Abstract
Background:
The purpose of this study is to assess which personal characteristics and external factors are important contributors to eventual success.
Methods:
The authors distributed a survey to all members of the American Association of Plastic Surgeons and asked responders to rate the importance of 10 preselected qualities in contributing to their personal success. Survey outcomes were analyzed across different demographic groups.
Results:
Of the 580 American Association of Plastic Surgeons members who were surveyed, 295 returned completed surveys. Overall analysis indicates that hard work, compassion, and manual dexterity are the 3 most important attributes. Many significant differences are observed across demographic groups, indicating potential biases among the survey responders. Notably, we find that male surgeons attribute mentorship to success much more so than female surgeons (Column Trend Exact [CTE], P = 0.021), whereas female surgeons are more likely to attribute their success to hard work (CTE, P = 0.023). Similarly, those who have been program directors credit their success to mentoring more so than nonprogram directors (CTE, P < 0.00001). The authors also found that senior surgeons, as measured by years in practice, place greater emphasis on mentoring and career opportunities than younger surgeons (Mantel-Haenszel Trend, P = 0.003 and 0.0009, respectively). It is also interesting to note that individual talent qualities tend to be favored by more senior surgeons and those with more distant ties to academia.
Conclusion:
The authors believe that recognizing the relative importance of such factors, and their associated biases, is essential for the process of selecting and developing future successful plastic surgeons.
Applicants to plastic surgery residencies are seeking to join a competitive, innovatory profession. With high aspirations to live up to, one may wonder what personal qualities make and define a successful plastic surgeon. Although success—by definition and by practice—dynamically changes and may vary by whom it is being characterized, having the opinion of those who have “succeeded” may be helpful not only in choosing residents but also for these aspiring ones, who are more primed for achievement, thereby increasing the progression of the plastic surgery field as a whole. In reviewing current literature, there is an absence of studies focusing on the potential for career success of applicants to plastic surgery residency programs.
Previous studies have shown what personal characteristics are deemed important during the residency selection process. Such studies have a predictive component, looking at qualities that may lead to success during residency. Our earlier study showed that members of the distinguished American Association of Plastic Surgeons (AAPS) identified the character qualities of intelligence, dexterity, spatial sense, honesty, hardworking nature, patient commitment, teamwork, maturity, compassion, and personality as among the key, sought-after attributes in selecting residents.1 In otolaryngology, excellent academic achievement during medical school was correlated with high performance during residency.2 A similar study in orthopedics indicated academic honors in medical school clinical clerkships as most predictive of resident performance.3 The study also found a relationship between participation in fine motor activities and psychomotor performance. In general surgery, a connection was shown between recommendation letters, faculty evaluations of applicant personal characteristics, and future resident clinical performance.4 Although numerous publications pertaining to resident selection across various medical specialties stress the importance of such qualities, their effect on a surgeon’s ultimate success has not been evaluated.
Building on previous studies, the aim of this article is to show—rather than predict—what makes one an accomplished plastic surgeon. The closest study of this kind was conducted to evaluate predictors of future success in otolaryngology residency applicants5; although the goal may have been similar to that of our study, the methodology differed from that utilized here.
In this article, we address the qualities that are claimed by AAPS members to lead to career success. We respect the opinion of these surgeons, as they are considered to be admirable leaders and educators in the field of plastic surgery. Our purpose is to identify which factors—as identified in previous studies as important resident selection criteria—are key contributors in shaping successful plastic surgeons. Our analysis also aims to highlight potential response bias, as linked to respondent demographic groups. In this way, we seek to identify qualities of success as defined by these distinct groups and to highlight potential areas for conciliation when it comes to defined factors of achievement, which may 1) pave the way for a more consistent and reliable resident selection process, 2) offer resident educators an objective set of metrics important for future career success, and 3) provide guidance for aspiring young plastic surgeons.
