Abstract
We report the case of a 64-year-old white male who presented to his primary care physician with complaints of fatigue. Physical exam was unremarkable and laboratory studies revealed profound anemia, for which the patient received a transfusion. Esophagogastroduodenoscopy revealed a bleeding mass in the proximal stomach that was histologically determined to be malignant melanoma, with immunohistochemical staining demonstrating positivity for SOX10, S100, MART-1, and HMG-45. After an extensive dermatological exam no other primary lesion was identified. Whole body positron emission tomography (18-FDG-PET/CT) demonstrated pathologic uptake only in the area of the proximal stomach. For this reason, primary gastric melanoma was suspected in this patient. The patient underwent subtotal gastrectomy with mass excision followed by Roux-en-Y reconstruction. Very few cases of primary gastric melanoma have been reported. We report this case and present diagnostic criteria for primary non-cutaneous melanoma and discuss potential non-surgical therapies.
Key words: melanoma, surgery, gastric, gastrointestinal
Introduction
Melanoma represents 1-3% of all malignant cancers and typically appears in sites where melanocytes are commonly found, including the skin, eyes, meninges, and anal region, most commonly in the rectum and sigmoid colon.1 Primary gastric melanoma is a rare clinical entity with 11 cases reported worldwide.2-12 Most melanomas identified in the stomach represent metastases from cutaneous sources. According to a historical clinicopathologic analysis of 652 patients with disseminated melanoma, 58% demonstrated small bowel metastases upon autopsy, 26% were found to have gastric metastases, but only 1.5% were identified to have any gastrointestinal lesions antemortem.13,14 Therefore thorough physical examination, laboratory studies, and imaging are required to rule out metastatic disease in the setting of gastric melanoma.
We report the case of a 64-year-old white male with a large, ulcerated mass located in the proximal greater curvature region of the stomach, which manifested itself with fatigue and profound anemia and no other initial presenting symptoms. Biopsy of the mass and subsequent histological examination identified the lesion as a malignant melanoma and detailed clinical, laboratory, and imaging studies revealed no other primary lesion. Very few cases of gastric melanoma with no primary lesion have been described and we believe this represents an exquisitely rare presentation of primary melanoma.
Case Report
A 64-year-old white male presented to his primary care physician with a history of nonspecific fatigue. Physical exam was unremarkable. Laboratory studies revealed profound anemia that required transfusion of six units of blood. Suspicion for intra-abdominal bleeding prompted a colonoscopy, which was unremarkable, and an Esophagogastroduodenoscopy (EGD), which revealed a large 7.6×5.3 cm ulcerated mass along the greater curvature of the stomach. Endoscopic biopsy demonstrated nests of cells with large nuclei, prominent nucleoli, and abundant cytoplasm expanding the lamina propria. Histological examination of the biopsy revealed IHC positivity for SOX10, S100, MART-1, and HMG 45 confirming malignant melanoma. A thorough dermatologic examination revealed no concerning cutaneous lesions and upon further investigation the patient had no recollection of a regressed skin lesion. Whole-body positron emission tomography (18-FDG-PET/CT) scan revealed avidity only in the region of the anterior stomach, suggesting the diagnosis of primary gastric melanoma (Figure 1). Surgical exploration demonstrated a large, pigmented, ulcerated mass along the greater curvature of the stomach that was excised with a subtotal gastrectomy and lymph node dissection.
Figure 1.
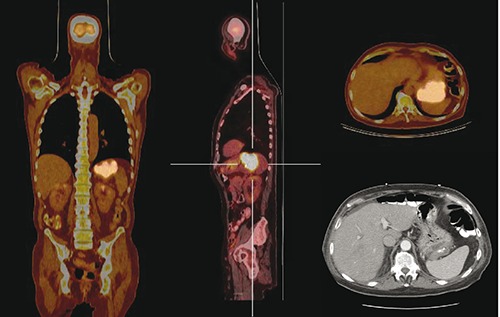
Whole body positron emission tomography (18-FDG-PET/CT) scan identifying the location of the malignancy and demonstrating no pathological uptake in any other organs. Left: coronal section PET/CT scan identifying location of primary gastric cancer. Center: pathologic uptake of 18-FDG in primary gastric cancer, sagittal section. Top right: transverse PET/CT of primary gastric cancer. Bottom right: transverse section CT scan identifying large, ulcerated neoplasm.
