Abstract
Background
Pain is one of the most important consequences of spinal cord injury (SCI). It may affect several aspects of life, especially the quality of life (QoL). Hence, this study was conducted to establish an understanding of pain and its correlates and effects on patients with SCI in our community.
Methods
In a cross-sectional study, 58 male veterans suffering from SCI were admitted to our center for a regular follow-up. Demographic and SCI-related descriptive information were gathered using a self-reported questionnaire. To evaluate the patients' pain quality and the effect of pain on daily life, a questionnaire in 3 parts of lumbar, cervical and shoulder pain was administered. EuroQoL questionnaire and General Health Questionnaire (GHQ) 12 were also used to assess the patients' QoL.
Results
The mean age of the participants was 45.91 ± 6.69 with mean injury time of 25.54 ± 5.91. forty-four patients (75.9%) reported pain, including lumbar pain (63%), cervical pain (39%) and shoulder pain (51%). The presence of pain was associated with lower QoL. Patients with lumbar pain reported a significant amount of pain affecting their daily life and this effect was higher in patients with lower GHQ score or anxiety/depressive disorder.
Conclusions
Musculoskeletal pain, is a common complaint in veterans with SCI and is inversely associated with functioning and general health status. Lumbar and shoulder pain affects patient's daily living more than cervical pain.
Keywords: Anxiety, Back pain, Depressive disorder, Musculoskeletal pain, Neck pain, Quality of life, Questionnaires, Shoulder pain, Spinal cord injury
INTRODUCTION
Chronic pain is a common complaint among patients with spinal cord injury (SCI) [1,2,3,4,5]. It affects several aspects of their life, mostly the quality of life (QoL) [6,7]. Therefore, it has received increasing attention among researchers within the last several years.
Recent studies have attempted to define or categorize various types of pain following SCI, which have led to significant advances in understanding and managing pain [2,8,9,10,11]. Most classifications were based on the source or site of pathology, etiology, mechanism and the severity of pain. However, the quality of pain and the location of pain have also been considered. Among different methods of SCI pain classification, the preferred one categorizes pain into 4 major divisions: musculoskeletal (nociceptive), visceral, neuropathic (at-level and below-level) and other types of pain not meeting the criteria of any group [10]. Among these, nociceptive pain refers to the pain that arises from musculoskeletal structures and is assumed to be present at any region where there is some preserved sensation above, at or below the spinal lesion [10]. According to the nature of this type of pain, it is believed it can be effectively managed by traditional therapies, compared to the other types of SCI pain [12,13]. Besides, in patients with SCI, it seems that the lumbar, cervical and shoulder are the most common sites of musculoskeletal pain, and their effect on patients' daily living is clear.
Previous studies have evaluated the predictors of pain and the impact of pain on the QoL of patients with SCI, which have resulted in the belief that pain is one of the most significant consequences of SCI, causing inability in both fields of physical and psychological functioning [7,14,15]. However, there is not much known about the characteristics and correlates of musculoskeletal pain in patients with SCI.
This study aimed to evaluate lumbar, cervical and shoulder pain (the most disabling types of musculoskeletal pain), their correlates and their effects on patients' day-to-day life in a population of war veterans with SCI, in order to help designing more effective programs for the rehabilitation of these patients.
MATERIALS AND METHODS
A cross-sectional study was performed at Khatam-Al-Anbia hospital during May and August 2011, including male veterans suffering from spinal cord injury admitted to our center for regular follow-up. Data was gathered using a self-reported questionnaire distributed to the participants. Each questionnaire was accompanied with an introductory statement explaining the purpose of the study and the patient's privacy. This information served as the informed consent statement, as required by the Institutional Ethics Committee.
A general questionnaire was developed consisting of three parts of patients' basic information, QoL and pain related questions. A number of questions were designed to assess the patients' demographic and SCI related information such as age, years since injury, age at SCI, weight, height, body mass index (BMI), educational level, cause of injury and level of injury. Patients' weight was measured using a wheelchair balance scale by subtracting the wheelchair weight from the patient and wheelchair total weight, and for abled patients by standing on the same scale. Height was measured using a wall mounted stadiometer for patients able to stand erect and by a supine stadiometer for those unable to stand. BMI was calculated using the [weight / (height)*2] formula. The level of injury and the presence of pressure ulcer were confirmed by a neurosurgeon.
