Abstract
Purpose
The aim of this study is to demonstrate the validity and responsiveness of the Jebsen-Taylor Hand Function Test (JTT) in measuring hand function in patients undergoing hand surgery.
Methods
A prospective cohort of patients with the following conditions: (1) rheumatoid arthritis (n=37), (2) osteoarthritis (n=10), (3) carpal tunnel syndrome (n=18), and (4) distal radius fracture (n=46), were evaluated preoperatively and at 9 – 12 months follow-up. The JTT and Michigan Hand Outcomes Questionnaire (MHQ) were administered. Correlation and receiver operating characteristic (ROC) analysis were performed to evaluate the validity of the JTT as a measure of disability. Effect size and standardized response means (SRM) were calculated to determine responsiveness.
Results
Correlation studies revealed poor correlation of the JTT to MHQ total scores and subsets that relate to hand function. Patients with high MHQ scores generally perform well on the JTT; however, patients with good JTT scores do not necessarily have high MHQ scores. ROC curves for each condition show that the change in JTT total score had poor ability to discriminate between high and low MHQ score subjects, with area under the curve (AUC) of 0.52 – 0.66 for each of the conditions. Effect size and SRM for all states showed greater responsiveness with the MHQ for each condition when compared to JTT.
Conclusions
We found poor correlation between the change in JTT and absolute JTT scores after surgery when compared to change in MHQ and absolute MHQ scores. In addition, the JTT has poor discriminant validity based on the MHQ as a reference. This study showed that the time to complete activities does not correlate well with patient reported outcomes. We conclude that the JTT should not be used as a measure of disability or clinical change after surgical intervention.
Type of Study
Prospective cohort
Level of Evidence
Level III
Keywords: hand surgery outcomes, Jebsen-Taylor Test (JTT), Michigan Hand Outcomes Questionnaire (MHQ), responsiveness, validity
In the current era of the outcomes movement, many more tools are available to assess outcomes in the field of hand surgery (1). One such outcomes tool is the Jebsen-Taylor Hand Function Test (JTT) (2), which was proposed in 1969 to assess impairment and the effectiveness of treatment for hand conditions. This test was created to provide quantitative measurements of standardized tasks to assess broad aspects of hand function commonly used in everyday activities. Norms for age and sex were developed (2). Seven subsets of the test represent a broad spectrum of hand function, which includes writing, turning over 3x5 inch cards (to simulate page turning), picking up small common objects, simulated feeding, stacking checkers, picking up large light objects, and picking up large heavy objects. To evaluate patient performance, each subset is timed and can be compared to the established norms. The JTT has been widely used in the clinical and research setting. By conducting a Medline literature search of all articles with “Jebsen” in the title or abstract, we found more than 135 papers published using this test as one of the outcomes tools. Nearly half of these papers have been published in the last three years, signaling the increasing application of this test. These papers include conditions such as stroke, spinal cord injury, cerebral palsy, multiple sclerosis, hand and wrist fractures, carpal tunnel syndrome, osteoarthritis, and rheumatoid arthritis (3-11).
Standardized outcomes instruments must demonstrate reliability, validity, and responsiveness to detect change after an intervention (12). Reliability is the ability to obtain consistent measurements at different points in time given similar patient characteristics. Reliability is often tested by test-retest analysis. Validity is the ability of an instrument to measure what is intended. Validity can be measured in a variety of quantitative and qualitative manners. One method to establish validity is to compare a new instrument to a “gold standard” or previously established instrument that has been validated to measure a specific characteristic. Responsiveness is the ability of a test to detect clinical change. Responsiveness is typically measured by effect size or standardized response mean. These calculations are described in detail in the methods section. It is important that outcomes measures are reliable, give results that evaluate what is intended, and are able to detect clinically significant change. Instruments that are easy to use and administer are also ideal. Jebsen and Taylor’s original article (2) and several subsequent studies have demonstrated the reliability of this instrument (5, 10, 13). However, despite its widespread use, we were unable to find studies beyond the original article to affirm the validity of the JTT as a measure of hand function when performing the aforementioned Medline literature search.
Hand function tests vary in the amount of time and clinical support staff needed for their administration. In our experience, considerable effort is needed to administer the JTT. Patients spend on average 15 minutes to complete the test, while staff members must also spend an equivalent amount of time with the patient to administer the test. In a busy hand surgery practice, using the test as a regular tool to assess hand function can be quite time and resource consuming. Given the effort and money that is invested in the administration of the JTT, it is important that clinicians trust this instrument to contribute valid clinical data.
