Abstract
Background
Air pollutants from wildfires and obesity independently exacerbate asthma, yet no study has determined the combined effects of these 2 variables on asthma outcomes.
Objective
To determine the effect of 2 catastrophic wildfires affecting the Southern California region (in 2003 and 2007) on several asthma outcomes in a cohort of children.
Methods
To investigate the association between wildfire exposure and asthma outcomes, we stratified our study population by body mass index categories (underweight, normal, overweight, and obese) and zip codes (to distinguish individuals who were closer to the fires vs farther away). The primary outcome was the prevalence of physician-dispensed short-acting β-agonist (SABAs). Secondary outcomes included the rate of emergency department visits and/or hospitalizations for asthma, the frequency of oral corticosteroid use for asthma, and number of new diagnoses of asthma.
Results
A total of 2,195 and 3,965 asthmatic children were analyzed as part of our retrospective cohort during the 2003 and 2007 wildfires, respectively. SABA dispensing increased the most in the obese group after the 2003 wildfires (P <.05). Increased prevalence of SABA dispensing was also noted in the obese group in 2007, but this was not statistically higher than the increases seen in other body mass index groups. There was no observed increase in emergency department and/or hospitalization rates, oral corticosteroid dispensing frequency, or new asthma diagnoses after either wildfire.
Conclusion
Catastrophic wildfires lead to worsening asthma outcomes, particularly in obese individuals. This study gives further evidence of a link between obesity and asthma severity and suggests that air pollutants released during wildfires can have substantial detrimental effects on asthma control.
Introduction
The catastrophic wildfires of 2003 and 2007 in Southern California offer a unique environment in which to examine the adverse health effects on asthmatic individuals related to the sudden high levels of airborne pollutants. In late October 2003, wildfires burned more than 3,000 km2 and resulted in higher rates of reported wheezing, asthma exacerbations, medication use for symptoms, and physician visits.1 The severity of these symptoms appeared to be dose dependent because individuals who experienced 6 or more days of fire smell had a greater odds ratio of experiencing asthma symptoms than those only experiencing 1 to 5 days of fire smell. The effects of the wildfires on San Diego air quality were also evaluated and revealed that fine particulate matter levels exceeded the federal daily 24-hour average standard during the fire and that ozone precursor levels were also increased.1
Although air pollution and wildfire worsen asthma outcomes, a separate body of literature suggests that obesity can also lead to a more severe asthma phenotype. Asthma is a heterogeneous disease with genetic and environmental factors that affect the development, progression, and severity of the disease. Studies have highlighted obesity as a risk factor for developing asthma and enhancing disease morbidity.3–10 We have previously described a cohort of 32,321 asthmatic children within the Southern California Kaiser Permanente Medical Group (KPMG) and found a dose effect between obesity and indexes of disease severity (numbers of rescue inhalers dispensed per year and oral corticosteroid courses dispensed per year).11 Recently, animal models using obese mice (either leptin-deficient or leptin receptor–deficient mice, which both have massive obesity, hyperinsulinemia, hyperglycemia, and increased plasma cholesterol)12–14 indicate that obesity itself predisposes to airway hyperresponsiveness. This is believed to be multifactorial with a combination of mechanical factors, lung development, and chronic systemic inflammation because of the increased production of adipokines (in particular tumor necrosis factor α, leptin, and adiponectin). The aggregate data suggest that obesity is a true risk factor for asthma.
Thus, there is evidence to independently link air pollution (from wildfires) and obesity to poor asthma outcomes. However, no study has yet examined the combined effects of these 2 variables in a single cohort. To study the effect of obesity and wildfires on asthma outcomes, we used a previously described pediatric cohort11 and analyzed several asthma outcome measures, including prevalence of short-acting β-agonists (SABAs) dispensed by physicians, emergency department (ED) visit and/or hospitalization rates, frequency of physician-prescribed oral corticosteroids (OCSs), and rate of new diagnosis of asthma before vs after the San Diego wildfires of 2003 and 2007. In addition, these patients were stratified by body mass index (BMI) into 4 groups: (1) underweight (BMI ≤ 18.5), (2) normal weight (BMI of 18.5–24.9), (3) overweight (BMI of 25–30), and (4) obese (BMI >30). We hypothesized that asthma outcomes after exposure to catastrophic wildfires would be worse in obese asthmatic children than in nonobese asthmatic children.
