Abstract
The composition of the pulmonary intersegmental septum has not been clearly identified by thoracic surgeons who regard Kohn's pores as the main channel that causes air leakage when determining the intersegmental septum by segmental ventilation. In this study, we aimed to examine this possible misinterpretation by focusing on a detailed description of the microscopic anatomy of the intersegmental septum. To accomplish this aim, 50 lung samples of the intersegmental septum from fresh cadavers without emphysema were studied by histological and electron microscopy. The findings of light microscopy and electron microscopy showed that the intersegmental septum is composed of three layers. The alveolar walls of adjacent segments serve as the superficial layer. They are integral, and no Kohn's pores were identified. The deep layer contains collagen fibres. As shown by our findings, Kohn's pores are absent within the intersegmental septum. Therefore, they could not be the main channel for the collateral ventilation between inflated and deflated lung segments during a pulmonary segmentectomy.
Keywords: anatomy, electron microscopy, histology, intersegmental septum, lung
Introduction
The pulmonary intersegmental septum is a layer of the interstitial septum ascending from the visceral pleura that separates two adjacent pulmonary segments. It has attracted interest from thoracic surgeons for a long time due to its key anatomical feature as a segmental border. In a segmentectomy, the intersegmental septum is regarded as an ideal cutting surface to separate diseased from healthy lung segments. Therefore, one of the most important factors in a segmentectomy is to identify the intersegmental septum. In recent years, thoracic surgeons have established and improved many methods used to identify the intersegmental septum during operations based on different anatomical features, such as segmental ventilation (Tsubota, 2000; Matsuoka et al. 2003; Kamiyoshihara et al. 2007; Okada et al. 2007) and dye injection and ligature of segmental vessels (Misaki et al. 2010; Sugimoto et al. 2011; Sekine et al. 2012; Pardolesi et al. 2014).
Thoracic surgeons have only determined how to identify the intersegmental septum during an operation and have not clearly defined its composition. A lack of knowledge of the composition of the intersegmental septum still exists, which is exemplified by the explanation of why air leakage occurs when identifying the intersegmental septum through segmental ventilation in patients without emphysema. Thoracic surgeons have assumed that Kohn's pores can account for collateral ventilation that occurs under positive pressure (Tsubota, 2000; Matsuoka et al. 2003; Okada et al. 2007). The existence of Kohn's pores within the intersegmental septa and their ability to exchange substances with adjacent segments has not been demonstrated.
We doubt the existence of Kohn's pores within the intersegmental septa. First, Kohn's pores are known as apertures in the interalveolar septum. They communicate with the adjacent alveoli and are easy to find in pulmonary haematoxylin and eosin (H&E) sections. However, there is no direct evidence to support the presence of Kohn's pores within intersegmental septa. Second, if Kohn's pores do exist within the intersegmental septa, the pulmonary segment no longer represents an integral and independent unit within lungs because adjacent segments communicate. Therefore, a pulmonary segmentectomy may lose its anatomical basis.
Unfortunately, the composition of the intersegmental septum has not been clearly described. Few studies have generally reported the anatomy of the intersegmental septum (Berkmen et al. 1992; Chicco et al. 2001; Zuo et al. 2013), and its composition is only visible in H&E sections at low magnification (Berkmen et al. 1992). To examine the composition of the intersegmental septum, two different methods, including histology and electron microscopy, were used. In this way we can determine whether Kohn's pores are the main channels that cause the air leakage when using segmental ventilation to identify the intersegmental septum during an operation.
Materials and methods
Lung samples
This study was approved by the internal Ethics Review Board of Nanjing Medical University, and written informed consent was obtained from all participants for the use of patient biomaterial. Twenty-five normal lungs were obtained by autopsy from 13 fresh cadavers without emphysema (mean age, 53.6 years, eight male and five female). The intersegmental septa were identified after we injected different dyes into different segmental bronchi. The transitional zone between two colours was regarded as the precise position of the intersegmental septum. We excised two tissue blocks containing intersegmental septum from every lung. In total, 50 lung tissue blocks were obtained from the fresh lungs. These samples were randomised using a computerised random-number generator. We used two different methods to determine the integrity of the pulmonary intersegmental septum, including histology and electron microscopy. Forty-eight samples were used for histological analysis. Two samples were used for electron microscopy.
Histology
Intersegmental septa were identified following the injection of different dyes into segmental bronchi (Fig.1). Lung samples (5 × 5 × 5 mm) were individually embedded in paraffin. Tissue specimens were sectioned serially to provide 5-μm-thick sections, which were then stained with H&E. Digital pictures were obtained from all intact histological sections with a universal light microscope.
Figure 1.