To evaluate the patients' QoL and subjective quantitative health status, EuroQoL [16] was used, consisting of EuroQoL 5-Dimensions 3-levels (EQ-5D-3L) and EuroQoL Visual Analogue Scale (EQ-VAS) in 5 dimensions of mobility, self-care, usual activity, pain/discomfort and anxiety/depression. General Health Questionnaire (GHQ) 12 [17] was applied to assess the patients' self-reported health status during the last several weeks as well. Using the conventional scoring for GHQ, the method of (0-0-1-1) with the max score of 12 was used to estimate the patients' mental health problems; so the higher the score, the greater the severity of the problem. The survey also included a number of questions covering sleep disorders, underlying diseases (UD) and lifestyle, including exercise and smoking habits.
The questionnaire contained questions of pain itself in three regions of lumbar, cervical and shoulder pain. Each part was designed to assess the quality of pain, severity of pain and the influence of pain on daily life consisting of activities such as shopping, self-care and usual house work, working abilities and participating in social activities. Pain severity included 3 questions about the pain at the time of admission, the most severe pain experienced by the patient during the last 6 months and mean pain severity during the last 6 months. Answers for pain severity and the influence of pain on daily life were in the range of 0-10 (0 the min and 10 the max) reported by the responders. The patients were also asked to report the number of days that pain had influenced their daily activities, such as personal and routine activities, during the last 6 months.
SPSS software version 16.00 (SPSS Inc., Chicago, IL) was applied for statistical analysis. To compare quantitative values, student's t test or correlate binary test and to compare the proportions the chi-square test or Fisher's exact test were used. Level of statistical significance was set as P < 0.05.
RESULTS
During the study, a total of 134 patients with SCI were admitted to Khatam-Al-Anbia hospital. However 62 patients were either not able or not willing to participate in the study which led to the response rate of 53.74%. Furthermore, a total of 14 patients refused to answer the musculoskeletal part or partially completed the questionnaire remaining 58 responders for final assessment. The demographic and SCI-related descriptive information of the 58 participants and their association with the presence of pain are presented in Table 1 regarding the pain site. The results showed that patients with cervical pain were significantly much more obese than patients without cervical pain. Additionally, patients with lumbar pain were more likely to be injured by missiles, metal shrapnel fragment and blast injury compared to the patients without lumbar pain, among whom motor vehicle accidents and falling were the most likely causes of injury in these patients.
Table 1. The Demographic and SCI-related Descriptive Information of the Patients and Their Association with the Presence of Pain Regarding the Pain Site.
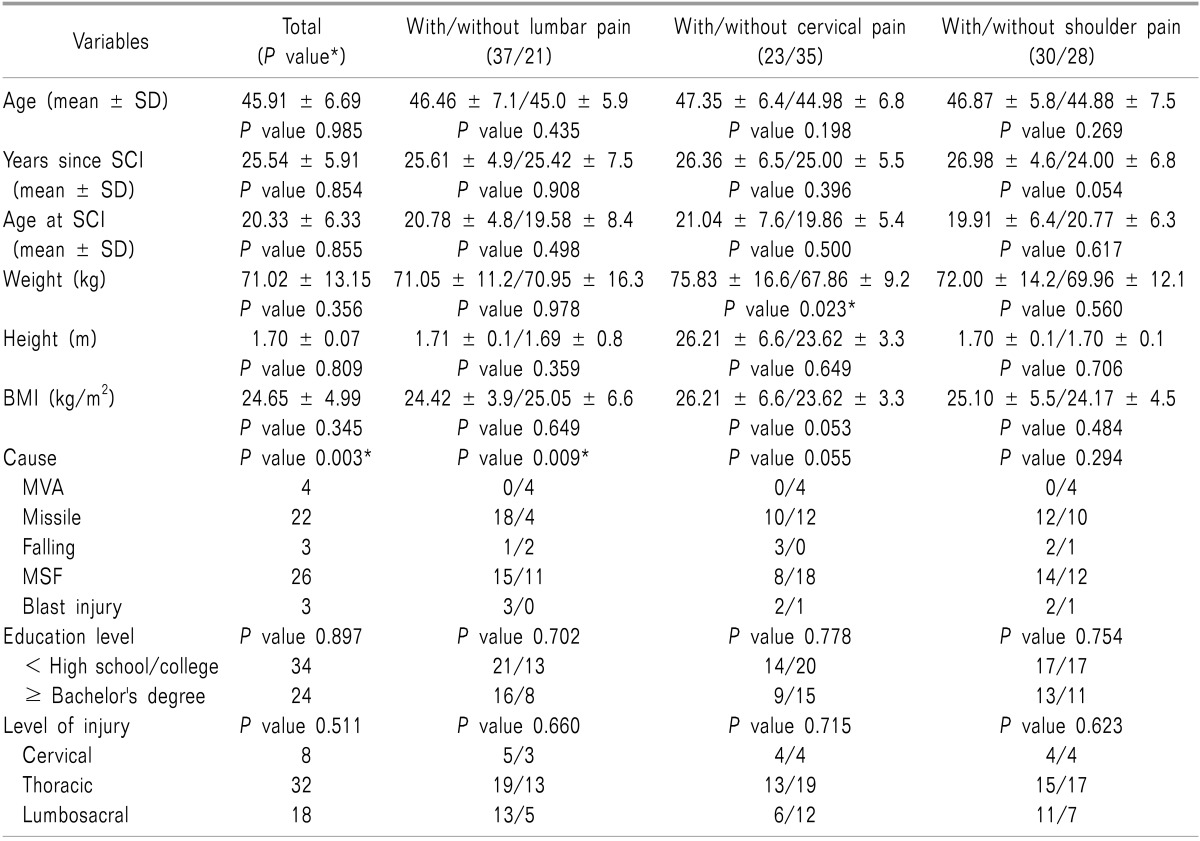
*P value for groups of with and without pain in any region. MSF: metal shrapnel fragment, MVA: motor vehicle accident.
