Abstract
Background:
Most of the women suffer from vaginal atrophy and dryness, and therefore, efficient and safe treatment is needed to improve vaginal lubrication. Vitamin D has several important functions which may be effective in proliferation and repair of the epithelial tissue. This study aimed to evaluate the effect of vitamin D vaginal suppositories on maturation index, pH, and dryness in postmenopausal women.
Materials and Methods:
Women were enrolled in this double-blind clinical trial, in whom menopause occurred at least one year ago. Those women who had an abnormal Papanicolaou smear, had undergone hormonal treatment, or have had vaginal infection in the previous year were excluded. Forty-four women who found eligible were randomized into two equal groups, the treatment and control groups, which received vitamin D and placebo vaginal suppository daily for 8 weeks, respectively. Vaginal pH and maturation value were measured at the beginning and end of the study. Pain, dryness, and paleness were assessed before treatment and at the end of the 2, 4, and 8 weeks of treatment.
Results:
In the treatment group, the number (Mean ± SD) of superficial cells increased (69.76 ± 12.4) and vaginal pH decreased (1.42 ± 0.67) significantly compared to the control group after 56 days. The mean pain significantly reduced after 8 weeks in the treatment group (1.23 ± 0.53) compared to the control group 1.95 ± 0.74 (P < 0.001). The mean of dryness and paleness reduced significantly in the treatment group versus control at 56 days.
Conclusions:
Vitamin D is effective in improving the maturation index and decreased the pH and dryness of the vaginal atrophy due to menopause.
Keywords: Estrogen replacement, Iran, menopause, vaginal suppository, vitamin D
INTRODUCTION
Menopause is the stage of a woman's reproductive life that is accompanied by estrogen deficiency which has many negative effects on the vaginal mucosa, such as dryness, irritation, and vaginal atrophy.[1,2] There is evidence that vulvovaginal atrophy is a common condition in postmenopausal women.[3,4] In a normal condition, the vaginal epithelium is rugated, moist, and thick, whereas in estrogen deficiency, it becomes dry and thin.[5] Therefore, estrogen hormone is essential to maintain the normal structure and function of the vaginal tract. So, external intervention is needed to reduce the common symptoms including postcoital bleeding, dyspareunia, pruritus, and soreness in postmenopausal women.[6] Various treatments such as hormonal therapy and vaginal moisturizers have been considered and evaluated for vaginal atrophy.[7,8] Although vaginal estrogens are an effective treatment for vulvovaginal atrophy, there are concerns in some women with a history of breast or endometrial hyperplasia.[9] Also, a report says that the systemic estrogen can increase the thrombosis and breast cancer risk.[10] So, non-hormonal alternative treatment is necessary to get rid of the adverse effects of exogenous estrogen. Vitamin D [1,25-dihydroxyvitamin D3 (1,25(OH) 2D3] is a promoter of keratinocyte differentiation and proliferation in the epidermis.[11] It has been documented that the vaginal epithelium becomes atrophic in the absence of estradiol.[12] Another study showed that the use of calcitriol has a beneficial effect on vaginal atrophy in postmenopausal women and it could be an alternative to estrogen therapy.[13] Also, 1,25(OH) 2D3 can used in different diseases including diabetes, cancer, and psoriasis.[14] Furthermore, in an experimental study, treatment with exogenous vitamin D3 in ovariectomized rats led to expression of vitamin D receptor in the superficial layers of the vaginal epithelium.[12] Conflicting reports suggest that calcium with Vitamin D treatment following discontinuation of postmenopausal hormone therapy in osteoporotic women cause the worsening of vaginal atrophy symptoms.[15] This contrasting evidence created some questions about the beneficial effects of 1,25(OH) 2 D3 on vaginal atrophy which have not been answered. Thus, this clinical trial was conducted to evaluate whether vitamin D vaginal suppository could improve the sexual pain, maturation index, and vaginal atrophy in postmenopausal women.
