improvement in P1 students’ knowledge, confidence, and attitudes related to HL after completing the course. First year students (postcourse) rated their confidence levels and attitudes higher than P3 students.
Conclusion. The use of integrated, active-learning activities is effective at improving P1 pharmacy students’ knowledge, abilities, confidence levels, and attitudes related to HL.
Keywords: health literacy, communication
INTRODUCTION
Health literacy (HL) is the degree to which individuals can obtain, process, understand, and communicate health-related information needed to make health decisions.1-3 Patients with low HL can have difficulty following medical instructions, understanding health information, and performing self-management tasks. Over 90 million Americans have inadequate HL skills, which can lead to poor health outcomes including increased hospitalizations, poor disease control, and poor medication adherence and self-management behaviors.1,4-7
Health care professionals must be able to identify patients with limited HL and modify communication strategies to meet their health care needs. Organizations such as the Institute of Medicine, the American Medical Association, and the American Pharmacists Association recommend that health care professional programs incorporate HL into their professional curricula.8-10 The American Pharmacists Association encourages all pharmacists and student pharmacists to increase their awareness of HL and modify communication strategies for patients with limited HL.10
Since limited HL can lead to poor outcomes, especially with regard to medication use, pharmacists can play a key role in improving health care among these patients.1 However, many pharmacists are unaware of issues related to HL or fail to make attempts to identify or assist patients with limited HL.11,12 These deficiencies could be adequately addressed through changes in pharmacy education. Both the Accreditation Council for Pharmacy Education (ACPE) and the Center for the Advancement of Pharmaceutical Education (CAPE) require pharmacy schools to address HL.13,14 Specifically, the ACPE and CAPE outcome statements mandate that pharmacy students be able to provide patient-centered care through the ability to address HL and to modify communication strategies to meet patients’ needs.13,14
A handful of studies have examined strategies to incorporate HL in pharmacy education. Sicat and Hill evaluated the impact of a 50-minute lecture and small-group active- learning activities in a communication course on P1 students’ knowledge about HL and comfort with low HL patient populations.15 Most students agreed that they had previously underestimated the prevalence of low HL in patient populations and that the activities were useful. Chen and colleagues reported that in one doctor of pharmacy (PharmD) program, as part of a required administration course, P3 students gained a greater understanding and awareness of HL issues after completing a 3-hour module and accompanying HL assignment.16 Another program examined an active-learning, multi-session HL module in a cultural competency course, which included activities such as patient counseling exercises, HL assessment, and improving the readability of education materials, improved P3 students’ knowledge and confidence.17,18 Ha and Lopez evaluated the effects of case-based learning on P3 students’ HL knowledge and skills.19 After completing one patient case that involved a patient with poor HL, the majority of students agreed that the activity was effective at meeting the HL-related learning objectives. To address a curricular mandate, these studies showed initial strategies to incorporate HL into pharmacy education. However, no study has examined P1 students’ knowledge, confidence, and attitudes regarding HL using multiple, integrated, active-learning strategies.
The University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences introduced a new curriculum in the fall of 2012. A patient-centered communication course was developed, and an HL component was included in order improve students’ knowledge and abilities in this area. The objective of this study was to evaluate the impact of the course on students’ knowledge, abilities, confidence, and attitudes regarding HL.
DESIGN
Patient-Centered Communication 1, a required, 3-credit course, is offered during the fall semester of the P1 year of the PharmD program. The course is part of a 2-course series designed to help students effectively communicate with patients, caregivers, and health care providers in order to achieve optimal patient outcomes. The course was developed in 2011-2012 and offered for the first time in 2012 as part of a renewed curriculum. The previous curriculum did not include an independent communication course. The HL portion of the course occurred during weeks 7 through 12 of the semester to partially integrate it with the self-care counseling portion of the course. The primary goals of the HL component were to improve students’ knowledge, abilities, confidence, and attitudes regarding HL and to enable students to recognize, assess, and assist patients with low HL. The course had several HL-related outcomes: (1) assess the HL level of a patient using a validated HL screening tool; (2) assess the readability level of medication-related instructions or educational materials; (3) develop easy-to-read, patient-friendly written education materials or instructions; (4) counsel a patient with low HL using effective communication techniques; and (5) modify communication strategies to meet the needs of patients with low HL.