Patients' mean age was 45.91 ± 6.69 years (20-66 years) and the mean injury time was 25.54 ± 5.91 years (1-47 years). A total of 44 patients (75.9%) reported pain in at least one region including lumbar, cervical or shoulder pain; however, 14 patients (24.1%) had no complaints of pain. The prevalence of lumbar, cervical and shoulder pain was respectively 63.8% (37 patients), 39.7% (23 patients) and 51.7% (30 patients).
The association between factors related to QoL including EQoL parameters, GHQ score, UD and exercise and smoking habits with the presence of pain in each region individually are presented in Table 2. The results defined that patients with overall pain reported more discomfort compared to those without pain. This was clear for patients with lumbar and cervical pain. Furthermore, the smoking rate was significantly higher in patients with cervical pain compared to those without cervical pain.
Table 2. The Association between Variables Related to Quality of Life with the Presence of Pain Regarding the Pain Site (*P < 0.05).
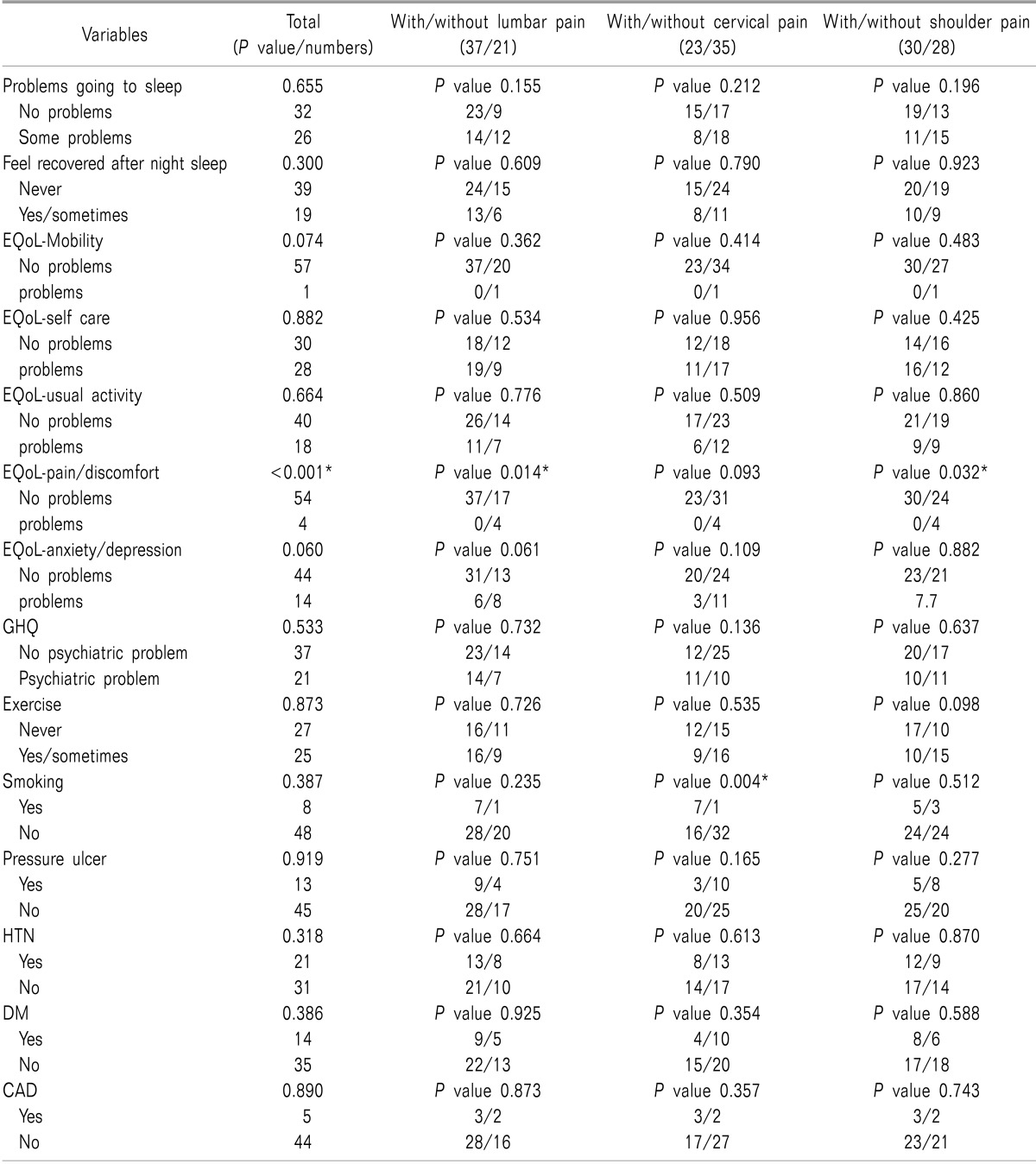
CAD: coronary artery disease, DM: diabetes mellitus, EuroQoL: euro quality of life, GHQ: general health questionnaire, HTN: hypertension.