Methods
Study Period Dates and Outcome Measures
The 2003 Southern California fires peaked between October 25 and November 3, whereas the 2007 Southern California fires peaked between October 20 and November 9. The primary asthma outcome was frequency of physician-dispensed SABAs for asthma. The secondary asthma outcomes that we measured were frequency of ED and/or hospitalization for asthma exacerbations (ED visit and/or hospitalization), frequency of physician-prescribed OCS bursts linked to asthma as a primary diagnosis, and prevalence of newly diagnosed asthma (new asthma). These asthma outcomes were collected for a 1-year period before and after the fires in 2003 and 2007.
Statistical Analysis
To investigate the association between wildfire exposure and asthma outcomes, we stratified our study population by BMI categories (underweight, normal, overweight, and obese) and zip codes (to distinguish individuals who were closer to the fires vs farther away). The McNemar test was used to compare asthma outcomes before and after the fire to obtain a P for each BMI category. The χ2 test was used to compare asthma outcomes across BMI categories. Statistical significance was set at P < .05 after adjusting for multiple comparisons using the Bonferroni method. The Cochran-Armitage trend test was used to test whether asthma outcomes (ie, SABA dispensing) increase linearly with higher levels of BMI categories.15–17 SAS Enterprise Guide, version 4.3, was used for all statistical analyses (SAS institute Inc, Cary, North Carolina).
Results
Study Dates and Demographics
Table 1 and Table 2 give the demographic composition of asthmatic children enrolled in the San Diego Kaiser Permanente registry in 2003 and 2007.
Table 1.
Demographics and characteristics for the children in the 2003 fire in the San Diego, CA, zip code area
| Characteristic | No. (%) of children | P value | ||||
|---|---|---|---|---|---|---|
| Underweight (n = 43) |
Normal (n = 1,183) |
Overweight (n = 407) |
Obese (n = 562) |
Total (n = 2,195) |
||
| Age, y | .30 | |||||
| 5–11 | 30 (69.8) | 807 (68.2) | 288 (70.8) | 408 (72.6) | 1,533 (69.8) | |
| 12–17 | 13 (30.2) | 376 (31.8) | 119 (29.2) | 154 (27.4) | 662 (30.2) | |
| Sex | .007 | |||||
| Female | 18 (41.9) | 535 (45.2) | 183 (45) | 206 (36.7) | 942 (42.9) | |
| Male | 25 (58.1) | 648 (54.8) | 224 (55) | 356 (63.3) | 1,253 (57.1) | |
| Race/ethnicitya | <.001 | |||||
| White | 16 (37.2) | 556 (47) | 164 (40.3) | 179 (31.9) | 915 (41.7) | |
| African American | 6 (14) | 105 (8.9) | 38 (9.3) | 62 (11) | 211 (9.6) | |
| Hispanic | 11 (25.6) | 290 (24.5) | 137 (33.7) | 227 (40.4) | 665 (30.3) | |
| Asian | 5 (11.6) | 115 (9.7) | 37 (9.1) | 39 (6.9) | 196 (8.9) | |
| Other | 1 (2.3) | 25 (2.1) | 5 (1.2) | 16 (2.8) | 47 (2.1) | |
| Unknown | 4 (9.3) | 92 (7.8) | 26 (6.4) | 39 (6.9) | 161 (7.3) | |
Because of rounding, not all percentages total 100%.
Table 2.