The specific aims of this study are to 1) evaluate the validity of the JTT as a measure of disability and 2) evaluate the responsiveness of the JTT in measuring hand function in patients undergoing hand surgery for a variety of conditions, including rheumatoid arthritis, osteoarthritis, distal radius fracture, and carpal tunnel syndrome. We aim to determine the validity of using this test to assess disability because the JTT is often used in the literature as a measure of the ability of patients to perform activities of daily living (ADLs) (2, 5, 14-16). In addition, we will determine whether the JTT is a responsive measure of global hand function in patients with varying degree of disability resulting from a variety of common diseases.
MATERIALS AND METHODS
Study Design
Data were collected from a prospective cohort of patients (17-20) with the following conditions: (1) rheumatoid arthritis (RA) (2) osteoarthritis (3) carpal tunnel syndrome and (4) distal radius fracture, to measure the validity and responsiveness of the JTT. Patients were evaluated preoperatively (except in the case of patients with distal radius fractures) and at follow-up period up to one-year postoperatively. Sixty-seven patients with rheumatoid arthritis were evaluated preoperatively before undergoing silicone metacarpophalangeal arthroplasty. Forty patients were evaluated at one year postoperatively. Twenty-five patients with thumb carpometacarpal (CMC) osteoarthritis were evaluated at baseline before undergoing trapeziectomy with abductor pollicis longus suspension arthroplasty. Eleven patients were evaluated at one year follow-up. Ninety-three patients with carpal tunnel syndrome were evaluated at baseline before carpal tunnel release. Fifty-four patients were evaluated at mean follow-up of 9 months with a range of 5 to 30 months. One hundred eight patients with distal radius fractures were evaluated at 3 months status post injury. Sixty-five patients were re-evaluated at one year status post open reduction and internal fixation. The goal of treatment for all conditions was to treat the underlying pathology and improve hand function.
The JTT and Michigan Hand Outcomes Questionnaire (MHQ) domains were measured preoperatively and at the final follow-up period as part of the research protocol for our outcomes studies. Patients were excluded from analysis if they did not complete both the MHQ and JTT and if they were not available at both baseline and follow-up evaluations. Thirty-seven rheumatoid arthritis patients, 46 distal radius patients, 18 carpal tunnel patients, and 10 thumb osteoarthritis patients remained for analysis.
The MHQ is a 37-question, hand-specific outcomes instrument (21) with six domains: (1) overall hand function, (2) activities of daily living (ADL), (3) pain, (4) work performance, (5) aesthetics, and (6) patient satisfaction. Each domain except for work is assessed separately on each hand, with a total score reported for each hand. The MHQ is self-administered and takes approximately 15 minutes to complete. The MHQ has shown to be a reliable, valid, and responsive instrument to measure outcomes of hand and upper limb conditions (22-26) and has been used concomitantly with the JTT in the four clinical studies outlined in this project. Several hand specific patient-rated outcomes instruments are available for use. The MHQ was chosen for its unique ability to perform analyses based on overall hand function as well as based on separate domains related to ability to perform activities (ADL, work performance, and hand function subsets). Each domain is assigned a score, thus we are able to determine the effect that domains have on overall hand function and its relation to the JTT. Due to the ability of the test to score each hand individually, the affected hand that underwent surgery is evaluated separate from the contralateral hand. This allows us to better determine the effect of the intervention on hand function. Similarly, all JTT subsets except for writing were evaluated separately for each hand in all patients.
Data Analysis
Data analysis was performed using STATA Data Analysis and Statistical Software (STATA, version 10, StataCorp, College Station, TX). All data analysis were performed on each cohort of patients (carpal tunnel, rheumatoid arthritis, thumb osteoarthritis, distal radius fracture) separately. Data from the hand that was operated on was assessed separately from the contralateral hand, with the data presented in this study being the affected side only. Paired t-tests were performed to detect significance of change of the JTT and the MHQ scores from baseline to the final follow-up period. Construct validity of the JTT as a measure of disability was evaluated by generating scatterplots and using Pearson’s correlation of JTT scores compared to the MHQ domains. In addition to comparing JTT to the total MHQ score, the JTT score was evaluated against MHQ domains of function, ADLs, and work performance, as the test is frequently used as a measure of patient’s ability to perform ADLs.