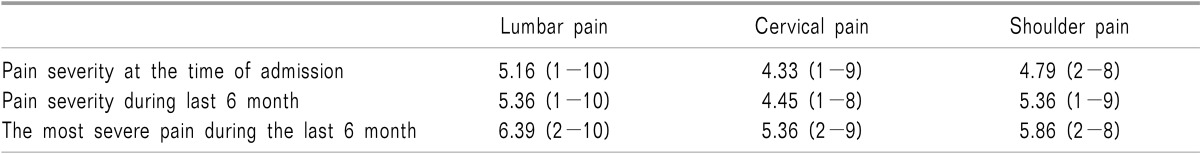
At the time of admission, the most severe pain experienced by a patient during the last 6 months and the mean pain severity in the last 6 months are shown in Table 3. Report of pain severity at the time of admission was higher among the patients with lumbar pain compared to the patients with cervical and shoulder pain. The mean days of pain influencing patients daily activities during the last 6 months was 10 (0-180) days for lumbar pain, 17 (0-90) days for cervical pain and 17.5 (0-90) days for shoulder pain.
Table 3. Patients' Report of the Severity of Pain at the Time of Admission, the Most Severe Pain Experienced by the Patient during the Last 6 Months and the Mean Pain Severity in the Last 6 Months Regarding the Pain Site (Mean, Minimum and Maximum).
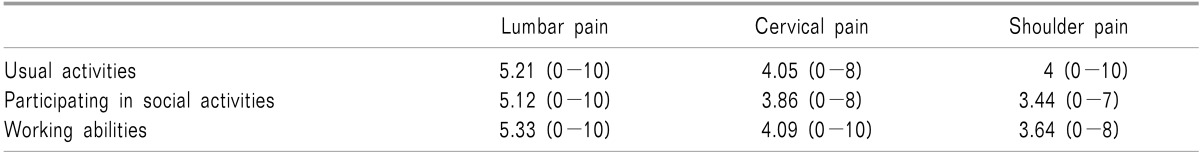
Patients' report of the influence of pain on daily activities, participating in social activities and working abilities is presented in Table 4 regarding the pain site. The overall influence of pain in daily life was higher in patients with lumbar pain.
Table 4. Patients' Report of the Influence of Pain in Daily Activities, Participating in Social Activities and Working Abilities Regarding the Pain Site (Mean, Minimum and Maximum).
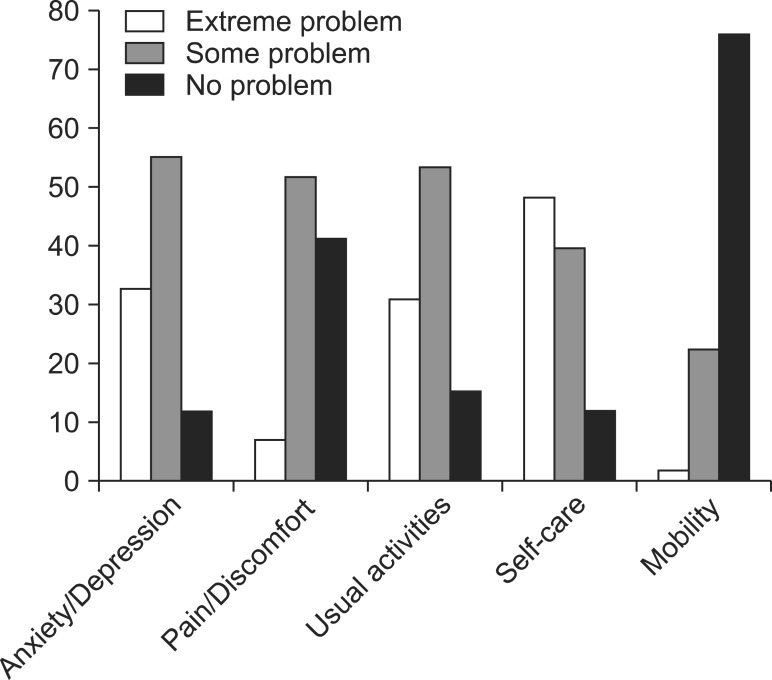
The demographics of the patients' QoL are presented in Fig. 1. A total of 37 patients had general health problems. The highest and the lowest rate of extreme problems reported by the patients were in the fields of mobility (75.9%) and self-care (12.1%).