MATERIALS AND METHODS
This study was a double-blind clinical trial that was approved by the institutional ethics committee of medical sciences and was registered in the Iranian registry of clinical trials (http://irct.ir) with IRCT No.: IRCT201111185109N1. A follicle-stimulating hormone (FSH) test were used to confirmed whether the women has gone through menopause. postmenopausal women were enrolled in this clinical trial who menopause occurred for at least 1 year up to 4 years. Those women who had an abnormal Papanicolaou smear or have had hormonal treatment or existence of vaginal infection in the previous year were excluded from the study. Forty-four women who found eligible were randomized into two equal groups, the treatment and control groups, which received vitamin D and placebo vaginal suppository daily for 8 weeks, respectively.
Suppository preparation
Placebo suppositories consisted of Suppocire AM-15, a semi-synthetic fatty acid glyceride (courtesy Gattefosse, Lyon, France), and vitamin D suppositories 1000 IU vitamin D (Rocatrol, Roche, Sweden) were mixed with placebo suppositories. They were stored refrigerated until the time of their usage.
Placebo and vitamin D suppositories were placed in the same envelopes, and the statistical consultant encoded them using a random number from 1 to 44 so that the researcher and the patient were not aware of the content. Forty-four women were randomized to one of two medication regimens and were educated to insert the suppositories into the vagina daily for 8 weeks.
Specimen preparation and outcome measures
Samples were obtained from the vaginal mucosa by rotating a special brush (Vibabrush; Rovers BV, Oss, the Netherlands) near the posterior fornix of the vaginal wall. Smears were put on a glass slide, immediately fixed with Spray-Cyte, and stained by the Papanicolaou procedure. To determine the vaginal maturation value (VMV), the numbers of parabasal, intermediate, and superficial cells in 100 cells from the smear were counted before treatment and at 56 days of the study. A 100-cell count was performed to classify cells as superficial (S), intermediate (I), and parabasal (P) squamous cell types. As previously described, the VMV has a range of 0–100 and it was calculated using the equation (1 × S) + (0.5 × I) + (0 × P).[16] Vaginal pH was measured using pH meter strip (Macherey- Nagel, Germany). to the posterior wall of the vaginal wall at the beginning and the end of the study. A questionnaire was used to collect information about the demographic characteristics. The diagnosis of pain on touch of the vestibule or intercourse was established based on self-assessment, whereas dryness and paleness were assessed before treatment and at the end of 2, 4, and 8 weeks after treatment by a midwife who was not aware of the groups. Pain, dryness, and intensity of paleness were assessed as none, mild, moderate, or severe. Then, the researcher gave a score in terms of the 4-point scale (0 = absent, 1 = mild, 2 = moderate, 3 = severe).
Statistical analysis
Statistical analysis was performed by using SPSS. A comparison of a nominal variable, vaginal pH scores, and VMV between the two groups was performed using the independent samples t-test. Data are expressed as mean ± SD; the significance level was set up at P less than 0.05.
RESULTS
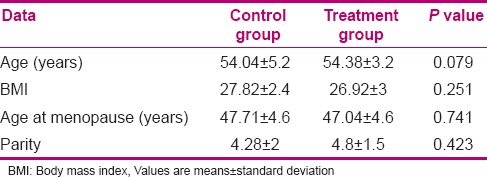
As shown in Table 1, the results indicated no significant relation in age, body mass, the age at menopause, and parturition between the two groups [Table 1].
Table 1.
