Abstract
Background
The most definitive diagnosis of neck pain caused by facet joints can be obtained through cervical medial branch blocks (CMBBs). However, intravascular injections need to be carefully monitored, as they can increase the risk of false-negative blocks when diagnosing cervical facet joint syndrome. In addition, intravascular injections can cause neurologic deficits such as spinal infarction or cerebral infarction. Digital subtraction angiography (DSA) is a radiological technique that can be used to clearly visualize the blood vessels from surrounding bones or dense soft tissues. The purpose of this study was to compare the rate of detection of intravascular injections during CMBBs using DSA and static images obtained through conventional fluoroscopy.
Methods
Seventy-two patients were included, and a total of 178 CMBBs were performed. The respective incidences of intravascular injections during CMBBs using DSA and static images from conventional fluoroscopy were measured.
Results
A total of 178 CMBBs were performed on 72 patients. All cases of intravascular injections evidenced by the static images were detected by the DSAs. The detection rate of intravascular injections was higher from DSA images than from static images (10.7% vs. 1.7%, P < 0.001).
Conclusions
According to these findings, the use of DSA can improve the detection rate of intravascular injections during CMBBs. The use of DSA may therefore lead to an increase in the diagnostic and therapeutic value of CMBBs. In addition, it can decrease the incidence of potential side effects during CMBBs.
Keywords: Complications, Digital subtraction angiography, Fluoroscopy, Medial branch, Neck pain, Spine, Zygapophyseal joint
INTRODUCTION
Cervical facet joints represent a clinically important source of acute and chronic axial neck pain. They are reported to be responsible for 25-65% of axial neck pain cases [1], and can also occasionally cause pain in other areas, including the head, the upper back, and the shoulder areas. However, imaging studies including x-rays, CTs, and MRIs provide little additional information to facilitate the detection of facet joint problems as the cause of neck pain. Good medical history-taking and physical examination by a trained physician will normally clinch the diagnosis. However, the validity of physical examinations for diagnosing the specific causes of neck pain has been questioned. Therefore, the most definitive diagnosis for neck pain caused by facet joints can be obtained by blocking the cervical medial branch that innervates the specific facet joint [2,3]. Cervical medial branch blocks are considered to be accurate, easy to perform, and reliable. However, there are potential risks associated with the blocks. These include infections, bleeding, puncture of the dura mater, allergic responses to injected agents, vasovagal syncope, and intravascular injections [4,5]. Although the risk is low, intravascular injections should be carefully monitored as they can increase the risk of false-negative blocks when diagnosing cervical facet joint syndrome [6]. In addition, the intravascular injection of particulate steroids can cause fatal neurologic deficits, such as spinal infarction or cerebral infarction [7,8,9,10]. The incidence of inadvertent intravascular injections during cervical medial branch blocks (CMBBs) using static images was reported to be 3.9% [5]. However, according to a study by Smuck et al. [11], in comparison with real-time fluoroscopy, interpretations from static images obtained through conventional fluoroscopy missed 57% of the cases of intravascular injections during cervical and lumbar transforaminal epidural blocks. It has also been found that the detection rate of intravascular injections during transforaminal epidural blocks obtained from digital subtraction angiography (DSA) was significantly higher than that obtained from real-time fluoroscopy [12,13].
Therefore, in this study we compared the detection rate of intravascular injections during CMBBs using DSA and static images obtained through conventional fluoroscopy.
MATERIALS AND METHODS
Having obtained approval from the Institutional Review Board and the written informed consent of the participants, we prospectively examined 72 patients scheduled to receive CMBBs. The incidence of intravascular injection during CMBBs can be influenced by patient factors and/or by practitioner factors [12]. For a better study design, two pain physicians with more than 5 years' experience of interventional treatment for spine pain were therefore involved in this study. All the CMBBs were performed by the same physician and were simultaneously observed by the second physician. The inclusion criteria for this study were as follows: patients over 18 years of age, with a history of chronic neck pain for at least 3 months, and with no history of surgical procedures on the cervical spine. The exclusion criteria included pregnancy, allergy to contrast media, the experience of disc-related pain with radicular symptoms, and persistent contraindications to nerve blocks, such as coagulopathy and infections of the injection site. The patients did not receive any sedation, and were made to lie on their side with the painful side facing up. Using a c-arm, the silhouettes of the articular pillars for both sides of a target segment were superimposed in order to obtain a true lateral view of the cervical spine (Ziehm vision, ziehm imaging, Nuremberg, Germany). In the lateral fluoroscopic view, a 25-gauge, Quinke-type needle (Taechang Industrial Co, Kongju, Korea) was inserted to the center of the articular pillar by lateral approach for C3-6 CMBBs. However, for C7 CMBBs, the needle tip was positioned more superiorly, as the C7 medial branch lies high on the apex of the articular process of C7, due to the transverse process. The needle was advanced until the tip reached the articular pillar.
