Abstract
Background
Patients with indeterminate form of Chagas disease/cardiac normality (ICD/CN) exhibited normal electrocardiograms and chest X-rays; however, more sophisticated tests detected some degree of morphological and functional changes in the heart.
Objective
To assess the prevalence of systolic and diastolic dysfunction of the right ventricle (RV) in patients with ICD/CN.
Methods
This was a case–control and prevalence study. Using Doppler two-dimensional echocardiography (2D), 92 patients were assessed and divided into two groups: group I (normal, n = 31) and group II (ICD/CN, n = 61).
Results
The prevalence of RV systolic dysfunction in patients in groups I and II was as follows: fractional area change (0.0% versus 0.6%), mobility of the tricuspid annulus (0.0% versus 0.0%), and S-wave tissue Doppler (6.4% versus 26.0%, p = 0.016). The prevalence of global disorders such as the right myocardial performance index using tissue Doppler (16.1% versus 27.8%, p = 0.099) and pulsed Doppler (61.3% versus 68%, p = 0.141) and diastolic disorders such as abnormal relaxation (0.0% versus 6.0%), pseudonormal pattern (0.0% versus 0.0%), and restrictive pattern (0.0% versus 0.0%) was not statistically different between groups.
Conclusion
The prevalence of RV systolic dysfunction was estimated to be 26% (S wave velocity compared with other variables), suggesting incipient changes in RV systolic function in the ICD/CN group.
Keywords: Chagas Disease; Ventricular Dysfunction Right; Echocardiography, Doppler
Introduction
Chagas disease is an infection caused by the protozoa Trypanosoma cruzi, discovered by Carlos Chagas in 19091,2.
This disease presents in three stages: acute, chronic indeterminate (ICD) and chronic (in the following variants: cardiac, digestive, cardio–digestive, and the nervous system)3,4.
The indeterminate stage was defined as the presence of T. cruzi infection and the absence of clinical, radiological, and electrocardiographic indications of cardiac or digestive involvement5. Half of the patients infected in endemic areas fall in this ICD stage, and although the principal characteristic of these patients is the absence of these abnormalities, morphofunctional cardiac alterations are observed when using other complementary methods such as exercise testing6, dynamic electrocardiography7, noninvasive autonomic tests8, radionuclide ventriculography9, and echocardiography10.
Doppler echocardiogram is a noninvasive heart assessment method, and various morphological and functional analyses of patients with Chagas disease have demonstrated the usefulness of M mode11 and 2-D in analyzing global and segmental contractility of the ventricles as well as systolic and diastolic left and right ventricular function and detecting thrombi and aneurysms12,13.
In Chagas disease, RV involvement appears early and frequently14. Although echocardiography is a noninvasive and versatile diagnostic tool for assessing cardiac morphology and function, RV assessment is technically limited and subjective. In 2010, guidelines were published15 with quantitative suggestions for analyzing systolic and diastolic RV function.
The present study aimed to determine the prevalence of early systolic and diastolic RV dysfunction in adult patients with ICD/CN, according to the recommendations of the aforementioned guidelines15.
Methods
Description of the study
This was an observational, epidemiological case–control study, with descriptions and prevalence16, approved in 2011 by the HC-UFG Ethics and Research Committee.
Patients
The patients were selected and divided in a nonblinded manner into two groups. The patients selected for group I (n = 31) were without previous pathologies, blood donors, and with normal results for electrocardiogram (ECG), hemoglobin (HB), creatinine (CT), thyroid-stimulating hormone (TSH), and glucose (G) levels as well as nonreactive indirect immunofluorescence serology (IgG IFI)17 for Chagas disease.
Patients selected for group II (n = 61) were diagnosed with ICD/CN (regardless of origin, the patients did not undergo proctological evaluation to rule out intestinal involvement) and were seen on an outpatient basis at the HC-UFG Chagas and cardiology clinic; they had the following test results:
Normal ECG and chest X-ray.
Reactive serology for Chagas disease using two of the following three tests: IgG IFI17, enzyme-linked immunosorbent assay (ELISA)17, and hemagglutination inhibition (HAI)17.
Normal CT, G, TSH, and HB levels.
The free and informed consent form (ICF) was signed by all patients or legal guardians.
Exclusion criteria
Inadequate cardiac window
Systemic arterial hypertension (SAH).
Pregnancy.
Chronic alcoholism.
Hematologic, thyroid, and rheumatic diseases.
Diabetes mellitus and glucose intolerance.
Kidney and liver diseases.
Heart and lung diseases of any etiology.
Inability to sign the consent form.
Age < 18 years.
Echocardiographic assessment
Echocardiography was performed using an Xsario device (Toshiba), with images being digitally recorded; it was performed by a single observer. Each measurement for the variable was obtained in the online mode as the average of three consecutive beats in regular sinus rhythm18,19. Images were recorded in parasternal longitudinal planes, transverse short axis, and apical two-, three-, and four-chamber (A4C) views 20.
