Abstract
Background
Venous thromboembolism (VTE) affects as many as 1 in 1000 individuals in the United States. Although Blacks are disproportionately affected by VTE, few genetic risk factors have been identified in this population. The inducible heme oxygenase-1 (HMOX1) gene encodes a key cytoprotective enzyme with anti-inflammatory, antioxidant and anticoagulant activity acting in the vascular system. A (GT)n microsatellite located in the promoter of the HMOX1 gene influences the level of response.
Methods and Results
Using the Genetic Attributes and Thrombosis Epidemiology (GATE) study, we examined the association between HMOX1 repeat length and VTE events in 883 Black and 927 White patients and matched controls. We found no association between HMOX1 genotypes and VTE in Whites. However, in Black patients, carrying two long (L) alleles (≥34 repeats) was significantly associated with provoked (odds ratio (OR) 1.86, 95% confidence interval (CI): 1.19–2.90) or recurrent (OR 3.13, 95% CI: 1.77–5.53) VTE events.
Conclusions
We have demonstrated for the first time an association between genetic variation in HMOX1, and VTE in Blacks. Our results support a key role for the heme oxygenase system in protecting patients at increased risk for thrombosis and suggest a potential mechanism for targeted screening and intervention.
Keywords: Deep vein thrombosis, heme oxygenase-1, oxidative stress, genetic association
Introduction
Venous thromboembolism (VTE) is a chronic, sometimes fatal disease with significant public health impact worldwide [1]. Defined clinically as inappropriate clotting of the blood presenting as either deep vein thrombosis (DVT), pulmonary embolism (PE) or both, VTE is estimated to affect approximately 1 in 1000 individuals per year in the U.S. alone [2, 3]. Surviving VTE patients also face increased risk of recurrent thromboembolism and significant morbidity with post-thrombotic syndrome symptoms including pain, swelling and leg ulceration from venous reflux and post-thrombotic syndrome [4, 5]. In spite of the high burden of VTE, much of the underlying etiology remains unexplained.
The inflammatory process is increasingly being recognized as an important mechanism regulating thrombus formation and resolution [6, 7]. Biomarkers for inflammation, including C-reactive protein, have been reported to be increased in patients with VTE [8, 9]. The lysis of red blood cells (RBCs) abundant in the early thrombus may contribute to further endothelial dysfunction and thrombus propagation through cascading RBC lysis. Free heme from the released hemoglobin is highly inflammatory and a major source of oxidative stress on the endothelium [7, 10, 11].
Heme oxygenase-1 (HO-1), the inducible isoform responsible for the catabolism of heme, is a key cytoprotective enzyme acting in the vascular system [12]. HO-1 is upregulated in response to stress and is induced by stimuli including heme, oxidants, hypoxia, and certain cytokines. The anti-inflammatory, antioxidant and anti-apoptotic effects of HO-1 can be mediated through the two-fold effects of the degradation of heme. First, the removal of heme, which is very oxidative, prevents it from damaging cells and promoting programmed cell death. Second, the products of heme catabolism by HO-1, namely ferrous iron, carbon monoxide and biliverdin, are themselves cytoprotective acting as signaling or upstream molecules in anti-inflammatory, antioxidant pathways in the endothelium [12, 13].
Recent studies suggest that HO-1 activity may play an important role in VTE. Knockout mice which do not express HO-1 have been shown to have an enhanced inflammatory response and significantly impaired resolution of experimentally induced venous thrombosis [14]. Humans carry a (GT)n microsatellite (rs3074372) located in the promoter of the heme oxygenase-1 (HMOX1) gene that may influence the level of HO-1 response whereby individuals with lower numbers of repeats have higher inducible expression [15]. Indeed, Austrian VTE patients who carried longer HMOX1 (GT)n repeat lengths have been reported to be at an increased risk of recurrence [16].
No studies to date have explored the role of HO-1 in first VTE in Whites or in any VTE in Black populations, where, in spite of elevated risk, limited data on genetic factors for thrombosis exists [17, 18]. The Genetic Attributes and Thrombosis Epidemiology (GATE) study provides a unique opportunity to simultaneously determine contribution of genetic polymorphisms to VTE in both Black and White populations [17]. Using this case-control study in which both of these groups are nearly equally represented, we examine associations between HMOX1 (GT)n repeat length and various types of VTE events.
Materials and Methods
Study population and clinical definitions
The GATE study design and characteristics have been previously described in detail [17, 18]. Briefly, cases were adult patients 18–70 years of age who were admitted to one of two university hospitals in Atlanta, Georgia during between 1998 and 2005 and were diagnosed with a first or recurrent VTE. Cases were identified by review of medical charts of patients receiving unfractionated or low-molecular-weight heparin. DVT was confirmed by Doppler ultrasonography, computed tomography (CT), magnetic resonance imaging, or contrast venography. Confirmation of PE was made by positive angiogram, ventilation–perfusion lung scan, or CT. Patients with severe illness or with cognitive deficits were excluded [17].