One-hundred sixty-two students were enrolled in Patient Centered Communications 1 in the fall 2012 semester. The course was directed by 3 faculty members, one associate level professor and 2 assistant level professors. One of the 3 course directors was primarily responsible for the HL portion of the course. Students were in class for approximately 4 hours per week including 2 class sessions per week. Class time was divided as follows: (1) a 1-hour didactic session in a large classroom setting with all enrolled students focusing on introducing new information or debriefing about practice sessions or out-of-class activities; and (2) a 3-hour laboratory session in the pharmaceutical care learning center (PCLC) with half the enrolled students per session providing students with active-learning or practice opportunities in small groups. The PCLC was equipped with 42 computer stations, a mock pharmacy, and counseling rooms. Small breakout learning rooms were also used when necessary. Standardized patients were used routinely. Additionally, students were assigned to a local community pharmacy site for their introductory pharmacy practice experiences (IPPEs). Specific IPPE activities related to the course were integrated and coordinated among the course, the experiential education office, and the IPPE sites. The course also was integrated with the Pharmacotherapy Self-Care one course for some practice sessions and one evaluation. Students utilized the course website (Blackboard, Inc; Washington, DC) for course related announcements, assignments, self-study materials, and videos.
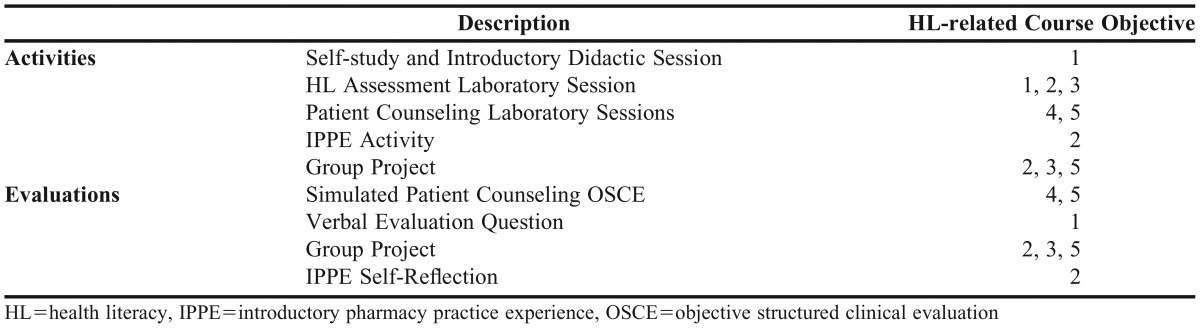
The HL component of the course included a variety of teaching and learning methods, including self-study, interactive didactic teaching, active-learning sessions, formative assessments, a group project, and experiential activities. The content originated from a national curricula model developed by the Agency for Healthcare Research and Quality (AHRQ)20 and was modified by the primary course director. Students were given multiple opportunities to practice their communication skills, both written and verbal, and to work both in groups and independently. Table 1 maps each activity to the HL-related course objectives.
Table 1.
Course Activities and Evaluations Mapped to Course Objectives
Students were introduced to HL concepts via a number of methods. First, students completed a self-study session that included a presentation via Adobe Presenter adopted from the AHRQ HL curriculum and 2 videos developed by the American College of Physicians Foundation and the American Medical Association Foundation.20-22 The self-study presentation defined HL, discussed the scope of the problem, and provided patient perspectives. After the self-study was completed, students attended a 50-minute didactic session. During this session, an interactive group discussion was held regarding the self-study assignment, and methods to identify patients with limited HL were introduced.
Laboratory sessions were designed to provide students the opportunity to apply, practice, and build upon knowledge gained from didactic sessions. In the first 3-hour laboratory session, students practiced administering 2 commonly used, valid, and reliable HL screening tools, the Newest Vital Signs (NVS), and the Rapid Estimate of Adult Literacy in Medicine (REALM).23,24 Next, students attended active-learning sessions on approaches to communicating with patients with low HL and communicating medical terminology using patient-friendly language. Students evaluated and modified medication labels, written education materials, and instructions to improve readability. Students also were introduced to and practiced using readability software.
Students completed 2 patient counseling practice laboratory sessions. The first week, students learned and practiced the basic approach to counseling a patient about a self-care product. The second week, students practiced self-care counseling with case scenarios of patients with low HL. Students were encouraged to use patient-friendly language and a slow speaking pace, to focus on 2 take-home points, and to use the teach-back method to ensure patient understanding. Both weeks, students worked in groups of 3 and received formative feedback from peers in their group. The following week, students completed formative assessments, which required students to counsel a standardized patient with low HL on a self-care product. Students received formative feedback from the standardized patient, other students, and a faculty facilitator.
The IPPE activity required students to evaluate the HL practices of their community pharmacy sites and to identify strategies to improve those practices. Students first informally assessed the pharmacy’s physical environment and staff interactions with patients. Students then used the AHRQ Pharmacy Health Literacy Assessment Tour to assess their pharmacy’s promotion of services, print materials, and clear verbal communication using a rating scale (with a 1 for something the pharmacy did not appear to be doing, 2 for something the pharmacy was doing but could make some improvements on, 3 for something the pharmacy was doing well), or N/A.20 Students also evaluated the patient-friendliness and readability of labeling of 2 self-care products. After completing the IPPE activity, students completed written self-reflections and participated in a reflective group exercise.
