Abstract
Background:
Rehabilitative ultrasound Imaging (RUSI) is increasingly used in the management of musculoskeletal conditions as it provides an objective measure of muscle function while being less invasive than needle electromyography. While research has documented the ability to reliably measure trunk muscles in patients with back pain, no study to date has used RUSI to quantify infraspinatus muscle function in patients with shoulder impingement syndrome (SIS).
Hypothesis/Purpose:
The purpose of this study was to examine the intra‐rater and inter‐rater reliability of measuring infraspinatus muscle thickness with RUSI and to compare such measures during resting versus contracted muscle states and in the symptomatic versus asymptomatic shoulders in patients with SIS.
Study Design:
Cross‐sectional, measurement study
Methods:
Fifty‐two participants with unilateral SIS underwent a standard baseline examination to include RUSI of the infraspinatus muscle bilaterally. Images were acquired at rest and during a submaximal isometric contraction, by two novice examiners. The isometric contraction was elicited by having prone participants externally rotate their shoulder from a position of 90° abduction into a dynamometer and hold a static force of 20 mmHg (approximately 20‐30% maximal voluntary contraction). Images were captured using a standardized placement of the transducer placed just inferior to the spine of the scapula along the medial scapular border and measured off‐line using Image J software (V1.38t, National Institutes of Health, Bethesda, Maryland).
Results:
Estimates (ICCs) for thickness measurements ranged between 0.96 and 0.98 for intra‐rater reliability and between 0.87 and 0.92 for inter‐rater reliability. Reliability was substantially lower (ICC = 0.43 to 0.79) for calculations of percent thickness change. The infraspinatus muscle was significantly thicker when contracted (19.1mm) than during rest (16.2mm) in both shoulders (p < 0.001). There was also a statistically significant interaction between contraction state and shoulder (p = 0.026), indicating that the change in thickness that occurred during contraction was significantly smaller in the symptomatic shoulder than in the asymptomatic shoulder.
Conclusion:
RUSI measurements of infraspinatus muscle thickness appear to be highly reliable, both within the same examiner and between different examiners, in patients with SIS. Moreover, such measurements were different in rested and contracted states of the infraspinatus, as well as, between the symptomatic and asymptomatic shoulders of patients with unilateral SIS.
Level of evidence:
Level 2
Keywords: Infraspinatus muscle, muscle function, reliability, shoulder impingement syndrome, shoulder pain, ultrasound imaging
INTRODUCTION
Shoulder disorders are second only to low back pain as the most common musculoskeletal disorder, with shoulder impingement syndrome (SIS) being the most prevalent.1,2 SIS is described as pain or pathology located in the rotator cuff tendons, subacromial bursa and subacromial space.2 There are many factors that are believed to be involved with the pathogenesis of SIS; repetitive use of the shoulder muscles, incorrect scapulothoracic rhythm, instability of the glenohumeral joint, degeneration of the rotator cuff tendons, and altered shapes of the acromion.3,4 Patients with SIS have been found to have decreased strength during resisted external rotation of the shoulder5 and a significantly elevated position of the humeral head during arm elevation when compared to individuals without shoulder pain.6,7 Alterations in the relative contribution of the deltoid and rotator cuff muscles during shoulder activities have also been reported in patients with SIS potentially leading to unwanted humeral head superior translation.8,9 It is hypothesized that the decreased function of the infraspinatus, as seen in SIS, contributes to the production of SIS pain.3,4
Although the construct of muscle function is multifactorial, the function of the infraspinatus has been measured through manual muscle testing (isometric force), electromyography (electrical activity), isokinetic testing (isokinetic force), and magnetic resonance imaging (volume changes) studies.5,8–10 These methods can be costly, time consuming, non‐specific, and invasive or uncomfortable procedures. An evolving, non‐invasive method of quantifying muscle function is rehabilitative ultrasound imaging (RUSI).11,12 Used to date primarily in the muscles of the trunk, RUSI relies on measurements taken of muscle morphology (thickness or cross sectional area) at rest and comparing them to morphology measurements during isometric muscle contraction. The amount of change in morphology (thickness or cross sectional area) during the contraction or task is considered an indirect measure of muscle function.11 Studies have consistently found RUSI to provide reliable measures of abdominal and lumbar multifidus muscle thickness.13 Similar studies of trunk muscles have also found RUSI to be helpful in discriminating between patients with back pain and those without back pain.14–16 However, when comparing RUSI measures to the criterion standard of kinesiological EMG, studies have found mixed results that seem to depend both upon the muscle being studies and the contraction strategy used.17
Most studies to date have focused on muscles of the trunk in patients with back pain, however recent studies have examined the use of RUSI in scapular and shoulder muscles.18–22 Specifically, the reliability of RUSI measures of trapezius muscle morphometry and function have been described.21–24 Two studies have measured muscle function of shoulder muscles using RUSI, however, they were either performed in asymptomatic individuals or the results were not quantified numerically.19,20 Therefore, the purpose of this study was to estimate the intra‐rater and inter‐rater reliability of RUSI measurements of infraspinatus muscle thickness in patients with unilateral SIS. Additionally, RUSI measurements of infraspinatus muscle thickness during resting versus contracted muscle states were compared and in the symptomatic versus asymptomatic shoulders.