The parameters for RV systolic function were as follows: tricuspid annulus movement (TAM), calculation of fractional area change (FAC), and systolic velocity (S wave) obtained by tissue Doppler (TD)15.
TAM is a method that estimates the distance of systolic excursion of the lateral tricuspid valve annulus and should be obtained using the M-mode cursor in the longitudinal A4C view, measuring the largest longitudinal displacement of the tricuspid base toward the apex during systole15,21.
FAC is defined as follows: end diastolic area (RV EDA) − end systolic area (RV ESA)/(EDA × 100). FAC measures RV systolic function with a good correlation with ejection fraction (RVEF) estimated by nuclear magnetic resonance (NMR)15,22,23. It was performed by tracing the RV endocardial edge in the telediastole and telesystole.
TD of the lateral annulus in the basal segment of the RV free wall provides the longitudinal velocity of the systolic excursion wave (S wave), and it was conducted in the A4C window obtained by pulsed Doppler (PD) in the middle of the basal portion of the free wall, being relevant and reproducible15.
The right myocardial performance index (RMPI) represents the overall index of systolic and diastolic function, defined by the following ratio: isovolumetric relaxation time (IVRT) and contraction time (IVCT) divided by ejection time (ET), or [(IVRT + IVCT)/ET]. The opening and closing time (OCT) is IVCT + ET + IVRT. RMPI can be obtained by two methods: PD and TD. In PD, ET was measured in the RV outflow tract at the level of the pulmonary valve and OCT was measured at the level of the tricuspid valve. In TD, ET was estimated using the duration of the S wave and OCT was measured using the duration of the time from the end of the late expansion wave (a') to the beginning of the initial expansion wave (e')15,24.
Analysis of RV diastolic function was performed in the A4C window by PD aligned parallel to the tricuspid flow, placing the sample volume at 1 cm from the tip of the leaflets of the tricuspid valve25, and measurements were performed at the end of expiration26. E and A waves were measured along with the E/A ratio, deceleration time (DT), and IVRT. In addition, e' and a' waves as well as e'/a' and E/e' ratios were assessed using TD.
The area (RAA) and volume of the right atrium (RAV) were obtained in the A4C window using planimetry15,27 and the Simpson method28, respectively.
The right atrial pressure (RAP) was assessed by measuring the diameter of the inferior vena cava (IVC) in the subcostal projection (JSC) at 0.5–3.0 cm from the RA ostium at the end of expiration as well as the estimated inspiratory collapse (CIVC)15,29,30.
RA inflow was observed using subcostal projection at the level of the hepatic vein31 because for normal or low RAP, the predominance of systolic wave velocity (Vs) is greater than that of diastolic wave velocity (Vd). When RAP is elevated, Vs decreases in the ratio Vs/Vd < 115. The fraction of hepatic vein diastolic filling is the ratio Vs/Vs + Vd, and the value < 55% was the most sensitive and specific finding for elevated RAP15,32,33.
The systolic pulmonary artery pressure (SPAP) was estimated from the measurement of the velocity of the tricuspid regurgitant jet with the addition of RAP because there was no obstruction of the right ventricular outflow15,34.
Echocardiographic criteria
The definition of systolic and diastolic dysfunction of RV was based on one of the following criteria15:
1. Systolic dysfunction:
RMPI > 0.40 by PD and > 0.55 by TD.
TAM < 16 mm.
FAC < 35%.
S < 10 cm/s.
2. Diastolic dysfunction:
Statistical analysis
Data were entered and analyzed in the Statistical Package for Social Sciences (SPSS) (17.0) software program. Continuous quantitative variables were expressed as means and standard deviation, and categorical variables were expressed as frequency and percentage. The Komolgorov–Smirnov test was used to assess whether the continuous quantitative variables presented normal distribution. When the variables and the groups they showed normal distribution, Student's t-test was used; when they did not, the Mann–Whitney test was used. To compare discrete variables as well as the groups, Fisher's exact test was used. For all analyses, a 95% confidence level was used (p < 0.05 as significant).
Considering that there are five new cases per week of patients with ICD referred to the Chagas clinic, it was estimated that during the period of data collection (32 weeks), the presumed population would be 130 patients. With a 5% significance level, test power of 80%, and 5% margin of error, the sample size would be 92 patients, divided into 31 for group I and 61 for group II.
Results
Of the 92 patients evaluated, the mean and standard deviation for the variables of general and echocardiographic characteristics between groups I and II are shown in Tables 1 and 2, respectively.
Table 1.