Controls were selected from a list of patients who visited a university affiliated primary care clinic between 1997 and 2000; those currently taking anti-coagulant therapy or who had a history of VTE were ineligible. Similar to cases, controls with severe illness or cognitive defects were also excluded. Controls were frequency matched to cases on age, gender and race [17]. All self-identified Black and White individuals with DNA available for genotyping were included in the present analysis.
Provoked cases were distinguished from idiopathic as VTE arising within 1 week of any of the following settings: with cancer, in conjunction with the placement of a central line, during or after attendance in the intensive care unit, during or after a pregnancy, or after surgery, an injury, or prolonged immobilization within the previous 4 weeks. The mean time between the trigger for the event and its diagnosis was less than 1 week for provoked cases. First events were also distinguished from recurrent by self-reported history of VTE [18].
DNA analysis
Polymerase chain reaction (PCR) fragment size analysis was used to determine HMOX1 promoter (GT)n dinucleotide repeat (rs3074372) length, using a FAM labeled forward primer, AGA GCC TGC AGC TTC TCA GA and an unlabeled reverse primer, ACA AAG TCT GGC CAT AGG AC. Amplification was performed in a 10 µl reaction (final concentration 1× GeneAmp® PCR buffer with MgCl2 (Applied Biosystems, Foster City, CA), 0.5 mM dNTPs, 0.625 µM primers (each), 5% dimethyl sulfoxide (DMSO), 0.25 U Amplitaq (Applied Biosystems). The PCR conditions used for labeling were 96°C for 10 minutes, 40 cycles (92°C for 30 seconds; 51°C for 30 seconds; 72°C for 30 seconds) and 72°C for 7 minutes, followed by a 4°C hold. Labeled products were run with an internal size standard (GeneScan™ −500 LIZ®) in Hi-Di™ Formamide on a 3730 DNA Analyzer, and fragment size was determined using GeneMapper® Software Version 4.0 software (Applied Biosystems).
Approximately 5% of samples were validated by DNA sequence analysis to confirm HMOX1 repeat length. Initial fragment amplification was performed as described above for fragment analysis substituting unlabeled primers. Following an ExoSap-IT (Affymetrix, Santa Clara, CA) reaction to remove unused primers and nucleotides, BigDye® Terminator v1.1 Cycle Sequencing Kit (Applied Biosystems) was used to prepare the samples for automated sequencing according to the manufacturer’s recommendations. Sequencing reactions were further cleaned up by ethanol precipitation and re-suspended in Hi-Di™ Formamide. Samples were then run on an ABI 3730 DNA Analyzer, and sequences were reviewed using Sequencing Analysis 5.2 (Applied Biosystems).
(GT)n repeat classification
For initial analyses, the observed HMOX1 (GT)n repeat sizes were divided into three allele classes, short (S) with 25 or fewer repeats, medium (M) with 26 to 33 repeats, and long (L) with 34 or more repeats. To model the effect of carrying the longer “risk” alleles in logistic regression analyses, small and medium alleles were grouped together and compared to long (L) alleles with 34 or more repeats.
Statistical analysis
Differences in the distribution of demographic and clinical characteristics and repeat length categories between cases and controls were assessed using two-tailed chi-square tests, t-tests, and Fisher’s exact tests, where appropriate. Conditional logistic regression was used to calculate odds ratios and 95% confidence intervals for the association between repeat length (L/L vs. other) and VTE among Blacks, conditioning on age and sex. Because no White cases had the L/L genotype, Whites were omitted from the regression analyses. The 10% change in effect estimate criterion was used to evaluate potential confounders (diabetes, obesity, high blood pressure, current smoker, family history of VTE, history of cancer, sickle cell disease, and Factor V Leiden). As such, the crude odds ratio was compared with the adjusted odds ratio for each variable individually, and those variables associated with a difference of 10% or more were considered confounders [19]. However, after applying the criterion, none of the covariates remained in the final model; thus, crude odds ratios are presented. SAS 9.2 software (SAS Institute, Cary, NC) was used for all analyses.
Results
Clinical characteristics
Demographic and clinical characteristics for VTE cases and controls included in this study are reported in Table 1. Results are reported by race, and VTE event types are dichotomized as follows: DVT only vs. PE and/or DVT; first occurrence vs. recurrent; and provoked vs. idiopathic. Regardless of race, the frequency of diabetes, family history of VTE, and history of cancer was higher in cases than controls. Among whites, significantly greater proportions of cases were obese, had high blood pressure, were current smokers and carried the Factor V Leiden mutation compared with controls. For both race subgroups, more than 60% of VTE events were classified as DVT only. The proportion of provoked VTE was 62% for White cases and 58% for Black cases, and the proportion of recurrent VTE was 24% for White cases and 20% for Black cases.
