Summary:
Fine hairs of the head and nape areas have been used as donor sources in eyelash transplantation but are straight, coarse, and grow rapidly, requiring frequent eyelash maintenance. This is the first reported case of eyelash transplantation by follicular unit extraction using leg hair as a donor source; findings were compared with that of another patient who underwent a similar procedure with donor hairs from the nape area. Although both patients reported marked improvement in fullness of eyelashes within 3 months postsurgery, the transplanted leg hair eyelashes required less frequent trimming (every 5–6 weeks) compared with nape hair eyelashes (every 2–3 weeks). Additionally, in leg hair eyelashes, the need for perming to sustain a natural looking eyelash curl was eliminated. Eyelash transplantation using leg donor hair in hirsute women may result in good cosmetic outcomes and require less maintenance compared with nape donor hair.
Eyelashes serve as the eyeball’s barrier, shielding it from small foreign bodies and irritants and participating in the reflex that closes the eye.1,2 They also play an important aesthetic role in the perception of beauty, facial expression, and personal interaction2—individuals suffering from madarosis report low self-esteem and confidence.2
Several methods exist to reconstruct eyelashes using head hair from the safe donor area, including reverse follicular unit grafting, follicular unit strip surgery, or follicular unit extraction (FUE).3–5 Although neck nape hair and finer hairs from the sides of the head have been used as donor sources,3 these hairs are usually straight instead of curled, relatively rigid, and grow rapidly. Such features demand frequent maintenance in the transplanted hair, including curling, perming, and trimming, and a potential for an unnatural look from thick donor hair.3
This case report describes the results of a patient undergoing an eyelash transplant by FUE using leg hair as the donor source compared with another patient who underwent a similar procedure (same surgeon, same technique) with nape area used as the donor hair source.
METHODS
Written consent for the surgery and permission to use photographs were obtained from both patients.
Two women were born with thin, sparse eyelashes and no medical history to explain the condition (eg, alopecia areata, trichotillomania, lupus erythematosus, trauma, blepharitis, eyelid surgery, thyroid disease, ectodermal dysplasia, or radiation/chemotherapy). Both women sought treatment for lack of length and fullness of their natural eyelashes but did not want an approved prostaglandin analogue (bimatoprost ophthalmic solution), which requires continuous use. Both had abandoned the use of eyelash extensions and false eyelashes due to potential eyelash loss and an insufficiently natural look.
Patient 1, a 20-year-old Hispanic woman with an eyelid length of 3.8 cm (Fig. 1), was sufficiently hirsute that leg hair could be used as a donor source in the FUE procedure (Fig. 2). Patient 2 was a 35-year-old Hispanic woman with an eyelid length of 3.5 cm. In contrast to patient 1, nape hair was used as a donor source in her procedure because she was not sufficiently hirsute for use of leg hair. Both patients were operated on within 1 week of each other using leg and nape hair extraction methods previously reported.6,7
Fig. 1.
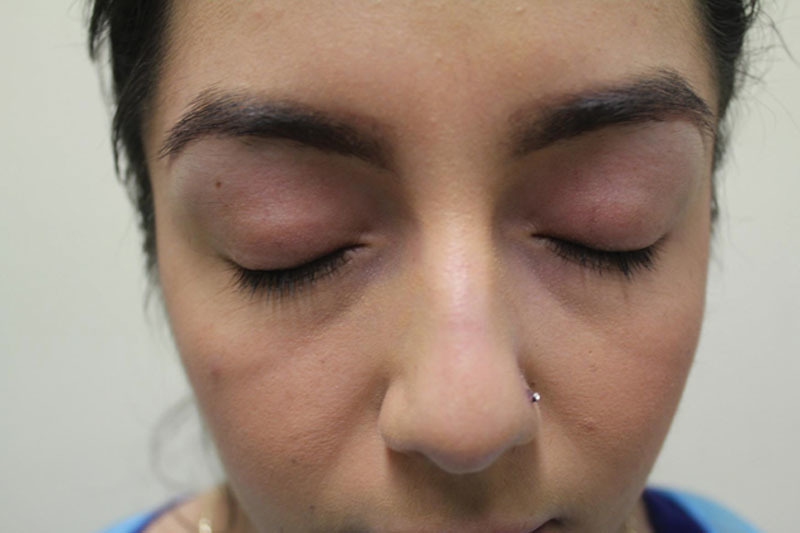
Patient 1, before leg-to-eyelash hair transplantation.
Fig. 2.