Methods
Participants
Fifty‐two volunteers between the ages of 18‐60 with current unilateral shoulder pain were recruited through email, flyers, and service announcements that were posted around or electronically distributed to military installations around San Antonio, Texas. Participants were included if they had shoulder impingement syndrome, as defined by; anterior and/or lateral shoulder pain that reached at least 4/10 on the Numerical Pain Rating Scale (NPRS) with daily activity and were positive for at least two of the three following clinical diagnostic criteria for SIS5: positive Hawkins‐Kennedy impingement sign, painful arc between 60‐120°, and/or pain or weakness with the infraspinatus manual muscle test. Participants were excluded if they had a history of prior trauma or shoulder surgery, signs of cervical radiculopathy, radiculitis or referral from the cervical spine, evidence of full‐thickness rotator cuff tear, signs of adhesive capsulitis, known pregnancy, or any previous injection, acupuncture, dry needling or strengthening interventions within the past six months. Participants were also included in an interventional dry needling study, therefore, anyone with potential contraindications to dry needling (known pregnancy, anticoagulation medications and blood clotting disorders) were also excluded.
Examiners
All RUSI measures were performed by physical therapy doctoral students with no previous experience in RUSI. Prior to testing, examiners underwent approximately 12 hours of hands on training with faculty co‐investigators experienced with RUSI. Additionally, examiners performed pilot assessments on 10 asymptomatic participants for practice and methodology refinement. Ultrasound examiners were blinded to the subject’s affected shoulder side and to all prior measurements during imaging.
Procedures
The RUSI device used in this study was the SonoSite Titan and M‐Turbo with a 38mm linear array transducer. Imaging began with the left shoulder for all participants regardless of which side was symptomatic. Subjects were prone with their left shoulder abducted to 90 degrees. Subjects’ shoulders and upper arm were supported by the table while the crease of the subject’s elbow rested comfortably on the edge of the table and allowed the forearm to passively hang vertically. Their wrist was secured to a pressure cuff, which was also secured to the table to prevent unintended movement and enable a measureable, standardized isometric contraction of the infraspinatus muscle. The subject’s head was turned ipsilaterally so they could see the pressure cuff gauge measuring the mmHg exerted against the cuff (Figure 1).
Figure 1.
Imaging and isometric infraspinatus muscle contraction procedure
During imaging, the examiner first identified the medial border of the scapula while scanning in the transverse plane parallel with the orientation of the infraspinatus muscle fibers. The ultrasound transducer was then positioned so the superomedial border of the spine of the scapula was lined up on the left side of the ultrasound screen. Examiners exerted as little pressure through the ultrasound head as possible to avoid compressing the infraspinatus muscle and inadvertently changing its shape and/or thickness. After an image of the subject’s infraspinatus was taken at rest, they were then instructed to externally rotate their shoulder until a pressure of 20 mmHg (approximately 20‐30% maximal voluntary contraction) was exerted through the cuff secured to their wrist. The subject maintained that pressure, using visual feedback from the gauge, until an ultrasound image of their isometrically contracted infraspinatus was taken. A submaximal contraction was desired for the study and 20 mmHg was chosen to standardize the subjects’ contractile force. This pressure was chosen in an attempt to reduce variability between subjects and was low enough that subjects could maintain the contraction without increasing their pain or causing fatigue while still showing a change in muscle thickness. As soon as the image was taken the subject was allowed to relax and the transducer was removed.