General characteristics of normal patients and patients with ICD/CN
| Variables | Group | p | |
|---|---|---|---|
| Normal (n = 31) | ICD/CN (n = 61) | ||
| Age (years)* | 45.32 ± 12.36 | 39.73 ± 12.94 | 0.071 |
| Weight (kg)* | 67.66 ± 12.37 | 71.29 ± 14.91 | 0.270 |
| Height (cm)* | 156.88 ± 30.56 | 159.24 ± 32.63 | 0.749 |
| BSA* | 1.69 ± 0.19 | 1.77 ± 0.24 | 0.174 |
| HR* | 70.36 ± 9.83 | 71.90 ± 10.43 | 0.509 |
| LVDD* | 47.05 ± 5.22 | 46.71 ± 5.21 | 0.779 |
| LVEF (Teichholz)* | 73.56 ± 7.35 | 73.55 ± 6.66 | 0.996 |
| Sex (female)** | 24/77.4% | 45/73.8% | 0.190 |
Student’s t-test;
Fisher’s exact test.
Cm: centimeters; LVDD: LV diastolic dimension in millimeters; HR: heart rate, beats per minute; LVEF: left ventricular ejection fraction, %; ICD/CN: indeterminate form of Chagas disease/cardiac normality; BSA: body surface area; kg: kilogram.
Table 2.
Comparison of echocardiographic variables between groups I (normal) and II (ICD/CN)
| Variables | Group | p | |||
|---|---|---|---|---|---|
| n | Normal (n = 31) | n | FIDC/NC (n = 61) | ||
| RV EDA2 | 30 | 15,53 ± 8,17 | 61 | 12,41 ± 3,28 | 0,026* |
| RV ESA1 | 30 | 6,85 ± 2,39 | 61 | 6,22 ± 1,54 | 0,199 |
| RAA1 | 31 | 10,72 ± 2,04 | 59 | 10,89 ± 2,64 | 0,741 |
| IVC1 | 30 | 15,83 ± 2,91 | 54 | 14,91 ± 3,82 | 0,219 |
| CIVC1 | 30 | 8,21 ± 2,83 | 55 | 7,45 ± 2,34 | 0,218 |
| RAP1 | 30 | 5,00 ± 0,00 | 58 | 5,10 ± 0,55 | 0,309 |
| SPAP1 | 11 | 18,06 ± 9,02 | 27 | 19,73 ± 10,18 | 0,623 |
| RAV1 | 30 | 24,16 ± 7,90 | 58 | 23,74 ± 8,64 | 0,820 |
| IRVV1 | 24 | 14,34 ± 4,45 | 50 | 13,49 ± 6,12 | 0,499 |
| TAM1 | 31 | 23,74 ± 3,33 | 61 | 23,67 ± 3,83 | 0,927 |
| ET using TD1 | 31 | 283,95 ± 36,08 | 61 | 284,79 ± 35,44 | 0,915 |
| OCT using TD1 | 31 | 409,98 ± 42,35 | 61 | 425,23 ± 43,21 | 0,110 |
| RMPI using TD2 | 31 | 0,46 ± 0,17 | 61 | 0,51 ± 0,21 | 0,159 |
| ET using PD1 | 31 | 298,05 ± 28,39 | 60 | 300,23 ± 33,90 | 0,747 |
| OCT using PD1 | 31 | 419,23 ± 32,41 | 60 | 442,41 ± 35,78 | 0,003* |
| RMPI using PD1 | 31 | 0,41 ± 0,08 | 60 | 0,49 ± 0,20 | 0,037* |
| FAC1 | 30 | 0,54 ± 0,08 | 61 | 0,50 ± 0,07 | 0,014* |
| S wave1 | 31 | 11,73 ± 1,64 | 61 | 10,98 ± 1,83 | 0,051 |
| E1 | 31 | 49,89 ± 12,40 | 61 | 47,37 ± 9,53 | 0,324 |
| A1 | 31 | 29,19 ± 7,33 | 61 | 30,95 ± 9,95 | 0,339 |
| E/A1 | 31 | 1,83 ± 0,71 | 61 | 1,69 ± 0,62 | 0,355 |
| DT1 | 31 | 214,77 ± 78,36 | 61 | 240,30 ± 61,90 | 0,120 |
| e'1 | 31 | 13,09 ± 3,18 | 61 | 11,20 ± 2,65 | 0,006* |
| a'1 | 31 | 10,85 ± 3,43 | 61 | 11,31 ± 3,73 | 0,550 |
| e'/a'2 | 31 | 1,71 ± 2,49 | 61 | 1,08 ± 0,40 | 0,034* |
| E/e'1 | 31 | 4,02 ± 1,29 | 61 | 4,43 ± 1,18 | 0,149 |
| Vs1 | 19 | 49,83 ± 26,39 | 36 | 54,71 ± 23,41 | 0,503 |
| Vd1 | 19 | 36,56 ± 19,75 | 36 | 38,09 ± 18,08 | 0,780 |
| Vr1 | 19 | 23,71 ± 6,82 | 36 | 24,93 ± 9,27 | 0,582 |
| Vs (Vs + Vd)1 | 19 | 0,57 ± 0,06 | 35 | 0,57 ± 0,13 | 0,979 |
Variables with normal distribution: Student’s t-test.