After the ideal needle tip position was confirmed, 0.6 ml of contrast media (Omnipaque 300, GE Healthcare, Little Chalfont, Buckinghamshire, UK) was injected at a rate of 0.1 ml/s. The static image was taken after 0.3 ml of contrast media had been injected, and DSA was used as the rest of the contrast media was being administered. When contrast intravascular injection was detected, the needle was repositioned.
The data collected for each patient in this study included their age, weight, height, gender, level of injection, and incidence of intravascular injection. The data was analyzed with a McNemar test, using SAS software version 9.1 (Cary, NC). A P value under 0.05 was considered statistically significant.
RESULTS
A total of 178 CMBBs were performed on 72 patients. There were no complications associated with the CMBBs. The characteristics of the study participants are presented in Table 1. The incidence of intravascular injection at each level is presented in Table 2. The detection rate of intravascular injections was higher from the DSA images than from the static images (10.7% vs. 1.7%, P <0.01). All cases of intravascular injection evidenced by the static images were also detected by the DSAs (Fig. 1).
Table 1. Demographic Data (n = 72).
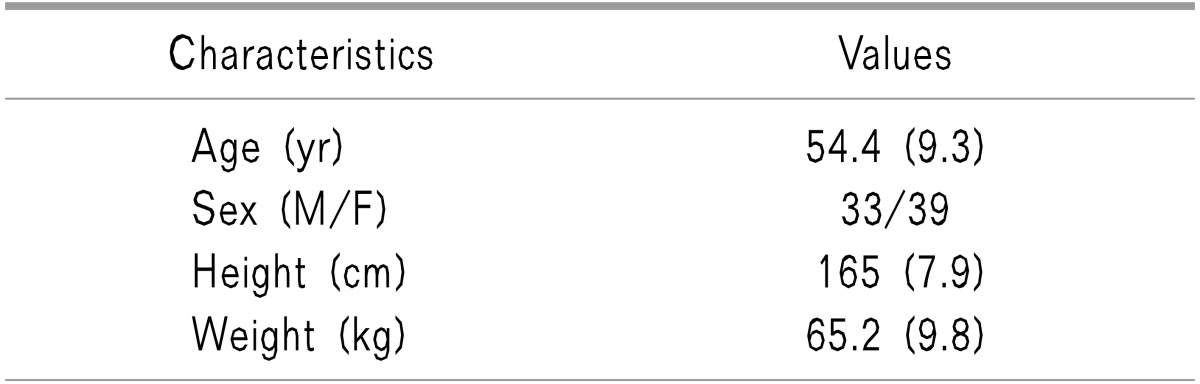
Values are expressed as means (SD) or numbers.
Table 2. Detection Rate of Intravascular Injections at Different Levels of the Cervical Spine.
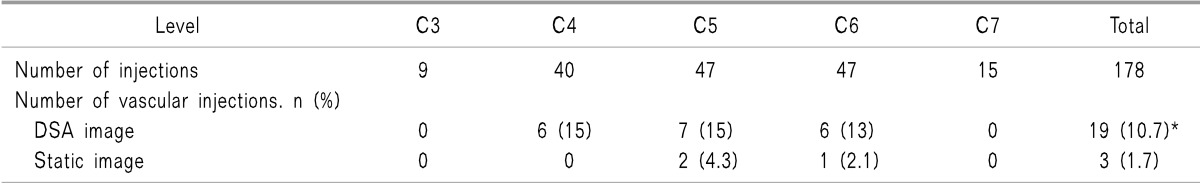
DSA: digital subtraction angiography. *P < 0.001 vs. static image.
Fig. 1. Comparison of contrast flow with static image and digital subtraction angiography (DSA). (A) Contrast flow using static images. (B) Contrast flow using DSA.
DISCUSSION
This study demonstrated that the detection rate of intravascular injections during CMBBs was significantly improved with DSA, as compared to that from static images obtained through conventional fluoroscopy.
DSA is a radiological technique that can be used to clearly visualize the blood vessels from surrounding bones or compact tissues by subtracting the pre-contrast image from the image after injecting the contrast [14,15]. In a previous report, the incidence of inadvertent intravascular injection during CMBBs using static images was 3.9% [5]. However, Smuck et al. [11] reported that in comparison to live fluoroscopy, the accuracy of static conventional fluoroscopy for the detection of intravascular injections during transforaminal epidural blocks was significantly lower.
In the present study, the incidence of intravascular injections when interpreting from static images was 1.7% (3/178), which was significantly lower than the 10.7 % incidence (19/178) from DSA images. We presume that it is difficult to detect contrast medium in the blood vessels on a spot image, due to the rapid wash-out of the injected contrast medium with the blood flow. Therefore, another study is needed to compare live fluoroscopy with DSA for detecting the incidence of intravascular injections during CMBBs.