Table 1.
Characteristics of cases and controls by race
| Whites | Blacks | |||||
|---|---|---|---|---|---|---|
| Cases | Controls | p-value | Cases | Controls | p-value | |
| N=416 | N=511 | N=440 | N=443 | |||
| Age (SD) | 50.5 (12.7) | 50.8 (12.8) | 0.79 | 47.1 (12.5) | 47.8 (12.4) | 0.42 |
| Sex (%) | ||||||
| Male | 57.9 | 56.8 | 0.72 | 42.5 | 40.9 | 0.62 |
| Female | 42.1 | 43.2 | 57.5 | 59.1 | ||
| Diabetes (%) | 14.9 | 4.9 | <.0001 | 25.2 | 15.8 | 0.0005 |
| Obese (%) | 38.7 | 22.1 | <.0001 | 42.5 | 45.4 | 0.39 |
| High blood pressure (%) | 39.7 | 28.8 | 0.0005 | 50.5 | 45.2 | 0.11 |
| Current smoker (%) | 37.4 | 30.3 | 0.0002 | 22.3 | 21.7 | 0.31 |
| Family history VTE (%) | 30.5 | 12.6 | <.0001 | 26.6 | 11.2 | <.0001 |
| History of cancer (%) | 36.9 | 16.2 | <.0001 | 22.1 | 6.3 | <.0001 |
| Sickle cell disease (%) | 0 | 0 | 2.1 | 0 | 0.002* | |
| Sickle cell trait (%) | 0 | 0 | 10.7 | 6.6 | 0.03 | |
| Factor V Leiden (%) | 12.3 | 6.7 | 0.003 | 2.1 | 1.1 | 0.27 |
| Event type (%) | ||||||
| DVT only | 63.0 | N/A | 64.1 | N/A | ||
| PE ± DVT | 37.0 | N/A | 35.9 | N/A | ||
| Recurrent | 24.3 | N/A | 19.8 | N/A | ||
| Provoked | 61.8 | N/A | 57.7 | N/A | ||
Fisher’s exact p-value computed.
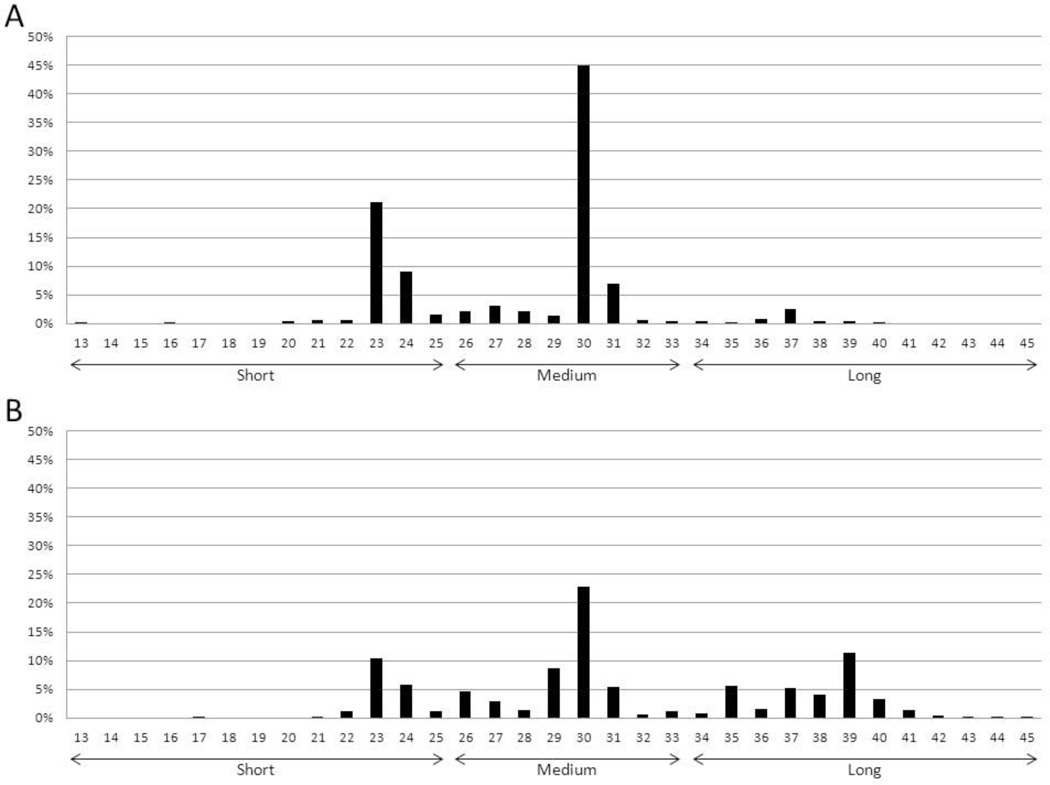
HMOX1 (GT)n repeat distribution
The HMOX1 (GT)n repeat was highly polymorphic, and the distribution of alleles differed by race with greater variation observed in the Black population (Figure 1). Overall, we observed 28 different alleles with the number of dinucleotide repeats varying from 13 to 45. In addition to peaks at 23 and 30 repeats, we observed a third peak at 39 repeats in the Black population that was absent from the White population.