Variables not showing normal distribution: Mann–Whitney test.
A: late diastolic wave; a': late diastolic wave in TD; RAA: right atrial area; RV EDA: end diastolic area of the right ventricle; RV ESA: end systolic area of the RV; CIVC: collapsed inferior vena cava; TD: tissue Doppler; PD: pulsed Doppler; E: initial diastolic wave; e': initial diastolic wave in TD; RMPI: right myocardial performance index; FAC: fractional area change; TAM: tricuspid annulus movement; S wave: systolic wave in TD; RAP: right atrial pressure; SPAP: systolic pulmonary artery pressure; DT: deceleration time; ET: ejection time; OCT: opening and closing time; RAV: right atrial volume; IVC: inferior vena cava; Vd: diastolic wave velocity; RAVI: right atrial volume index; Vr: reverse diastolic velocity of the hepatic vein; Vs: systolic wave velocity.
Parameters for RV systolic function (EDA, ESA, FAC, TAM, and S wave), indices such as RMPI (ET and OCT in TD or PD), diastolic function (E and A waves, DT, e' and a' waves, E/A, e'/a', and E/e' ratios, Vs, Vd, Vr, and (Vs/Vs + Vd), as well as the dimensions of RA and IVC for groups I and II are described in Table 2 (measurements conducted in the online mode).
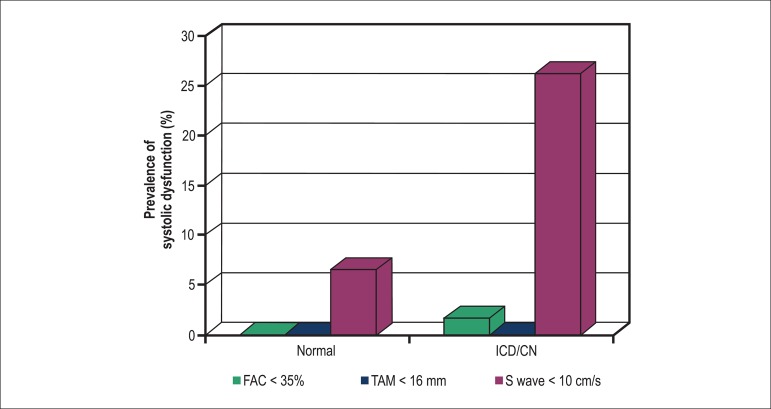
The prevalence of RV systolic dysfunction in both groups was as follows: FAC (0.0% versus 0.6%), TAM (0.0% versus 0.0%), and S wave (6.4% versus 26.0% with p = 0.016), as seen in Figure 1.
Figure 1.
Prevalence of RV systolic dysfunction. ICD/CN: indeterminate form of Chagas disease/cardiac normality; S wave: systolic S wave velocity in tissue Doppler; FAC: fractional area change; TAM: tricuspíd annulus movement.
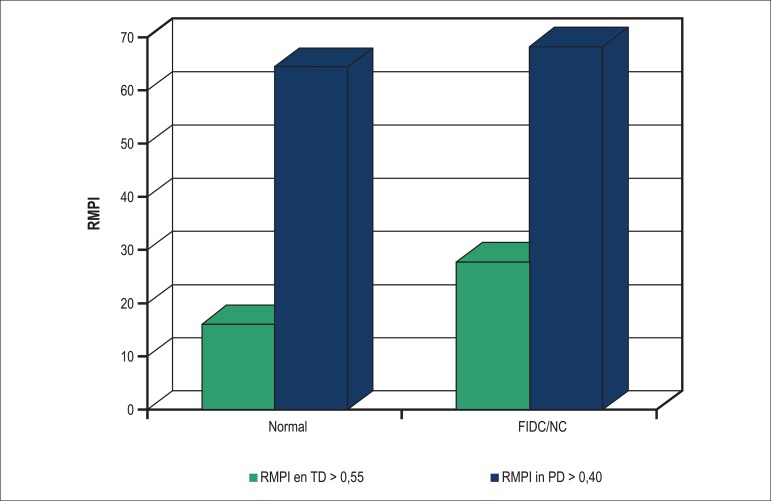
The prevalence of global RV dysfunction in groups I and II was as follows: RMPI in TD (16.1% versus 27.8%, p = 0.099) and in PD (61.3% versus 68%, p = 0.141), with no statistically significant difference, as shown in Figure 2.
Figure 2.
Prevalence of overall RV systolic dysfunction. PD: pulsed Doppler; TD: tissue Doppler; ICD/CN: indeterminate form of Chagas disease/cardiac normality; RMPI: right myocardial performance index; R V: right ventricle.