Fig. 1. The demographics of the patients' quality of life assessed by EuroQoL questionnaire. EuroQoL: Euro Quality of Life.
We selected the patients with lumbar, cervical and shoulder pain each time separately to assess the association between predictive factors with the patients' report of the influence of pain on 3 parts of daily life in each group. The results are presented in Table 5. Lower educational level and lower GHQ score in patients with lumbar pain and higher BMI, presence of self-care problems and anxiety/depressive disorder in patients with shoulder pain were associated with a greater influence of pain on patients' daily living.
Table 5. The Association between Predictive Factors with the Patients' Report of the Influence of Pain in 3 Fields of Day Life Including Usual Activities (Field 1), Participating in Social Activities (Field 2), and Working Abilities (Field 3), in Each Group of Pain Individually (P values are Presented; *P < 0.05).
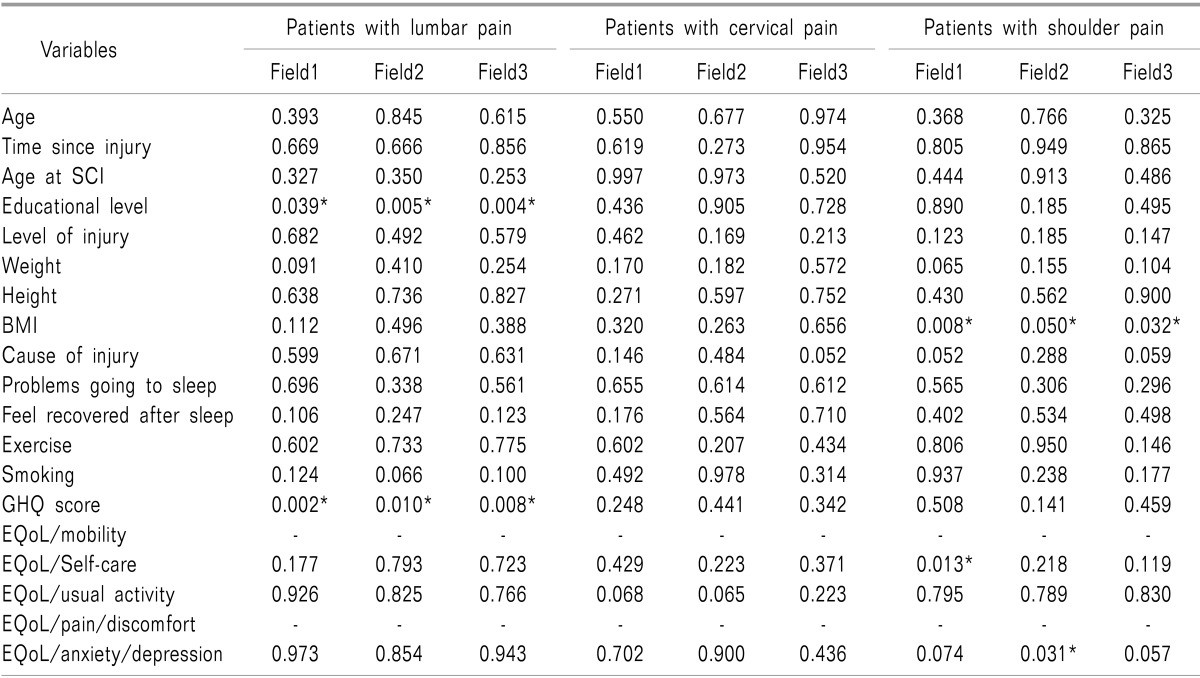
BMI: body mass index, EuroQoL: euro quality of life, GHQ: general health questionnaire, SCI: spinal cord injury.