Students were assigned to work in small groups to design a patient-friendly education document about a common health topic for a specific population with low HL. The document needed to include a balance of pictures with text, clear language, large fonts, white space, and active voice. Examples of health topics covered included putting eye drops into a child’s eyes, quitting smoking, and recognizing signs of stroke. Students were given resources on how to design an easy-to-read document and to evaluate a document for readability level.25-29 After completing the assignment, each student group provided a peer assessment of one other group’s document.
Student achievement of HL-related course outcomes was evaluated with 2 written quizzes to assess knowledge, a simulated patient counseling OSCE to assess students’ abilities to counsel a patient with low HL, a verbal evaluation question regarding HL screening tools, the written patient education handout group project to assess students’ abilities to develop patient-friendly written material, and the IPPE self-reflection to assess students’ abilities to determine the HL friendliness of a pharmacy practice site.
The 2 quizzes were each worth 2.5% of the course grade, were comprised of multiple-choice and short-answer questions, and were administered during class time. The OSCE was worth 18% of the course grade and required students to counsel a standardized patient with low HL on a self-care product. The standardized patients, after training, completed the evaluation rubrics, which included the following specific item related to HL: “Provided patient-friendly education, used plain language a patient would likely understand, avoided medical jargon, defined medical terms, provided clear instructions, emphasized key information, avoided overloading with information, was concise, used slow pace.” The verbal evaluation question was worth 2% of the course grade and required students to answer a question related to HL assessment tools. It was graded as full credit, half credit, or no credit. The group project was worth 10% of the course grade and was graded using a standardized evaluation rubric that assessed content, organization, writing style, readability, appearance, layout, typography, and appropriateness and appeal to target audience. The IPPE assignment was worth 10% of the course grade and was graded using a standardized evaluation rubric that assessed the depth and breadth of the HL pharmacy tour and answers to reflective questions.
Confidential student information was de-identified and results were evaluated by the course directors. Student performance on HL-related course evaluations was used to assess the impact of incorporating HL content and activities on students’ skills and abilities related to HL.
The impact of the course on student confidence levels, attitudes, and knowledge was evaluated by administering a survey to the P1 students immediately before (P1 precourse) and after (P1 postcourse) the course. The survey consisted of 38 questions broken down to 7 confidence, 13 attitude, and 18 knowledge questions. In addition, the survey was administered to P3 students who did not participate in any HL activities in their curriculum or take the course. Students rated their confidence regarding HL behaviors on a 5-point Likert scale, with 1=not at all confident and 5=very confident. Attitudes regarding HL concepts were rated on a 5-point Likert scale, with 1=strongly disagree and 5=strongly agree. Knowledge was assessed using a true-false or multiple-choice format. Two comparisons of the survey data were performed, P1 precourse vs P1 postcourse responses and P1 postcourse vs P3 responses. Confidence and attitude questions were compared using the Mann-Whitney test. Knowledge questions were compared using the Chi-square test. A p value less than 0.05 was considered significant.
Additionally, P1 student perceptions about the course as a whole were assessed through standardized university course evaluations at the end of the semester. Student course evaluations consisted of 22 questions related to the perceived benefit of course outcomes, materials, structure/format, and educational activities using a 5-point Likert scale and open-ended questions regarding positive aspects of the course and suggestions for improvement. The standard student course evaluations did not specifically ask questions about the HL component of the course. This study was approved by the Colorado Multiple Institutional Review Board.
EVALUATION AND ASSESSMENT
For the patient counseling OSCE, all students (n=162) “met or exceeded expectations” based on the grading rubric. Of the 162 students, 150 (92.6%) provided patient-friendly education in plain language “most of the time,” and 12 did (7.4%) “some of the time.” For the verbal question regarding HL assessment tools, 109 students (67%) received full credit, 34 students (21%) received half credit, and 19 (12%) received no credit. The average scores on the 2 quizzes were 77% and 80%, with 83% and 76% of students scoring 70% or higher. For the group project, the average score was 89.9% (range 78-99%) based on the grading rubric. Overall, 30 groups met or exceeded expectations, and one group met expectations with limitations. Twenty-nine groups met or exceeded expectations on the readability criteria of the document (eg, easy to understand, uses common words and short sentences, no technical jargon, appropriate reading level). Two groups met the readability expectations with limitations. Thirty groups met or exceeded expectations on the text appearance criteria (eg, uncluttered, ample white space, appropriate font, serif type, use of subheadings); 3 groups met expectations with limitations. Twenty-eight groups met or exceeded expectations on the visuals criteria (eg, symbols used sparingly, purposeful and easily understood graphs and illustrations, instructive rather than decorative visuals); 5 groups met expectations with limitations. The average score on the IPPE activity self-reflection was 89% with 91% of students scoring 70% or higher.