Analyses with receiver operating characteristic (ROC) curves were performed to compare the ability of the JTT score to discriminate among patients who rate hand function as being good or poor as assessed by the MHQ. ROC curves measure the ability of a test to predict the outcome of a “reference standard” comparison test that has a dichotomous variable. In this case, the ROC curves are used to determine the ability of the JTT to discriminate against positive and negative patient outcomes using the MHQ as the reference comparison. For this study, positive outcome or normal state of function using MHQ was judged having a score >75. Whereas a negative outcome or abnormal state of function was judged as having a score ≤75. ROC curves are generated by varying the cutoff point of a test that makes an outcome positive or negative. The sensitivity and 1-specificity (false positive) are plotted based on the predicted outcome for that given cutoff point compared to the reference standard. For example, a cutoff point of 30 seconds for the JTT will set an abnormal state as having a score ≥30 seconds and normal state as having a score <30 seconds. The accuracy of predicting normal and abnormal states is compared to the accuracy of the MHQ in determining normal and abnormal state based on having a score greater than or less than 75. A true positives and false positive are determined and represent one point on the ROC curve. The cutoff point, which determines positive and negative outcomes are varied across the entire spectrum of possible JTT scores and this generates a point for every cutoff, which in turn creates the entire ROC curve. The curve has the ability to tell what JTT cutoff points have ideal sensitivity and specificity. ROC curves have a corresponding area under the curve (AUC) which represents the probability that the JTT will rank a randomly chosen positive MHQ instance higher than a randomly chosen negative MHQ instance. The higher the AUC, the better the test is at predicting positive and negative outcomes based on the reference standard. For example, for a curve to have an AUC of 1.0, the curve must have 100% sensitivity and 0% false positives at each point, thus an ideal test. An AUC of 0.5 means that the test has a 50% probability in predicting positive and negative outcomes when compared to the reference standard. This is the same as random guessing and would be a poor test. In general, tests with AUC of 0.75 or greater are considered to have useful discriminative ability (27).
ROC curves were generated to determine whether change in JTT scores had the ability to discriminate among patients that had significant change in MHQ scores after surgery; likewise, ROC curves were generated to compare the ability of absolute JTT scores to distinguish among patients with abnormal absolute MHQ scores preoperatively and postoperatively. Specifically, ROC curves were plotted for each condition to determine whether JTT change scores could discriminate against patients that had greater than a 20-point change in the MHQ score. ROC curves were also plotted for each condition to determine whether the absolute JTT score could discriminate against patients that had MHQ scores >75 (normal state).
Standardized response mean (SRM) and effect size are measures of responsiveness to clinical change as a result of treatment. Standardized response mean is calculated as the mean change divided by the standard deviation of the change scores. Alternatively, effect size is calculated as mean change divided by the standard deviation of the mean at baseline. SRM and effect size were calculated to evaluate the responsiveness of JTT and MHQ to clinical change at final follow-up compared to baseline for all four clinical conditions.
RESULTS
Total JTT and MHQ and their respective subsets are reported for the affected hand in Table 1. If patients had bilateral disease, the score is reported for the hand in which the patient underwent surgery. Table 1 shows that patients with each of the four conditions saw a statistically significant change in mean total MHQ score postoperatively. Patients with RA, osteoarthritis of the thumb basilar joint, and carpal tunnel syndrome experienced similar mean change after surgery of approximately 16 – 20 points. Patients with distal radius fractures had a mean change of 11 points from 3 months after surgery to 1 year postoperatively. Patients with RA and distal radius fractures saw statistically significant change in total JTT scores at 1 year follow-up, whereas no statistically significant change in JTT score was seen postoperatively for patients after carpal tunnel release and treatment of thumb osteoarthritis. Thus, patients that have improvement in MHQ score after surgery do not always have a similar improvement in JTT.