The prevalence of RV systolic dysfunction in both groups was as follows:
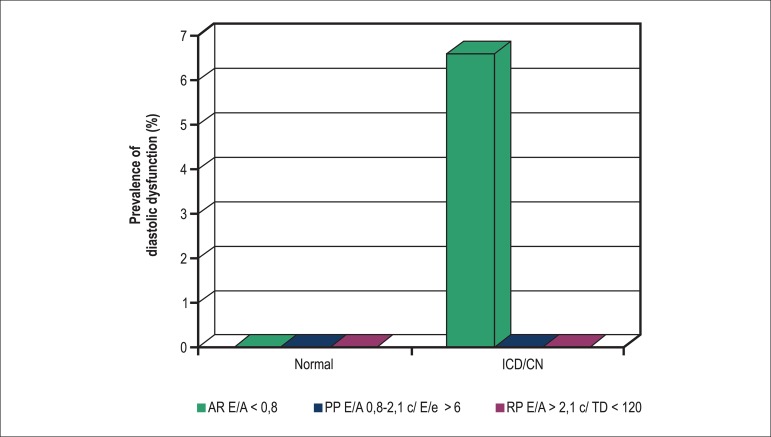
RA (0.0% versus 6.0%), PP (0.0% versus 0.0%), and RP (0.0% versus 0.0%), with no significant difference between the groups (p > 0.05), as seen in Figure 3.
Figure 3.
Prevalence of RV diastolic dysfunction in patients in groups I and II (ICD): A: transtricuspíd velocity A; AR: alteration in relaxation; E: transtricuspid velocity E; e': initial diastolic velocity in tissue Doppler; ICD/CN: indeterminate form of Chagas disease/cardiac normality; PP: pseudonormal pattern; RP: restrictive pattern; DT: deceleration time.
Discussion
We analyzed 92 patients in our series, and there was no significant statistical difference between the two groups with regard to age, sex, weight, height, BSA, LVEF, and LVDD; however, there was a predominance of females (24/77.4% versus 45/73.8%) in both the groups. In comparison, Barros et al.36 studied a sample with 12 patients in the control group and 18 with Chagas disease.
As shown in Table 2, three echocardiographic variables (RV EDA, RMPI in TD, and e'/a' ratio) did not present normal distribution and were subjected to the Mann–Whitney test. The variables RV, EDA, and e'/a' ratio were statistically significant, while RMPI in TD was not.
The other variables [RV ESA, IVC, CIVC, RAP, SPAP, RAV, IRVV, TAM, ET, and OCT in TD, ET and OCT and RMPI in PD, FAC, S wave, E, A, DT, e', a', Vs, Vd, and Vr, as well as E/A, E/e', and (Vs/Vs + Vd) ratios] showed normal distribution, with a significant value for p between the groups for variables RMPI in PD, FAC, and e'.
As a continuous variable, in both the groups, the mean S wave in TD presented values greater than 10 cm/s as normal. However, in such a relatively small sample, as a categorical variable, compared with group II, a statistically significant prevalence of 26% for S wave velocity < 10 cm/s was identified in patients in group II (6.4%), suggesting that TD is important in evaluating incipient damage to longitudinal RV contractile function in ICD/CN. In the study by Barros et al.36, this change in TD was not identified, and only a change in IVCT was identified in the RV free wall in patients with Chagas disease (90.2 ± 2.9 versus 106.5 ± 2.3 p = 0.0003).
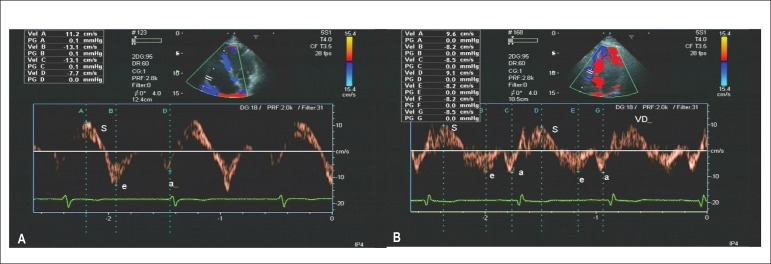
Pavlicek et al37 in a cohort with 203 non-Chagas patients, studied the variables of RV systolic function best related to RVEF, obtained by NMR. The patients were divided into three groups: group I, 129 patients with RVEF > 50%; group II, 67 patients with RVEF between 30%–50%; and group III, 27 patients with RVEF < 30% (Figures 4A and B). A strong correlation was observed between S wave < 11 cm/s in TD in the RV lateral annulus and RVEF < 50% obtained by NMR (95% confidence intervals).
Figure 4.
A) TD of the lateral annulus of the RV free wall demonstrating S wave of 11.2 cm/s in patients from group I. B) TD with S waves of 9.6 cm/s and 9.1 cm/s in patients from group II.
FAC averages in both the groups were above the lower limit for normal, with statistically significant differences; however, the variable RV EDA presented an average below the recommended values, without normal distribution between the groups. In the guidelines for assessing RV in adults15, reviews of approximately 20 studies showed average values for RV EDA to be around 18 (16–19). This scattering of averages can be explained by the difficulty in tracing the endocardial edges at the apex of RV where the trabeculae meet15.