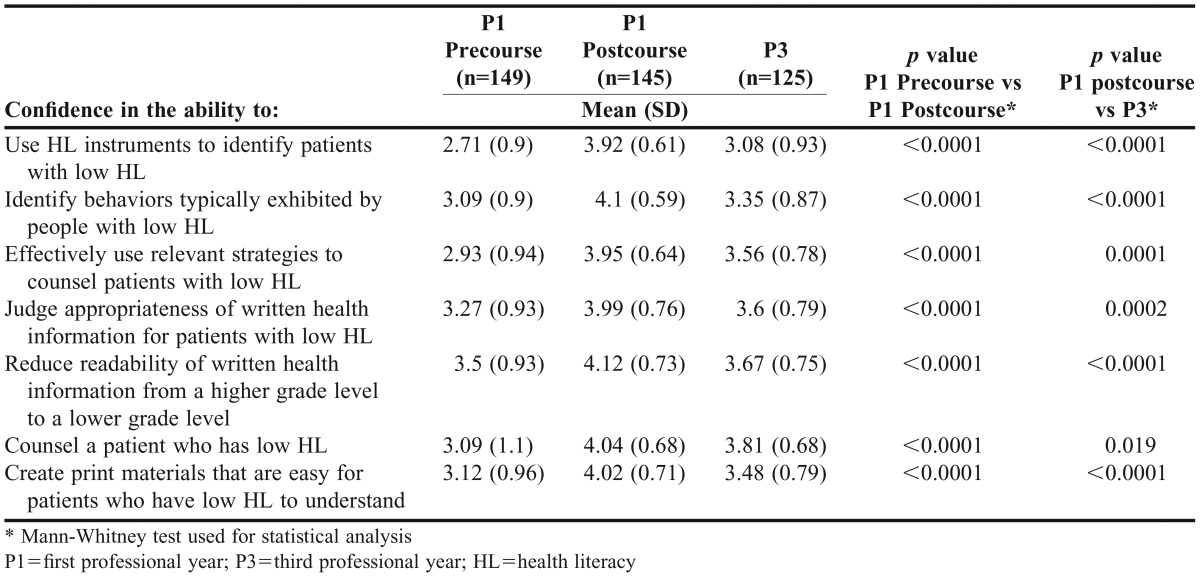
Students who completed the course had significant increases in confidence levels regarding HL (Table 2). All postcourse confidence scores in each of the 7 questions significantly improved from baseline (p<0.001 for all). Students who completed the course had significantly higher confidence levels in each of the 7 questions compared to P3 students who did not take the course (p<0.05 for all). Students felt more confident identifying behaviors exhibited by patients with low HL and using screening instruments to identify such patients. Students felt more confident counseling patients with low HL using relevant strategies. Students also were more confident in their ability to judge the appropriateness of written information, reduce readability levels from a higher grade to a lower one, and create easy-to-understand print materials.
Table 2.
Student Confidence Levels in HL-related Abilities
Student attitudes were generally appropriate (either positive or negative depending on the context of the question) both precourse and postcourse (Table 3). Student attitudes improved in 6 of the 13 questions from precourse to postcourse. Importantly, attitudinal improvement could be a shift either up or down the Likert scale, depending on the specific question. After the completion of the course, fewer students agreed with the following statements, “Patients who have trouble reading prescription labels will ask their pharmacist for help,” (p=0.008), “Pharmacy labels are written to be easily understood,” (p<0.0001), and “Warning labels are a clear and concise way to communicate potential side effects to patients” (p<0.0001). After completing the course, more students agreed with the statement, “Pharmacists should find out if their patients have reading difficulties” (p=0.002). Fewer students agreed with the statement “Pharmacists should ask patients, ‘Do you understand?’ or ‘Do you have questions?’” (p<0.0001). These changes all show an improvement in attitudes, with the last statement showing that more students, after completing the course, were more familiar with the shortcomings of close-ended questions to assess patient understanding.
Table 3.