Figure 1. HMOX1 (GT)n repeat distribution among Genetic Attributes and Thrombosis Epidemiology (GATE) study participants by race.
Allele lengths were scored as number of dinucleotide repeats and ranged from 13 to 45 repeats. ‘Small’ is defined as ≤25 repeats; ‘Medium’ is defined as 26–33 repeats; and ‘Long’ is defined as ≥34 repeats. Distribution of alleles is shown for A) 927 White and B) 883 Black patients and matched controls.
HMOX1 (GT)n repeat and VTE
For initial comparisons, the observed HMOX1 (GT)n repeat sizes were grouped into three allele classes: short (S) with 25 or fewer repeats, medium (M) with 26 to 33 repeats, and long (L) with 34 or more repeats. The distribution of the 6 possible genotype classes in cases and controls are shown by race in Table 2. We found no significant association between HMOX1 genotypes and VTE in Whites. However, the distribution of HMOX1 genotype classes was significantly different between Black cases and controls, with an increased frequency of L/L in all patients with VTE (Table 2A). When patients were stratified by event type, this effect became much more pronounced with an increased frequency of L/L genotypes in patients with provoked as well as recurrent VTE (Tables 2C and 2E). HMOX1 allele distribution was not significantly different in Black cases with idiopathic or first VTE events compared to controls (Tables 2B and 2D). The relationship between genetic variation in HMOX1 and pulmonary embolism alone was not separately assessed due to the limited number of patients presenting with PE only.
Table 2.
Repeat length frequency by race
| Whites | Blacks | |||||
|---|---|---|---|---|---|---|
| Repeat length‡ | Case n (%) |
Control n (%) |
p-value | Case n (%) |
Control n (%) |
p-value |
| A. All VTE | ||||||
| S/S | 47 (11.3) | 58 (11.4) | p=0.49 | 26 (5.9) | 14 (3.2) | p=0.02 |
| S/M | 170 (40.9) | 212 (41.5) | 72 (16.4) | 86 (19.4) | ||
| S/L | 9 (2.2) | 21 (4.1) | 49 (11.1) | 43 (9.7) | ||
| M/M | 161 (38.7) | 191 (37.4) | 91 (20.7) | 112 (25.3) | ||
| M/L | 29 (7.0) | 28 (5.5) | 131 (29.8) | 143 (32.3) | ||
| L/L | 0 | 1 (0.2) | 71 (16.1) | 45 (10.2) | ||
| B. Idiopathic VTE | ||||||
| S/S | 17 (10.7) | 58 (11.4) | p=0.40 | 7 (3.8) | 14 (3.2) | p=0.78 |
| S/M | 71 (44.7) | 212 (41.5) | 34 (18.3) | 86 (19.4) | ||
| S/L | 1 (0.6) | 21 (4.1) | 20 (31.8) | 43 (9.7) | ||
| M/M | 61 (38.4) | 191 (37.4) | 43 (23.1) | 112 (25.3) | ||
| M/L | 9 (24.3) | 28 (5.5) | 56 (30.1) | 143 (32.3) | ||
| L/L | 0 | 1 (0.2) | 26 (14.0) | 45 (10.2) | ||
| C. Provoked VTE | ||||||
| S/S | 30 (11.7) | 58 (11.4) | p=0.72 | 19 (7.5) | 14 (3.2) | p=0.002 |
| S/M | 99 (38.5) | 212 (41.5) | 38 (15.0) | 86 (19.4) | ||
| S/L | 8 (3.1) | 21 (4.1) | 29 (11.4) | 43 (9.7) | ||
| M/M | 100 (38.9) | 191 (37.4) | 48 (18.9) | 112 (25.3) | ||
| M/L | 20 (7.8) | 28 (5.5) | 75 (29.5) | 143 (32.3) | ||
| L/L | 0 | 1 (0.2) | 45 (17.7) | 45 (10.2) | ||
| D. First event | ||||||
| S/S | 36 (11.4) | 58 (11.4) | p=0.59 | 23 (6.5) | 14 (3.2) | p=0.09 |
| S/M | 134 (42.5) | 212 (41.5) | 58 (16.4) | 86 (19.4) | ||
| S/L | 6 (22.2) | 21 (4.1) | 42 (11.9) | 43 (9.7) | ||
| M/M | 120 (38.1) | 191 (37.4) | 78 (22.1) | 112 (25.3) | ||
| M/L | 19 (6.0) | 28 (5.5) | 105 (29.8) | 143 (32.3) | ||
| L/L | 0 | 1 (0.2) | 47 (13.3) | 45 (10.2) | ||
| E. Recurrent VTE | ||||||
| S/S | 11 (10.9) | 58 (11.4) | p=0.54 | 3 (3.5) | 14 (3.2) | p=0.0008 |
| S/M | 36 (35.6) | 212 (41.5) | 14 (16.1) | 86 (19.4) | ||
| S/L | 3 (3.0) | 21 (4.1) | 7 (8.1) | 43 (9.7) | ||
| M/M | 41 (40.6) | 191 (37.4) | 13 (14.9) | 112 (25.3) | ||
| M/L | 10 (9.9) | 28 (5.5) | 26 (29.9) | 143 (32.3) | ||
| L/L | 0 | 1 (0.2) | 24 (27.6) | 45 (10.2) | ||
‘S’ is ≤25, ‘M’ is 26–33, and ‘L’ is ≥34.