Table 1.
Comparison of mean Michigan Hand Outcomes Questionnaire (MHQ) and Jebsen-Taylor Test (JTT) scores at baseline and final follow-up
| MHQ | JTT | ||||||
|---|---|---|---|---|---|---|---|
| n | MHQ | SD | P | JTT (seconds) |
SD | P | |
| RA | |||||||
| Baseline | 37 | 41 | 19 | 51 | 15 | ||
| 1 year | 37 | 61 | 22 | <0.0001 | 44 | 16 | 0.005 |
| Distal Radius | |||||||
| 3 months | 46 | 79 | 15 | 33 | 8 | ||
| 1 year | 46 | 90 | 13 | <0.0001 | 30 | 7 | 0.0006 |
| Carpal Tunnel | |||||||
| Baseline | 18 | 51 | 19 | 39 | 14 | ||
| Postop* | 18 | 67 | 23 | <0.0008 | 40 | 33 | 0.87 |
| CMC Arthritis | |||||||
| Baseline | 10 | 48 | 16 | 45 | 18 | ||
| 1 year | 10 | 69 | 20 | 0.02 | 33 | 4 | 0.07 |
RA = rheumatoid arthritis; CMC = carpometacarpal; SD = standard deviation
post-operative follow-up ranges average 9 months, range 5-30 months
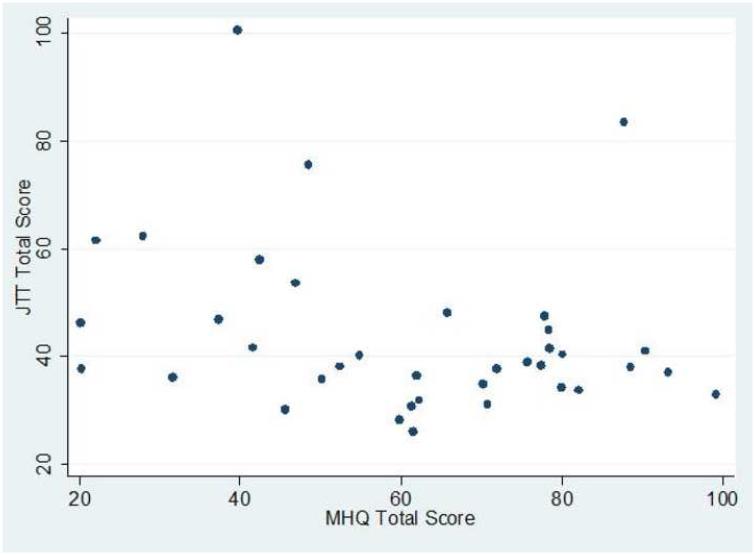
Comparison of the change in total MHQ and JTT scores postoperatively show poor correlation between the two studies as demonstrated in Table 2, with Pearson’s correlation coefficient of 0.19 in patients with RA, 0.04 in patients with osteoarthritis, and 0.36 in patients with distal radius fractures. There is moderate correlation of change in total MHQ and JTT scores for patients with carpal tunnel syndrome, with a correlation coefficient of 0.59. Correlation between absolute scores at final follow-up is also poor in patients with RA, osteoarthritis, and distal radius fractures. Again, patients with carpal tunnel syndrome have moderate correlation in absolute MHQ and JTT scores. Comparing JTT scores to MHQ subsets that assess function, ADLs, and work, there is no improvement in the measure of correlation coefficients. Similarly, correlation to the patient satisfaction subset of the MHQ is also poor in patients with RA, osteoarthritis, and distal radius fractures (range correlation coefficient 0.10 – 0.30), and has moderate correlation in patients with carpal tunnel syndrome (correlation coefficient 0.56). Scatterplots were evaluated to further evaluate the relationship between the two hand function tests to provide qualitative rationale of their poor correlation. Closer examination of the scatterplots of absolute MHQ and JTT scores, as seen in Figure 1, show that at higher ends of the scale (MHQ >80), JTT score is in or near normal range of established norms, which is approximately 16.8 – 51 seconds depending on dominance of hand and age group tested (2). This relationship is seen similarly within all of the conditions examined. Figure 1 also shows that data within JTT scores in the range of established norms have a large span of MHQ scores, with some patients having very poor MHQ scores, which is similarly seen in all four patient conditions. A similar phenomenon can be seen comparing total JTT scores to individual subsets of the MHQ questionnaire. However, Figure 1 also demonstrates that patients with abnormal JTT (>50) more reliably have poor MHQ scores. The correlation studies demonstrate that many of the conditions showed poor correlation to the MHQ total scores and subsets that relate to ability to use the hand (work, function, ADL). Patients with high MHQ scores generally perform well on the JTT, and patients with poor JTT generally scored poorly on MHQ. However, patients with good JTT scores have quite a variety of MHQ scores with many having very low scores.
Table 2.
Correlation of Jebsen-Taylor Test (JTT) score to Michigan Hand Outcomes Questionnaire (MHQ) total score and MHQ subsets
| Correlation | ||||||
|---|---|---|---|---|---|---|
| JTT/MHQ Change |
JTT/MHQ Total |
JTT/Function | JTT/ADL | JTT/Work | JTT/Satisf | |
| RA | ||||||
| Baseline | −0.43 | −0.50 | −0.50 | −0.47 | −0.39 | |
| 1 year | 0.19 | −0.27 | −0.27 | −0.41 | −0.18 | −0.10 |
| Distal Radius | ||||||
| 3 months | −0.38 | −0.27 | −0.25 | −0.49 | −0.20 | |
| 12 months | 0.36 | −0.30 | −0.13 | −0.22 | −0.29 | −0.30 |
| Carpal Tunnel | ||||||
| Baseline | −0.32 | −0.43 | −0.51 | −0.03 | −0.09 | |
| Postop* | 0.59 | −0.63 | −0.69 | −0.68 | −0.38 | −0.56 |
| CMC Arthritis | ||||||
| Baseline | −0.66 | −0.62 | −0.74 | −0.61 | −0.60 | |
| 12 months | 0.04 | 0.20 | 0.18 | 0.13 | 0.11 | 0.19 |
Satisf = MHQ satisfaction domain; ADL = MHQ activities of daily living domain; RA = rheumatoid arthritis; CMC = carpometacarpal
post-operative follow-up ranges average 9 months, range 5-30 months
Figure 1.