Student Attitudes Toward HL-related Statements
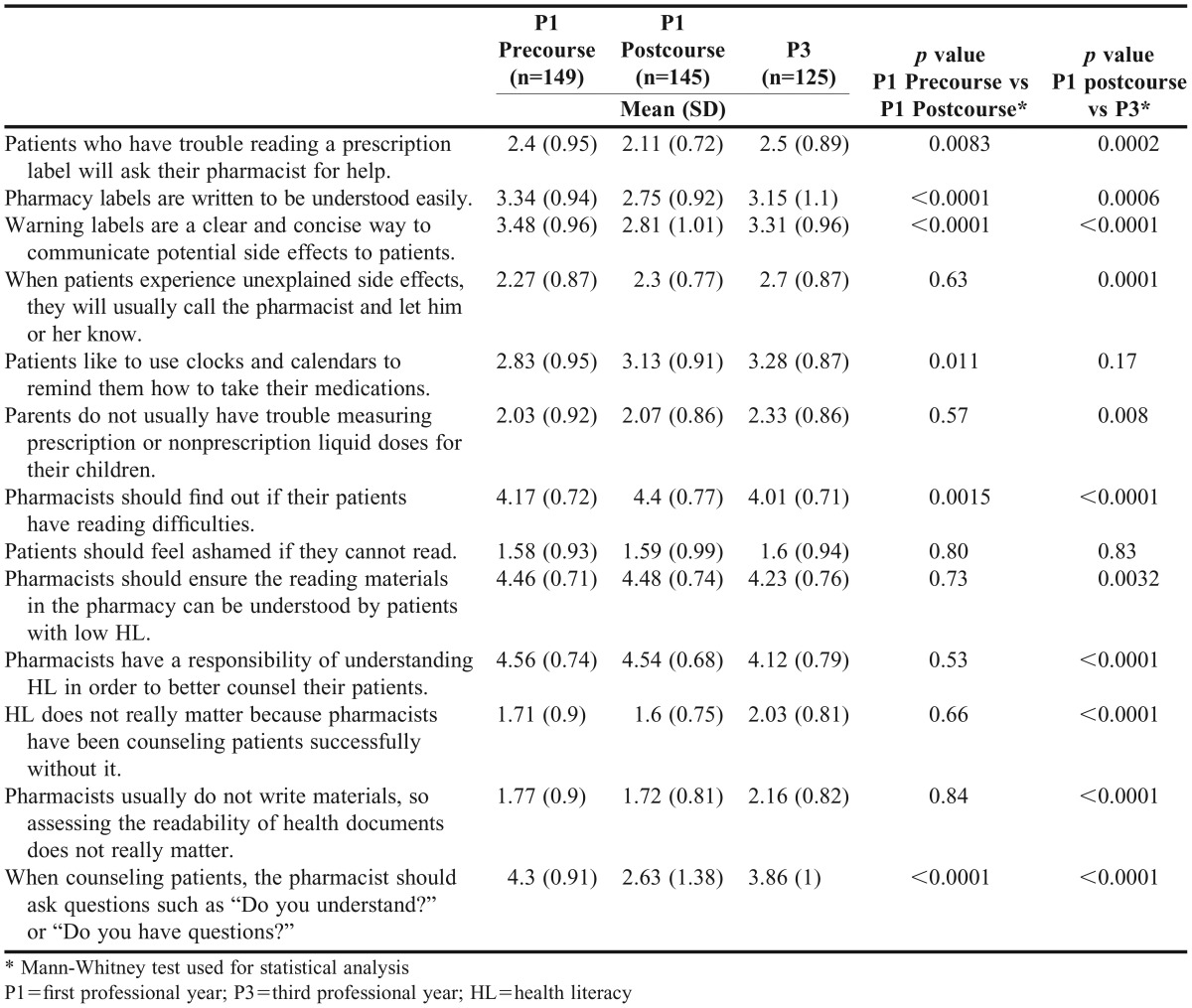
Attitudinal responses of the P1 students’ (postcourse) were more positive than the P3 students for 11 of the 13 questions (Table 3). In addition to the 6 statements above, fewer P1 students agreed than P3 students with the following statements: “When patients experience unexplained side effects, they will usually call the pharmacist and let him or her know” (p=0.0001); “Parents do no usually have trouble measuring prescription or nonprescription liquid doses for their children” (p=0.008); “HL does not really matter because pharmacists have been counseling patients successfully without it” (p<0.0001); and “Pharmacists usually do not write materials, so assessing the readability of health documents does not really matter” (p<0.001). The P1 students (postcourse) agreed more than P3 students with the statements “Pharmacists should ensure the reading materials in the pharmacy can be understood by patients with low HL” (p=0.003), and “Pharmacists have a responsibility of understanding HL in order to better counsel their patients” (p<0.0001).