Demographic characteristics in both groups (mean±SD)
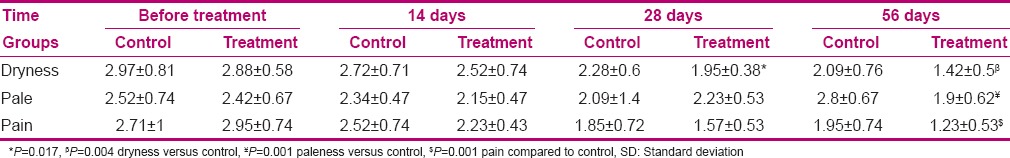
As shown in Table 2, independent samples t-test showed no significant relation in mean pain during intercourse before treatment and from the first to the fourth week of the study. Results showed that the difference in the mean pain scores between the two groups increased from the 2nd week toward the 8th week [Table 2]. The mean pain scores decreased in the treatment group significantly compared to the control group after 56 days. Results also showed the mean values of dryness and paleness were the same before treatment and until 14 days of the study [Table 2], whereas dryness and paleness decreased significantly in the treatment group compared to the control group at 56 days [Table 2].
Table 2.
Mean pain, dryness, and paleness in both groups (mean±SD)
The mean of pH in women with vitamin D vaginal suppository was significantly lower than in women with placebo suppositories (P < 0.001) at 56 days after treatment [Table 3]. The numbers of parabasal, intermediate, and superficial cells from the smear were counted before treatment and at 56 days of the study in both the groups. Independent samples t-test showed there was not any significant difference between the two groups before treatment [Table 3]. Eight weeks after the study, the mean of superficial cells (Mean ± SD: 69.76 ± 12.4) in the treatment group increased significantly in comparison to the control group (54.66 ± 18.38) [Table 3]. Epithelial parabasal cells increased in women with placebo vaginal suppository compared to the number in the women of treatment group [Figure 1].
Table 3.
Vaginal pH and histological findings in both groups
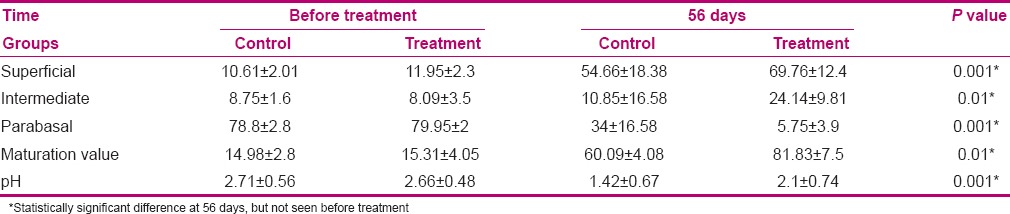
Figure 1.
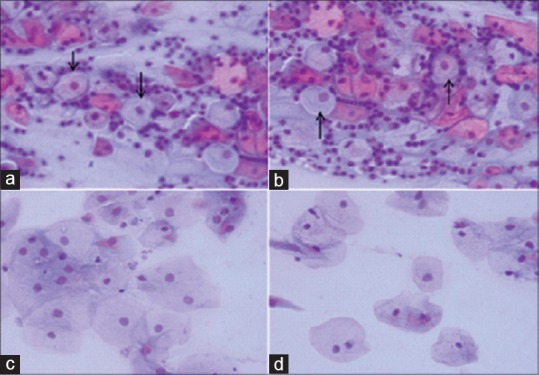
Posterior vaginal wall smear showing decrease in the number of parabasal cells (arrow) and increase in superficial cells in women with vitamin D vaginal suppository (a, c) compared to the placebo suppositories (b, d), 8 weeks after treatment. Papanicolaou, scale bar: 100 µm (a, b), 50 µm (c, d)
DISCUSSION
This clinical trial showed that vitamin D vaginal suppositories have protective effects that decrease the mean pain during intercourse, vaginal pH, dryness, and paleness and help increase the vaginal maturation value compared to the placebo suppositories. These findings are in agreement with the study of Yildirim and colleagues who reported that the biological effect of vitamin D on vaginal epithelium is mediated by its receptors.[17] The findings of the study showed the mean of the superficial cells in the treatment group increased from nearly 10 to 68 cells during the study. These findings are supported by the result of Abban and colleagues that the intracellular receptors of vitamin D are in the basal and suprabasal layers of the vaginal epithelium.[12,18] Further, these receptors not only exist in stratified squamous epithelium, but also are found on vascular smooth muscle, endothelium, and cardiomyocytes.[19] In the present study, vitamin D vaginal suppositories protected the vaginal squamous epithelium and caused an increase of superficial cells [Figure 1].
