Abstract
Resistant hypertension (RHTN) is a multifactorial disease characterized by blood pressure (BP) levels above goal (140/90 mmHg) in spite of the concurrent use of three or more antihypertensive drugs of different classes. Moreover, it is well known that RHTN subjects have high prevalence of left ventricular diastolic dysfunction (LVDD), which leads to increased risk of heart failure progression. This review gathers data from studies evaluating the effects of phosphodiesterase-5 (PDE-5) inhibitors (administration of acute sildenafil and short-term tadalafil) on diastolic function, biochemical and hemodynamic parameters in patients with RHTN. Acute study with sildenafil treatment found that inhibition of PDE-5 improved hemodynamic parameters and diastolic relaxation. In addition, short-term study with the use of tadalafil demonstrated improvement of LVDD, cGMP and BNP-32 levels, regardless of BP reduction. No endothelial function changes were observed in the studies. The findings of acute and short-term studies revealed potential therapeutic effects of IPDE-5 drugs on LVDD in RHTN patients.
Keywords: Hypertension, Left Ventricular Dysfunction, Phosphodiesterase 5 Inhibitors / therapeutic use, Heart Failure, Vasodilator Agents / therapeutic use
Introduction
Resistant hypertension (RHTN) is a multifactorial condition characterized by blood pressure (BP) levels above goal (140/90 mmHg) in spite of the concurrent use of three or more antihypertensive drugs of different classes or controlled BP with the use of four or more agents1. The overall prevalence is estimated from 15% to 18% of all hypertensive individuals in population-based studies2,3 and frequently the increasing number of antihypertensive drugs used in the course of disease1,4 is associated with with overweight or obesity and diabetes type 2; however, those conditions are not enough to primarily explain the individuals' physical limitations and cardiovascular complaints. In an echocardiography study, it was observed that 95% of RHTN and 72% of controlled hypertensive subjects had left ventricular diastolic dysfunction (LVDD) with preserved systolic function5.
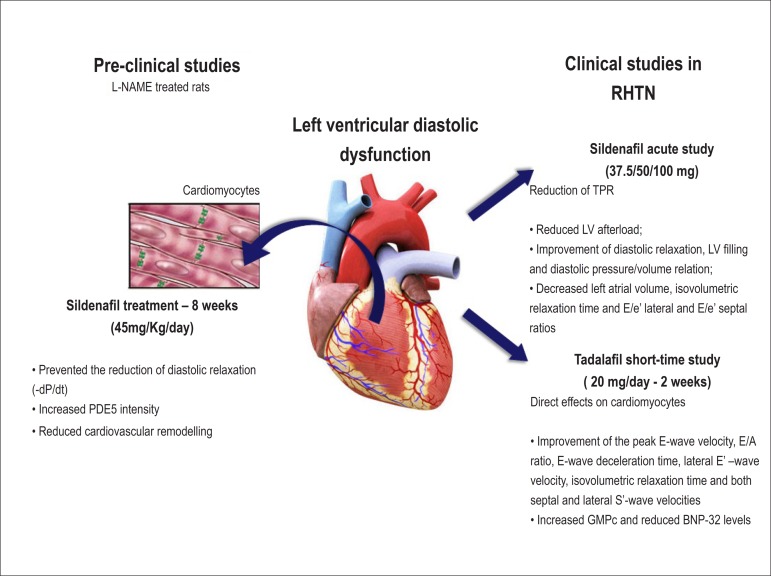
Previous studies have demonstrated that hypertensive rat models produced by chronic treatment with nitric oxide (NO) inhibitor - NG-nitro-L-arginine methyl ester (L-NAME) - showed marked impairment of the first temporal derivative negative pressure of the LV diastolic pressure (-dP/dt, in mmHg/s), indicating LVDD in those animals 6,7. Curiously, this effect was reversed by oral administration of sildenafil, a selective phosphodiesterase type 5 inhibitor (IPDE-5) after 8 weeks of treatment8. Indeed, immunohistochemistry revealed reduced L-NAME-related myocardial lesions, in addition to increased PDE-5 intensity in the intercalary discs between myocytes 9. Hence, this finding was related to improvement in LVDD due to direct sildenafil effect on cardiac relaxation in L-NAME-treated rats.