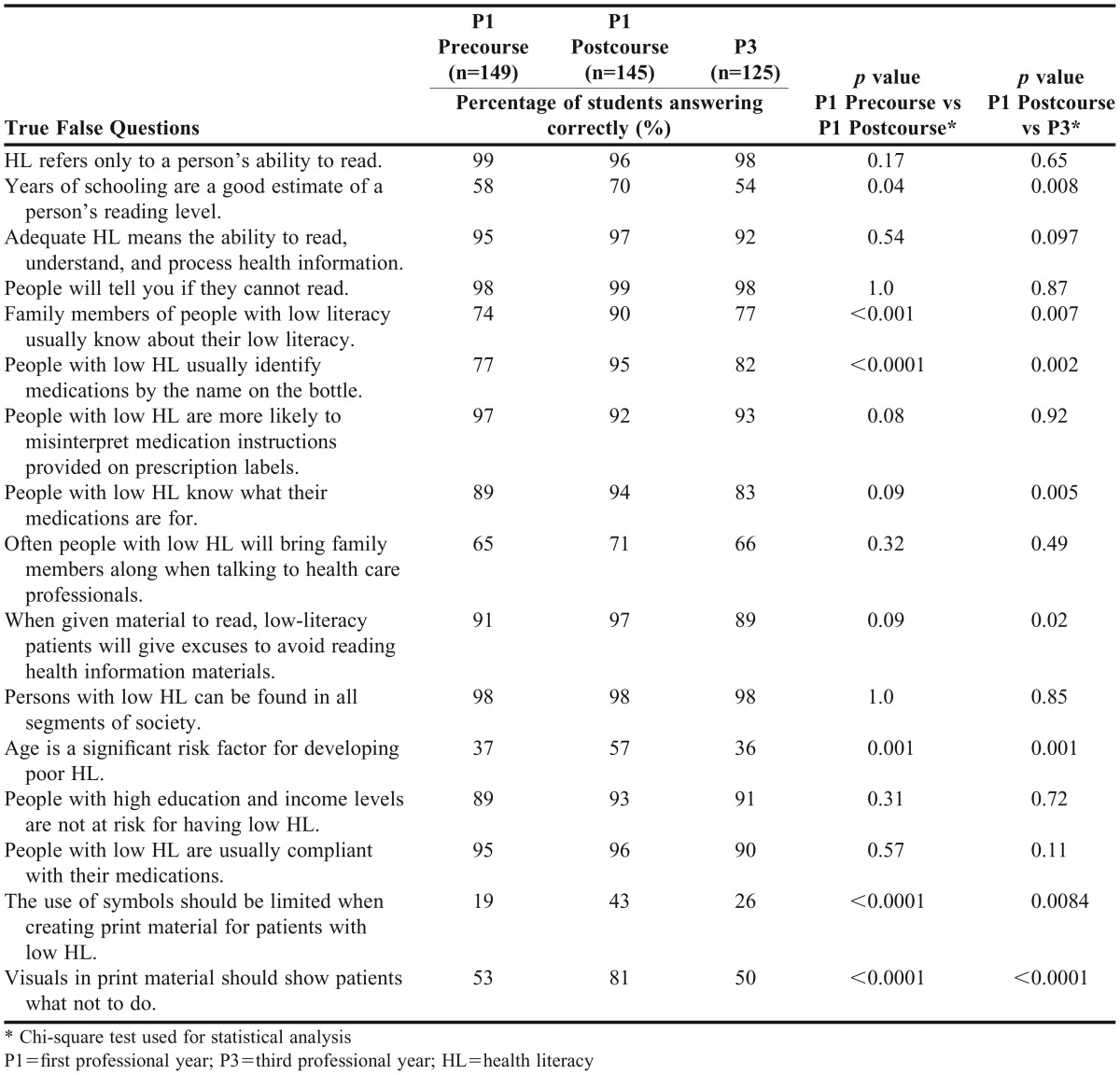
Scores improved in 6 of the 18 knowledge questions from baseline (Table 4). However, most of the precourse scores were already high. Students scored significantly higher with the statements “Family members of people with low literacy usually know about their low literacy,” (p<0.0001) and “People with low HL usually identify medications by the name on the bottle” (p<0.0001). Students demonstrated learning by recognizing age as an important factor among those with low HL (p=0.001). Students also demonstrated increased knowledge in terms of print materials. Specifically, at the end of the course, students understood that use of symbols should be limited when creating print materials for patients with low HL (p<0.0001), and visuals should show patients what to do, as opposed to what not to do (p<0.0001). Knowledge scores were similar between P1 students’ precourse and P3 students for all questions.
Table 4.
Percentage of Students Answering HL Knowledge Questions Correctly
One hundred fifty students (93%) completed the standard course evaluation. Mean scores ranged from 3.6 to 4.2 on the 5-point Likert scale. Eighty-two percent of students strongly agreed or agreed that the course was designed in a manner to meet the course outcomes. Eighty-five percent of students strongly agreed or agreed that the course helped them meet expectations for professional behavior. Seventy-five percent strongly agreed or agreed that the active-learning strategies used in the class helped them meet course objectives. Seventy-five percent strongly agreed or agreed that a variety of learning strategies were offered to stimulate learning. Eighty-one percent strongly agreed or agreed that the course was made relevant to the practice of pharmacy.
DISCUSSION
This integrated approach to teaching and learning HL was effective at improving attitudes and confidence in P1 students, who demonstrated greater confidence in all 7 key areas from precourse to postcourse. Certain P1 student attitudes improved from precourse to postcourse, especially regarding print materials and recognizing specific patient risk factors for low HL. Additionally, the majority of P1 students were successful during the patient counseling, verbal question, and group project components of the course. After completing the course, P1 students’ knowledge, confidence levels, and attitudes were more positive than those of the P3 students, who did not have formal education related to HL. These results built upon previously conducted studies regarding health literacy in pharmacy education.17,18 Devraj and colleagues concluded that active-learning health literacy activities in a P3 cultural competency course improved students’ knowledge and confidence in their ability to care for patients with low health literacy.18 Our results indicated similar positive results in knowledge and confidence in P1 students, which suggests that this content could successfully be introduced earlier in the curriculum. In addition, our study showed improvement in students’ attitudes about patient health literacy.