Demographics and characteristics for the children in the 2007 fire in the San Diego, CA, zip code area
| Characteristic | No. (%) of children | P value | ||||
|---|---|---|---|---|---|---|
| Underweight (n = 83) |
Normal (n = 2,058) |
Overweight (n = 774) |
Obese (n = 1,050) |
Total (n = 3,965) |
||
| Age, y | <.001 | |||||
| 5–11 | 62 (74.7) | 1,223 (59.4) | 494 (63.8) | 741 (70.6) | 2,520 (63.6) | |
| 12–17 | 21 (25.3) | 835 (40.6) | 280 (36.2) | 309 (29.4) | 1,445 (36.4) | |
| Sex | <.001 | |||||
| Female | 31 (37.3) | 976 (47.4) | 365 (47.2) | 411 (39.1) | 1,783 (45) | |
| Male | 52 (62.7) | 1,082 (52.6) | 409 (52.8) | 639 (60.9) | 2,182 (55) | |
| Race/ethnicitya | <.001 | |||||
| White | 33 (39.8) | 856 (41.6) | 300 (38.8) | 310 (29.5) | 1,499 (37.8) | |
| African American | 8 (9.6) | 180 (8.7) | 81 (10.5) | 113 (10.8) | 382 (9.6) | |
| Hispanic | 16 (19.3) | 580 (28.2) | 242 (31.3) | 452 (43) | 1,290 (32.5) | |
| Asian | 12 (14.5) | 159 (7.7) | 55 (7.1) | 68 (6.5) | 294 (7.4) | |
| Other | 5 (6) | 38 (1.8) | 14 (1.8) | 19 (1.8) | 76 (1.9) | |
| Unknown | 9 (10.8) | 245 (11.9) | 82 (10.6) | 88 (8.4) | 424 (10.7) | |
Because of rounding, not all percentages total 100%.
Prevalence of SABA Dispensing Increased in Obese Asthmatic Patients After Wildfires
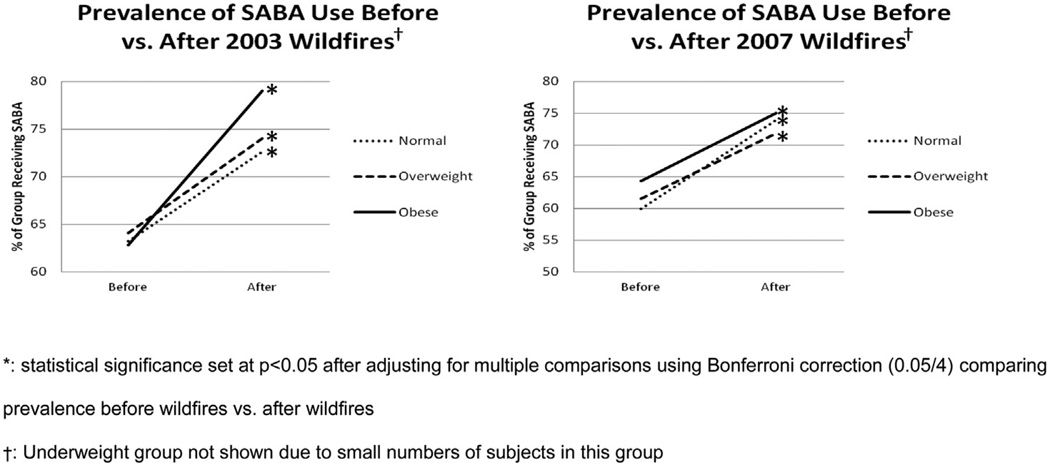
Analysis of prefire vs postfire prevalence of SABA dispensing in 2003 revealed an increase across all BMI groups (Fig 1 and eTable 1). Similar findings are noted after the 2007 wildfires (Fig 1 and eTable 2). The largest increase in 2003 was seen in the obese BMI group (+16%, P < .05). This difference was significantly higher than the increase in other BMI groups (P = .040; eTable 1). There was also a significant trend (P = .01 for trend) toward higher prevalence of physician-prescribed SABA canisters as a function of increasing BMI after the wildfires in 2003 (Table 3). When only individuals within the fire zip codes were examined, obese patients had the largest increase in rate of SABA dispensing in 2003, although this finding did not reach statistical significance (+15%, eTable 1).
Figure 1.
The change in prevalence of SABA use before versus after wildfires.
Table 3.
Prevalence ratio of short-acting β-agonist dispensing before and after the 2003 wildfires
| BMI group | Prevalence ratio (95% CI)a |
|---|---|
| Underweight | 1.10 (0.55–2.20) |
| Normal weight | 1.00 (Reference) |
| Overweight | 1.07 (0.83–1.38) |
| Obese | 1.42 (1.12–1.80) |
Abbreviations: BMI, body mass index; CI, confidence interval.
Significant P value for the trend of .01 (using the Cochran-Armitage trend test).
Although the 2007 wildfire data also indicated a significant increase in SABA dispensing in the obese population (+10.5%, P < .05), the increases among other BMI groups were similar (+14% in the normal group and +10% in the overweight group). When the individuals within the 2007 fire zip codes were examined, the overweight group had the largest statistically significant increase (+26%, eTable 2). The trend toward higher prevalence of physician-prescribed SABA canisters as a function of increasing BMI was not noted in 2007 (Table 4).