DISCUSSION
Pain is a major problem among patients with SCI, imposing several limitations to the patients. A previous study in England reported that 11% of patients with SCI consider pain rather than mobility disorder as a deterrent in their daily activities [18]. Another study reported 37% of patients with high level lesions and 23% of patients with low level lesions were willing to exchange loss of reacquired physiologic functions for pain relief [19]. Hence, it is important to look for possible predictors of pain and try to reduce them in patients with SCI. This study was performed to evaluate the prevalence of pain and its correlates in a population of war veterans with SCI and to assess the impact of pain in patients' daily life.
In our study, 75.9% of patients with SCI reported pain in at least one region including lumbar, cervical or shoulder pain and the prevalence of lumbar pain (63%) was higher compared to shoulder pain (51%) and cervical pain (39%). The reports of the prevalence of pain in patients with SCI were different in previous studies. The condensation of 10 studies during last decade, showed that pain was present in 69% of patients with SCI and almost one third of patients reported severe pain, which was consistent with two other studies that had reported pain in 66% of patients with SCI [20,21]. In a longitudinal study, the prevalence of pain, 6 months after the injury was 64% and 12 months after patients' discharge from hospital was 63% [22]. However, other studies have reported pain in 34% to 90% of patients with SCI and the prevalence of severe pain was in a range of 12% to 30% in different studies [23,24].
Despite the high prevalence of pain in patients with SCI, there is not a clear understanding of its predictive factors. The association between age and the presence of pain is controversial in previous findings [3,25]. The results of our study showed that there is not a significant association between age and pain. Besides, our results were consistent with previous findings that had reported no association between injury duration and age at SCI with the presence of pain [26,27]. Factors such as level of injury and cause of injury have been considered as predictive factors of pain in previous findings [4,21,28]. The results of our study showed that there is a significant association between cause of injury and the presence of pain, mostly lumbar pain; however, no association was found between the level of injury and pain.
Previous studies have shown the negative impact of pain on the QoL of patients with SCI [7,14,15,29]. Chronic pain is also reported to be associated with anxiety/depressive disorder [26]. The results of our study showed that pain, especially lumbar and shoulder pain, are accompanied by feelings of discomfort in patients with SCI. Sleep is another major problem in patients with SCI [30]. Despite a previous study that has reported pain as a primary reason for poor quality of sleep [31], we did not find any association between pain and sleep disorders. This difference may be because of other factors affecting patients' sleep quality. Patients with SCI and chronic pain are supposed to have increased risk of coronary artery disease (CAD), diabetes mellitus (DM), hypertension (HTN) and pressure ulcer due to their low activity lifestyle. However, in our study there was not a significant association between these factors and the presence of pain in any region. Smoking and obesity are also considered as accompanying factors of pain in general population [32,33]. In our study, obesity and smoking were associated with the presence of cervical pain. Other factors related to QoL were not significantly different between patients with and without pain.
Previous studies reported frequent interference of pain with daily activities in patients with SCI [34,35,36]. The interference was even present in a number of important basic activities of daily living [37]. In our study, patients with lumbar pain reported a greater effect of pain on 3 fields of daily life, including usual activities, working abilities and participating in social activities, rather that patients with cervical and shoulder pain. The results showed that in patients with lumbar pain, educational level and GHQ score were associated with the interference of pain with daily activities. In patients with shoulder pain, high BMI was directly associated with a greater influence of pain on daily activities; however, in these group, patients with self-care problems reported a greater effect of pain on routine activities and patients with anxiety/depressive disorder had more problems in social activities.
Our study's sample size was quite small and the investigation was restricted to men in order to obtain a homogenous sample. However, we failed to gather complete data in some fields, such as completeness of injury. These factors may impose limits to our results.
In conclusion, the results of our study showed the high prevalence of musculoskeletal pain, notably lumbar pain among patients with SCI. Patients with lumbar and shoulder pain rather than cervical pain suffer from feelings of discomfort and the impact of pain on a patient's daily living is significantly higher than those with lumbar pain. Hence, it is important to set priorities and design effective programs in the management of pain and the improvement of QoL in patients with SCI.
ACKNOWLEDGEMENTS
The authors have no financial support or relationships that may impose a conflict of interest.