It was interesting to note how similar the P3 survey results were to the P1 precourse results, especially in terms of knowledge and confidence. These results indicate that HL concepts and skills cannot be gained systematically by all students through typical pharmacy experiences, such as IPPEs or other courses. In terms of student attitudes, P3 student responses demonstrated more negative attitudes regarding HL than responses from either precourse and postcourse P1 students. Compared to P1 students, more P3 students felt pharmacists did not have a responsibility to understand HL, and more P3 students felt that assessing readability of documents and ensuring documents could be understood patients with low HL did not matter. These attitudes extended to patient care as well. Compared to P1 students, more P3 students felt that parents did not have trouble measuring medications for their children and that if patients had unexplained side effects, they would call their pharmacists. We believe these attitudes are most likely due to a lack of awareness regarding the high prevalence and health-related consequences of low HL and could be improved by including HL as a required component of a pharmacy curriculum. These attitudinal responses regarding HL from P3 students could also indicate that students become more resistant to HL concepts as they progress through their pharmacy program and HL content should be formally introduced and taught early in the pharmacy curriculum. Importantly, the survey results seem to indicate that students simply cannot assimilate knowledge, improve attitudes, or gain confidence regarding HL through other courses or experiences.
This study demonstrated several key strengths. First, many of the course activities were adapted from the AHRQ HL curriculum, and students were introduced to validated HL screening tools such as NVS and REALM. These activities and tools can easily be accessed and used by other pharmacy programs. Second, this course incorporated a multi-dimensional approach to teaching, learning, and assessing HL content. Learning activities included large and small group activities, multiple practice sessions with a variety of case scenarios, formative assessments, interactions with standardized patients, a group project, IPPE activities, written and verbal self-reflections, and peer evaluations. Many activities were also integrated with another course, Self-Care Pharmacotherapy. This multi-dimensional, active-learning approach enhanced students’ confidence, possibly because they were able to practice their understanding of HL multiple times in various ways. Finally, because the pharmacy school’s curriculum changed, we were able to make a comparison between P1 students enrolled in the course and P3 students, who had never been formally introduced to any required content regarding HL.
While most previously published studies focused on incorporating HL teaching and learning into P3 coursework,16-19 we believe that the P1 year is an appropriate point in the curriculum to introduce HL. However, key concepts should be reinforced throughout the curriculum. If students are more aware of HL issues at the beginning of their program, they may be more likely to appropriately base their counsel during IPPEs and advanced pharmacy practice experiences (APPEs) on these experiences, making them more enriching and rewarding.
The study had several limitations. First, students did well on the knowledge survey data precourse, so there was little room for improvement postcourse. There was no information regarding students’ precourse skill data (such as OSCEs or written group projects) to compare to postcourse skill data. Second, the survey was subjected only to face validity. However, it was adapted with permission from Devraj and colleagues, thereby increasing the validity.18 Students scored similarly in knowledge in both studies, even though our study assessed P1 students and Devraj and colleagues’ study assessed P3 students. This may indicate that the knowledge portion of the survey is too simple. Finally, the study only included students from one institution, which limits the generalizability of the results.
Future studies may want to examine how HL content and skills are reinforced and how students retain knowledge and demonstrate confidence regarding HL throughout their curriculum, especially during APPEs. Studies could be conducted to determine if students who learn about HL incorporate the concepts into future pharmacy practice. Further research could also examine an interprofessional approach to HL in different practice settings.
SUMMARY
An integrated approach to teaching and learning HL in a PharmD program was effective at improving P1 students’ abilities, skills, attitudes, and confidence related to HL. Identifying patients with low HL and tailoring communication strategies to them are essential components to any patient care practice. Introducing HL concepts early in the curriculum allows students the opportunity to practice and gain confidence throughout their program. We developed a comprehensive introduction to this important content area, which can be transferred easily to other institutions.
REFERENCES
- 1.Agency for Healthcare Research and Quality (2011). Health literacy interventions and outcomes: an updated systematic review. Evidence report, technology assessment number 199. http://www.ahrq.gov/downloads/pub/evidence/pdf/literacy/literacyup.pdf. Accessed February 6, 2014.
- 2.Kutner M, Greenberg E, Baer J. Washington, DC: National Center for Education Statistics, US Department of Education; 2005. A first look at the literacy of America’s adults in the 21st century. [Google Scholar]
- 3.Kirsch IS, Jungeblut A, Jenkins L, Kolstad A. Adult literacy in America: a first look at the national adult literacy survey. Jessup, MD: National Center for Education Statistics; 1993. NCES publication no. 93275.