Scatterplot of Jebsen-Taylor Test (JTT) versus Michigan Hand Outcomes Questionnaire (MHQ) score in RA patients at 1 year follow-up
ROC analysis shows that the change in JTT score and absolute JTT score had poor ability to differentiate patients with positive and negative outcomes as measured by the MHQ. Table 3 demonstrates ROC curves that test discriminate ability of the change in JTT total score have area under the curve (AUC) of 0.52 – 0.66 for each of the four conditions. Likewise Table 4 shows poor discriminate ability of the absolute JTT score to detect patients with MHQ >75 as having a positive outcome in all conditions except distal radius fractures. Patients at follow-up with RA, osteoarthritis, and carpal tunnel syndrome had AUC values of 0.48, 0, and 0.65 respectively, with 95% confidence intervals that show no statistically significance difference when compared to random guessing. The distal radius follow-up group AUC was 0.76, which had a statistically significant difference when compared to random guessing. The ROC analyses show that the JTT cannot reliably predict positive patient-reported outcome as assessed by the MHQ.
Table 3.
ROC (AUC) analysis for Jebsen-Taylor Test (JTT) discriminant ability in patients with Michigan Hand Outcomes Questionnaire (MHQ) change >20
| ROC Analysis MHQ Change >20 | |||
|---|---|---|---|
| n | AUC | 95% CI | |
| RA | |||
| 1 year | 37 | 0.52 | 0.32 - 0.71 |
| Distal Radius | |||
| 1 year | 46 | 0.59 | 0.38 - 0.81 |
| Carpal Tunnel | |||
| 9 months | 18 | 0.66 | 0.40 - 0.93 |
| CMC Arthritis | |||
| 1 year | 10 | 0.58 | 0.17 - 0.99 |
ROC = receiver operating characteristic; AUC = area under the curve; CI = confidence interval; RA = rheumatoid arthritis; CMC = carpometacarpal
post-operative follow-up ranges average 9 months, range 5-30 months
Table 4.
ROC (AUC) analysis for Jebsen-Taylor Test (JTT) discriminant ability in patients with Michigan Hand Outcomes Questionnaire (MHQ) score >75
| ROC Analysis MHQ >75 | |||
|---|---|---|---|
| n | AUC | 95% CI | |
| RA | |||
| Baseline | 37 | 0.78 | 0.49 - 1.0 |
| 1 year | 37 | 0.48 | 0.29 - 0.67 |
| Distal Radius | |||
| 3 months | 46 | 0.71 | 0.54 - 0.87 |
| 12 months | 46 | 0.76 | 0.62 - 0.91 |
| Carpal Tunnel | |||
| Baseline | 18 | 0.56 | 0.24 - 0.89 |
| Postop* | 18 | 0.65 | 0.38 - 0.93 |
| CMC Arthritis | |||
| Baseline | 21 | ** | ** |
| 12 months | 10 | 0.00 | 0 - 0.63 |
ROC = receiver operating characteristic; AUC = area under the curve; CI = confidence interval; RA = rheumatoid arthritis; CMC = carpometacarpal
post-operative follow-up ranges average 9 months, range 5-30 months
unable to perform the analysis because there is no area under the curve
Table 5 demonstrates greater effect size and standardized response means with MHQ for each condition when compared to JTT for all conditions, indicating less ability of the JTT to detect clinical change compared to the MHQ.
Table 5.
Effect size (ES) and standardized response mean (SRM) at final follow-up for Michigan Hand Outcomes Questionnaire (MHQ) and Jebsen-Taylor Test (JTT)
| MHQ | JTT | |||
|---|---|---|---|---|
| ES | SRM | ES | SRM | |
| RA | 1.05 | 1.07 | 0.47 | 0.49 |
| Distal Radius | 0.74 | 0.91 | 0.35 | 0.54 |
| Carpal Tunnel | 0.84 | 0.96 | 0.05 | 0.04 |
| CMC Arthritis | 1.30 | 0.93 | 0.67 | 0.66 |
RA = rheumatoid arthritis; CMC = carpometacarpal
Because of the loss of a fraction of patients at follow-up, our analysis includes only patients at baseline and follow-up who were able to complete both tests and who were available at both time points. However, we had concern that excluding some patients may have bias on the overall result. Thus, we repeated the data analysis using all available data at baseline and follow-up. This analysis included some patients who were able to only complete one of the tests and included some patients who may have been lost to follow-up. These patients were originally excluded from the analysis. We found that the overall results are similar. Both the JTT and the MHQ have the same statistical significance at baseline and follow-up, with the change of MHQ after surgery being statistically significant for all conditions and the change in JTT being statistically significant for RA and distal radius fracture patients only. Correlation coefficients were similar, with poor correlation coefficients between the JTT and MHQ with the exception of the carpal tunnel cohort, which had moderate correlation. ROC analysis for the change in JTT was identical, as the analysis is only performed on patients that have scores obtained at both points in time. ROC analysis for the absolute JTT score showed that only the distal radius cohort had area under the curve (AUC) results that had 95% confidence intervals outside the range of random guessing (0.5). This was similar to the results obtained with the prior analysis. Effect size and standardized response means also continue to be greater for the MHQ for all patient cohorts compared to the JTT with the reanalysis.