In relation to the prevalence of systolic dysfunction using TAM and FAC, it was not possible to calculate the p value because the sample of patients with alterations was insufficient.
RMPI in PD exhibited above-normal values, with significant p values, and this is probably because of measuring ET in heart cycles other than OCT, which is not observed in RMPI in TD. The prevalence of global RV dysfunction in groups I and II showed considerable values, but without statistical significant difference. Pinto et al.38 observed altered RMPI in 28% of Chagas patients without apparent heart disease in comparison with the control group (0.34 ± 0.10 versus 0.26 ± 0.07, p = 0.001) using PD38.
In the study by Pavlicek et al.37, RMPI > 0.55 in TD showed a strong correlation with RVEF < 30% in NMR (95% confidence interval).
The parameters used in this study to assess diastolic RV function were essentially the same for the left side and were classified into AR, PP, and RP, according to the current recommendations in the guideline for assessing the right heart in adults15. The presence of RV diastolic dysfunction can be clinically useful because it serves as an easily quantifiable early marker of subclinical RV dysfunction (diastolic dysfunction is present before systolic dysfunction is apparent and before dilatation or RV hypertrophy)15, a fact not observed in this study (26% prevalence of S wave < 10 cm/s).
However, in this study, using AR, PP, and RP as categorical variables, it was not possible to calculate the prevalence of diastolic dysfunction because of the few changes with significant p values and the small sample size.
The guideline for assessing the in adults15, in a review of 40 studies with 1,688 patients, revealed e' wave values of 8–20 to be normal, with a mean of 14 cm/s with 95% confidence interval. However, in our study, patients had normal average values for e' wave, with p values being only marginally significant between the groups, and this finding was similar to that of Barros et al. (18.8 ± 0.8 versus 15.9 ± 0.7, p = 0.014)36.
As shown in Table 2, the quantification of RAA, RAV, and IRVV and the mean values and standard deviation found for RAA were within normal limits15. The mean and standard deviation values for RAV and IRVV will be useful information that may contribute in studying RV diastolic function in the near future.
The dimensional parameters between the groups for IVC, CIVC, and RAP showed values within normal limits15.
SPAP was measured in 35% and 44% of patients from groups I and II, respectively, with normal mean and standard deviation values, without significant differences between the groups. According to Badesch et al.34, the normal value for SPAP is < 35 mmHg.
Final Considerations
In this study, in relatively small samples that were nonetheless matched in terms of general characteristics, we observed that TD could identify abnormalities of longitudinal contraction in patients with ICD/CN (26% of the patients with S wave < 10 cm/s compared with the control group, p = 0.016), although the average S wave value was normal between the groups.
The prognostic significance of these real findings has not yet been established, and studies with strain rate and threedimensional echocardiogram must be performed for early diagnosis and for determining the prognostic significance; echocardiography should be routinely incorporated into the evaluation of these patients with ICD.
Other limitations of this study were the predominance of female patients in both the groups and the assessments performed by a single observer with a learning curve for the objective evaluation of RV.
Conclusions
In a relatively small sample, compared with the control group, 26% of patients with ICD/CN showed prevalent systolic RV dysfunction (S wave < 10 cm/s), suggesting that TD is important for assessing potential incipient damage in longitudinal RV contraction in ICD/CN.
No significant statistical difference was found between the groups with regard to the prevalence of global dysfunction.
It was not possible to estimate the prevalence of RV diastolic dysfunction between the groups. In TD, e' wave showed above-normal values between the groups, with a significant p value; however, at present, this is not an established criterion for diastolic dysfunction15.
Footnotes
Author contributions
Conception and design of the research: Furtado RG, Romano MMD, Schmidt A, Rassi S; Acquisition of data: Furtado RG, Rassi S; Analysis and interpretation of the data: Furtado RG, Frota DCR, Silva JBM, Romano MMD, Rassi S; Obtaining financing: Furtado RG; Statistical analysis: Furtado RG, Romano MMD, Rassi S; Writing of the manuscript: Furtado RG, Frota DCR, Silva JBM, Rassi S; Critical revision of the manuscript for intellectual content: Furtado RG, Frota DCR, Silva JBM, Romano MMD, Almeida Filho OC, Schmidt A, Rassi S; Private funding in research: Furtado RG.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study. Study Association
Study Association
This article is part of the dissertation of master submitted by Rogério Gomes Furtado from Programa de Pós-graduação in Ciências da Saúde da Faculdade de Medicina da UFG.