References
- 1.de Miguel M, Kraychete DC. Pain in patients with spinal cord injury: a review. Rev Bras Anestesiol. 2009;59:350–357. doi: 10.1590/s0034-70942009000300011. [DOI] [PubMed] [Google Scholar]
- 2.Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249–257. doi: 10.1016/S0304-3959(02)00452-9. [DOI] [PubMed] [Google Scholar]
- 3.Subbarao JV, Klopfstein J, Turpin R. Prevalence and impact of wrist and shoulder pain in patients with spinal cord injury. J Spinal Cord Med. 1995;18:9–13. doi: 10.1080/10790268.1995.11719374. [DOI] [PubMed] [Google Scholar]
- 4.Adriaansen JJ, Post MW, de Groot S, van Asbeck FW, Stolwijk-Swüste JM, Tepper M, et al. Secondary health conditions in persons with spinal cord injury: a longitudinal study from one to five years post-discharge. J Rehabil Med. 2013;45:1016–1022. doi: 10.2340/16501977-1207. [DOI] [PubMed] [Google Scholar]
- 5.Hu Y, Mak JN, Wong YW, Leong JC, Luk KD. Quality of life of traumatic spinal cord injured patients in Hong Kong. J Rehabil Med. 2008;40:126–131. doi: 10.2340/16501977-0150. [DOI] [PubMed] [Google Scholar]
- 6.Wollaars MM, Post MW, van Asbeck FW, Brand N. Spinal cord injury pain: the influence of psychologic factors and impact on quality of life. Clin J Pain. 2007;23:383–391. doi: 10.1097/AJP.0b013e31804463e5. [DOI] [PubMed] [Google Scholar]
- 7.Post M, Noreau L. Quality of life after spinal cord injury. J Neurol Phys Ther. 2005;29:139–146. doi: 10.1097/01.npt.0000282246.08288.67. [DOI] [PubMed] [Google Scholar]
- 8.Putzke JD, Richards JS, Hicken BL, Ness TJ, Kezar L, DeVivo M. Pain classification following spinal cord injury: the utility of verbal descriptors. Spinal Cord. 2002;40:118–127. doi: 10.1038/sj.sc.3101269. [DOI] [PubMed] [Google Scholar]
- 9.Siddall PJ, Taylor DA, Cousins MJ. Classification of pain following spinal cord injury. Spinal Cord. 1997;35:69–75. doi: 10.1038/sj.sc.3100365. [DOI] [PubMed] [Google Scholar]
- 10.Widerström-Noga E, Biering-Sørensen F, Bryce T, Cardenas DD, Finnerup NB, Jensen MP, et al. The international spinal cord injury pain basic data set. Spinal Cord. 2008;46:818–823. doi: 10.1038/sc.2008.64. [DOI] [PubMed] [Google Scholar]
- 11.Richards JS. Chronic pain and spinal cord injury: review and comment. Clin J Pain. 1992;8:119–122. doi: 10.1097/00002508-199206000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Ragnarsson KT. Management of pain in persons with spinal cord injury. J Spinal Cord Med. 1997;20:186–199. [PubMed] [Google Scholar]
- 13.Kim MJ, Hong BH, Zhang EJ, Ko YK, Lee WH. Antinociceptive effects of intraperitoneal and intrathecal vitamin E in the rat formalin test. Korean J Pain. 2012;25:238–244. doi: 10.3344/kjp.2012.25.4.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Budh CN, Osteråker AL. Life satisfaction in individuals with a spinal cord injury and pain. Clin Rehabil. 2007;21:89–96. doi: 10.1177/0269215506070313. [DOI] [PubMed] [Google Scholar]
- 15.Donnelly C, Eng JJ. Pain following spinal cord injury: the impact on community reintegration. Spinal Cord. 2005;43:278–282. doi: 10.1038/sj.sc.3101702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med. 1979;9:139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 18.Rose M, Robinson JE, Ells P, Cole JD. Pain following spinal cord injury: results from a postal survey. Pain. 1988;34:101–102. doi: 10.1016/0304-3959(88)90187-X. [DOI] [PubMed] [Google Scholar]
- 19.Nepomuceno C, Fine PR, Richards JS, Gowens H, Stover SL, Rantanuabol U, et al. Pain in patients with spinal cord injury. Arch Phys Med Rehabil. 1979;60:605–609. [PubMed] [Google Scholar]
- 20.Fenollosa P, Pallares J, Cervera J, Pelegrin F, Inigo V, Giner M, et al. Chronic pain in the spinal cord injured: statistical approach and pharmacological treatment. Paraplegia. 1993;31:722–729. doi: 10.1038/sc.1993.114. [DOI] [PubMed] [Google Scholar]
- 21.Störmer S, Gerner HJ, Grüninger W, Metzmacher K, Föllinger S, Wienke C, et al. Chronic pain/dysaesthesiae in spinal cord injury patients: results of a multicentre study. Spinal Cord. 1997;35:446–455. doi: 10.1038/sj.sc.3100411. [DOI] [PubMed] [Google Scholar]