- 4.Consumer Health Informatics Research Resource (CHIRr) http://chirr.nlm.nih.gov/health-literacy.php. Accessed February 6, 2014.
- 5.Cavanaugh K, Huizinga MM, Wallston KA, et al. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- 6.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 7.Marden S, Thomas PW, Sheppard ZA, et al. Poor numeracy skills are associated with glycaemic control in type 1 diabetes. Diabet Med. 2012;29(5):662–669. doi: 10.1111/j.1464-5491.2011.03466.x. [DOI] [PubMed] [Google Scholar]
- 8.American Medical Association. Health literacy: report of the council on scientific affairs Ad hoc committee of health literacy for the council on scientific affairs. JAMA. 1999;281(16):552–557. [PubMed] [Google Scholar]
- 9.Institute of Medicine 2004Health literacy: a prescription to end confusion Washington DC: National Academies Press; 2004 [PubMed] [Google Scholar]
- 10.Report of the 2002 APhA House of Delegates. Actions of the official legislative body of the American Pharmaceutical Association. J Am Pharm Assoc. 2002;42(5s1):S60–S63. [Google Scholar]
- 11.Praska JL, Kripalani S, Seright AL, Jacobson TA. Identifying and assisting low-literacy patients with medication use: a survey of community pharmacies. Ann Pharmacother. 2005;39(9):1441–1445. doi: 10.1345/aph.1G094. [DOI] [PubMed] [Google Scholar]
- 12.Shoemaker SJ, Staub-DeLong L, Wasserman M, Spranca M. Factors affecting adoption and implementation of AHRQ health literacy tools in pharmacies. Res Soc Adm Pharm. 2013;9(5):553–563. doi: 10.1016/j.sapharm.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 13. ACPE Accreditation Standards and Guidelines Revised Pharm D Standards. Adopted January 23, 2011. www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0pdf. Accessed February 6, 2014.
- 14.Medina MS, Plaza CM, Stowe CD, et al. Center for the Advancement of Pharmacy Education. 2013 Educational Outcomes. Am J Pharm Educ. 2013;77(8):Article 162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sicat BL, Hill LL. Enhancing student knowledge about the prevalence and consequences of low health literacy. Am J Pharm Educ. 2005;69(4):460–466. [Google Scholar]
- 16.Chen AM, Noureldin M, Plake KS. Impact of a health literacy assignment on student pharmacist learning. Res Soc Admin Pharm. 2013;9(5):531–541. doi: 10.1016/j.sapharm.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 17.Poirier TI, Butler LM, Devraj R, Gupchup GV, Santanello C, Lynch JC. A cultural competency course for pharmacy students. Am J Pharm Educ. 2009;73(5):Article 81. doi: 10.5688/aj730581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Devraj R, Butler LM, Gupchup GV, et al. Active learning strategies to develop health literacy knowledge and skills. Am J Pharm Educ. 2010;74(8):Article 137. doi: 10.5688/aj7408137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ha H, Lopez T. Developing health literacy knowledge and skills through case-based learning. Am J Pharm Educ. 2014;78(1):Article 17. doi: 10.5688/ajpe78117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Advancing Pharmacy Health Literacy Practices Through Quality Improvement: Curricular Modules for Faculty. December 2011. Agency for Healthcare Research and Quality. http://www.ahrq.gov/professionals/education/curriculum-tools/pharmlitqi/index.html. Accessed April 4, 2014.
- 21.The American College of Physicians Foundation. Health Literacy Video. http://www.acponline.org/multimedia/?bclid=782539368001&bctid=790962260001. Accessed April 9, 2014.
- 22.American Medical Association Foundation. Health Literacy Program Video: Health literacy and patient safety: Help patients understand. 2007. https://www.youtube.com/watch?v=cGtTZ_vxjyA. Accessed April 9, 2014.
- 23.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult health literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391–395. [PubMed] [Google Scholar]
- 25.Agency for Healthcare Research and Quality. Health Literacy Toolkit; Rockville, MD: 2011. http://www.ahrq.gov/qual/literacy/healthliteracytoolkit.pdf. Accessed: August 22, 2014. [Google Scholar]
- 26.U.S. Department of Health and Human Services. Center for Disease Control and Prevention. Simply Put: a guide for creating easy-to-understand materials. http://www.cdc.gov/healthliteracy/pdf/Simply_Put.pdf. Accessed: August 22, 2014.
- 27.National Center for Health Marketing. Plain Language Thesaurus for Health Communications. http://depts.washington.edu/respcare/public/info/Plain_Language_Thesaurus_for_Health_Communications.pdf. Accessed: August 22, 2014.
- 28.Doak CC, Doak LG, Root JH. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1996. Teaching patients with low literacy skills; pp. 41–60. [Google Scholar]
- 29.Readability Formulas. http://www.readabilityformulas.com/free-readability-formula-tests.php. Accessed: August 22, 2014.