These methods were repeated two more times on the left shoulder for a total of six images; three at rest and three contracted. Although the exact time between images was not standardized, the protocol resulted in approximately one minute between each image acquisition. Once the primary examiner collected all six images, the second examiner then repeated the process again on the left shoulder and collected six more images. After twelve images total had been captured, the process was repeated on the subject’s right shoulder with the examiners resuming their original roles and once more each taking a set of six images. These 24 images completed the image collection process.
Measurements
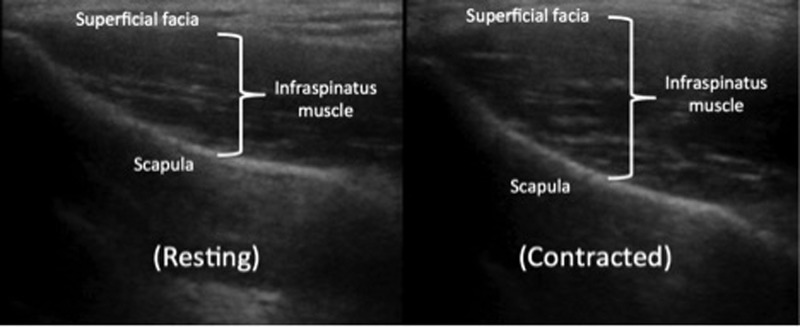
After data collection, the images were downloaded to a laptop computer and measured using Image J software (V1.38t, National Institutes of Health, Bethesda, Maryland). The thickness of the infraspinatus muscle was measured in the center of the image and reported in millimeters (to the nearest hundredth). This measurement was taken from the inferior‐most aspect of the superficial fascia to the most superior aspect of the infraspinous fossa; which appeared as a bright, continuous hyperechoic line spanning the width of the screen (Figure 2). This process was repeated on every image. After all the measurements were taken, the depth of the infraspinatus at rest was subtracted from the depth during contraction to find the difference.
Figure 2.
Image measurement procedure
Statistical Analysis
All data were analyzed with SPSS Version 21 software (Chicago, IL). The dependent measures were resting thickness, contracted thickness, and percent thickness change of the infraspinatus muscle. Percent thickness change was calculated by the equation (Thicknesscontracted–Thicknessrest)/Thicknessrest.
Intraclass correlation coefficients (ICCs) with 95% CIs were calculated to assess intra‐rater (ICC3,3) and inter‐rater (ICC2,1) reliability. Based on previous work investigating RUSI of reliability of abdominal muscles, the mean of three measures was used as the analysis of interest for intra‐rater reliability.25 To quantify measurement error, standard error of measurement (SEM) was calculated as (SD 3 √ [1‐ICC]). Minimal detectable change (MDC) was calculated as (1.96 3 SEM 3 √2) and represents the minimal change in thickness that must occur to be 95% confident that a true change occurred.26,27 Both SEM and MDC were calculated using the ICC estimates for intra‐rater reliability.
Differences in RUSI measurements were assessed using 2x2 repeated measures analysis of variance (ANOVA) on muscle thickness for contraction state (resting vs. contracted) and shoulder (symptomatic vs. asymptomatic) using alpha = 0.05. A main effect for contraction state was examined to determine if RUSI was able to distinguish between resting and contracted states. The interaction between contraction state and shoulder was examined to determine if RUSI was able to discriminate the amount of thickness change between symptomatic and asymptomatic shoulders.
Results
Demographic and patient history information for the 52 participants is listed in Table 1. Participants’ symptoms were generally chronic in nature and caused moderate shoulder‐related disability. Mean infraspinatus muscle thickness values and percent thickness change from rest to contracted state are listed in Table 2. Point estimates (ICCs) for thickness measurements ranged between 0.89 and 0.92 for intra‐rater reliability and between 0.96 and 0.98 for inter‐rater reliability. Reliability was substantially lower (ICC = 0.43 to 0.79) for calculations of percent thickness change (Table 2). Estimates of measurement error were very small for thickness measures (0.6mm to 0.8mm), but substantially larger for percent thickness change (5.7 to 5.8%).
Table 1.