The posterior venous or arterial plexus around the posterior cervical spine are very complicated. Therefore, intravascular injections can reduce the diagnostic and therapeutic value of CMBBs. In addition, the intra-arterial administration of particulate steroids can cause fatal neurologic problems [8]. In previous studies, despite using real-time fluoroscopy and/or DSA, it has sometimes been impossible to describe the vascular contrast pattern during cervical epidural transforaminal injections as venous or arterial, as the patterns were ambiguous [12]. In the present study, we were also unable to differentiate between the two types of vascular uptake. In addition, there were no side effects associated with the CMBBs.
Several methods have been proposed by previous studies to reduce the risk of intravascular injections of steroids during transforaminal epidural injections. These methods have included using short-beveled or blunt-type needles, using large-diameter needles, using non-particulate steroids, using test dosing with a local anesthetic to determine the incidence of intravascular injection, the slow injection of corticoids with frequent heme-negative aspiration, and using imaging modalities such as real-time fluoroscopy or digital subtraction angiography (DSA) [10].
In conclusion, these findings indicate that the use of DSA can improve the detection rate of intravascular injections during CMBBs. Therefore, the use of DSA may lead to an increase in the diagnostic and therapeutic value of CMBBs. In addition, it can decrease the incidence of potential side effects during CMBBs.
References
- 1.Aprill C, Bogduk N. The prevalence of cervical zygapophyseal joint pain. A first approximation. Spine (Phila Pa 1976) 1992;17:744–747. doi: 10.1097/00007632-199207000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Falco FJ, Erhart S, Wargo BW, Bryce DA, Atluri S, Datta S, et al. Systematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventions. Pain Physician. 2009;12:323–344. [PubMed] [Google Scholar]
- 3.Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009;12:699–802. [PubMed] [Google Scholar]
- 4.Rathmell JP, Lake T, Ramundo MB. Infectious risks of chronic pain treatments: injection therapy, surgical implants, and intradiscal techniques. Reg Anesth Pain Med. 2006;31:346–352. doi: 10.1016/j.rapm.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Verrills P, Mitchell B, Vivian D, Nowesenitz G, Lovell B, Sinclair C. The incidence of intravascular penetration in medial branch blocks: cervical, thoracic, and lumbar spines. Spine (Phila Pa 1976) 2008;33:E174–E177. doi: 10.1097/BRS.0b013e318166f03d. [DOI] [PubMed] [Google Scholar]
- 6.Boswell MV, Trescot AM, Datta S, Schultz DM, Hansen HC, Abdi S, et al. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007;10:7–111. [PubMed] [Google Scholar]
- 7.Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001;91:397–399. doi: 10.1016/S0304-3959(00)00437-1. [DOI] [PubMed] [Google Scholar]
- 8.Heckmann JG, Maihöfner C, Lanz S, Rauch C, Neundörfer B. Transient tetraplegia after cervical facet joint injection for chronic neck pain administered without imaging guidance. Clin Neurol Neurosurg. 2006;108:709–711. doi: 10.1016/j.clineuro.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Karasek M, Bogduk N. Temporary neurologic deficit after cervical transforaminal injection of local anesthetic. Pain Med. 2004;5:202–205. doi: 10.1111/j.1526-4637.2004.04028.x. [DOI] [PubMed] [Google Scholar]
- 10.Tiso RL, Cutler T, Catania JA, Whalen K. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J. 2004;4:468–474. doi: 10.1016/j.spinee.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Smuck M, Fuller BJ, Chiodo A, Benny B, Singaracharlu B, Tong H, et al. Accuracy of intermittent fluoroscopy to detect intravascular injection during transforaminal epidural injections. Spine (Phila Pa 1976) 2008;33:E205–E210. doi: 10.1097/BRS.0b013e31816960fe. [DOI] [PubMed] [Google Scholar]
- 12.McLean JP, Sigler JD, Plastaras CT, Garvan CW, Rittenberg JD. The rate of detection of intravascular injection in cervical transforaminal epidural steroid injections with and without digital subtraction angiography. PM R. 2009;1:636–642. doi: 10.1016/j.pmrj.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 13.Lee MH, Yang KS, Kim YH, Jung HD, Lim SJ, Moon DE. Accuracy of live fluoroscopy to detect intravascular injection during lumbar transforaminal epidural injections. Korean J Pain. 2010;23:18–23. doi: 10.3344/kjp.2010.23.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jasper JF. Role of digital subtraction fluoroscopic imaging in detecting intravascular injections. Pain Physician. 2003;6:369–372. [PubMed] [Google Scholar]
- 15.Sehgal N, Dunbar EE, Shah RV, Colson J. Systematic review of diagnostic utility of facet (zygapophysial) joint injections in chronic spinal pain: an update. Pain Physician. 2007;10:213–228. [PubMed] [Google Scholar]