METHODS
In 2008, the authors of this article electronically distributed a survey to the 580 members of the AAPS. The survey was closed after 1 month. Within the survey, responders were asked to rate the importance of 10 qualities in contributing to their personal success. These qualities were intelligence, hard work, compassion, artistic sense, spatial sense, engineering mindset, manual dexterity, career opportunities, mentorship, and supportive family. Responders selected among categories (irrelevant, not important, neutral, important, and very important) for each of the qualities. For statistical analysis, each category was converted to an ordinal number scale; “irrelevant” was assigned a value of 1 and “very important” a value of 5.
Additionally, the survey contained questions pertaining to nonidentifiable demographic information. These data included gender, history (or lack thereof) of serving as a program director, training background, years in practice, if retired from operating, involvement in interviewing residents, interaction with residents, and nature of practice (see Appendix of Liang et al1).
Survey outcomes were analyzed using SAS v9.2 (SAS Institute, Cary, N.C.) across different demographic groups, using Column Trend Exact (CTE) test for ordinal variables, Mantel-Haenszel Trend (MHT) test for interval variables, and Fisher’s exact test for discrete variables. Statistical significance was defined as P < 0.05 (two-tailed).
RESULTS
Respondent Numbers and Demographics
As reported in our previous article,1 295 of the 580 AAPS members returned completed surveys, a 51% response rate. Of the responders, 271 (92%) were men. About one third of survey participants (98) had been program directors in the past, whereas 66 individuals were currently so. Most responders endorsed former training in another field: general surgery (256), otolaryngology (11), other (10), oral-maxillofacial surgery (4), orthopedics (3), and neurosurgery (1). The number of years the survey participants had been in practice was normally distributed, with most reporting 21–30 years. A vast majority of the responding surgeons (238) were still in practice, while 51 were retired. Additionally, 205 surgeons noted regularly interviewing residency applicants; 39 occasionally interviewed applicants and 45 never did so. Most survey participants (232) reported constant interaction with residents, whereas 34 had intermittent interaction and 21 had little or no interaction. Many responders were affiliated with academic practices (134), as opposed to private (54) or combined practices (94).
Ranking of Characteristics
Analysis of survey responses shows that hard work, compassion, and manual dexterity are the 3 most important attributes that AAPS members credit to their career success. Hard work is the highest rated characteristic (μ = 4.81; SD = 0.40), with compassion and dexterity respectively following (μ = 4.52, 4.36; SD = 0.59, 0.60). Of slightly lesser significance—in descending order—are mentorship, spatial sense, supportive family, and intelligence, with little variability in score (μ = 4.22, 4.21, 4.21, 4.15; SD = 0.84, 0.79, 0.87, 0.58). The characteristics that most responders believe to be neutral for success are artistic sense, career opportunities, and an engineering mindset. These bottom 3 seem to cluster together away from the rest of the metrics (μ = 3.67, 3.50, 3.30; SD = 0.95, 1.00, 0.92), representing a bimodal distribution of the data. Furthermore, their larger SD values indicate a decreased consensus among responders with respect to the rating of these last 3 characteristics (Fig. 1).
Fig. 1.
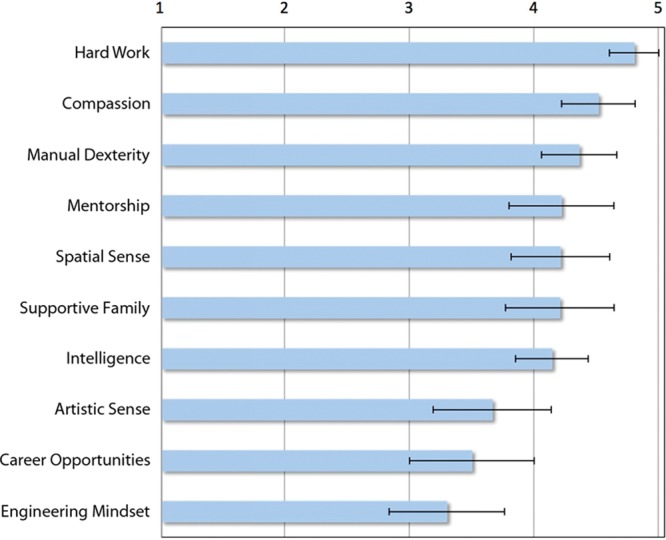
Characteristics important for career success as ranked by AAPS members, with a rating of 5 meaning “very important” and a rating of 1 meaning “irrelevant.”