For logistic regression modeling, we tested a recessive genetic effect, comparing individuals with L/L genotypes to all other genotype classes (Table 3). Homozygous L/L individuals were rare in the White population with only one control having this genotype; thus we were unable to model this characteristic in Whites. For Black patients, L/L genotype was significantly associated with provoked (odds ratio (OR) 1.86, 95% confidence interval (CI): 1.19–2.90) or recurrent (OR 3.13, 95% CI: 1.77–5.53) VTE events. The association between genotype and idiopathic or first VTE events did not reach statistical significance in these cases, although both ORs were elevated for the L/L genotype.
Table 3.
Odds ratio and 95% confidence intervals for the association between genotype and VTE among Blacks*
| Repeat length‡ | Case n (%) |
Control n (%) |
Odds Ratio† | 95% CI |
|---|---|---|---|---|
| A. All VTE | ||||
| S*/S*+S*/L | 369 (83.9) | 398 (89.8) | REF | |
| L/L | 71 (16.1) | 45 (10.2) | 1.69 | 1.13–2.52 |
| B. Idiopathic VTE | ||||
| S*/S*+S*/L | 160 (86.0) | 398 (89.8) | REF | |
| L/L | 26 (14.0) | 45 (10.2) | 1.36 | 0.80–2.30 |
| C. Provoked VTE | ||||
| S*/S*+S*/L | 209 (82.3) | 398 (89.8) | REF | |
| L/L | 45 (17.7) | 45 (10.2) | 1.86 | 1.19–2.90 |
| D. First event | ||||
| S*/S*+S*/L | 306 (86.7) | 398 (89.8) | REF | |
| L/L | 47 (13.3) | 45 (10.2) | 1.36 | 0.88–2.10 |
| E. Recurrent VTE | ||||
| S*/S*+S*/L | 63 (72.4) | 398 (89.8) | REF | |
| L/L | 24 (27.6) | 45 (10.2) | 3.13 | 1.77–5.53 |
Findings for Whites were not modeled due to lack of cases with L/L genotype.
‘S*’ is ≤33, and ‘L’ is ≥34.
Logistic regression models conditioned on age (≤40, 41–50, 51–60, 60+) and sex.
To explore the difference in findings by VTE subtype post-hoc case-case analyses were conducted for the Black cases only (n = 440). In conditional logistic regression models assessing differences in the L/L genotype for provoked versus idiopathic, the association was not statistically significant (OR 1.29, 95% CI: 0.76–2.19). However, the L/L genotype was significantly associated with recurrent VTE compared with first VTE (OR 2.47, 95% CI: 1.40–4.36, p=.002).
Discussion
Blacks are disproportionately affected by VTE, yet there remains limited data on the etiology [20]. Family history of VTE has been shown to increase risk; however, other than one report of sickle cell trait, no genetic risk factors have been well characterized in Blacks [18, 21]. In the present study, we demonstrated a novel association between genetic variation in the vascular cytoprotective enzyme, HO-1, and VTE in Blacks. Additionally, this study is the first to test (GT)n repeat alleles for associations with first VTE and idiopathic versus provoked events in any population. Specifically, we found that Black patients with L/L HMOX1 promoter (GT)n repeat genotypes were at significantly increased risk for provoked as well as recurrent VTE.