Baseline Demographic and History Information
| Characteristics | Mean +/‐ SD |
|---|---|
| Age, (years) | 43.6 ± 10.2 |
| Sex (% women/%men) | 37%/63% |
| BMI, (kg/m2) | 28.4 ± 4.8 |
| Pain in dominant shoulder | 64% |
| Duration of symptoms, m* | 11.2 (5.1, 38.3) |
| PSS, total# | 64.3 ± 10.3 |
| Pain subscale | 16.7 ± 4.5 |
| Satisfaction subscale | 4.1 ± 2.4 |
| Function subscale | 43.4 ± 6.6 |
Abbreviations: BMI, body mass index; PSS, Pennsylvania Shoulder Score
Median, Interquartile range
PSS total: 0–100, 100 = no pain, fully satisfied with shoulder use, and full function. Pain subscale: 0–30, 30 = no pain. Satisfaction subscale: 0–10, 10 = fully satisfied with shoulder use. Function subscale: 0–60, 60 = full function
Table 2.
Reliability of Infraspinatus RUSI measures
| Mean +/‐ SD | Inter‐rater ICC (95% CI) | Intra‐rater ICC (95% CI) | SEM | MDC | |
|---|---|---|---|---|---|
| Symptomatic Shoulder | |||||
| Relaxed Thickness | 16.4 +/‐ 4.1 mm | .89 (.82‐.94) | .96 (.94‐.98) | 0.8mm | 2.4mm |
| Contracted Thickness | 19.0 +/‐ 4.3 mm | .92 (.87‐.96) | .98 (.96‐.99) | 0.7mm | 1.9mm |
| % Thickness Change | 17.1% +/‐ 10.6% | .43 (.19‐.62) | .79 (.67‐.87) | 5.7% | 15.8% |
| Asymptomatic Shoulder | |||||
| Relaxed Thickness | 16.0 +/‐ 3.6 mm | .87 (.78‐.92) | .98 (.96‐.98) | 0.6mm | 1.6mm |
| Contracted Thickness | 19.1 +/‐ 4.0 mm | .90 (.83‐.94) | .97 (.96‐.98) | 0.7mm | 1.8mm |
| % Thickness Change | 19.9% +/‐ 10.3% | .61 (.41‐.75) | .54 (.38‐.68) | 5.8% | 16.1% |
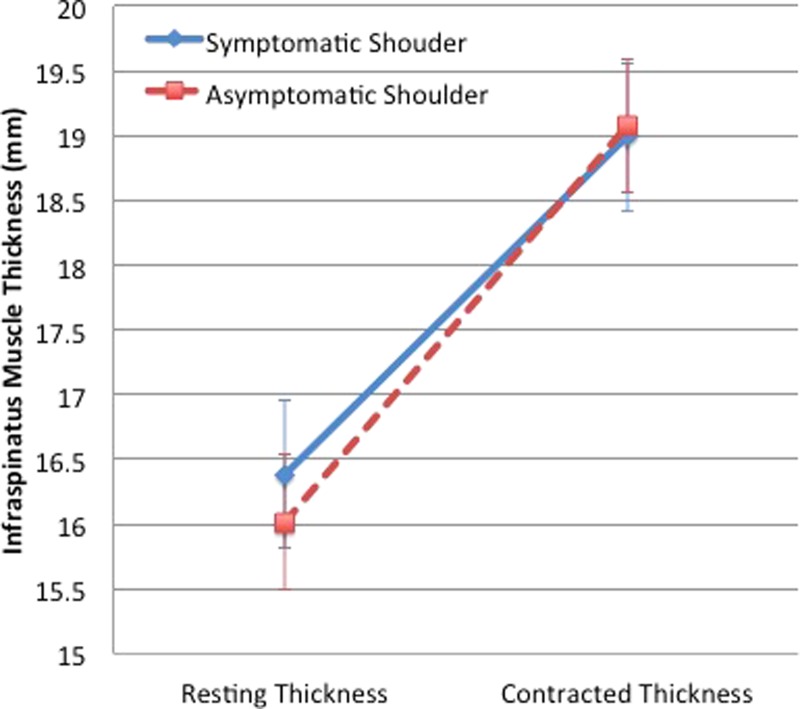
There was a statistically significant main effect for contraction state (p < 0.001) indicating that the infraspinatus muscle was significantly thicker when contracted (19.1mm) than during rest (16.2mm) across both shoulders. There was also a statistically significant interaction between contraction state and shoulder (p = 0.026), indicating that the change in thickness that occurred during the submaximal contraction was significantly smaller in the symptomatic shoulder than in the asymptomatic of patients with SIS (Figure 3).