Characteristics Favored by Respondent Demographic Groups
There are perceptible differences in responses among the demographic groups composing the respondent pool. Such discrepancies, while signifying potential biases among the survey participants, could represent innate consistency with their respective demographics.
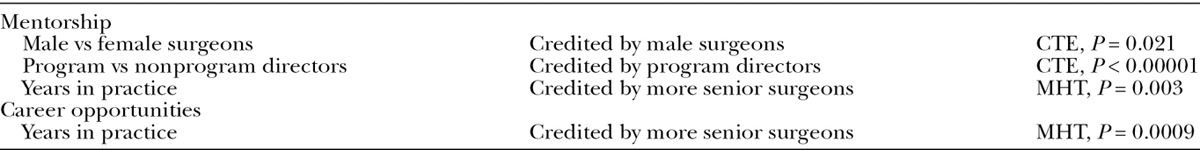
Male surgeons credit mentorship for their success more so than female surgeons (CTE, P = 0.021). Surgeons who have been program directors note mentorship as key remarkably more so than those who have never been program directors (CTE, P< 0.00001). Senior surgeons, as classified by years in practice, value mentorship more so than younger surgeons (MHT, P = 0.003). There is also a very strong correlation in attributing career opportunities to the reason for success as one spends more years in practice (MHT, P = 0.0009) (Table 1).
Table 1.
Comparison of Opinions among Respondent Demographic Groups for Mentorship and Career Opportunities
Female respondents endorse hard work as a factor contributing to their success, whereas male surgeons place less emphasis on this attribute (CTE, P = 0.023). In fact, all female respondents rank hard work very highly (giving it a rating of 5), whereas only 80% of males noted this characteristic as “very important.” Surgeons who do not work with residents as often also credit hard work as essential for their success (CTE, P = 0.035) (Table 2).
Table 2.
Comparison of Opinions among Respondent Demographic Groups for Hard Work and Compassion
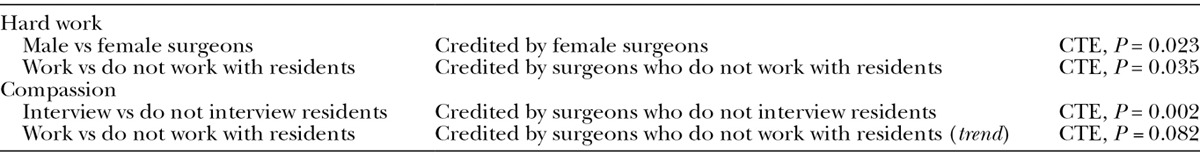
Surgeons who infrequently interview residents attribute success to compassion more highly than those who interview regularly (CTE, P = 0.002). There also seems to be a trend that the less one works with residents, the higher one rates compassion (CTE, P = 0.082) (Table 2).
Consistencies are present among certain demographic groups’ opinions of “talent qualities,” innate characteristics including intelligence, artistic sense, spatial sense, engineering mindset, and manual dexterity. With regard to intelligence, retired surgeons think that this metric factors in more so than do currently practicing surgeons (CTE, P = 0.038). Additionally, a trend seems to exist in that more senior surgeons believe intelligence contributed more to their success than is thought by younger surgeons (MHT, P = 0.063). There is also a noteworthy trend that surgeons who do not interview residents as often place greater emphasis on their intelligence contributing to their success (CTE, P = 0.061; Fisher’s exact test, P = 0.047) (Table 3).