Therefore, because of the high prevalence of LVDD (95%) observed in our Outpatient Clinic specialized in RHTN (Campinas, Brazil) 5 and the lack of standard treatment, which reduces mortality rates 10, our group recently sought to investigate LVDD condition by echocardiography - a non-invasive diagnostic method frequently used - in association with IPDE-5 in acute (sildenafil) and short-term (tadalafil) administration. Thus, this clinical update report two recently published findings that evaluated the effects of PDE-5 inhibitors on diastolic function in the specific group of resistant hypertensive subjects 11,12.
LVDD TREATMENT in RHTN: primary clinical studies using IPDE-5 drugs
Acute study
The hypothesis for the first recently published study involved a selective IPDE-5 and LVDD in RHTN patients, considering that acutely administered sildenafil could improve hemodynamic parameters, endothelial and left ventricular diastolic functions 11. This crossover, single-blind and placebo-controlled study included 26 subjects diagnosed with RHTN (Clinicaltrial.gov - Protocol ID: CAAE-0758.0.146.000-09). Endothelial function (assessed by flow-mediated dilation method-FMD) and echocardiogram were determined during pre and post-sildenafil treatment, as well as measures of nitrite and plasma cyclic guanosine monophosphate (cGMP) levels. Additionally, non-invasive hemodynamic parameters (Finometer - Finapres Medical Systems; Amsterdam, Netherlands) were evaluated prior to and during the entire period of sildenafil treatment, with increasing dose administration (37.5, 50 and 100 mg) at 30-minute intervals.
No differences were found in nitrite and cGMP levels, as well as in endothelial function after sildenafil use. Conversely, hemodynamic evaluation revealed that sildenafil administration contributed to the decrease in mean blood pressure (MAP) at increasing doses, when compared to baseline levels (84.17±21.04 to 75±17.21 mmHg, p<0.05). Total peripheral resistance (TPR) was markedly reduced after the first dose of 37.5 mg (1149±459.7 to 1037±340 dyn.s/cm-5, p<0.05), but heart rate increased progressively with cumulative doses of this short-acting IPDE-5. Finally, improvement in diastolic function with reduction of: (1) left atrial volume (25.4±1.1 to 20.9±0.9 mL, p<0.05), (2) isovolumetric relaxation time (104.4±3.8 to 88.3±3.0 ms, p<0.05), (3) E/e' lateral and E/e' septal ratios (7.7±0.7 to 6.4±0.6 and 9.8±0.8 to 7.9±0.6, respectively, p<0.05) was found, when compared to pre-sildenafil echocardiogram.
The findings suggested that acute inhibition of PDE-5 improves hemodynamic parameters - reducing MAP levels through TPR reduction - as well as diastolic relaxation, although endothelial function changes were not observed 11 .
Short-term study
In a second recently published study, our group investigated whether tadalafil use, a long-acting IPDE-5 drug, improved LVDD in RHTN patients, regardless of BP reduction12. A total of 19 patients were included in this crossover, single-blind and placebo-controlled study (ClinicalTrials.gov - Protocol ID: CAAE-0044.0.146.000-09). All subjects received oral tadalafil (20 mg/day) for 2 weeks. Endothelial (FMD method) and LV diastolic (echocardiography) functions, nitrite, plasma cGMP and B-type natriuretic peptide (BNP-32) levels were determined at baseline and post-tadalafil treatment.