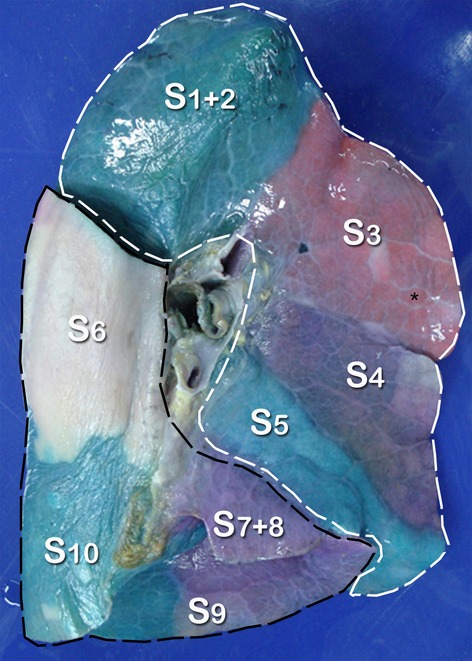
A medial view of the left lung with anterior to the right. The transitional zone between two colours is the precise location of the intersegmental septum. Dashed lines show the region of the superior lobe (white dashed line) and inferior lobe (black dashed line), respectively. A pulmonary lobule (black asterisk) is seen beneath the visceral pleura. (S1+2, apicoposterior segment; S3, anterior segment; S4, superior lingular segment; S5, inferior lingular segment; S6, superior segment; S7+8, anteromedial basal segment; S9, lateral basal segment; S10, posterior basal segment).
Transmission electron microscopy
Tissue specimens were cut into blocks (3 × 1 × 1 mm) and immersed in 2.5% glutaraldehyde in 0.1 m cacodylate buffer (pH 7.4) for 2 h. After postfixation in 1% OsO4 in 0.1 m cacodylate buffer (pH 7.4) for 1 h, the specimens were dehydrated in graded ethanol solutions and embedded in Durcupan ACM (Fluka). For the histological identification of the regions of interest, semi-thin sections were obtained and stained with 1% toluidine blue or equal parts of 1% toluidine blue and 1% pyronin. Ultrathin sections were cut on an LKB ultramicrotome, contrasted with 7% uranyl acetate and 2.6% lead citrate for 30 min, and examined by a transmission electron microscope (Hitachi 500).
Scanning electron microscopy
Tissue specimens were cut into blocks (5 × 3 × 2 mm) and fixed in 3% glutaraldehyde buffered with 0.1 m phosphate buffer at pH 7.2 for at least 24 h at 4–8 °C. The tissue sections were postfixed with a 2% osmium tetroxide solution for 12 h at 25 °C, dehydrated with a graded ethanol series, critical point dried with liquid CO2, mounted on scanning electron microscope stubs, sputtered with gold, and examined using a Hitachi S-3000N scanning electron microscope.
Results
In the histological slides (Fig.2A,B), the intersegmental septum is visible as a septum extending into two adjacent pulmonary segments. It is seen as a thin line with uniform thickness. It is obvious that the intersegmental septum is composed of three layers. The deep layer is composed of loose connective tissue. The alveolar walls of the two adjacent segments serve as the superficial layers. The superficial layers are integral, and no Kohn's pores were found. The interlobular septa branch off from the intersegmental septum.
Figure 2.
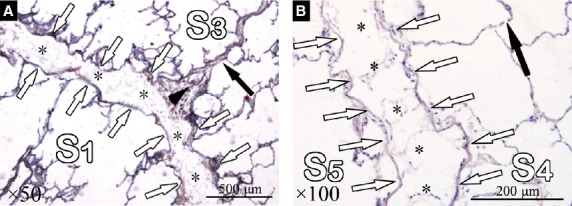
(A,B) Photomicrograph showing the constitution of the pulmonary intersegmental septum (stain, H&E). The intersegmental septum is composed of superficial layers (white arrows) and a deep layer (black asterisk). (A) The interlobular septum (black arrow) originates from the intersegmental septum, and the arrowhead shows its origin. (B) A Kohn's pore (black arrow) is seen on the alveolar wall.
At the electron microscopy level, we found that alveolar walls and collagen fibres constitute the superficial and deep layers, respectively (Fig.3A). The superficial layer is integral. Kohn's pores can be observed in other parts of the alveoli but not even the alveolar wall, which serves as the superficial layer of the intersegmental septum (Fig.3B). The deep layer contains collagen fibres. Type I cells can be observed on the alveolar wall. They are connected by tight junctions (Fig.3C). The collagenous fibre is composed of numerous, loose, low-density collagen fibrils. Meanwhile, fibroblasts surrounded by collagen fibrils can be observed in the deep layer (Fig.3D).
Figure 3.