Table 3.
Comparison of Opinions among Respondent Demographic Groups for Talent Qualities
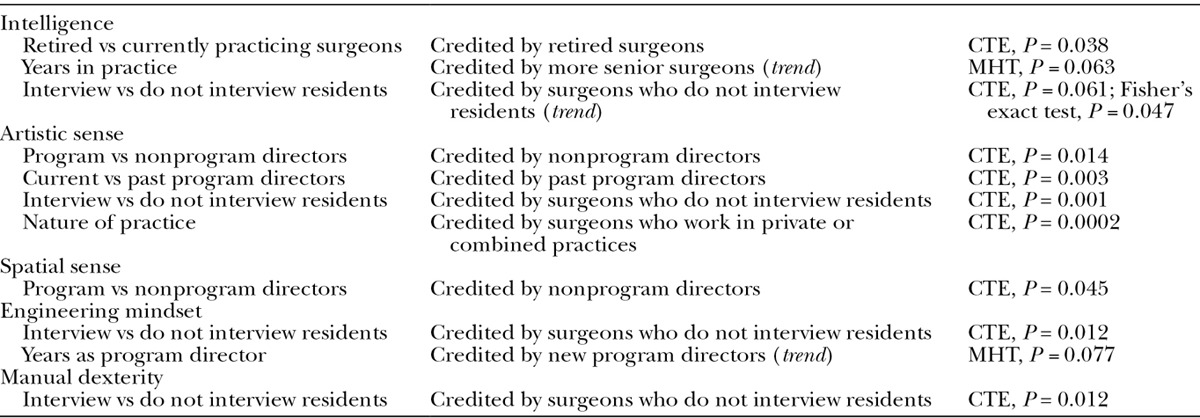
Current program directors credit their success much less to artistic sense than nonprogram directors (CTE, P = 0.014). In fact, they emphasize this trait even less so than surgeons who at one point were program directors (CTE, P = 0.003). A correlation also exists between interviewing less and attributing success more highly to artistic sense (CTE, P = 0.001). Furthermore, surgeons who work in private or combined practices rate artistic sense more highly than those who work in academic settings (CTE, P = 0.0002) (Table 3).
Program directors also give less credit to spatial sense than nonprogram directors (CTE, P = 0.045). Analysis also shows there is a trend in that the more years one spends as a program director, the less one associates an engineering mindset with success (MHT, P = 0.077). Additionally, interviewing more is linked to placing less emphasis on having an engineering mindset (CTE, P = 0.012). Also, the more one interviews, the less credit one gives to good dexterity (CTE, P = 0.012) (Table 3).
DISCUSSION
Although there have been studies, both in plastic surgery and in other fields, about desirable qualities of applicants and factors essential for success during residency, there are few studies that look into the ingredients for career success. A study with a similar goal to that of this article was performed in otolaryngology.5 Program graduates and faculty rated application factors’ correlation with posttraining success, and it was found that excellence in teamwork is a predictor of continued achievement in clinical medicine. This approach of measuring near-future success through quantitative educational metrics has previously been performed in plastic surgery.6 Our current study is an introspective—rather than purely retrospective—examination of career success in the long term.
For this article, we sought the input of members of AAPS, whose opinion we value as they are leaders in the field and have achieved career success of their own. We found that the top-rated characteristics for career success as classified by AAPS surgeons are hard work, compassion, and manual dexterity. There is consistency between these results and those of our previous study,1 where it was found that 2 of these qualities (hard work and compassion) are important factors for resident selection as indicated, likewise, by members of the AAPS. The remaining characteristics—mentorship, spatial sense, intelligence, supportive family, artistic sense, career opportunities, engineering mindset—also provide valuable insight and points for interpretation.