Table 4.
Prevalence ratio of short-acting β-agonist dispensing before and after the 2007 wildfires
| BMI Group | Prevalence ratio (95% CI)a |
|---|---|
| Underweight | 0.98 (0.85–1.12) |
| Normal weight | 1.00 (Reference) |
| Overweight | 0.97 (0.92–1.02) |
| Obese | 1.01 (0.97–1.06) |
P value for the trend of .61.
ED and Hospitalization Rates of Obese Asthmatic Patients After Wildfires
In the year after the 2003 or 2007 wildfires in San Diego, no significant change in ED visit or hospitalization rates were noted (eTable 3 and eTable 4) in any of the BMI groups compared with before the fires.
Prevalence of OCS Use in Obese Asthmatic Children After Wildfires
The prevalence of physician-dispensed OCSs after the 2003 and 2007 wildfires was consistently higher in the obese group compared with the other groups, but this finding did not reach statistical significance in either year (eTable 5 and eTable 6).
Prevalence of New Asthma Diagnoses in Obese Asthmatic Children After Wildfires
After the 2003 wildfires, we observed that there was actually a decrease across all BMIs in the prevalence of new asthma diagnoses compared with before the fires (eTable 7). These decreases were statistically significant in patients who had a normal, overweight, or obese BMI. After the 2007 wildfires, there were no statistically significant changes in any BMI group compared with before the wildfires (eTable 8).
Discussion
The association between obesity and asthma has been strongly suggested by various studies published in the last several years.4,18–20 Air pollution from wildfires has also been previously linked to worsened asthma outcomes.1,2 Using a previously defined cohort of pediatric patients,11 we examined the combined effects of these 2 risk factors for asthma by studying a population of over-weight or obese asthmatic patients after exposure to 2 catastrophic wildfires in southern California. The primary outcome evaluated whether individuals with higher BMI (obese patients) were provided more physician-dispensed SABA canisters after wildfire exposure. Secondary outcomes included rates of ED visits or hospitalizations, prevalence of physician dispensed OCS prescriptions, and new diagnoses of asthma. Our 2003 analysis of the prevalence of physician-dispensed SABAs yielded the strongest results and indicated that obese pediatric patients exposed to wildfires that year had a higher prevalence of physician-dispensed SABA canisters than compared children with normal BMI. Although the increase in SABA dispensing before vs after the wildfires in 2007 was also significantly increased in obese asthmatic children, it was not significantly different than in asthmatic children with normal or overweight BMIs. Possible reasons for this discordance are discussed further below.
Emerging data in recent years have revealed that exposure to airborne pollutants (such as ozone, particulate matter, diesel exhaust, and cigarette smoke) activates Toll-like receptor signaling pathways that result in a proinflammatory response.21 It is not surprising, then that these airborne pollutants have been linked to worsening asthma outcomes.22–26 Although it is likely that asthma exacerbations in patients exposed to wildfires are due to increased exposure to airborne particulate matter levels1 and ozone precursors,2 our data suggest that patients with higher BMIs may be particularly susceptible to the increased pollutant levels during a wildfire.
Our study had also analyzed particulate matter data based on air samples from 6 separate San Diego Air Pollution Control centers in San Diego County without evidence of significant correlation between asthma outcomes and particulate matter exposure (data not shown). This is despite increases in particulate matter levels during the 2003 and 2007 fires (generally 2- to 3-fold) compared with before the fires (data not shown). Similar fold increases in particulate matter levels were observed in both the regions directly affected by the fire and indirectly affected, suggesting that wind patterns disseminated particulate matter diffusely throughout San Diego County.