No changes in endothelial function or nitrite levels were observed. On the other hand, cGMP increased and BNP-32 reduced after the use of tadalafil (62.4±32.2 to 112.6±75.3 pmol/mL and143.3±33.3 to 119.3±31.3 pg/mL, respectively, p<0.05). Echocardiography revealed improvement of the LVDD variables: (1) peak E-wave velocity (67.8±18.3 to 77.8±16.0 cm/s, p<0.05); (2) E/A ratio (0.9±0.3 to 1.08±0.3, p<0.05); (3) E-wave deceleration time (234.1±46.0 to 194.4±43.3 ms, p<0.05); (4) lateral E'-wave velocity (7.7±2.1 to 8.8±2.8 cm/s, p<0.05); (5) isovolumetric relaxation time (128.7±17.6 to 96.8±26.9 ms, p<0.05); and (6) both septal and lateral S'-wave velocities (6.3±1.4 to 7.7±1.7 and 7.5±2.3 to 8.3±2.2 cm/s, respectively, p<0.05) post-tadalafil treatment. Moreover, the study showed reductions in dyspnea, palpitations, and fatigue reported by the patients.
In summary, this short-term study demonstrated clinical relevance with the use of tadalafil for 2 weeks on LVDD treatment and diastolic function-related biomarkers in RHTN subjects, and this effect was independent of BP reduction 12.
Mechanism discussion
The findings of the acute study with increasing doses of sildenafil (37.5, 50 and 100 mg at 30-minute intervals) showed improvement in the hemodynamic profile and LVDD in RHTN patients.
Previously, studies have evaluated the administration of IPDE-5 inhibitor in hypertensive groups. Firstly, it was demonstrated that sildenafil use during 16 days reduced ambulatory BP levels in untreated hypertensive subjects 13. A second study has demonstrated BP reduction with acute sildenafil administration in a single dose (50 mg) in RHTN 14. This study also found that the combination of sildenafil and organic nitrate (isosorbide mononitrate) was well tolerated and resulted in a greater decrease in brachial and central BP levels, raising the idea that this new therapeutic approach might be effective to RHTN patients. Despite these important findings, the mechanism of BP reduction was not reported.
The proposal to investigate hemodynamic parameters continuously contributed to detect that BP reduction was due to TPR reduction, since cardiac output remained unaltered. Curiously, the marked decrease in MAP levels and TPR occurred after the first sildenafil dose (37.5 mg), which was not sustained with consecutive administration of increasing doses (50 mg and 100 mg). In accordance with previous studies 15,16, those findings indicated that sildenafil did not have a dose-dependent effect 11.
The proposed causal mechanism for LVDD improvement in the acute study was also due to TPR reduction 11. Taken together, those findings suggest that LVDD is characterized by increased afterload - resulting from increased TPR - with myocardial relaxation impairment of the left ventricle. Hence, it contributes to resistance in ventricular filling and alterations of diastolic pressure/volume ratio17,18 (figure 1).
Figure 1.
Potential mechanisms for the improvement of left ventricular diastolic dysfunction in preclinical and clinical studies.
The short-term study assessed the effects of long-acting IPDE-5 (tadalafil 20 mg/day for 2 weeks) and resulted in LVDD improvement, regardless of BP reduction, and in cGMP and BNP-32 alterations after drug use in RHTN subjects. However, no nitrite and endothelial function changes were observed 12. Those findings reinforced the hypothesis of the direct tadalafil effects on cardiomyocytes, as we could exclude the potential influence of NO-mediated vasodilation, and consequently, reduction of ventricular afterload (TPR was not altered).