Our data demonstrated that dryness decreased by 26% in women with vitamin D vaginal suppositories. This result is in agreement with Checa et al.'s report that vitamin D is effective in treating vaginal dryness with its receptors.[15] Importantly, our data showed the decrease in vaginal pH which improves the microenvironment of the epithelial layers of the mucous membrane, and also hydration and elasticity of the vaginal mucosa. The acidic conditions of the vagina indicate a healthy vaginal ecology and is a potential to prevent growth of pathogens such as Gardnerella vaginalis, Mycoplasma hominis and anaerobes, which are increased in diseased vagina.[20] Although estrogen therapy is the main approach to treat vaginal atrophy and has numerous protective effects on the urogenital tissue,[21] it is contraindicated in many women with a history of breast cancer, stroke, dementia, or venous thromboembolism.[22] So, hormone replacement therapy is beneficial for postmenopausal women to reduce the risk of cardiovascular disease, endometrial hyperplasia, and colon cancer.[23] Thus, vaginal moisturizers and lubricants are the alternative choices for vaginal atrophy. Furthermore, it has been found that there is no report regarding the side effect of vitamin D.[13] Therefore, vitamin D vaginal suppository is available without prescription and is used as a lubricant and vaginal moisturizer. Thus, it can be a new strategy to treat vaginal atrophy.[13] Vitamin D was also found to have antiapoptotic and antifibrotic effects and acts as a pleiotropic hormone with proliferative and differentiation effects on numerous cell types.[24] Other non-hormonal alternative treatment, such as Replens, has been shown to be effective in relieving menopausal atrophic vaginitis, but it needs a carbomer-polycarbophil system.[25] Although vitamin D reduces friction and vaginal dryness, contrasting evidence indicates that lubricants and moisturizers are ineffective to treat vaginal atrophy symptoms.[24] But in the present study, reduction of vaginal pH and increase of superficial cells in the vaginal epithelium demonstrated that vitamin D is effective to repair the histology and alleviate existing symptoms. The possible mechanism by which vitamin D brings about the restoration of vaginal epithelium could be explained by its regulatory action on calcium and phosphate metabolism in stratified squamous epithelium.[26] Although low-dose vaginal estrogen could restore the thickness and flexibility of the vaginal tissue, some adverse effects, such as vaginal bleeding and breast pain, have been associated with conjugated equine estrogen cream therapy.[27] Thus, some hormone replacement therapy could be more effective for vaginal maturation and to restore the morphology of vaginal atrophy in post-menopausal women than an estrogen cream.[28] In accordance with an earlier report, our result also showed vitamin D supplementations improve vaginal maturation.[13]
CONCLUSION
The results of this study showed vitamin D have protective effects for vaginal atrophy in postmenopausal women, and in particular this methods is expensive, practical and easy to reach. It is a new safe therapeutically agent, without any reaction and have effects in improving the VMV. Therefore, the application of vitamin D in vaginal atrophy treatment should be pursued.
ACKNOWLEDGMENT
This article was extracted from an MSc thesis in Ahvaz University of Medical Sciences, No.: B-90/0020. We wish to thank Dr. Mossavi, Ph.D. in Biostatistics from Yasuj University of Medical Sciences, for his helpful comments and statistical analysis.
Footnotes
Source of Support: Ahvaz University of Medical Sciences.
Conflict of Interest: There is no conflict of interest in this paper.