DISCUSSION
Hand function can be evaluated with respect to impairment, which would include abnormalities in measures such as range of motion, grip strength, and other performance tests. Alternatively, hand function can also be represented by patient-rated disability, or limitations in physical activities, such as activities of daily living. The MHQ is a measure of disability. We chose to use the MHQ as opposed to other hand-specific measures of disability, such as the Disabilities of the Arm, Shoulder, and Hand (DASH) Questionnaire for several reasons (28). We used the MHQ as a measure of disability because of its ability to assess each hand separately. This allows one to determine whether the injured hand and dominance of the hand has an overall effect on outcomes. We are also able to assess the effect that patient satisfaction, pain, work, function, ADLs, and aesthetics each have on overall hand related outcomes.
The JTT has been utilized in the literature as a measure of both impairment and disability. While the JTT has been shown to be a valid measure of impairment in some conditions (6, 29, 30), other studies have demonstrated poor correlation between the JTT and hand function measures obtained from patient-centered questionnaires (5, 19, 24, 31). In the assessment of outcomes, it is important to be aware of the specific disability or impairment that tools are intended to evaluate and whether what is being measured is important to patients and physicians. Despite multiple studies that have demonstrated reliability of the JTT, little has been done to evaluate its validity as a measure of ADLs and hand function, while some studies would suggest that it is poorly responsive to clinical change (32, 33). Similar conclusions were found in this study. We found that correlation coefficients comparing total JTT scores to total MHQ scores and individual subsets relating to function are poor among patients with several different hand conditions. The JTT had poor ability to discriminate among patients reporting high functioning MHQ scores (>75) and large change in MHQ scores (>20). Lastly, we found that the JTT had less responsiveness to change compared to the patient-centered MHQ questionnaire.
The JTT is a performance-based quantitative evaluation based on patients’ ability to perform seven tests, measured in time. Time is used as a measure of dexterity and efficiency of movement; however, this study has shown that time to complete activities does not relate well to patient reported outcomes. JTT not only correlates poorly with MHQ, but also correlates poorly with other measures of patient-reported outcomes (5, 19, 24, 31, 33-36). A study by Bovend’Eerdt et al. (5) compared the JTT against the nine-hole peg test, also a timed measure of hand function, which showed excellent correlation between the two timed tests, but no significant correlation for the two timed tests and the University of Maryland Arm Questionnaire for Stroke (a patient-reported outcome questionnaire). This study gives further evidence of poor correlation of a timed hand function test with patient-reported outcomes.
We found that the JTT does not relate well to patient satisfaction or their perception of their hand function. In other words, the validity of the JTT in measuring disability is uncertain. Patients with JTT scores within the range of established norms have a wide variety of MHQ scores ranging from high to poor functioning levels. Patient reported questionnaires are better at identifying poor hand function and are more sensitive to change after treatment. It is possible that performance tests that focus on the quality of completing a series of tasks may be better than the time it takes to complete the tasks. The speed of performing tasks is likely of varying importance to individual patients, which may explain some of the variability of scores when comparing the JTT to the MHQ. Some patients may complete an activity within range of established norms, but may be bothered by pain or feeling of clumsiness of movement. Other patients may not care about the time it takes to complete an activity, but whether or not they are able to complete the activity at all. Discordance between the two tests may also relate to the fact that the MHQ also includes characteristics such as pain, satisfaction, and aesthetics that are likely not captured in the JTT. In addition disagreement can be related to the possible lesser sensitivity to change of the JTT. Thus, for application in clinical practice, the JTT is not practical because it is able to identify some, but not all patients who report poor hand function.
When using hand function tests in research or routine clinical use, it is important for clinicians to know precisely what the tool is measuring, and that it is reliable, valid, and responsive. The JTT has been used in the literature as a measure of impairment and disability. We found that the JTT does not correlate well to patient-reported outcomes of disability, including patient satisfaction and domains that relate to work, function, and activities of daily living as assed by the MHQ. Similarly the JTT is not as sensitive as the patient-reported responses obtained from the MHQ in detecting change after hand surgery. This study demonstrates discordance of the JTT and MHQ patient-reported outcomes for four conditions, which strengthens our conclusion that the JTT is a poor indicator of patient improvement after surgery. Based on our results, we conclude that clinicians should not use the JTT alone to assess efficacy of treatments in hand surgery nor to evaluate ability of patients to perform activities of daily living.