Figure 3.
Change in infraspinatus muscle thickness between rest and contraction by shoulder
Discussion
RUSI is an evolving tool used to non‐invasively quantify muscle function.11 Studies using RUSI to date have primarily focused on muscles of the trunk in relation to patients with back pain.13,17 Rotator cuff muscles, particularly the infraspinatus, have been found to have deficits in patients with SIS,8,9 however, quantifying such deficits has been challenging, as it has predominantly involved either imprecise subjective methods (manual muscle testing) or technically complex procedures (electromyography). The current study is the first to use RUSI to quantify infraspinatus muscle function in patients with SIS. Measurements of infraspinatus muscle thickness were found to be highly reliable, both within the same examiner and between different examiners. Additionally, RUSI measurements of infraspinatus muscle thickness were different in resting and contracted conditions and between the symptomatic and asymptomatic shoulders of individuals with unilateral SIS.
The reliability estimates in the current study were very similar to those found using RUSI to measure abdominal and lumbar muscle thickness across multiple studies (ICC greater than 0.90) for both intra‐rater and inter‐rater reliability.13 Reliability estimates were also similar to the studies that have investigated RUSI measures of thickness of the trapezius muscle.21,23 As expected, intra‐rater reliability was generally higher than inter‐rater reliability, especially when such estimates were based on a mean of three measurements. Additionally, the reliability estimates of percent thickness change calculations were substantially lower than those derived from thickness measures.25,28 As previously hypothesized, the reason for this decrement of reliability likely has to do with the compounding of measurement error when performing calculations based on both resting and contracted thicknesses.28
The finding that RUSI measurements of infraspinatus muscle thickness were able to distinguish between resting and contracted conditions and between the symptomatic and asymptomatic shoulders helps establish a low level of initial validity of such measurements. Discriminative validity (also called extreme groups27 or known groups method26) is considered a form of construct validity that is supported when measures can discriminate between individuals or conditions that are thought to be different on a relevant construct.26 Construct validity of RUSI measures of trunk muscle function has been supported by differences based on pain‐related conditions (e.g. different in patients with back pain vs. asymptomatics29), posture or activity (e.g. different between slouched sitting and erect standing30), and anthropometric conditions (e.g. different in men vs. women31).17 Criterion validity of RUSI measures has been supported in other muscles by studies comparing them to criterion standard measures such as EMG or MRI.17,22 Two previous studies have preliminarily investigated the RUSI of the infraspinatus muscle. Jull‐Kristensen et al20 compared resting infraspinatus muscle thickness as measured by RUSI and MRI and found an 8% mean difference between the measures in asymptomatic individuals. Of note, the mean infraspinatus muscle thickness was very similar to the resting thickness found in the current study (18 mm vs. 16 mm). Boehm et al19 imaged the infraspinatus muscle during contraction in patients with varying shoulder pathologies. Although they didn’t quantify muscle thickness, they subjectively assessed the contraction patterns and reported good agreement between different raters’ assessments. The only other study to compare the muscle thickness measures between shoulder of patients with unilateral shoulder pain did so of the lower, middle, and upper trapezius.24 Unlike the current study, they did not find any differences between the symptomatic and asymptomatic shoulders nor between people with and without shoulder pain.
Limitations
Although the current study found clear differences in infraspinatus muscle thickness between resting and contracted conditions, the differences between asymptomatic and symptomatic shoulders were very small and within estimates of measurement error. Therefore, while one can conclude that such differences are not solely due to sampling error, they may be attributable to measurement error. Moreover, since only one other study to date has quantified infraspinatus muscle thickness using RUSI,20 there is currently no data to determine what degree of “thickening” constitutes clinically relevant change. Additionally, this study did not document whether participants experienced pain with active infraspinatus contraction during the measurements. Pain during muscle contraction may have caused compensatory muscle action (e.g. more teres minor contraction) in order to perform the described task, which may have affected results. However, the methods were designed to minimize variance in volitional muscular contractions with the standardized contraction pressure measured by the pressure cuff. Each participant was able to externally rotate their shoulder to meet the standardized pressure.