REFERENCES
- 1.Minkin MJ, Maamari R, Reiter S. Improved compliance and patient satisfaction with estradiol vaginal tablets in postmenopausal women previously treated with another local estrogen therapy. Int J Womens Health. 2013;5:133–9. doi: 10.2147/IJWH.S41897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sparavigna A, Tenconi B, De Ponti I, Bulgheroni A, Scarci F. A controlled, randomized, open label study in postmenopausal women to assess the safety and the efficacy of a vaginal moisturizer: An instrumental approach. Open J Obstet Gynecol. 2013;3:395–9. [Google Scholar]
- 3.Reiter S. Barriers to effective treatment of vaginal atrophy with local estrogen therapy. Int J Gen Med. 2013;6:153–8. doi: 10.2147/IJGM.S43192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berman JR, Adhikari SP, Goldstein I. Anatomy and physiology of female sexual function and dysfunction: Classification, evaluation and treatment options. Eur Urol. 2000;38:20–9. doi: 10.1159/000020247. [DOI] [PubMed] [Google Scholar]
- 5.Castelo-Branco C, Cancelo MJ, Villero J, Nohales F, Julia MD. Management of post-menopausal vaginal atrophy and atrophic vaginitis. Maturitas. 2005;52:46–2. doi: 10.1016/j.maturitas.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 6.Derzko C, Elliott S, Lam W. Management of sexual dysfunction in postmenopausal breast cancer patients taking adjuvant aromatase inhibitor therapy. Curr Oncol. 2007;14:21–40. doi: 10.3747/co.2007.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lian U. The role of local vaginal estrogen treatment in urogenital atrophy. Expert Rev Obstet Gynecol. 2012;7:545–6. [Google Scholar]
- 8.Van der Laak JA, De Bie LM, De Leeuw H, De Wilde PC, Hanselaar AG. The effect of Replens on vaginal cytology in the treatment of postmenopausal atrophy: Cytomorphology versus computerised cytometry. J Clin Pathol. 2002;55:446–1. doi: 10.1136/jcp.55.6.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Unfer V, Casini ML, Costabile L, Mignosa M, Gerli S, Di Renzo GC. Endometrial effects of long-term treatment with phytoestrogens: A randomized, double-blind, placebo-controlled study. Fertil Steril. 2004;82:145–8. doi: 10.1016/j.fertnstert.2003.11.041. [DOI] [PubMed] [Google Scholar]
- 10.Notelovitz M, Funk S, Nanavati N, Mazzeo M. Estradiol absorption from vaginal tablets in postmenopausal women. Obstet Gynecol. 2002;99:556–2. doi: 10.1016/s0029-7844(01)01385-0. [DOI] [PubMed] [Google Scholar]
- 11.Bikle D, Teichert A, Hawker N, Xie Z, Oda Y. Sequential regulation of keratinocyte differentiation by 1,25(OH) 2D3, VDR, and its coregulators. J Steroid Biochem Mol Biol. 2007;103:396–4. doi: 10.1016/j.jsbmb.2006.12.063. [DOI] [PubMed] [Google Scholar]
- 12.Abban G, Yildirim NB, Jetten AM. Regulation of the vitamin D receptor and cornifin beta expression in vaginal epithelium of the rats through vitamin D3. Eur J Histochem. 2008;52:107–4. doi: 10.4081/1200. [DOI] [PubMed] [Google Scholar]
- 13.Yildirim B, Kaleli B, Düzcan E, Topuz O. The effects of postmenopausal Vitamin D treatment on vaginal atrophy. Maturitas. 2004;49:334–7. doi: 10.1016/j.maturitas.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Zhu X, Wang B, Zhao G, Gu J, Chen Z, Briantais P, et al. An investigator- masked comparison of the efficacy and safety of twice daily applications of calcitriol 3 microg/g ointment vs. calcipotriol 50 microg/g ointment in subjects with mild to moderate chronic plaquetype psoriasis. J Eur Acad Dermatol Venereol. 2007;21:466–72. doi: 10.1111/j.1468-3083.2006.01913.x. [DOI] [PubMed] [Google Scholar]