We have found that certain ratings of characteristics follow trends with respect to the demographic of the respondent. For instance, mentorship is favored by male surgeons, program directors, and senior surgeons, whereas hard work is credited more by females and surgeons who do not work with residents as much. Plastic surgery is a traditionally male-dominated field, and therefore, men have more in common with mentors, whereas women may feel more isolated and dependent on themselves. Although there may be significant bias reflected in our results, as the vast majority (271 of 295) of respondents were male, this discrepancy—and that in the field as a whole—may have been a major factor behind the survey responses of female surgeons, for instance ranking hard work more highly and mentorship less highly than their male counterparts. Nevertheless, hard work still landed the top spot for most important attribute for career success (rated 5 by all female and 80% of male responders), whereas mentorship (highly appraised by male responders) did not make the top 3 for female surgeons. It is interesting to speculate whether, had there been a greater proportion of female respondents, the top-rated characteristics would have differed from those found.
The observation that mentorship is credited by program directors—a demographic associated with academic settings—is hardly surprising, given that this quality is hallmark of a cultivating, academic environment. On the other hand, surgeons who do not work with residents rate hard work as essential to success. Many of these surgeons are in solo practices, where success is more dependent on how hard one works rather than being able to rely on an environment that is more nurturing, such as academia. This is comparable to the trend among female surgeons, who are, as discussed above, similarly self-reliant.
As shown through our survey results, more senior surgeons credit much of their success to mentorship, while being mentors themselves. The career opportunity metric is also favored by this group, which has relevance in that these surgeons have been around for longer and have likely served as both mentors and mentees. With respect to the senior physician demographic, there is the notion that the older you get, the wiser you become. As people age, they are able to reflect on past experiences and draw conclusions. It is often that we turn to those senior to us in years and experience for guidance with many aspects of our lives. Likewise, senior surgeons are commonly regarded as knowledgeable and capable of providing sound advice. In this regard, one may conclude that either these seniors in the field have a useful big picture view or they may be self-selecting.
With regard to compassion, it is observed that those surgeons who are not involved with residency education credit this characteristic as foreshadowing of success. This group is mainly made up of surgeons in private practice. Thus, an individual quality has again outweighed aspects of a nurturing academic environment (as was seen with hard work).
Similar findings were evident with what we termed as “talent qualities”; these seem to be favored by senior surgeons and those not working in academia. There is a notable partiality for artistic sense among those surgeons who are not involved in resident education. Given that this group is vastly made up of surgeons in private practice, where cosmetic procedures are more common, the encouragement for artistic sense is understandable. On the other hand, program directors—a demographic associated with academic settings—generally think otherwise of the talent-oriented metrics, especially artistic sense, spatial sense, and engineering mindset. It is interesting that the nature of one’s practice may have such an effect on opinion; personal traits that are generally thought to be important are not highly credited by the program directors, who think other factors are more important for career success. In this regard, academic programs perhaps should focus on developing such qualities during residency training.
Intelligence, another example of a talent quality, is strongly favored by retired surgeons. The survey responses of this demographic bring an interesting perspective, as these may be considered as reflective opinions of their careers. Retired surgeons have likely reached—or at least neared—their full potential, whereas currently practicing surgeons are still working to better their practices by learning from their successes and their mistakes. After all, one may not teach any monkey how to operate well, as often joked about in academic training.
As was found among those who work with residents, our results indicate that greater involvement in resident interviews is correlated with less emphasis toward “soft characteristics,” such as compassion, artistic sense, engineering mindset, manual dexterity, and intelligence. The survey responses of these surgeons may have reflected a preference more for a successful resident candidate within an academic setting, rather than a successful future surgeon. In other words, our data seem to uncover a tendency in academic programs to search for good residents rather than those who have potential to become accomplished surgeons.