Future research should compare measures of infraspinatus muscle activation measured by EMG with changes in thickness measured by RUSI. Future research should also assess the clinical responsiveness of RUSI measures of infraspinatus muscle thickness longitudinally during a course of rehabilitation aimed at improving muscle function.
Conclusion
RUSI measurements of infraspinatus muscle thickness appear to be highly reliable, both within the same examiner and between different examiners, in patients with SIS. Furthermore, in the current study, RUSI measurements of infraspinatus muscle thickness were different in resting and contracted conditions and between the symptomatic and asymptomatic shoulders. Although the differences in infraspinatus muscle thickness between resting and contracted conditions were fairly large, the differences between asymptomatic and symptomatic shoulders were very small and within estimates of measurement error. If validated in future research, RUSI may allow for more objective quantifications of muscle impairments and be a useful adjunct to the physical examination in patients with SIS.
REFERENCES
- 1.Feleus A Bierma‐Zeinstra S Miedema H Bernsen R Verhaar J Koes B Incidence of non‐traumatic complaints of arm, neck and shoulder in general practice. Man Ther. 2008;13(5):426‐433. [DOI] [PubMed] [Google Scholar]
- 2.Koester M George M Kuhn J Shoulder impingement syndrome. Am J Med. 2005;118(5):452‐455 doi:10.1016/j.amjmed.2005.01.040. [DOI] [PubMed] [Google Scholar]
- 3.Escamilla R Hooks T Wilk K Optimal management of shoulder impingement syndrome. Open Access J Sports Med. 2014:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Page P Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther. 2011;6(1):51. [PMC free article] [PubMed] [Google Scholar]
- 5.Park H Yokota A Gill H El Rassi G McFarland E Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J B J S (Am). 2005;87(7):1446‐1455. [DOI] [PubMed] [Google Scholar]
- 6.Deutsch A Altchek DW Schwartz E Otis JC Warren RF Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5(3):186‐193. [DOI] [PubMed] [Google Scholar]
- 7.Royer PJ Kane EJ Parks KE, et al. Fluoroscopic assessment of rotator cuff fatigue on glenohumeral arthrokinematics in shoulder impingement syndrome. J Shoulder Elbow Surg. 2009;18(6):968‐975. [DOI] [PubMed] [Google Scholar]
- 8.Clisby EF Bitter NL Sandow MJ Jones MA Magarey ME Jaberzadeh S Relative contributions of the infraspinatus and deltoid during external rotation in patients with symptomatic subacromial impingement. J Shoulder Elbow Surg. 2008;17(1):S87‐S92. [DOI] [PubMed] [Google Scholar]
- 9.Myers JB Hwang J‐H Pasquale MR Blackburn JT Lephart SM Rotator cuff coactivation ratios in participants with subacromial impingement syndrome. J Sci Med Sport. 2009;12(6):603‐608. [DOI] [PubMed] [Google Scholar]
- 10.Talbert RJ Michaud LJ Mehlman CT, et al. EMG and MRI are independently related to shoulder external rotation function in neonatal brachial plexus palsy. J Pediatr Orthop. 2011;31(2):194‐204. [DOI] [PubMed] [Google Scholar]
- 11.Teyhen D Koppenhaver S Rehabilitative ultrasound imaging. J Physiother. 2011;57(3):196. [DOI] [PubMed] [Google Scholar]
- 12.Teyhen DS Rehabilitative ultrasound imaging symposium San Antonio, TX, May 8‐10, 2006. J Orthop Sports Phys Ther. 2006;36(8):A1‐A3. [PubMed] [Google Scholar]
- 13.Hebert J Koppenhaver S Parent E Fritz J A systematic review of the reliability of rehabilitative ultrasound imaging for the quantitative assessment of the abdominal and lumbar trunk muscles. Spine Phila Pa 1976. 2009;34(23):E848‐E856. [DOI] [PubMed] [Google Scholar]