A robust heme oxygenase response may be particularly important to protect individuals with VTE disease by inhibiting thrombus formation or expansion induced by free heme and redox-active iron. Free pro-oxidative iron and heme-containing moieties in the bloodstream are highly toxic to the vasculature and can lead to endothelial dysfunction and vascular disease [10, 22, 23]. Interestingly, recent studies have demonstrated an important role of red blood cell hemolysis and hemoglobin oxidation in promoting iron-induced vascular injury and thrombosis in an ex vivo model system [11]. Further, these authors provided evidence that free hemoglobin may also contribute to thrombus development by exacerbating red blood cell lysis and further driving a damaging oxidative cycle [11].
Inducible HO-1 is the rate limiting enzyme responsible for the removal of damaging, highly oxidative free heme from the circulation. Additionally, the products of the degradation of heme, ionic iron, CO and biliverdin, or their immediate downstream products also contribute to an anti-oxidative, anti-inflammatory state and have anti-thrombotic activity [12, 24, 25]. DNA polymorphisms which impair or reduce HO-1 response may therefore lead to increased risk of endothelial dysfunction and vascular disease, including resolution of venous thrombosis [14]. Human patients with shorter HMOX1 promoter (GT)n repeat alleles might benefit by having a stronger inducible heme oxygenase response [15, 26], and indeed, long alleles were associated with increased risk of recurrent VTE in the only other study to date to examine the role of this polymorphism in VTE [16].
The distribution of allele lengths differed dramatically between Blacks and Whites in our study and may help to explain the difference in the incidence of VTE in the two populations in the U.S. Whites were significantly less likely to carry longer “risk” alleles, and the prominent 23 and 30 repeat sizes accounted for more than half of the alleles present. Unlike Mustafa and colleagues who examine risk of recurrence in a case-only series of patients with spontaneous first VTE [16], we found no association between HMOX1 (GT)n repeat length and VTE in White patients in our case-control study. The discrepancy in findings may be due to differences in recurrent VTE sample size and analytical approaches. The frequency of long alleles was similar in both studies, and a sample size of over 850 White patients was necessary to identify only 3 individuals with L/L genotypes [16]. Because of this rarity of long alleles, a larger sample size will be necessary to clarify the role of this polymorphism in thrombotic disease in Whites.
In contrast, we identified a pattern of greater genetic variation that was shifted toward longer repeats in Blacks, and more than one-quarter of the (GT)n alleles were 34 repeats or greater. This increased prevalence of long repeat alleles was similar to that seen in the few studies to date characterizing this microsatellite polymorphism in individuals with African ancestry [27]. We found a significant association in these patients with long allele length and all VTE that became more pronounced in the provoked and recurrent categories when patients were stratified by event type. Although the ORs were elevated for idiopathic or first VTE events, the association with L/L genotype did not reach statistical significance in Blacks. It is intriguing that our exploratory case-only analysis of L/L genotype with recurrent versus first VTE was significant in Blacks. However, our results are based on a relatively small number of cases, and additional studies will be necessary to verify whether the heme oxygenase response plays a differential role in the etiologies of these subtypes.
Our results support a key role for the heme oxygenase system in protecting patients at increased risk for thrombosis. Our findings also suggest a potential mechanism for targeted screening and intervention, particularly since the risk-conferring alleles are relatively common in Blacks. For example, additional or extended thromboprophylactic treatment might be beneficial in patients at risk of provoked VTE or to prevent recurrence in those individuals that also carry long HMOX1 (GT)n alleles.
Our findings are subject to several limitations. First, the low prevalence of L/L genotype in White cases precluded the evaluation of the association between repeat length and VTE in the White population. Second, the cases for the GATE study represented only those patients who were hospitalized and did not include those who were treated for VTE in outpatient settings. Findings from recent studies indicate that 50–73% of patients with VTE presented in an outpatient setting [28, 29]; therefore our findings are only representative of individuals with VTE severe enough to require hospitalization. Finally, although longer HMOX1 (GT)n promoter repeats have been associated with impaired inducible heme oxygenase [15, 27, 30], no functional measurements of expression levels or enzyme activity were available in our patient samples.
In summary, we demonstrated a novel association with genetic variation in the heme oxygenase system in Blacks, a population disproportionately affected by VTE in the United States. The odds of carrying L/L HMOX1 promoter (GT)n repeat genotypes were approximately two and three times greater in patients with provoked and recurrent VTE, respectively, compared to controls. Our findings support a key role for the heme oxygenase system in protecting patients at increased risk for thrombosis and suggest a novel approach for future targeted screening and intervention. Additional clinical and functional studies will be necessary to confirm our findings and further elucidate the role of impaired heme oxygenase response in patients at risk for VTE.