Previous studies have demonstrated that PDE-5, through cGMP signaling pathway, leads to adverse cardiac remodeling 19-22 and its inhibition - with increased levels of cGMP - results in positive effects, such as the blocking of adrenergic, hypertrophic and apoptotic signaling pathways 23. In accordance with these clinical findings, a study demonstrated the increase in plasma cGMP levels and left ventricular diastolic and systolic capacitance and decrease in measurements of cardiomyocyte passive stiffness during serial treatment with sildenafil and with BNP 24. The PDE-5 enzyme was found in the intercalary discs between myocytes and IPDE-5 may have a potential relevance for diastolic relaxation by preventing the L-NAME-induced impairment in -dP/dt measurement. Thus, attenuation of deleterious hemodynamic and morphological alterations observed with L-NAME treatment might be modulated by PDE5 inhibition in cardiac myocytes 9. In addition, IPDE-5 treatment may reduce cardiac inflammation followed by an improved remodeling process, as well as cardiac apoptosis, resulting in improved LV function in experimental models of angiotensin II-induced heart failure 25. These mechanisms highlight the importance of PDE-5 as a strategic pharmacological target for cardiomyocytes relaxation and, consequently, for LVDD improvement by increasing cGMP levels after treatment with IPDE-5 drugs.
Finally, the reduction of BNP-32 levels - a clinical biomarker widely used for diagnosis, prognosis, and treatment of heart failure 26 - in the short-term study revealed a close association with LVDD 12. Similarly to previous studies, which demonstrated that natriuretic peptides were strong predictors of diastolic dysfunction 27-29, the short-term study suggested the potential diagnostic role in measuring BNP-32 levels to evaluate cardiovascular alterations related to LVDD (Figure 1).
Clinical Implications
Resistant hypertension is a chronic disease and several factors that contribute to a complex pathophysiology might differ among the subjects, which compromise the efficacy of therapeutic regimens. Hence, those many different mechanisms may result in greater difficulties to achieve BP control, even despite the use of multiple drugs with confirmed adherence, leading to resistance to antihypertensive treatment 30,31. The challenge of RHTN treatment points out that the inclusion of new drugs is necessary to the therapeutic scheme of resistant hypertensive patients. In this context, recently IPDE-5 drugs were tested as antihypertensive treatment 13,14. Moreover, due to the high prevalence of LVDD in RHTN subjects 5 - which is associated with worse outcomes 32 - and evidence from preclinical studies that have demonstrated diastolic function improvement 6,24, IPDE-5 emerges as a highly promising candidate for the treatment of clinical conditions, such as LVDD, associated with resistance to antihypertensive therapy.
Some studies have sustained the hypothesis that IPDE-5 drug use is a viable pharmacological strategy for improvement in LV relaxation due to (1) shortening in both lateral and septal T E-E´(a Doppler-derived index of LV relaxation performance) 33; (2) the reverse cardiac remodeling effect; and (3) the reduced levels of BNP precursor over time 34. LVDD treatment in RHTN population is important because LVDD does not have a standard treatment, therefore the use of therapeutic candidates could reduce mortality, especially in resistant hypertensive subjects, who have high cardiovascular risk35.
Recent studies, including the acute study from our group11, have shown BP reduction after sildenafil administration14,26. This effect must be carefully interpreted. Although those studies may point out to a meaningful clinical effect on BP, we must consider that they were conducted in a short period of time, not allowing us to conclude that a chronic treatment would have the same impact on BP levels.
Finally, both acute and short period administration of IPDE-5 drugs (sildenafil and tadalafil, respectively) were well tolerated according to patient self-reports. This may represent a great clinical advantage, especially when treating RHTN subjects, since those patients are taking multiple drugs and the adverse effects are relevant for treatment adherence 36.
The results of the abovementioned acute and short-term studies contributed to advance our knowledge about potential therapeutic effects of IPDE-5 drugs on LVDD in RHTN patients. As we did not investigate drug action in the long term, those findings reinforce that future prospective clinical studies must be conducted to evaluate efficacy and safety of IPDE-5 candidates in treatment of LVDD using a larger RHTN population in a long-term trial.
Footnotes
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author contributions
Conception and design of the research: Moreno H; Acquisition of data: Faria APC; Analysis and interpretation of the data and Critical revision of the manuscript for intellectual content: Faria APC, Modolo R, Domingues-Moreno BV, Moreno H; Statistical analysis and Writing of the manuscript: Faria APC, Modolo R, Moreno H.