- 14.Hides J Belavy D Cassar L Williams M Wilson S Richardson C Altered response of the anterolateral abdominal muscles to simulated weight‐bearing in subjects with low back pain. Eur Spine J. 2009;18(3):410‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hides J Stanton W McMahon S Sims K Richardson C Effect of stabilization training on multifidus muscle cross‐sectional area among young elite cricketers with low back pain. J Orthop Sports Phys Ther. 2008;38(3):101‐108. [DOI] [PubMed] [Google Scholar]
- 16.Kiesel K Underwood F Matacolla C Nitz A Malone T A comparison of select trunk muscle thickness change between subjects with low back pain classified in the treatment‐based classification system and asymptomatic controls. J Orthop Sports Phys Ther. 2007;37(10):596‐607. [DOI] [PubMed] [Google Scholar]
- 17.Koppenhaver S Hebert J Parent E Fritz J Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub‐maximal contractions: a systematic review. Aust J Physiother. 2009;55(3):153‐169. [DOI] [PubMed] [Google Scholar]
- 18.Bentman S O’Sullivan C Stokes M Thickness of the middle trapezius muscle measured by rehabilitative ultrasound imaging: description of the technique and reliability study. Clin Physiol Funct Imaging. 2010;30(6):426‐431. [DOI] [PubMed] [Google Scholar]
- 19.Boehm T Kirschner S Mueller T Sauer U Gohlke F Dynamic ultrasonography of rotator cuff muscles. J Clin Ultrasound. 2005;33(5):207‐213. [DOI] [PubMed] [Google Scholar]
- 20.Juul‐Kristensen B Bojsen‐Moller F Holst E Ekdahl C Comparison of muscle sizes and moment arms of two rotator cuff muscles measured by ultrasonography and magnetic resonance imaging. Eur J Ultrasound. 2000;11(3):161‐173. [DOI] [PubMed] [Google Scholar]
- 21.O’Sullivan C Bentman S Bennett K Stokes M Rehabilitative ultrasound imaging of the lower trapezius muscle: technical description and reliability. J Orthop Sports Phys Ther. 2007;37(10):620‐626. [DOI] [PubMed] [Google Scholar]
- 22.O’Sullivan C Meaney J Boyle G Gormley J Stokes M The validity of Rehabilitative Ultrasound Imaging for measurement of trapezius muscle thickness. Man Ther. 2009;14(5):572‐578. [DOI] [PubMed] [Google Scholar]
- 23.Bentman S O’Sullivan C Stokes M Thickness of the middle trapezius muscle measured by rehabilitative ultrasound imaging: description of the technique and reliability study: Ultrasound imaging of middle trapezius muscle. Clin Physiol Funct Imaging. 2010;30(6):426‐431. [DOI] [PubMed] [Google Scholar]
- 24.O’Sullivan C McCarthy Persson U Blake C Stokes M Rehabilitative ultrasound measurement of trapezius muscle contractile states in people with mild shoulder pain. Man Ther. 2012. [DOI] [PubMed] [Google Scholar]
- 25.Koppenhaver S Parent E Teyhen D Hebert J Fritz J The effect of averaging multiple trials on measurement error during ultrasound imaging of transversus abdominis and lumbar multifidus muscles in individuals with low back pain. J Orthop Sports Phys Ther. 2009;39(8):604‐611. [DOI] [PubMed] [Google Scholar]
- 26.Portney LG Watkins MP Foundations of Clinical Research: Applications to Practice (3rd Edition). Upper Saddle River, NJ: Pearson Prentice Hall; 2008. [Google Scholar]
- 27.Streiner D Norman G Health Measurement Scales: A Practical Guide to Their Development and Use. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 28.Koppenhaver S Hebert J Fritz J Parent E Teyhen D Magel J Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch Phys Med Rehabil. 2009;90(1):87‐94. [DOI] [PubMed] [Google Scholar]
- 29.Ferreira PH Ferreira ML Hodges PW Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine. 2004;29(22):2560‐2566. [DOI] [PubMed] [Google Scholar]
- 30.Reeve A Dilley A Effects of posture on the thickness of transversus abdominis in pain‐free subjects. Man Ther. 2009. [DOI] [PubMed] [Google Scholar]
- 31.Rankin G Stokes M Newham DJ Abdominal muscle size and symmetry in normal subjects. Muscle Nerve. 2006;34(3):320‐326. [DOI] [PubMed] [Google Scholar]