Acknowledgements
This work was supported by a grant from the Centers for Disease Control and Prevention through the Associations of Schools of Public Health / CDC Cooperative Agreement mechanism. The authors would like to thank past and present members of the Division of Blood Disorders Laboratory Branch and the Genetic Attributes and Thrombosis Epidemiology study staff.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Abbreviations
- CI
confidence interval
- CT
computed tomography
- DMSO
dimethyl sulfoxide
- DVT
deep vein thrombosis
- GATE
Genetic Attributes and Thrombosis Epidemiology
- HMOX1
heme oxygenase-1
- HO-1
heme oxygenase-1
- L
long
- M
medium
- OR
odds ratio
- PCR
Polymerase chain reaction
- PE
pulmonary embolism
- RBC
red blood cell
- S
short
- VTE
venous thromboembolism
Footnotes
Conflict of Interest Statement:
The authors have reported no financial conflicts of interest.
References
- 1.Beckman MG, Hooper WC, Critchley SE, Ortel TL. Venous thromboembolism: a public health concern. American journal of preventive medicine. 2010;38:S495–S501. doi: 10.1016/j.amepre.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 2.Silverstein MD, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ., 3rd Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Archives of internal medicine. 1998;158:585–593. doi: 10.1001/archinte.158.6.585. [DOI] [PubMed] [Google Scholar]
- 3.Spencer FA, Emery C, Lessard D, Anderson F, Emani S, Aragam J, et al. The Worcester Venous Thromboembolism study: a population-based study of the clinical epidemiology of venous thromboembolism. Journal of general internal medicine. 2006;21:722–727. doi: 10.1111/j.1525-1497.2006.00458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heit JA, Mohr DN, Silverstein MD, Petterson TM, O'Fallon WM, Melton LJ., 3rd Predictors of recurrence after deep vein thrombosis and pulmonary embolism: a population-based cohort study. Archives of internal medicine. 2000;160:761–768. doi: 10.1001/archinte.160.6.761. [DOI] [PubMed] [Google Scholar]
- 5.Prandoni P, Bernardi E, Marchiori A, Lensing AW, Prins MH, Villalta S, et al. The long term clinical course of acute deep vein thrombosis of the arm: prospective cohort study. Bmj. 2004;329:484–485. doi: 10.1136/bmj.38167.684444.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodriguez AL, Wojcik BM, Wrobleski SK, Myers DD, Jr, Wakefield TW, Diaz JA. Statins, inflammation and deep vein thrombosis: a systematic review. Journal of thrombosis and thrombolysis. 2012;33:371–382. doi: 10.1007/s11239-012-0687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saha P, Humphries J, Modarai B, Mattock K, Waltham M, Evans CE, et al. Leukocytes and the natural history of deep vein thrombosis: current concepts and future directions. Arteriosclerosis, thrombosis, and vascular biology. 2011;31:506–512. doi: 10.1161/ATVBAHA.110.213405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bucek RA, Reiter M, Quehenberger P, Minar E. C-reactive protein in the diagnosis of deep vein thrombosis. British journal of haematology. 2002;119:385–389. doi: 10.1046/j.1365-2141.2002.03886.x. [DOI] [PubMed] [Google Scholar]
- 9.Reitsma PH, Rosendaal FR. Activation of innate immunity in patients with venous thrombosis: the Leiden Thrombophilia Study. Journal of thrombosis and haemostasis : JTH. 2004;2:619–622. doi: 10.1111/j.1538-7836.2004.00689.x. [DOI] [PubMed] [Google Scholar]
- 10.Balla J, Vercellotti GM, Jeney V, Yachie A, Varga Z, Jacob HS, et al. Heme, heme oxygenase, and ferritin: how the vascular endothelium survives (and dies) in an iron-rich environment. Antioxidants & redox signaling. 2007;9:2119–2137. doi: 10.1089/ars.2007.1787. [DOI] [PubMed] [Google Scholar]
- 11.Woollard KJ, Sturgeon S, Chin-Dusting JP, Salem HH, Jackson SP. Erythrocyte hemolysis and hemoglobin oxidation promote ferric chloride-induced vascular injury. The Journal of biological chemistry. 2009;284:13110–13118. doi: 10.1074/jbc.M809095200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gozzelino R, Jeney V, Soares MP. Mechanisms of cell protection by heme oxygenase-1. Annual review of pharmacology and toxicology. 2010;50:323–354. doi: 10.1146/annurev.pharmtox.010909.105600. [DOI] [PubMed] [Google Scholar]
- 13.Otterbein LE, Soares MP, Yamashita K, Bach FH. Heme oxygenase-1: unleashing the protective properties of heme. Trends in immunology. 2003;24:449–455. doi: 10.1016/s1471-4906(03)00181-9. [DOI] [PubMed] [Google Scholar]