Sources of Funding
This study was funded by FAPESP and CNPq.
Study Association
This article is part of the thesis of Doctoral submitted by Thiago Quinaglia Araújo Costa Silva and Rodrigo Cardoso Santos, from Faculdade de Ciências Medicas da Universidade Estadual de Campinas.
References
- 1.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403–1419. doi: 10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 2.Persell SD. Prevalence of resistant hypertension in the United States, 2003-2008. Hypertension. 2011;57(6):1076–1080. doi: 10.1161/HYPERTENSIONAHA.111.170308. [DOI] [PubMed] [Google Scholar]
- 3.Pimenta E, Calhoun DA. Resistant hypertension: incidence, prevalence, and prognosis. Circulation. 2012;125(13):1594–1596. doi: 10.1161/CIRCULATIONAHA.112.097345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faria AP, Sabbatini AR, Coca A, Moreno H. Phenotypic characteristics of resistant hypertension in the Brazilian population. Arq Bras Cardiol. 2013;100(6):579–582. doi: 10.5935/abc.20130100. [DOI] [PubMed] [Google Scholar]
- 5.Ubaid-Girioli S, Adriana de Souza L, Yugar-Toledo JC, Martins LC, Ferreira-Melo S, Coelho OR, et al. Aldosterone excess or escape: Treating resistant hypertension. J Clin Hypertens (Greenwich) 2009;11(5):245–252. doi: 10.1111/j.1751-7176.2009.00110.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arnal JF, el Amrani AI, Chatellier G, Menard J, Michel JB. Cardiac weight in hypertension induced by nitric oxide synthase blockade. Hypertension. 1993;22(3):380–387. doi: 10.1161/01.hyp.22.3.380. [DOI] [PubMed] [Google Scholar]
- 7.Pechanova O, Bernatova I, Pelouch V, Babal P. L-NAME-induced protein remodeling and fibrosis in the rat heart. Physiol Res. 1999;48(5):353–362. [PubMed] [Google Scholar]
- 8.Ferreira-Melo SE, Yugar-Toledo JC, Coelho OR, De Luca IM, Tanus-Santos JE, Hyslop S, et al. Sildenafil reduces cardiovascular remodeling associated with hypertensive cardiomyopathy in NOS inhibitor-treated rats. Eur J Pharmacol. 2006;542(1-3):141–147. doi: 10.1016/j.ejphar.2006.04.039. [DOI] [PubMed] [Google Scholar]
- 9.Ferreira-Melo SE, Demacq C, Lacchini S, Krieger JE, Irigoyen MC, Moreno H. Sildenafil preserves diastolic relaxation after reduction by L-NAME and increases phosphodiesterase-5 in the intercalated discs of cardiac myocytes and arterioles. Clinics (Sao Paulo) 2011;66(7):1253–1258. doi: 10.1590/S1807-59322011000700022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solomon SD, Janardhanan R, Verma A, Bourgoun M, Daley WL, Purkayastha D, et al. Valsartan In Diastolic Dysfunction (VALIDD) Investigators Effect of angiotensin receptor blockade and antihypertensive drugs on diastolic function in patients with hypertension and diastolic dysfunction: a randomised trial. Lancet. 2007;369(9579):2079–2087. doi: 10.1016/S0140-6736(07)60980-5. [DOI] [PubMed] [Google Scholar]
- 11.Quinaglia T, de Faria AP, Fontana V, Barbaro NR, Sabbatini AR, Sertorio JT, et al. Acute cardiac and hemodynamic effects of sildenafil on resistant hypertension. Eur J Clin Pharmacol. 2013;69(12):2027–2036. doi: 10.1007/s00228-013-1571-z. [DOI] [PubMed] [Google Scholar]