Pathological examination of the surgical specimen revealed a large melanoma of the greater curvature of the stomach, 10 cm in greatest diameter that invaded through the muscularis propria and into the subserosa but did not invade through the visceral peritoneum (Figure 2). Lymphovascular penetration was evident. Proximal and distal margins were negative for malignancy and there was no evidence of lymph node metastases. Histological analysis of the surgical specimen revealed IHC positivity for MART-1 and S100 (Figure 3). The patient’s immediate post-operative course was unremarkable and he was observed for recurrent disease in the absence of adjuvant therapy. Approximately 18 months later he presented with widespread small bowel metastases that were not amenable to resection and he expired shortly thereafter due to diffuse gastrointestinal necrosis secondary to thromboembolization caused by cardiac arrhythmia. Due to poor performance status during the latter presentation he was not a candidate for palliative chemotherapy.
Figure 2.
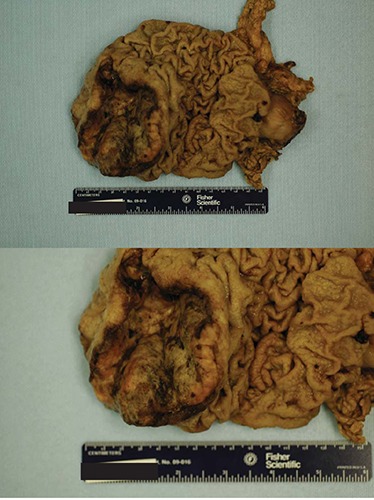
Subtotal gastrectomy specimen of primary gastric melanoma. A large, fungating, ulcerated mass filled with black pigment is demonstrated. Top: whole specimen of primary gastric melanoma. Bottom: zoomed in photograph of primary gastric melanoma.
Figure 3.
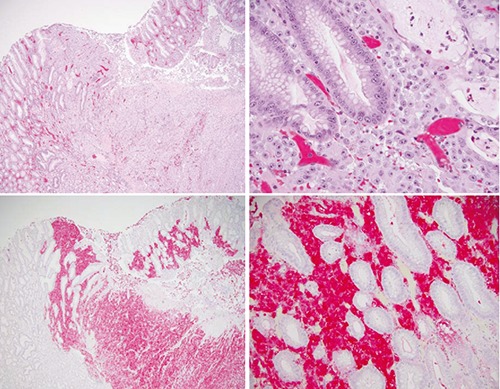
Histological sections of gastrectomy specimen of primary gastric melanoma. Top: Hematoxylin and Eosin sections at 4× and 20× magnification identifying primary neoplasm within the gastric architecture, demonstrating nests of cells with large nuclei, prominent nucleoli, and abundant cytoplasm that expand the lamina propria. Bottom: positive staining for MART-1 (4×) and S100 (20×) indicate a malignant melanocytic neoplasm.
Discussion
Melanoma is an aggressive cancer that commonly presents in tissues where melanocytes reside, including the skin, eyes, meninges, and anal region. Gastrointestinal melanoma is most often the result of metastatic disease, with up to 60% of patients with metastatic melanoma having gastrointestinal (GI) involvement upon autopsy.13,14 However, sporadic reports of primary gastric melanoma exist, totaling 11 cases in the literature.2-12 Additionally, cases involving the esophagus, small intestine, gall bladder, common bile duct, and transverse colon have also been reported.15-20 Esophageal melanoma appears to be the most common with 15 cases reported in 2014. The development and pathogenesis of primary melanoma within the GI tract is unknown and two mechanisms have been proposed. First, neural crest derivatives such as APUD cells may gain or retain the ability to de-differentiate into melanocytes and subsequently undergo malignant transformation.21 Second, ectopic migration of melanocytes into the GI tract was previously identified, suggested by the observation of benign melanosis involving the esophagus in cases of esophageal carcinoma, anal melanoma, and esophagitis, respectively.22-24 An extension of that observation makes primary gastric melanoma a reasonable possibility.