Patient 1, donor leg after hair follicle extraction.
The corneas were first locally anesthetized with proparacaine hydrochloride solution (0.5%) and lubricated with Maxitrol (neomycin and polymyxin B sulfates and dexamethasone ophthalmic suspension; Alcon Laboratories, Ft Worth, Tex.). Afterward, plastic corneal eye shields were inserted. Local anesthetic (approximately 2–4 mL each eyelid) consisting of a 1:5 bupivacaine and lidocaine 1:100,000 mix was injected into the subcutaneous layer of the lower two thirds of the upper eyelids. A rotary tool (UGraft prototype apparatus; Keck-Craig, Inc., Pasadena, Calif.) was used to mount a cutting punch device (UPunch Rotary; Dr. U Devices Inc., Redondo Beach, Calif.) that was fabricated at the author’s office. The customized punch tip has a cutting axis that points away from the follicles, thus minimizing trauma to the graft during extraction. Texturing at the punch tip pulls the graft up as it cuts around the follicle, thus minimizing the exactness with which the operator must trace the angles of the follicles below the skin surface. Patient 1 required 20-gauge punches due to the small caliber of leg hair, whereas patient 2 required use of 19-gauge punches due to thicker caliber nape grafts. Only single hair follicles were selected for grafting in both patients, and almost all surrounding skin was removed from the extracted grafts.
Hypodermic needle tips were customized to create curved slits to impart natural outward curl to the implanted grafts (away from the leading eyelid edge) and minimize the risk of trichiasis. Incisions were situated in the inferior tarsal border between preexisting eyelash follicles or superior to and abutting them. Patient 1 had 31 leg-derived grafts placed per eyelid, and patient 2 had 25 nape-derived grafts placed per eyelid. Chalazion clamps were not used.
Following the surgeries, no dressings were necessary. Maxitrol ointment was applied to the eyelids and inferior tarsal border for antibiotic prophylaxis and moisturization. Both patients used the ointment until their scabs fell off within 7 days. Patients were also advised to rinse the upper eyelids with distilled water, to remove debris by the gentle aid of Q tips, and to avoid rubbing the eyes or any rough handling of the eyelids post surgically.
RESULTS
Both patients reported drastic improvement in fullness of eyelashes within 3 months of surgery. In patient 1, the eyelashes with the transplanted leg hair never exceeded 1.5 cm, even when left untrimmed, reflecting the patient’s maximum leg hair length. As a result, the eyelashes did not require any trimming for the first 4 months after surgery and required trimming every 5–6 weeks thereafter. In contrast, the eyelashes with transplanted nape hair (patient 2) grew much longer, required trimming within the first 2 months and every 2–3 weeks thereafter. The leg donor area in patient 1 also healed with no cosmetically significant sequelae (Fig. 3).
Fig. 3.

Patient 1, donor leg 1 year after hair follicle extraction.
The transplanted leg hair eyelashes were more responsive to simple self-administered curling without the need for perming in a salon and maintained the natural curvature of the follicle, giving an appearance of full and naturally curved eyelashes (Fig. 4). In patient 2, the nape hair eyelashes were rather straight and unruly without perming (Fig. 5) and slightly more unnatural looking. To sustain an orderly, naturally curled eyelash, the patient felt that regular perming by a professional at monthly intervals was necessary.
Fig. 4.

Patient 1, after leg-to-eyelash hair transplantation. Leg hair in eyelashes sustains curl without perming.
Fig. 5.

Patient 2, post nape-to-eyelash hair transplantation. Nape hair is uncurled and unruly without perming.
A higher eyelash graft density was achieved during implantation with leg hair compared with nape hair (8.2 grafts/cm vs 7.2 grafts/cm), with thinner caliber contributing to a fuller, more natural outcome.
DISCUSSION
Gandelman3 originally advocated the use of delicate, thinner nape head hairs for eyelash transplantation, believing this would result in more natural eyelashes. However, those eyelashes generally grow at similar rates as scalp hair and require frequent trimming and curling (sustained by perming) at intervals of 2 weeks.3 Eyelash transplantation by FUE using leg hair is especially relevant in hirsute individuals who are born with thin eyelashes or have lost them due to trauma, surgery, inactive scarring, or inflammatory diseases. As described in the current report, transplanted leg hair might require minimal, postsurgical eyelash maintenance compared with transplanted nape and head hair, although it is possible that other body hairs with characteristics similar to leg hair could conceivably be used with similar results. Leg donor sites usually heal with no significant cosmetic scarring,6 and hair in this area is not desired by women.
PATIENT CONSENT
Patients provided written consent for the use of their images.
Footnotes
Disclosure: Dr. Umar is employed by FineTouch Dermatology, Inc. and has obtained a patent for the UPunch Rotary device and has applied for a patent for the UGraft apparatus; both are used in his surgeries. The Article Processing Charge was paid for by the author.
REFERENCES
- 1.Robins CR. Chemical and Physical Behavior of Human Hair. 4th ed. New York, N.Y.: Springer-Verlag; 2002. [Google Scholar]
- 2.Cohen JL. Enhancing the growth of natural eyelashes: the mechanism of bimatoprost-induced eyelash growth. Dermatol Surg. 2010;36:1361–1371. doi: 10.1111/j.1524-4725.2010.01522.x. [DOI] [PubMed] [Google Scholar]
- 3.Gandelman M. A technique for reconstruction of eyebrows and eyelashes. Semin Plast Surg. 2005;19:153–158. [Google Scholar]
- 4.Kumar A, Karthikeyan K. Madarosis: a marker of many maladies. Int J Trichology. 2012;4:3–18. doi: 10.4103/0974-7753.96079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Imagawa K. Eyelash transplant. In: Pathomvanich D, Imagawa K, editors. In: Hair Restoration Surgery in Asians. Tokyo: Springer; 2010. pp. 223–226. [Google Scholar]
- 6.Umar S. The transplanted hairline: leg room for improvement. Arch Dermatol. 2012;148:239–242. doi: 10.1001/archdermatol.2011.2196. [DOI] [PubMed] [Google Scholar]
- 7.Umar S. Eyebrow transplants: the use of nape and periauricular hair in six patients. Dermatologic Surg. 2014;40:1416–1418. doi: 10.1097/DSS.0000000000000169. [DOI] [PubMed] [Google Scholar]