Acknowledgments
Supported in part by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR047328) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
BIBLIOGRAPHY
- 1.Chung KC, Burns PB, Davis Sears E. Outcomes research in hand surgery: where have we been and where should we go? J Hand Surg [Am] 2006;31:1373–1379. doi: 10.1016/j.jhsa.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 2.Jebsen RH, Taylor N, Trieschmann RB, Trotter MJ, Howard LA. An objective and standardized test of hand function. Arch Phys Med Rehabil. 1969;50:311–319. [PubMed] [Google Scholar]
- 3.Beekhuizen KS, Field-Fote EC. Massed practice versus massed practice with stimulation: effects on upper extremity function and cortical plasticity in individuals with incomplete cervical spinal cord injury. Neurorehabilitation & Neural Repair. 2005;19:33–45. doi: 10.1177/1545968305274517. [DOI] [PubMed] [Google Scholar]
- 4.Alon G, Sunnerhagen KS, Geurts ACH, Ohry A. A home-based, self-administered stimulation program to improve selected hand functions of chronic stroke. Neurorehabilitation. 2003;18:215–225. [PubMed] [Google Scholar]
- 5.Bovend'Eerdt TJH, Dawes H, Johansen-Berg H, Wade DT. Evaluation of the Modified Jebsen Test of Hand Function and the University of Maryland Arm Questionnaire for Stroke. Clin Rehabil. 2004;18:195–202. doi: 10.1191/0269215504cr722oa. [DOI] [PubMed] [Google Scholar]
- 6.Charles JR, Wolf SL, Schneider JA, Gordon AM. Efficacy of a child-friendly form of constraint-induced movement therapy in hemiplegic cerebral palsy: a randomized control trial. Dev Med Child Neurol. 2006;48:635–642. doi: 10.1017/S0012162206001356. [DOI] [PubMed] [Google Scholar]
- 7.Feys P, Duportail M, Kos D, Van Asch P, Ketelaer P. Validity of the TEMPA for the measurement of upper limb function in multiple sclerosis. Clinical Rehabilitation. 2002;16:166–173. doi: 10.1191/0269215502cr471oa. [DOI] [PubMed] [Google Scholar]
- 8.Kreder HJ, Agel J, McKee MD, Schemitsch EH, Stephen D, Hanel DP. A randomized, controlled trial of distal radius fractures with metaphyseal displacement but without joint incongruity: closed reduction and casting versus closed reduction, spanning external fixation, and optional percutaneous K-wires. Journal of Orthopaedic Trauma. 2006;20:115–121. doi: 10.1097/01.bot.0000199121.84100.fb. [DOI] [PubMed] [Google Scholar]
- 9.Provinciali L, Giattini A, Splendiani G, Logullo F. Usefulness of hand rehabilitation after carpal tunnel surgery. Muscle & Nerve. 2000;23:211–216. doi: 10.1002/(sici)1097-4598(200002)23:2<211::aid-mus11>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 10.Jones E, Hanly JG, Mooney R, Rand LL, Spurway PM, Eastwood BJ, et al. Strength and function in the normal and rheumatoid hand. J Rheumatol. 1991;18:1313–1318. [PubMed] [Google Scholar]
- 11.Rettig LA, Luca L, Murphy MS. Silicone implant arthroplasty in patients with idiopathic osteoarthritis of the metacarpophalangeal joint. Journal of Hand Surgery - American Volume. 2005;30:667–672. doi: 10.1016/j.jhsa.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 12.Szabo RM. Outcomes assessment in hand surgery: when are they meaningful? J Hand Surg [Am] 2001;26:993–1002. doi: 10.1053/jhsu.2001.29487. [DOI] [PubMed] [Google Scholar]
- 13.Stern EB. Stability of the Jebsen-Taylor Hand Function Test across three test sessions. Am J Occup Ther. 1992;46:647–649. doi: 10.5014/ajot.46.7.647. [DOI] [PubMed] [Google Scholar]
- 14.Jain A, Ball C, Nanchahal J. Functional outcome following extensor synovectomy and excision of the distal ulna in patients with rheumatoid arthritis. J Hand Surg [Br] 2003;28:531–536. doi: 10.1016/s0266-7681(03)00099-8. [DOI] [PubMed] [Google Scholar]
- 15.Sharma S, Schumacher HR, Jr., McLellan AT. Evaluation of the Jebsen hand function test for use in patients with rheumatoid arthritis. Arthritis Care Res. 1994;7:16–19. doi: 10.1002/art.1790070105. [DOI] [PubMed] [Google Scholar]
- 16.Vliet Vlieland TP, van der Wijk TP, Jolie IM, Zwinderman AH, Hazes JM. Determinants of hand function in patients with rheumatoid arthritis. J Rheumatol. 1996;23:835–840. [PubMed] [Google Scholar]
- 17.Chung K, Burns P, Wilgis E, Burke F, Regan M, Kim M, et al. A multi-center clinical trial in rheumatoid arthritis patients by comparing silicone metacarpophalangeal joint arthroplasty with medical treatment. J Hand Surg [Am] 2009;34(5):815–23. doi: 10.1016/j.jhsa.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang EY, Chung KC. Outcomes of trapeziectomy with a modified abductor pollicis longus suspension arthroplasty for the treatment of thumb carpometacarpal joint osteoarthritis. Plast Reconstr Surg. 2008;122:505–515. doi: 10.1097/PRS.0b013e31817d5419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Klein RD, Kotsis SV, Chung KC. Open carpal tunnel release using a 1-centimeter incision: technique and outcomes for 104 patients. Plast Reconstr Surg. 2003;111:1616–1622. doi: 10.1097/01.PRS.0000057970.87632.7e. [DOI] [PubMed] [Google Scholar]
- 20.Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am. 2006;88:2687–2694. doi: 10.2106/JBJS.E.01298. [DOI] [PubMed] [Google Scholar]
- 21.Michigan Hand Outcomes Questionnaire. http://sitemaker.umich.edu/mhq/overview: Accessed March 12, 2009.