- 12.Santos RC, de Faria AP, Barbaro NR, Modolo R, Ferreira-Melo SE, Matos-Souza JR, et al. Tadalafil-induced improvement in left ventricular diastolic function in resistant hypertension. Eur J Clin Pharmacol. 2014;70(2):147–154. doi: 10.1007/s00228-013-1611-8. [DOI] [PubMed] [Google Scholar]
- 13.Oliver JJ, Melville VP, Webb DJ. Effect of regular phosphodiesterase type 5 inhibition in hypertension. Hypertension. 2006;48(4):622–627. doi: 10.1161/01.HYP.0000239816.13007.c9. [DOI] [PubMed] [Google Scholar]
- 14.Oliver JJ, Hughes VE, Dear JW, Webb DJ. Clinical potential of combined organic nitrate and phosphodiesterase type 5 inhibitor in treatment-resistant hypertension. Hypertension. 2010;56(1):62–67. doi: 10.1161/HYPERTENSIONAHA.109.147686. Erratum in: Hypertension. 2012;60(1):e8. [DOI] [PubMed] [Google Scholar]
- 15.Jackson G, Benjamin N, Jackson N, Allen MJ. Effects of sildenafil citrate on human hemodynamics. Am J Cardiol. 1999;83(5A):13C–20C. doi: 10.1016/s0002-9149(99)00043-0. [DOI] [PubMed] [Google Scholar]
- 16.Nichols DJ, Muirhead GJ, Harness JA. Pharmacokinetics of sildenafil after single oral doses in healthy male subjects: absolute bioavailability, food effects and dose proportionality. Br J Clin Pharmacol. 2002;53(Suppl 1):5S–12S. doi: 10.1046/j.0306-5251.2001.00027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leite-Moreira AF, Correia-Pinto J, Gillebert TC. Afterload induced changes in myocardial relaxation: a mechanism for diastolic dysfunction. Cardiovasc Res. 1999;43(2):344–353. doi: 10.1016/s0008-6363(99)00099-1. [DOI] [PubMed] [Google Scholar]
- 18.Brutsaert DL, Sys SU, Gillebert TC. Diastolic failure: pathophysiology and therapeutic implications. J Am Coll Cardiol. 1993;22(1):318–325. doi: 10.1016/0735-1097(93)90850-z. [DOI] [PubMed] [Google Scholar]
- 19.Borlaug BA, Melenovsky V, Marhin T, Fitzgerald P, Kass DA. Sildenafil inhibits beta-adrenergic-stimulated cardiac contractility in humans. Circulation. 2005;112(17):2642–2649. doi: 10.1161/CIRCULATIONAHA.105.540500. [DOI] [PubMed] [Google Scholar]
- 20.Francis SH, Busch JL, Corbin JD, Sibley D. cGMP-dependent protein kinases and cGMP phosphodiesterases in nitric oxide and cGMP action. Pharmacol Rev. 2010;62(3):525–563. doi: 10.1124/pr.110.002907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reffelmann T, Kloner RA. Cardiovascular effects of phosphodiesterase 5 inhibitors. Curr Pharm Des. 2006;12(27):3485–3494. doi: 10.2174/138161206778343073. [DOI] [PubMed] [Google Scholar]
- 22.Takimoto E, Champion HC, Li M, Belardi D, Ren S, Rodriguez ER, et al. Chronic inhibition of cyclic GMP phosphodiesterase 5A prevents and reverses cardiac hypertrophy. Nat Med. 2005;11(2):214–222. doi: 10.1038/nm1175. [DOI] [PubMed] [Google Scholar]
- 23.Kass DA, Champion HC, Beavo JA. Phosphodiesterase type 5: expanding roles in cardiovascular regulation. Circ Res. 2007;101(11):1084–1095. doi: 10.1161/CIRCRESAHA.107.162511. [DOI] [PubMed] [Google Scholar]
- 24.Bishu K, Hamdani N, Mohammed SF, Kruger M, Ohtani T, Ogut O, et al. Sildenafil and B-type natriuretic peptide acutely phosphorylate titin and improve diastolic distensibility in vivo. Circulation. 2011;124(25):2882–2891. doi: 10.1161/CIRCULATIONAHA.111.048520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Westermann D, Becher PM, Lindner D, Savvatis K, Xia Y, Frohlich M, et al. Selective PDE5A inhibition with sildenafil rescues left ventricular dysfunction, inflammatory immune response and cardiac remodeling in angiotensin II-induced heart failure in vivo. Basic Res Cardiol. 2012;107(6):308. doi: 10.1007/s00395-012-0308-y. [DOI] [PubMed] [Google Scholar]