A strength of our study is the ability to fully capture the health care use of the members within KPMG of Southern California. Electronic medical records of KPMG members are linked system-wide, and patients who interact with KPMG health care professionals for routine or urgent physician care, medication dispensing, and even telephone conversations are captured in our analysis. A limitation, though, of our study is that we are unable to account for the possibility that asthmatic patients may have taken more preventive actions1 (ie, wearing a mask or staying indoors) or may have even fled the wildfire areas due to local governmental warnings to evacuate high-risk areas. These individual patients, although part of KPMG and identified as asthmatic patients, may not have been present within the vicinity of the wildfire long enough to have adverse effects from wildfire exposure. However, the discordant results between the 2003 and 2007 SABA-dispensing data were not predicted. There are likely factors that contribute to this discrepancy that were not captured or controlled for in our study. Although our population was stratified by weight, the analysis did not require that the populations were longitudinally followed up. Future studies should focus on defining a specific cohort of individuals and following them up through sequential wildfire exposures to dissect these differences. Finally, this study found that there were very few underweight asthmatic children in our cohort, which supports the observation that childhood obesity is increasing in the United States but also limited our statistical power to detect any differences in the underweight BMI group.
Obese asthmatic patients were found in our study to have a significant increase in prevalence of SABA dispensing after wildfire exposure. This study adds to the body of evidence supporting the hypotheses that air quality and obesity adversely affect the asthmatic phenotype and that these 2 risk factors have a combined effect in vulnerable populations of asthmatic children.
Supplementary Material
Acknowledgments
We thank Bill Brick, senior meteorologist, at the San Diego County Air Pollution Control District, who provided all the particulate matter data.
Funding Sources: The project described was supported, in part, by the Department of Research and Evaluation within the Southern California Permanente Medical Group with funds from the Medical Group and the Kaiser Permanente Community Benefit Fund and by T32 National Institutes of Health training grant T32 AI 07469 (Dr Tse).
Footnotes
Disclosures: Authors have nothing to disclose.
Disclaimer: The contents and conclusions are solely the responsibility of the author and do not necessarily represent the official views of the department of Research and Evaluation and the Southern California Permanente Medical Group.
Supplementary Data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.anai.2015.01.018.
References
- 1.Kunzli N, Avol E, Wu J, et al. Health effects of the 2003 Southern California wildfires on children. Am J Respir Crit Care Med. 2006;174:1221–1228. doi: 10.1164/rccm.200604-519OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Viswanathan S, Eria L, Diunugala N, Johnson J, McClean C. An analysis of effects of San Diego wildfire on ambient air quality. J Air Waste Manag Assoc. 2006;56(1):56–67. doi: 10.1080/10473289.2006.10464439. [DOI] [PubMed] [Google Scholar]
- 3.Sin DD, Sutherland ER. Obesity and the lung, 4: obesity and asthma. Thorax. 2008;63(11):1018–1023. doi: 10.1136/thx.2007.086819. [DOI] [PubMed] [Google Scholar]
- 4.Camargo CA, Jr, Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159:2582–2588. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 5.Romieu I, Avenel V, Leynaert B, Kauffmann F, Clavel-Chapelon F. Body mass index, change in body silhouette, and risk of asthma in the E3N cohort study. Am J Epidemiol. 2003;158:165–174. doi: 10.1093/aje/kwg131. [DOI] [PubMed] [Google Scholar]
- 6.Chen Y, Dales R, Tang M, Krewski D. Obesity may increase the incidence of asthma in women but not in men: longitudinal observations from the Canadian National Population Health Surveys. Am J Epidemiol. 2002;155:191–197. doi: 10.1093/aje/155.3.191. [DOI] [PubMed] [Google Scholar]