References
- 1.Chagas C. Nova tripanossomíase humana. Mem Inst Oswaldo Cruz. 1909;1:159–218. [Google Scholar]
- 2.World Health Organization. WHO Expert Committee . Chagas’ disease. Geneva: 1984. ((WHO Technical Report Series, 697)). [Google Scholar]
- 3.Ribeiro AL, Rocha MO. Forma indeterminada da doença de Chagas: considerações acerca do diagnóstico e do prognóstico. Rev Soc Bras Med Trop. 1998;31(3):301–314. doi: 10.1590/s0037-86821998000300008. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization Expert Committee on the Control of Chagas Disease . Control of Chagas disease. Geneva: 1991. ((WHO Technical Reports Series, 811)). [PubMed] [Google Scholar]
- 5. Reunião de Pesquisa Aplicada em Doença de Chagas: validade do conceito de forma indeterminada de doença de Chagas. Rev Soc Bras Med Trop. 1985;18:46–46. [Google Scholar]
- 6.Gallo L, Jr, Neto JA, Manco JC, Rassi A, Amorim DS. Abnormal heart rate responses during exercise in patients with Chagas' disease. Cardiology. 1975;60(3):147–162. doi: 10.1159/000169713. [DOI] [PubMed] [Google Scholar]
- 7.de Almeida JW, Shikanai Yasuda MA, Amato V, Neto, de Castilho EA, Barretto AC. studo da forma indeterminada da doença de Chagas através da eletrocardiografia dinâmica. Rev Inst Med Trop. 1982;24(4):222–228. [PubMed] [Google Scholar]
- 8.Ribeiro AL, Rocha MO, Torres RM, Gontijo EC, Ferreira LM, Oliveira E, et al. Disfunção autonômica detectada através do teste da arritmia sinusal respiratória em chagásicos sem cardiopatia aparente. Arq Bras Cardiol. 1994;63(supl 1):88–88. [Google Scholar]
- 9.Arreaza N, Puigbo JJ, Acquatella H, Casal H, Giordano H, Valecillos R, et al. Radionuclide evaluation of left-ventricular function in chronic Chagas’ cardiomyopathy. J Nucl Med. 1983;24(7):563–567. [PubMed] [Google Scholar]
- 10.Pazin A, Filho, Almeida OC, Filho, Furuta LF, Viviani LF, Schmidt A, Simões MV, et al. Prognostic implications of Chagas’ disease. J Am Coll Cardiol. 1998;31(5):339C–339C. [Google Scholar]
- 11.Torres RM. Ecocardiografia na doença de Chagas [dissertação] Belo Horizonte: Faculdade de Medicina; Universidade Federal de Minas Gerais; 1997. [Google Scholar]
- 12.Friedmann AA. Desempenho ventricular na doença de Chagas. Estudo ecocardiográfico em fase pré-clínica [tese] São Paulo: Faculdade de Medicina; Universidade de São Paulo; 1978. [Google Scholar]
- 13.Machado FS, Barros MV. Silva CE. Ecocardiografia: princípios e aplicações clínicas. Rio de Janeiro: Revinter; 2007. Ecocardiografia na Doença de Chagas. In: Silva CE. Ecocardiografia: princípios e aplicações clínicas; pp. 713–723. [Google Scholar]
- 14.Marin JA, Neto, Andrade ZA. Por que é usualmente predominante a insuficiência cardíaca direita na doença de Chagas. Arq Bras Cardiol. 1991;57(3):181–183. [PubMed] [Google Scholar]
- 15.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacker MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Campana AO, Iaria CT, Freitas CB, Paiva SA, Hossne WS. Pesquisa clínica: investigação científica na área médica. São Paulo: Manole; 2001. pp. 125–143. [Google Scholar]
- 17.Ferreira AW, Ávila SL. Diagnóstico laboratorial das principais doenças infecciosas e autoimunes. 2ª. ed. Rio de Janeiro: Guanabara Koogan; 2001. [Google Scholar]
- 18.Galderisi M, Henein MY, D' hooge J, Sicari R, Badano LP, Zamorano JL, et al. European Association of Echocardiography Recommendations of the European Association of Echocardiography: how to use echo-Doppler in clinical trials: different modalities for different purposes. Eur J Echocardiogr. 2011;12(5):339–353. doi: 10.1093/ejechocard/jer051. [DOI] [PubMed] [Google Scholar]
- 19.Evangelista A, Flachskampf F, Lancellotti P, Badano L, Aguilar R, Monaghan M, et al. European Association of Echocardiography European Association of Echocardiography recommendations for standardization of performance, digital storage and reporting of echocardiographic studies. Eur J Echocardiogr. 2008;9(4):438–448. doi: 10.1093/ejechocard/jen174. [DOI] [PubMed] [Google Scholar]
- 20.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Chamber Quantification Writing Group. American Society of Echocardiography’s Guidelines and Standards Committee. European Association of Echocardiography. et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Kaul S, Tei C, Hopkins JM, Shan PM. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J. 1984;107(3):526–531. doi: 10.1016/0002-8703(84)90095-4. [DOI] [PubMed] [Google Scholar]