The rarity of gastric melanoma rightfully raises suspicion for a regressed primary cutaneous melanoma. An extensive dermatologic and imaging workup is warranted to identify any potential metastatic sources for the disease. In addition, a thorough patient history with particular attention to sun exposure and previous cutaneous lesions that were either excised or spontaneously regressed is critical. Specific suggestions have been recommended for the diagnosis of primary non-cutaneous melanoma including an absence of prior melanotic lesion removal from the skin and no involvement of other organs upon presentation.5 Subsequent imaging with 18-FDG-PET/CT modalities can define the extent of the disease ensuring limitation to the stomach. Another important criteria is documented disease-free survival of at least 12 months as less than 50% of patients diagnosed with metastatic, late-stage disease survive longer than 1 year and carry a median survival of 10 months.25-27
Adjuvant therapy for primary non-cutaneous melanoma is understudied and poorly understood so there are few current treatment indications for patients after surgical excision. A prior case report detailed a patient who underwent adjuvant therapy following surgical resection of a primary gastric melanoma.6 This patient was treated with partial gastrectomy and splenectomy followed by 12 months of interferon, and showed no evidence of disease upon EGD two years post-operatively. Another case report documents chemo-radiotherapy with dacarbazine for palliation after the patient developed metastases from a primary gastric melanoma.7 A third patient declined adjuvant therapy.12 Vemurafenib, a BRAF V600E inhibitor approved for the treatment of metastatic melanoma, has not been evaluated as a potential adjuvant treatment for patients presenting with primary noncutaneous melanomas. Some evidence exists that mucosal melanomas do not harbor BRAF/NRAS mutations suggesting that anti-BRAF therapy would be ineffective for patients with gastrointestinal melanoma.28 There is a need to study the genetics of noncutaneous melanoma, including primary gastric melanoma, in order to identify novel tumor vulnerabilities and to develop new therapies as an adjunct to surgical resection or as primary therapy when surgical resection is not an option.
Certainly, further insight is required, as case reports have detailed interferon therapy or chemotherapy for adjuvant treatment but no clear consensus exists. Finally, diagnosis of primary non-cutaneous melanoma can be made retrospectively if the patient survives more than 12 months as more than 50% of patients with metastatic melanoma will succumb in less than 1 year.
Conclusions
Primary gastric melanoma is an uncommon malignancy that manifests with symptoms such as abdominal pain, nausea, hematemesis, and melena, as well as nonspecific symptoms of fatigue, anemia, and weight loss. Accurate diagnosis depends on biopsy and IHC staining for melanoma markers such as SOX10, S100, and HMB-45. The designation of a primary lesion is dependent on an extensive dermatologic examination that does not identify an overt melanotic lesion and 18-FDG-PET/CT imaging that does not show pathologic 18-FDG uptake in any other organs. Adjuvant therapy has not been fully evaluated in patients with primary gastric melanoma.
Funding Statement
Funding: A.A. is supported by the UTSW Medical Scientist Training Program and the Ruth L. Kirschstein National Research Service Award for Individual Predoctoral MD/PhD Fellows (1F30CA168264).
References
- 1.Tas F, Keskin S, Karadeniz A, et al. Noncutaneous melanoma have distinct features from each other and cutaneous melanoma. Oncology 2011;81:353-8. [DOI] [PubMed] [Google Scholar]
- 2.Grilliot MA, Goldblum JR, Liu X.Signetring cell melanoma of the gastroesophageal junction: a case report and literature review. Arch Pathol Lab Med 2012;136:324-8. [DOI] [PubMed] [Google Scholar]
- 3.Yamamura K, Kondo K, Moritani S.Primary malignant melanoma of the stomach: report of a case. Surg Today 2012;42:195-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khaliq A, Siddappa PK, Thandassery RB, et al. Melanoma of stomach. J Gastrointest Cancer 2012;43:630-3. [DOI] [PubMed] [Google Scholar]