- 15.Checa MA, Garrido A, Prat M, Conangla M, Rueda C, Carreras R. A comparison of raloxifene and calcium plus Vitamin D on vaginal atrophy after discontinuation of long-standing postmenopausal hormone therapy in osteoporotic women A randomized, masked-evaluator, one-year, prospective study. Maturitas. 2005;52:70–7. doi: 10.1016/j.maturitas.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Meisels A. The maturation value. Acta Cytol. 1967;11:249–5. [PubMed] [Google Scholar]
- 17.Yildirim B, Abban G, Erdogan BS. Immunohistochemical detection of 1,25-dihydroxyvitamin D receptor in rat vaginal epithelium. Fertil Steril. 2004;82:1602–8. doi: 10.1016/j.fertnstert.2004.07.949. [DOI] [PubMed] [Google Scholar]
- 18.Kutuzova GD, Deluca HF. Gene expression profiles in rat intestine identify pathways for 1,25-dihydroxyvitamin D3 stimulated calcium absorption and clarify its immunomodulatory properties. Arch Biochem Biophys. 2004;432:152–6. doi: 10.1016/j.abb.2004.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Motiwala SR, Wang TJ. Vitamin D and cardiovascular risk. Curr Hypertens Rep. 2012;14:209–8. doi: 10.1007/s11906-012-0262-y. [DOI] [PubMed] [Google Scholar]
- 20.Skarin A, Sylwan F. Vaginal lactobacilli inhibiting growth of G vaginalis mobiluncus and others bacterial species cultured from vaginal content of women with bacterial vaginosis. Acta Pathol Microbiol Immune Scand. 1987;94:399–3. doi: 10.1111/j.1699-0463.1986.tb03074.x. [DOI] [PubMed] [Google Scholar]
- 21.Ulrich L. The role of local vaginal estrogen treatment in urogenital atrophy. Expert Rev Obstet Gynecol. 2012;7:545–6. [Google Scholar]
- 22.Scarabin PY, Oger E, Plu-Bureau G EStrogen and THrombo Embolism Risk Study Group. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet. 2003;362:428–2. doi: 10.1016/S0140-6736(03)14066-4. [DOI] [PubMed] [Google Scholar]
- 23.Grodstein F, Stampfer M. The epidemiology of coronary heart disease and estrogen replacement in postmenopausal women. Prog Cardiovasc Dis. 1995;38:199–10. doi: 10.1016/s0033-0620(95)80012-3. [DOI] [PubMed] [Google Scholar]
- 24.Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. A systematic review and meta-analysis. J Clin Endocrinol Metab. 2007;92:2017–29. doi: 10.1210/jc.2007-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nachtigall LE. Comparative study. Replens versus local estrogen in menopausal women. Fertil Steril. 1994;61:178–80. doi: 10.1016/s0015-0282(16)56474-7. [DOI] [PubMed] [Google Scholar]
- 26.Bikle D, Teichert A, Hawker N, Xie Z, Oda Y. Sequential regulation of keratinocyte differentiation by 1,25(OH) 2D3, VDR, and its coregulators. Steroid Biochem Mol Biol. 2007;103:396–4. doi: 10.1016/j.jsbmb.2006.12.063. [DOI] [PubMed] [Google Scholar]
- 27.Pritchard KI. The role of hormone replacement therapy in women with a previous diagnosis of breast cancer and a review of possible alternatives. Ann Oncol. 2001;12:301–10. doi: 10.1023/a:1011197007606. [DOI] [PubMed] [Google Scholar]
- 28.Bygdeman M, Swahn ML. Replens versus dienoestriol cream in the symptomatic treatment of vaginal atrophy in postmenopausal women. Maturitas. 1996;23:259–63. doi: 10.1016/0378-5122(95)00955-8. [DOI] [PubMed] [Google Scholar]