- 22.Lai WW, Gauvreau K, Rivera ES, Saleeb S, Powell AJ, Geva T. Accuracy of guideline recommendations for two-dimensional quantification of the right ventricle by echocardiography. Int J Cardiovasc Imaging. 2008;24(7):691–698. doi: 10.1007/s10554-008-9314-4. [DOI] [PubMed] [Google Scholar]
- 23.Anavekar NS, Gerson D, Skali H, Kwong RY, Yucel EK, Solomon SD. Twodimensional assessment of right ventricular function: an echocardiographic- MRI correlative study. Echocardiography. 2007;24(5):452–456. doi: 10.1111/j.1540-8175.2007.00424.x. [DOI] [PubMed] [Google Scholar]
- 24.Tei C, Dujardin KS, Hodge DO, Bailey KR, McGoon MD, et al. Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr. 1996;9(6):838–847. doi: 10.1016/s0894-7317(96)90476-9. [DOI] [PubMed] [Google Scholar]
- 25.Berman GO, Reichek N, Brownson D, Douglas PS. Effects of sample volume location, imaging view, heart rate and age on tricuspid velocimetry in normal subjects. Am J Cardiol. 1990;65(15):1026–1030. doi: 10.1016/0002-9149(90)91008-t. [DOI] [PubMed] [Google Scholar]
- 26.Klein AL, Leung DY, Murray RD, Urban LH, Bailey KR, Tajik AJ. Effects of age and physiologic variables on right ventricular filling dynamics in normal subjects. Am J Cardiol. 1999;84(4):440–448. doi: 10.1016/s0002-9149(99)00330-6. [DOI] [PubMed] [Google Scholar]
- 27.Otto C. The practice of clinical echocardiography. 3rd. ed. Philadelphia: Saunders Elsevier; 2007. [Google Scholar]
- 28.Feigenbaun H, Armstrong WF, Ryan T. Left atrium, right atrium and right ventricle. In: Feigenbaun H, editor. Feigenbaum's echocardiography. 6th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2005. pp. 181–213. [Google Scholar]
- 29.Moreno FL, Hagan AD, Holmen JR, Pryor TA, Strickland RD, Castle CH. Evaluation of size and dynamics of the inferior vena cava as an index of right-sided cardiac function. Am J Cardiol. 1984;53(4):579–585. doi: 10.1016/0002-9149(84)90034-1. [DOI] [PubMed] [Google Scholar]
- 30.Weyman A. Cross-sectional echocardiography. Philadelphia: Lea & Febiger; 1981. [Google Scholar]
- 31.Ommen SR, Nishimura RA, Hurrell DG, Klarich KW. Assessment of right atrial pressure with 2-dimensional and Doppler echocardiography: a simultaneous catheterization and echocardiographic study. Mayo Clin Proc. 2000;75(1):24–29. doi: 10.4065/75.1.24. [DOI] [PubMed] [Google Scholar]
- 32.Otto CM. Enchimento ventricular e função diastólica: fundamentos de ecocardiografia clínica. 3ª ed. Philadelphia: Elsevier; 2005. pp. 145–159. [Google Scholar]
- 33.Nagueh SF, Kopelen HA, Zoghbi WA. Relation of mean right atrial pressure to echocardiographic and Doppler parameters of right atrial and right ventricular function. Circulation. 1996;93(6):1160–1169. doi: 10.1161/01.cir.93.6.1160. [DOI] [PubMed] [Google Scholar]
- 34.Badesch DB, Champion HC, Sanchez MA, Hoeper MM, Loyd JE, Manes A, et al. Diagnosis and assessment of pulmonary arterial hypertension. J Am Coll Cardiol. 2009;54(1) Suppl:S55–S66. doi: 10.1016/j.jacc.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 35.Nagueh SF, Kopelen HA, Zoghbi WA, Quinones MA, Naghueh SF. Estimation of mean right atrial pressure using tissue Doppler imaging. Am J Cardiol. 1999;84(12):1448–1451. doi: 10.1016/s0002-9149(99)00595-0. [DOI] [PubMed] [Google Scholar]
- 36.Barros MV, Machado FS, Ribeiro AL, da Costa Rocha MO. Detection of early right ventricular dysfunction in Chagas' disease using tissue Doppler imaging. Pt 2J Am Soc Echocardiogr. 2002;15(10):1197–1201. doi: 10.1067/mje.2002.122966. [DOI] [PubMed] [Google Scholar]
- 37.Pavliceck M, Wahl A, Rutz T, de Marchi SF, Hille R, Wustmann K, et al. Right ventricular systolic function assessment: rank of echocardiographic methods vs. cardiac magnetic resonance imaging. Eur J Echocardiogr. 2011;12(11):871–880. doi: 10.1093/ejechocard/jer138. [DOI] [PubMed] [Google Scholar]
- 38.Pinto AS, Oliveira BM, Botoni FA, Ribeiro AL, Rocha MO. Disfunção miocárdica em pacientes chagásicos sem cardiopatia aparente. Arq Bras Cardiol. 2007;89(6):385–390. doi: 10.1590/s0066-782x2007001800006. [DOI] [PubMed] [Google Scholar]