- 22.Siddall PJ, Taylor DA, McClelland JM, Rutkowski SB, Cousins MJ. Pain report and the relationship of pain to physical factors in the first 6 months following spinal cord injury. Pain. 1999;81:187–197. doi: 10.1016/s0304-3959(99)00023-8. [DOI] [PubMed] [Google Scholar]
- 23.Munro D. Two-year end-results in the total rehabilitation of veterans with spinal-cord and cauda-equina injuries. N Engl J Med. 1950;242:1–16. doi: 10.1056/NEJM195001052420101. [DOI] [PubMed] [Google Scholar]
- 24.New PW, Lim TC, Hill ST, Brown DJ. A survey of pain during rehabilitation after acute spinal cord injury. Spinal Cord. 1997;35:658–663. doi: 10.1038/sj.sc.3100472. [DOI] [PubMed] [Google Scholar]
- 25.Werhagen L, Budh CN, Hultling C, Molander C. Neuropathic pain after traumatic spinal cord injury--relations to gender, spinal level, completeness, and age at the time of injury. Spinal Cord. 2004;42:665–673. doi: 10.1038/sj.sc.3101641. [DOI] [PubMed] [Google Scholar]
- 26.Rintala DH, Loubser PG, Castro J, Hart KA, Fuhrer MJ. Chronic pain in a community-based sample of men with spinal cord injury: prevalence, severity, and relationship with impairment, disability, handicap, and subjective well-being. Arch Phys Med Rehabil. 1998;79:604–614. doi: 10.1016/s0003-9993(98)90032-6. [DOI] [PubMed] [Google Scholar]
- 27.Demirel G, Yllmaz H, Gençosmanoğlu B, Kesiktaş N. Pain following spinal cord injury. Spinal Cord. 1998;36:25–28. doi: 10.1038/sj.sc.3100523. [DOI] [PubMed] [Google Scholar]
- 28.Haisma JA, van der Woude LH, Stam HJ, Bergen MP, Sluis TA, Post MW, et al. Complications following spinal cord injury: occurrence and risk factors in a longitudinal study during and after inpatient rehabilitation. J Rehabil Med. 2007;39:393–398. doi: 10.2340/16501977-0067. [DOI] [PubMed] [Google Scholar]
- 29.Westgren N, Levi R. Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil. 1998;79:1433–1439. doi: 10.1016/s0003-9993(98)90240-4. [DOI] [PubMed] [Google Scholar]
- 30.Norrbrink Budh C, Kowalski J, Lundeberg T. A comprehensive pain management programme comprising educational, cognitive and behavioural interventions for neuropathic pain following spinal cord injury. J Rehabil Med. 2006;38:172–180. doi: 10.1080/16501970500476258. [DOI] [PubMed] [Google Scholar]
- 31.Norrbrink Budh C, Hultling C, Lundeberg T. Quality of sleep in individuals with spinal cord injury: a comparison between patients with and without pain. Spinal Cord. 2005;43:85–95. doi: 10.1038/sj.sc.3101680. [DOI] [PubMed] [Google Scholar]
- 32.Heuch I, Hagen K, Heuch I, Nygaard Ø, Zwart JA. The impact of body mass index on the prevalence of low back pain: the HUNT study. Spine (Phila Pa 1976) 2010;35:764–768. doi: 10.1097/BRS.0b013e3181ba1531. [DOI] [PubMed] [Google Scholar]
- 33.Fernández-de-las-Peñas C, Hernández-Barrera V, Alonso-Blanco C, Palacios-Ceña D, Carrasco-Garrido P, Jiménez-Sánchez S, et al. Prevalence of neck and low back pain in community-dwelling adults in Spain: a population-based national study. Spine (Phila Pa 1976) 2011;36:E213–E219. doi: 10.1097/BRS.0b013e3181d952c2. [DOI] [PubMed] [Google Scholar]
- 34.Mann R, Schaefer C, Sadosky A, Bergstrom F, Baik R, Parsons B, et al. Burden of spinal cord injury-related neuropathic pain in the United States: retrospective chart review and cross-sectional survey. Spinal Cord. 2013;51:564–570. doi: 10.1038/sc.2013.34. [DOI] [PubMed] [Google Scholar]
- 35.Widerström-Noga EG, Felipe-Cuervo E, Yezierski RP. Chronic pain after spinal injury: interference with sleep and daily activities. Arch Phys Med Rehabil. 2001;82:1571–1577. doi: 10.1053/apmr.2001.26068. [DOI] [PubMed] [Google Scholar]
- 36.Valtonen K, Karlsson AK, Alaranta H, Viikari-Juntura E. Work participation among persons with traumatic spinal cord injury and meningomyelocele1. J Rehabil Med. 2006;38:192–200. doi: 10.1080/16501970500522739. [DOI] [PubMed] [Google Scholar]
- 37.Jensen MP, Hoffman AJ, Cardenas DD. Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord. 2005;43:704–712. doi: 10.1038/sj.sc.3101777. [DOI] [PubMed] [Google Scholar]