Abstract
Autoimmune hypothyroidism is a common medical condition. Its revelation by thyrotrophic hyperplasia is an unusual and may be misdiagnosed as a pituitary adenoma. A 35-year-old man is referred to us for endocrinological assessment before surgery of a pituitary macroadenoma with bitemporal hemianopsia. Biological data reveal profound primary hypothyroidism. With thyroid hormone substitution, the thyroid function was normalized. Follow-up magnetic resonance imaging, showed the complete shrinkage of the pituitary mass attesting of a thyrotrophic pituitary hyperplasia. This case highlights the importance of a multidisciplinary assessment of pituitary masses to avoid unnecessary surgery and to prevent consequences of sellar masses.
Key words: primary hypothyroidism, pituitary hyperplasia, pituitary macroadenoma, autoimmune thyroiditis
Introduction
Primary hypothyroidism is a common medical condition. Symptoms may be vague, misleading and thus delay the diagnosis, which can be made in unusual circumstances.
Thyrotrophic cell hyperplasia has been described in longstanding hypothyroidism and may mimic the appearance of a pituitary macroadenoma.1,2
We report the case of a patient with primary hypothyroidism revealed by a pituitary mass and we describe his clinical course during L-thyroxin replacement therapy.
Case Report
A 35-year-old man, with history of recent dyslipidemia treated by fenofibrate without etiological assessment, presented with chronic headaches without vomiting and without visual field changes clinically perceived.
A computed tomography (CT) scan was performed and showed a suprasellar mass measuring 12.5 mm.
Pituitary magnetic resonance imaging (MRI) revealed a 15×17×12 mm pituitary mass discreetly hyperintense on a T1 weighted image, hyperintense on a T2 weighted image, intensely enhanced following gadolinium injection with elevation of the optic chiasm and the pituitary stalk. The mass was bilaterally infiltrating the cavernous sinus (Figure 1) and was reported to be suggestive of a pituitary macroadenoma by radiologists.
Figure 1.
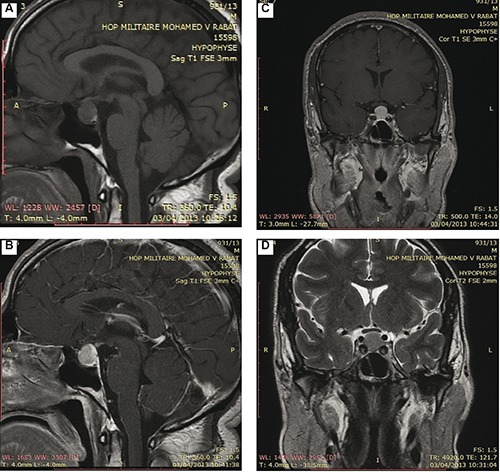
Sagittal (A and B) and coronal (C and D) magnetic resonance images showing an enlarged pituitary gland with suprasellar extension.
Computerized visual field showed bitemporal hemianopsia.
The patient was referred for an endocrinological assessment before planned surgery.
Upon careful questioning, the patient also reported a long history of tiredness, cold intolerance, hoarseness of voice, constipation and gain weight without lifestyle changing.
General examination reveals a bradycardia with a pulse rate at 55/min, and a body mass index of 30.5 kg/m2.
He had a dry skin, a pale puffy face with palpebral edema, thinning of the outer third of the eyebrow and macroglossia.
Thyroid gland was not palpable.
Thyroid function test was consistent with primary hypothyroidism with free thyroxine T4: 0 ng/dL [normalized ratio (NR): 0.61-1.12], free triiodothyronine T3: 1.88 pg/mL (NR: 2.50-3.90) and thyroid-stimulating hormone (TSH) us >100 µUI/mL (NR: 0.34-5.60).
Formal testing revealed mild hyperprolactinemia at 22.5 ng/mL (NR: 2.64-13.13), a serum testosterone at 2.04 ng/mL (NR: 2-10), FSH at 5.1 UI/L (NR: 1.27-19.26) and LH at 2.8 UI/L (NR: 1.24-8.62).
Thyroperoxidase antibodies testing revealed a raised level at 56.9 UI/mL (NR: 0.25-9) and thyroid ultrasound found an atrophic hypoechoic gland consistent with autoimmune thyroiditis.
Based on clinical, laboratory and imaging findings, we considered a diagnosis of primary hypothyroidism complicated by compensatory pituitary hyperplasia.
Despite visual field anomalies, we decided to cancel surgery and started the patient on Lthyroxin substitution therapy gradually increasing to 150 µg daily.
Four months later, the patient clinically improved. Thyroid function was normalized.
Follow up MRI study documented the complete shrinkage of the pituitary mass, the pituitary gland was at 10 mm homogeneously enhanced without any circumscribed lesion confirming the diagnosis of thyrotrophic pituitary hyperplasia (Figure 2).
Figure 2.
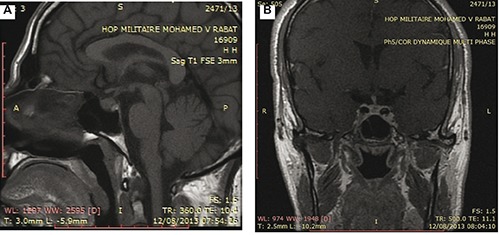
After 4 months of L-thyroxin replacement therapy, sagittal (A) and coronal (B) magnetic resonance images showing the complete resolution of the pituitary mass with normalization of its size and contour and no signs of bleeding or necrosis.