Interestingly, we did not find any demographic variation with regard to responders’ view of supportive family. This could be a reflection of the survey design; a lack in stratification of respondents’ familial situations may result in the appearance that everyone views this metric similarly. On the other hand, having a supportive family unit may very well be a standard that most individuals agree on, in spite of “family” being an arbitrary term.
The underlying strength behind this study is the pool of people surveyed. The AAPS is composed of relatively more senior and accomplished plastic surgeons, the best in the field. They are in fact our current educators, primed with years of experience. It is therefore intuitive that we hear from these surgeons, our seniors, to identify reasons pertaining to individuals’ attaining success. According to their responses to our survey, we see trends such as soft characteristics being seen as favorable, but such preferences are linked to the background of the respondent. A major divide in our results was found to be between those in academic and private practice. Success can be found in both practice settings; however, there is the paradox that while those in academia are doing the educating, many plastic surgeons do not have academic careers. As a significant number of plastic surgeons are in private practice, perhaps resident education needs to be tailored to encompass those metrics valued by the private practitioners, not only those favored by those in academia.
This study is the first of its kind in plastic surgery. Our findings build on earlier studies to provide a roadmap for aspiring students, guidelines for resident educators, and feedback for selection committees. By objectively applying such standards, we come closer toward the goal of illustrating the meaning of success in plastic surgery, as well as outlining how we can do things better and how we can improve as a field. Previously introduced was the concept of success as a plastic surgery resident being measured by educational metrics.6 Another study further added to these rudimentary metrics by eliciting the specific personal characteristics of residency applicants deemed important by AAPS members.1 Although the criteria in both studies were those used for choosing residents, functional application in the long term may be used to project clinical success, as indicated through our study.
CONCLUSIONS
In conclusion, the most important qualities that AAPS surgeons recognize as predictors of personal success are hard work, compassion, and manual dexterity. As biases do exist across respondent demographic groups in their assessment of important factors for success, these are important to identify during resident selection. For instance, we need to be mindful that we choose not only good residents but also, more importantly, those who possess the raw talent to become successful surgeons in the future. It is perhaps such qualities that future applicants should aspire to attain and resident educators should endorse. There are strong indications that the opinions of those with more years in practice should be highly valued. Reviewing what led to the success of the best in plastic surgery will aid in future progression of the field.
ACKNOWLEDGEMENT
This article is dedicated to Dr. Robert M. Goldwyn, whose insights and enthusiasm made this project possible.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Liang F, Rudnicki PA, Prince NH, et al. An evaluation of fundamental resident selection factors by AAPS surgeons. J Surg Educ. 2015;72:8–15. doi: 10.1016/j.jsurg.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Calhoun KH, Hokanson JA, Bailey BJ. Predictors of residency performance: a follow-up study. Otolaryngol Head Neck Surg. 1997;116(6 Pt 1):647–651. doi: 10.1016/S0194-5998(97)70242-0. [DOI] [PubMed] [Google Scholar]
- 3.Dirschl DR, Dahners LE, Adams GL, et al. Correlating selection criteria with subsequent performance as residents. Clin Orthop Relat Res. 2002;399:265–271. doi: 10.1097/00003086-200206000-00034. [DOI] [PubMed] [Google Scholar]
- 4.Brothers TE, Wetherholt S. Importance of the faculty interview during the resident application process. J Surg Educ. 2007;64:378–385. doi: 10.1016/j.jsurg.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Chole RA, Ogden MA. Predictors of future success in otolaryngology residency applicants. Arch Otolaryngol Head Neck Surg. 2012;138:707–712. doi: 10.1001/archoto.2012.1374. [DOI] [PubMed] [Google Scholar]
- 6.Guo L, Friend J, Kim E, et al. Comparison of quantitative educational metrics between integrated and independent plastic surgery residents. Plast Reconstr Surg. 2008;122:972–978; discussion 979–981. doi: 10.1097/PRS.0b013e3181811c6d. [DOI] [PubMed] [Google Scholar]