- 22.Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42:619–622. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg [Am] 1998;23:575–587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 24.Chung KC, Kotsis SV, Kim HM. A prospective outcomes study of Swanson metacarpophalangeal joint arthroplasty for the rheumatoid hand. J Hand Surg [Am] 2004;29:646–653. doi: 10.1016/j.jhsa.2004.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kotsis SV, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and the Disabilities of the Arm, Shoulder and Hand questionnaire in carpal tunnel surgery. J Hand Surg [Am] 2005;30:81–86. doi: 10.1016/j.jhsa.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 26.Kotsis SV, Lau FH, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and physical measurements in outcome studies of distal radius fracture treatment. J Hand Surg [Am] 2007;32:84–90. doi: 10.1016/j.jhsa.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 27.Fan J, Upadhye S, Worster A. Understanding receiver operating characteristic (ROC) curves. CJEM. 2006;8:19–20. doi: 10.1017/s1481803500013336. [DOI] [PubMed] [Google Scholar]
- 28.Disabilities of the Arm, Shoulder and Hand. http://www.dash.iwh.on.ca/: Accessed July 13, 2009.
- 29.Kimberley TJ, Lewis SM, Auerbach EJ, Dorsey LL, Lojovich JM, Carey JR. Electrical stimulation driving functional improvements and cortical changes in subjects with stroke. Exp Brain Res. 2004;154:450–460. doi: 10.1007/s00221-003-1695-y. [DOI] [PubMed] [Google Scholar]
- 30.Kreder HJ, Hanel DP, Agel J, McKee M, Schemitsch EH, Trumble TE, et al. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius: a randomised, controlled trial. J Bone Joint Surg Br. 2005;87:829–836. doi: 10.1302/0301-620X.87B6.15539. [DOI] [PubMed] [Google Scholar]
- 31.Synnott K, Mullett H, Faull H, Kelly EP. Outcome measures following metacarpophalangeal joint replacement. J Hand Surg [Br] 2000;25:601–603. doi: 10.1054/jhsb.2000.0402. [DOI] [PubMed] [Google Scholar]
- 32.Prabhu K, Babu KS, Samuel S, Chacko AG. Rapid opening and closing of the hand as a measure of early neurologic recovery in the upper extremity after surgery for cervical spondylotic myelopathy. Arch Phys Med Rehabil. 2005;86:105–108. doi: 10.1016/j.apmr.2004.01.037. [DOI] [PubMed] [Google Scholar]
- 33.Goossens PH, Heemskerk B, van Tongeren J, Zwinderman AH, Vlieland TP, Huizinga TW. Reliability and sensitivity to change of various measures of hand function in relation to treatment of synovitis of the metacarpophalangeal joint in rheumatoid arthritis. Rheumatology. 2000;39:909–913. doi: 10.1093/rheumatology/39.8.909. [DOI] [PubMed] [Google Scholar]
- 34.Bain GI, Pugh DM, MacDermid JC, Roth JH. Matched hemiresection interposition arthroplasty of the distal radioulnar joint. J Hand Surg [Am] 1995;20:944–950. doi: 10.1016/S0363-5023(05)80141-8. [DOI] [PubMed] [Google Scholar]
- 35.Edmunds I, Trevithick B, Honner R. Fusion of the first metacarpophalangeal joint for post-traumatic conditions. Aust N Z J Surg. 1994;64:771–774. doi: 10.1111/j.1445-2197.1994.tb04537.x. [DOI] [PubMed] [Google Scholar]
- 36.Goldfarb CA, Klepps SJ, Dailey LA, Manske PR. Functional outcome after centralization for radius dysplasia. J Hand Surg [Am] 2002;27:118–124. doi: 10.1053/jhsu.2002.30078. [DOI] [PubMed] [Google Scholar]