- 5.Lagoudianakis EE, Genetzakis M, Tsekouras DK, et al. Primary gastric melanoma: a case report. World J Gastroenterol 2006;12:4425-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alazmi WM, Nehme OS, Regalado JJ, et al. Primary gastric melanoma presenting as a nonhealing ulcer. Gastrointest Endosc 2003;57:431-3. [DOI] [PubMed] [Google Scholar]
- 7.Kim NR, Lee WK, Chung DH. Primary gastric melanoma with rhabdoid features: a case report. Korean J Pathol 2013;47:606-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ravi A. Primary gastric melanoma: a rare cause of upper gastrointestinal bleeding. Gastroenterol Hepatol 2008;4:795-7. [PMC free article] [PubMed] [Google Scholar]
- 9.Castro C, Khan Y, Awasum M, et al. Case report: primary gastric melanoma in a patient with dermatomyositis. Am J Med Sci 2008;336:282-4. [DOI] [PubMed] [Google Scholar]
- 10.Jelincic Z, Jakic-Razumovic J, Petrovic I, et al. Primary malignant melanoma of the stomach. Tumori 2005;91:201-3. [DOI] [PubMed] [Google Scholar]
- 11.Goral V, Ucmak F, Yildirim S, et al. Malignant melanoma of the stomach presenting in a woman: a case report. J Med Case Rep 2011;5:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ishizaki M, Aibara Y, Furuya K.Primary malignant melanoma of the esophagogastric junction: report of a case. Int J Surg Case Rep 2013;4:700-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dasgupta T, Brasfield R.Metastatic melanoma. A clinicopathologic study. Cancer 1964;17:1323-39. [DOI] [PubMed] [Google Scholar]
- 14.Shenoy S, Cassim R.Metastatic melanoma to the gastrointestinal tract: role of surgery as palliative treatment. W V Med J 2013;109:30-3. [PubMed] [Google Scholar]
- 15.Allaparthi S, Alkimawi KA. Unsteady gait: an uncommon presentation and course of malignant melanoma in terminal ileum-a case report and review of literature. Case Rep Gastrointest Med 2013;2013:958041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suganuma T, Fujisaki J, Hirasawa T, et al. Primary amelanotic malignant melanoma of the small intestine diagnosed by esophagogastroduodenoscopy before surgical resection. Clin J Gastroenterol 2013;6:211-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Houissa F, Bouzaidi S, Mouelhi L, et al. Diffuse primary malignant melanoma of the upper gastrointestinal tract. Gastroenterol Clin Biol 2010;34:85-7. [DOI] [PubMed] [Google Scholar]
- 18.Kotteas EA, Adamopoulos A, Drogitis PD, et al. Gastrointestinal bleeding as initial presentation of melanoma of unknown primary origin: report of a case and review of the literature. In Vivo 2009;23:487-9. [PubMed] [Google Scholar]
- 19.Kranzfelder M, Seidl S, Dobritz M, Brucher BL. Amelanotic esophageal malignant melanoma: case report and short review of the literature. Case Rep Gastroenterol 2008;2:224-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kenney B, Dotto J, Homer R, et al. Primary malignant melanoma of the transverse colon: report of a case and review of the literature. Int J Surg Pathol 2007;15:401-7. [DOI] [PubMed] [Google Scholar]
- 21.Krausz MM, Ariel I, Behar AJ. Primary malignant melanoma of the small intestine and the APUD cell concept. J Surg Oncol 1978;10:283-8. [DOI] [PubMed] [Google Scholar]
- 22.Horowitz M, Nobrega MM. Primary anal melanoma associated with melanosis of the upper gastrointestinal tract. Endoscopy 1998;30:662-5. [DOI] [PubMed] [Google Scholar]
- 23.Ghadially FN, Walley VM. Melanoses of the gastrointestinal tract. Histopathology 1994;25:197-207. [DOI] [PubMed] [Google Scholar]
- 24.Ohashi K, Kato Y, Kanno J, Kasuga T.Melanocytes and melanosis of the oesophagus in Japanese subjects-analysis of factors effecting their increase. Virchows Arch A Pathol Anat Histopathol 1990;417:137-43. [DOI] [PubMed] [Google Scholar]
- 25.Tas F. Metastatic behavior in melanoma: timing, pattern, survival, and influencing factors. J Oncol 2012;2012:647684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sachs DL, Lowe L, Chang AE, et al. Do primary small intestinal melanomas exist? Report of a case. J Am Acad Dermatol 1999;41:1042-4. [DOI] [PubMed] [Google Scholar]
- 27.Balch CM, Gershenwald JE, Soong SJ, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol 2009;27:6199-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smalley KS, McArthur GA. The current state of targeted therapy in melanoma: this time it’s personal. Sem Oncol 2012;39:204-14. [DOI] [PMC free article] [PubMed] [Google Scholar]