- 7.Ford ES, Mannino DM, Redd SC, Mokdad AH, Mott JA. Body mass index and asthma incidence among USA adults. Eur Respir J. 2004;24(5):740–744. doi: 10.1183/09031936.04.00088003. [DOI] [PubMed] [Google Scholar]
- 8.Gunnbjornsdottir MI, Omenaas E, Gislason T, et al. Obesity and nocturnal gastro-oesophageal reflux are related to onset of asthma and respiratory symptoms. Eur Respir J. 2004;24:116–121. doi: 10.1183/09031936.04.00042603. [DOI] [PubMed] [Google Scholar]
- 9.Huovinen E, Kaprio J, Koskenvuo M. Factors associated to lifestyle and risk of adult onset asthma. Respir Med. 2003;97:273–280. doi: 10.1053/rmed.2003.1419. [DOI] [PubMed] [Google Scholar]
- 10.Nystad W, Meyer HE, Nafstad P, Tverdal A, Engeland A. Body mass index in relation to adult asthma among 135,000 Norwegian men and women. Am J Epidemiol. 2004;160:969–976. doi: 10.1093/aje/kwh303. [DOI] [PubMed] [Google Scholar]
- 11.Quinto KB, Zuraw BL, Poon KY, Chen W, Schatz M, Christiansen SC. The association of obesity and asthma severity and control in children. J Allergy Clin Immunol. 2011;128:964–969. doi: 10.1016/j.jaci.2011.06.031. [DOI] [PubMed] [Google Scholar]
- 12.Shore SA. Obesity, airway hyperresponsiveness, and inflammation. J Appl Physiol (1985) 2010;108:735–743. doi: 10.1152/japplphysiol.00749.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shore SA, Fredberg JJ. Obesity, smooth muscle, and airway hyper-responsiveness. J Allergy Clin Immunol. 2005;115:925–927. doi: 10.1016/j.jaci.2005.01.064. [DOI] [PubMed] [Google Scholar]
- 14.Strissel KJ, Stancheva Z, Miyoshi H, et al. Adipocyte death, adipose tissue remodeling, and obesity complications. Diabetes. 2007;56:2910–2918. doi: 10.2337/db07-0767. [DOI] [PubMed] [Google Scholar]
- 15.Wolfinger RD, O’Connell M. Generalized linear models: a pseudo-likelihood approach. J Stat Computation Simulation. 1993;48:233–243. [Google Scholar]
- 16.Deddens JA, Petersen MR. Approaches for estimating prevalence ratios. Occup Environ Med. 2008;65:481, 501–506. doi: 10.1136/oem.2007.034777. [DOI] [PubMed] [Google Scholar]
- 17.Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1955;11:375–386. [Google Scholar]
- 18.Dixon AE, Holguin F, Sood A, et al. An official American Thoracic Society Workshop report: obesity and asthma. Proc Am Thorac Soc. 2010;7:325–335. doi: 10.1513/pats.200903-013ST. [DOI] [PubMed] [Google Scholar]
- 19.Taylor B, Mannino D, Brown C, Crocker D, Twum-Baah N, Holguin F. Body mass index and asthma severity in the National Asthma Survey. Thorax. 2008;63:14–20. doi: 10.1136/thx.2007.082784. [DOI] [PubMed] [Google Scholar]
- 20.Mosen DM, Schatz M, Magid DJ, Camargo CA., Jr The relationship between obesity and asthma severity and control in adults. J Allergy Clin Immunol. 2008;122:507.e6–511.e6. doi: 10.1016/j.jaci.2008.06.024. [DOI] [PubMed] [Google Scholar]
- 21.Bauer RN, Diaz-Sanchez D, Jaspers I. Effects of air pollutants on innate immunity: the role of Toll-like receptors and nucleotide-binding oligomerization domain-like receptors. J Allergy Clin Immunol. 2012;129:14–24. doi: 10.1016/j.jaci.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwartz J, Slater D, Larson TV, Pierson WE, Koenig JQ. Particulate air pollution and hospital emergency room visits for asthma in Seattle. Am Rev Respir Dis. 1993;147:826–831. doi: 10.1164/ajrccm/147.4.826. [DOI] [PubMed] [Google Scholar]
- 23.McDonnell WF, Abbey DE, Nishino N, Lebowitz MD. Long-term ambient ozone concentration and the incidence of asthma in nonsmoking adults: the AHS-MOG Study. Environ Res. 1999;80(2 pt 1):110–121. doi: 10.1006/enrs.1998.3894. [DOI] [PubMed] [Google Scholar]
- 24.Nordenhall C, Pourazar J, Ledin MC, Levin JO, Sandstrom T, Adelroth E. Diesel exhaust enhances airway responsiveness in asthmatic subjects. Eur Respir J. 2001;17:909–915. doi: 10.1183/09031936.01.17509090. [DOI] [PubMed] [Google Scholar]
- 25.Li N, Hao M, Phalen RF, Hinds WC, Nel AE. Particulate air pollutants and asthma: a paradigm for the role of oxidative stress in PM-induced adverse health effects. Clin Immunol. 2003;109:250–265. doi: 10.1016/j.clim.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 26.Lin S, Liu X, Le LH, Hwang SA. Chronic exposure to ambient ozone and asthma hospital admissions among children. Environ Health Perspect. 2008;116(12):1725–1730. doi: 10.1289/ehp.11184. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.