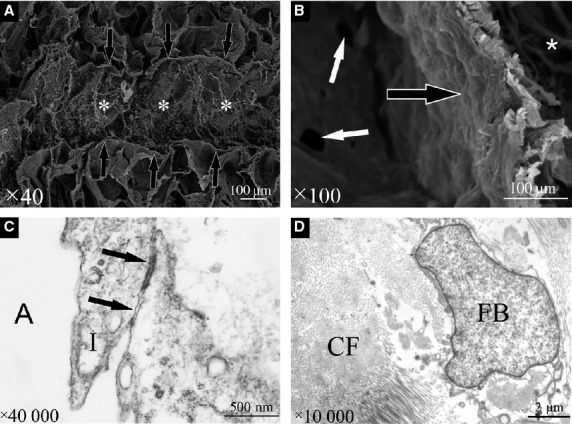
Scanning electron microscopy photographs of the intersegmental septum. (A) The intersegmental septum consists of three layers, including the superficial layers (black arrows) and deep layer (white asterisk). (B) The superficial layer (black arrow) is integral, and no Kohn's pores were identified. Kohn's pores (white arrows) are only seen on the alveolar wall between two alveoli. The deep layer (white asterisk) contains collagen fibres. Transmission electron microscopy photographs of the intersegmental septum are shown. (C) Type I cells constitute the alveolar wall and contain tight junctions (black arrows). (D) The deep layer is composed of collagen fibrils and fibroblasts. A, alveoli; CF, collagen fibres; FB, fibroblasts; I, type I cell.
Discussion
In this study, we systematically studied the composition of intersegmental septa at the level of micro-sectional anatomy by using histological and electron microscopy. In summary, these methods clearly revealed the composition of the intersegmental septum, which consists of three layers. The alveolar walls of two adjacent segments serve as the superficial layers. The deep layer is composed of collagenous fibres.
Our study clearly showed the composition of pulmonary intersegmental septa. Thus, we may conclude that collateral ventilation between two segments does not occur through Kohn's pores because no Kohn's pore could be found within the intersegmental septum. This conclusion was based on our careful analysis of the two-dimensional images of intersegmental septa. First, we carefully studied the H&E-stained sections of the intersegmental septum. Also, we observed transmission electron microscopy images. We found that Kohn's pores were easy to find everywhere within the lung specimens, except for the pulmonary septum, which includes the intersegmental septa. Therefore, the intersegmental septum is a contiguous membrane that completely separates pulmonary segments. However, thoracic surgeons need to preserve the integrity of the intersegmental septum during a segmentectomy because that integrity could help preserve post-operative pulmonary function. Some recent reports have even introduced a new method of using a mesh-covering to ensure the integrity of the intersegmental septum and the re-expansion of residual lung segments (Yoshimoto et al. 2011).
Conversely, if we postulate the existence of Kohn's pores within the intersegmental septum as previous studies have suggested (Tsubota, 2000; Matsuoka et al. 2003; Okada et al. 2007), we may speculate that the gas must escape to the deep layer before it reaches the adjacent segment. Therefore, the thickness of the intersegmental septum should be increased due to the presence of gas, which means that the density of the intersegmental septum would be as low as that of the surrounding tissues. Such a finding is not consistent with the information provided by a previous study (Berkmen et al. 1992; Zuo et al. 2013), and demonstrated that the intersegmental septa can be seen as lines with hyper-attenuation on multi-slice computed tomography (MSCT). The high density on MSCT scans of the intersegmental septum indicated the existence of local interstitial fluid. Thus, we confirmed the existence of interstitial fluid within the intersegmental septum. Consequently, the possibility of the existence of Kohn's pores on the superficial layer is also excluded because the interstitial fluid does not drain into the alveoli through pores.
Our study had several limitations. First, we could not demonstrate Kohn's pores in the intersegmental plane, but neither were we able to provide any other explanation for collateral ventilation between adjacent segments. However, we speculate that the existence of communicating branches of the bronchus between two adjacent segments is the main cause for intersegmental gas exchange. A fracture of the intersegmental septum caused by the positive pressure is also a possible reason for the intersegmental gas exchange. However, these hypotheses still need to be tested. Second, variations of intersegmental septum, such as the intersegmental fissure, were not included in this study. Figure4 shows a variation of the intersegmental septum in the superior lobe of the right lung. Third, normal light microscopy can clearly show most of the intrapulmonary structures, such as Kohn's pores. Therefore, we utilised histology as our main method to identify whether Kohn's pores exist within the intersegmental septum. Thus, we only performed electron microscopy on limited numbers of lung samples.
Figure 4.