Discussion
Pituitary hyperplasia is an enlargement of the pituitary gland due to a reversible increase in the number and/or hyperplasia in one or more hormone-producing cell types. It can occur as a normal response to physiological stimulation during infancy, pregnancy and lactation, or as a pathological condition.1
Pituitary tumorous hyperplasia due to primary hypothyroidism occurs most frequently among all feedback tumors, occupying 33.3%.3
Thyrotrophic hyperplasia can be explained by the classical negative feedback loop in which reduced circulating levels of thyroid hormone result in overstimulation of thyrotrophs by thyrotropin releasing hormone.2
Pituitary enlargement in primary hypothyroidism is mainly asymptomatic.4
The main complain of our patient was the chronic headaches that leaded to perform cerebral imaging first despite the marked clinical features of hypothyroidism which were disregarded by the patient and the clinician.
In fact, despite recent progress in medical imaging, to date, key imaging techniques including MRI, cannot distinguish pituitary macroadenoma from hyperplasia.1
The traditional CT criteria for pituitary macroadenoma include homogeneous enlargement of the gland to a height of greater than 10 mm, with or without erosion of the floor of the sella and deviation of the stalk.5 The CT findings of macroadenoma overlap considerably with those of a diffusely enlarged pituitary gland.
Different pituitary enhancement patterns between tumor and hyperplasia by MRI have been described in some cases,6 while a midline prominence of a pituitary mass with smooth contours (the nipple sign) has been proposed as suggestive of pituitary hyperplasia.7 Despite the above theoretical considerations, MRI findings suggestive of a TSH-secreting adenoma, i.e. central enhancing mass with a rim of normal compressed pituitary tissue, may also be seen in hypothyroidism-induced pituitary hyperplasia,8 as well as in the rare entity of hypophysitis.9
Therefore, the diagnosis of thyrotrophic pituitary hyperplasia must rely heavily on the patient’s past history and on detailed endocrine work-up.
Without knowledge of the patient’s hormonal profile, the pituitary mass was first reported as a macroadenoma. After documenting primary hypothyroidism, we considered the diagnosis of reactive pituitary hyperplasia, which was definitively confirmed by the regression of the pituitary mass on the MRI control after substitution therapy allowing us to avoid an unnecessary and dangerous surgery. Similar observations have been described in the literature emphasizing the importance of pituitary hormones assessment in the evaluation of pituitary masses.1-2
Thyrotrophic pituitary hyperplasia resolves completely with thyroxin therapy.2,8-10 Despite the evidence of bilateral hemianopsia and the elevation of the optic chiasma, we decide to run a thyroxin substitution therapy rather than surgery for decompression of the optic chiasma. Our decision was comforted by the Sarlis et al. report of a dramatic shrinkage of a pituitary mass in a case of primary hypothyroidism after only one week of acute thyroid hormone therapy.10 We believe that thyroxin therapy is the first intention treatment of thyrotrophic pituitary hyperplasia even with visual complications.
Conclusions
Primary hypothyroidism should be considered in the differential diagnosis of solid pituitary lesions, hence the need of a multidisciplinary assessment of pituitary masses involving endocrinologist, radiologist and neurosurgeons to avoid misdiagnosis, unnecessary and dangerous surgery and prevent complications of sellar and suprasellar masses.
References
- 1.Epunza Kanza R, Gagnon S, Villeneuve H, et al. Spontaneous ovarian hyperstimulation syndrome and pituitary hyperplasia mimicking macroadenoma associated with primary hypothyroidism. World J Radiol 2013;5:20-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Şimşek E, Şimşek T, Savaş-Erdeve Ş, et al. Pituitary hyperplasia mimicking pituitary macroadenoma in two adolescent patients with long-standing primary hypothyroidism: case reports and review of literature. Turk J Pediatr 2009;51:624-30. [PubMed] [Google Scholar]
- 3.Gu S, He R.Pituitary feedback tumor (18 cases analysis). Henan Med Info 1997;5:3-4. [Google Scholar]
- 4.Katz MS, Gregerman RI, Horvath E, et al. Thyrotroph cell hyperplasia of the human pituitary gland associated with primary hypothyroidism: clinical and morphological features. Acta Endocrinol (Copenh) 1980;95:41-8. [DOI] [PubMed] [Google Scholar]
- 5.Elster AD. Modern imaging of the pituitary. Radiology 1993;187:1-7. [DOI] [PubMed] [Google Scholar]
- 6.Kuroiwa T, Okabe Y, Hasuo K, et al. MR imaging of pituitary hypertrophy due to juvenile primary hypothyroidism: a case report. Clin Imaging 1991;15:202-5. [DOI] [PubMed] [Google Scholar]
- 7.Ahmed M, Banna M, Sakati N, et al. Pituitary gland enlargement in primary hypothyroidism: a report of 5 cases with follow-up data. Horm Res 1989;32:188-92. [DOI] [PubMed] [Google Scholar]
- 8.Wolanski LJ, Leavitt GD, Elias BJ, et al. MRI of pituitary hyperplasia in hypothyroidism. Neuroradiology 1996;38:50-2. [DOI] [PubMed] [Google Scholar]
- 9.Beressi N, Cohen R, Beressi J-P, et al. Pseudotumoral lymphocytic hypophysistis successfully treated by corticosteroid alone: first case report. Neurosurgery 1994;35:505-8. [DOI] [PubMed] [Google Scholar]
- 10.Sarlis NJ, Brucker-Davis F, Doppman JL, et al. MRI-demonstrable regression of a pituitary mass in a case of primary hypothyroidism after a week of acute thyroid hormone therapy. J Clin Endocrinol Metab 1997;82:808-11. [DOI] [PubMed] [Google Scholar]