- 26.Parekh N, Maisel AS. Utility of B-natriuretic peptide in the evaluation of left ventricular diastolic function and diastolic heart failure. Curr Opin Cardiol. 2009;24(2):155–160. doi: 10.1097/HCO.0b013e328320d82a. [DOI] [PubMed] [Google Scholar]
- 27.Yamaguchi H, Yoshida J, Yamamoto K, Sakata Y, Mano T, Akehi N, et al. Elevation of plasma brain natriuretic peptide is a hallmark of diastolic heart failure independent of ventricular hypertrophy. J Am Coll Cardiol. 2004;43(1):55–60. doi: 10.1016/j.jacc.2003.07.037. [DOI] [PubMed] [Google Scholar]
- 28.Lubien E, DeMaria A, Krishnaswamy P, Clopton P, Koon J, Kazanegra R, et al. Utility of B-natriuretic peptide in detecting diastolic dysfunction: comparison with Doppler velocity recordings. Circulation. 2002;105(5):595–601. doi: 10.1161/hc0502.103010. [DOI] [PubMed] [Google Scholar]
- 29.Grewal J, McKelvie R, Lonn E, Tait P, Carlsson J, Gianni M, et al. BNP and NT-proBNP predict echocardiographic severity of diastolic dysfunction. Eur J Heart Fail. 2008;10(3):252–259. doi: 10.1016/j.ejheart.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 30.Sarafidis PA. Epidemiology of resistant hypertension. J Clin Hypertens (Greenwich) 2011;13(7):523–528. doi: 10.1111/j.1751-7176.2011.00445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams B. Resistant hypertension: an unmet treatment need. Lancet. 2009;374(9699):1396–1398. doi: 10.1016/S0140-6736(09)61600-7. [DOI] [PubMed] [Google Scholar]
- 32.Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289(2):194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 33.Rivas-Gotz C, Khoury DS, Manolios M, Rao L, Kopelen HA, Nagueh SF. Time interval between onset of mitral inflow and onset of early diastolic velocity by tissue Doppler: a novel index of left ventricular relaxation: experimental studies and clinical application. J Am Coll Cardiol. 2003;42(8):1463–1470. doi: 10.1016/s0735-1097(03)01034-9. [DOI] [PubMed] [Google Scholar]
- 34.Guazzi M, Vicenzi M, Arena R, Guazzi MD. PDE5 inhibition with sildenafil improves left ventricular diastolic function, cardiac geometry, and clinical status in patients with stable systolic heart failure: results of a 1-year, prospective, randomized, placebo-controlled study. Circ Heart Fail. 2011;4(1):8–17. doi: 10.1161/CIRCHEARTFAILURE.110.944694. [DOI] [PubMed] [Google Scholar]
- 35.Pierdomenico SD, Lapenna D, Bucci A, Di Tommaso R, Di Mascio R, Manente BM, et al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens. 2005;18(11):1422–1428. doi: 10.1016/j.amjhyper.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 36.de Souza WA, Sabha M, de Faveri Favero F, Bergsten-Mendes G, Yugar-Toledo JC, Moreno H. Intensive monitoring of adherence to treatment helps to identify "true" resistant hypertension. J Clin Hypertens (Greenwich) 2009;11(4):183–191. doi: 10.1111/j.1751-7176.2009.00102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]