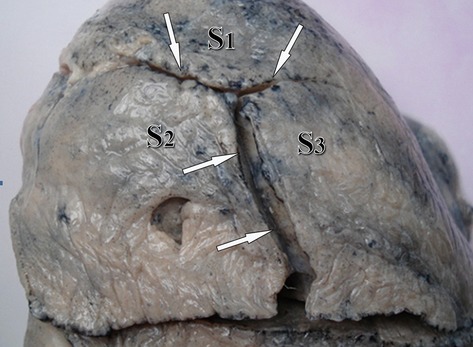
Variation of the intersegmental fissure (white arrows) in the superior lobe of the right lung.
Conclusions
In conclusion, the intersegmental septa are composed of three layers. Alveolar walls serve as the superficial layers, and the deep layer is composed of collagenous fibres and interstitial fluid. Kohn's pores are not found within the intersegmental septum. Therefore, they are not the main channel for collateral ventilation between inflated and deflated segments during a pulmonary segmentectomy.
Acknowledgments
This study was supported by the Chinese National Natural Science Foundation 31300983, Micro-sectional anatomy research of the pulmonary intersegmental plane and reconstruction of a three-dimensional model; and by Natural Science Research Projects in the colleges and universities of Jiangsu Province 13KJB310001, Anatomical research on the substance of the intersegmental plane and reconstruction of a digital model.
References
- Berkmen YM, Drossman SR, Marboe CC. Intersegmental (intersublobar) septum of the lower lobe in relation to the pulmonary ligament: anatomic histologic, and CT correlations. Radiology. 1992;185:389–393. doi: 10.1148/radiology.185.2.1410343. [DOI] [PubMed] [Google Scholar]
- Chicco P, Magnussen JS, Vu DH, et al. Determining the cross-sectional segmental anatomy of cadaveric human lungs. Clin Anat. 2001;14:10–14. doi: 10.1002/1098-2353(200101)14:1<10::AID-CA1001>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Kamiyoshihara M, Kakegawa S, Morishita Y. Convenient and improved method to distinguish the pulmonary intersegmental plane using a butterfly needle. Ann Thorac Surg. 2007;83:1913–1914. doi: 10.1016/j.athoracsur.2006.06.052. [DOI] [PubMed] [Google Scholar]
- Matsuoka H, Nishio W, Sakamoto T, et al. Selective segmental jet injection to distinguish the intersegmental plane using jet ventilation. Jpn J Thorac Cardiovasc Surg. 2003;51:400–401. doi: 10.1007/BF02719478. [DOI] [PubMed] [Google Scholar]
- Misaki N, Chang SS, Igai H, et al. New clinically applicable method for visualizing adjacent lung segments using an infrared thoracoscopy system. J Thorac Cardiovasc Surg. 2010;140:752–756. doi: 10.1016/j.jtcvs.2010.07.020. [DOI] [PubMed] [Google Scholar]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberopticjet followed by cautery cutting. J Thorac Cardiovasc Surg. 2007;133:753–758. doi: 10.1016/j.jtcvs.2006.11.005. [DOI] [PubMed] [Google Scholar]
- Pardolesi A, Veronesi G, Solli P, et al. Use of indocyanine green to facilitate intersegmental plane identification during robotic anatomic segmentectomy. J Thorac Cardiovasc Surg. 2014;148:737–738. doi: 10.1016/j.jtcvs.2014.03.001. [DOI] [PubMed] [Google Scholar]
- Sekine Y, Ko E, Oishi H, et al. A simple and effective technique for identification of intersegmental planes by infrared thoracoscopy after transbronchial injection of indocyanine green. J Thorac Cardiovasc Surg. 2012;143:1330–1335. doi: 10.1016/j.jtcvs.2012.01.079. [DOI] [PubMed] [Google Scholar]
- Sugimoto S, Oto T, Miyoshi K, et al. A novel technique for identification of the lung intersegmental plane using dye injection into the segmental pulmonary artery. J Thorac Cardiovasc Surg. 2011;141:1325–1327. doi: 10.1016/j.jtcvs.2010.09.029. [DOI] [PubMed] [Google Scholar]
- Tsubota N. An improved method for distinguishing the intersegmental plane of the lung. Surg Today. 2000;30:963–964. doi: 10.1007/s005950070056. [DOI] [PubMed] [Google Scholar]
- Yoshimoto K, Nomori H, Mori T, et al. Comparison of postoperative pulmonary function and air leakage between pleural closure vs mesh-cover for intersegmental plane in segmentectomy. J Cardiothorac Surg. 2011;6:61. doi: 10.1186/1749-8090-6-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuo YZ, Liu C, Liu SW. Pulmonary intersegmental planes: imaging appearance and possible reasons leading to their visualization. Radiology. 2013;267:267–275. doi: 10.1148/radiol.12121114. [DOI] [PubMed] [Google Scholar]