- 14.Tracz MJ, Juncos JP, Grande JP, Croatt AJ, Ackerman AW, Katusic ZS, et al. Induction of heme oxygenase-1 is a beneficial response in a murine model of venous thrombosis. The American journal of pathology. 2008;173:1882–1890. doi: 10.2353/ajpath.2008.080556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hirai H, Kubo H, Yamaya M, Nakayama K, Numasaki M, Kobayashi S, et al. Microsatellite polymorphism in heme oxygenase-1 gene promoter is associated with susceptibility to oxidant-induced apoptosis in lymphoblastoid cell lines. Blood. 2003;102:1619–1621. doi: 10.1182/blood-2002-12-3733. [DOI] [PubMed] [Google Scholar]
- 16.Mustafa S, Weltermann A, Fritsche R, Marsik C, Wagner O, Kyrle PA, et al. Genetic variation in heme oxygenase 1 (HMOX1) and the risk of recurrent venous thromboembolism. Journal of vascular surgery : official publication, the Society for Vascular Surgery [and] International Society for Cardiovascular Surgery, North American Chapter. 2008;47:566–570. doi: 10.1016/j.jvs.2007.09.060. [DOI] [PubMed] [Google Scholar]
- 17.Dowling NF, Austin H, Dilley A, Whitsett C, Evatt BL, Hooper WC. The epidemiology of venous thromboembolism in Caucasians and African-Americans: the GATE Study. Journal of thrombosis and haemostasis : JTH. 2003;1:80–87. doi: 10.1046/j.1538-7836.2003.00031.x. [DOI] [PubMed] [Google Scholar]
- 18.Austin H, Key NS, Benson JM, Lally C, Dowling NF, Whitsett C, et al. Sickle cell trait and the risk of venous thromboembolism among blacks. Blood. 2007;110:908–912. doi: 10.1182/blood-2006-11-057604. [DOI] [PubMed] [Google Scholar]
- 19.Rothman KJ, Greenland S. Modern epidemiology. 2nd ed. Philadelphia, PA: Lippincott-Raven; 1998. [Google Scholar]
- 20.Buckner TW, Key NS. Venous thrombosis in blacks. Circulation. 2012;125:837–839. doi: 10.1161/CIRCULATIONAHA.111.073098. [DOI] [PubMed] [Google Scholar]
- 21.Mili FD, Hooper WC, Lally C, Austin H. The impact of co-morbid conditions on family history of venous thromboembolism in Whites and Blacks. Thrombosis research. 2011;127:309–316. doi: 10.1016/j.thromres.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 22.Rother RP, Bell L, Hillmen P, Gladwin MT. The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin: a novel mechanism of human disease. JAMA : the journal of the American Medical Association. 2005;293:1653–1662. doi: 10.1001/jama.293.13.1653. [DOI] [PubMed] [Google Scholar]
- 23.Frei AC, Guo Y, Jones DW, Pritchard KA, Jr, Fagan KA, Hogg N, et al. Vascular dysfunction in a murine model of severe hemolysis. Blood. 2008;112:398–405. doi: 10.1182/blood-2007-12-126714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lindenblatt N, Bordel R, Schareck W, Menger MD, Vollmar B. Vascular heme oxygenase-1 induction suppresses microvascular thrombus formation in vivo. Arteriosclerosis, thrombosis, and vascular biology. 2004;24:601–606. doi: 10.1161/01.ATV.0000118279.74056.8a. [DOI] [PubMed] [Google Scholar]
- 25.Fujita T, Toda K, Karimova A, Yan SF, Naka Y, Yet SF, et al. Paradoxical rescue from ischemic lung injury by inhaled carbon monoxide driven by derepression of fibrinolysis. Nature medicine. 2001;7:598–604. doi: 10.1038/87929. [DOI] [PubMed] [Google Scholar]
- 26.Exner M, Minar E, Wagner O, Schillinger M. The role of heme oxygenase-1 promoter polymorphisms in human disease. Free radical biology & medicine. 2004;37:1097–1104. doi: 10.1016/j.freeradbiomed.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 27.Seu L, Burt TD, Witte JS, Martin JN, Deeks SG, McCune JM. Variations in the heme oxygenase-1 microsatellite polymorphism are associated with plasma CD14 and viral load in HIV-infected African-Americans. Genes and immunity. 2012;13:258–267. doi: 10.1038/gene.2011.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spencer FA, Lessard D, Emery C, Reed G, Goldberg RJ. Venous thromboembolism in the outpatient setting. Archives of internal medicine. 2007;167:1471–1475. doi: 10.1001/archinte.167.14.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldhaber SZ, Tapson VF, Committee DFS. A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. The American journal of cardiology. 2004;93:259–262. doi: 10.1016/j.amjcard.2003.09.057. [DOI] [PubMed] [Google Scholar]
- 30.Taha H, Skrzypek K, Guevara I, Nigisch A, Mustafa S, Grochot-Przeczek A, et al. Role of heme oxygenase-1 in human endothelial cells: lesson from the promoter allelic variants. Arteriosclerosis, thrombosis, and vascular biology. 2010;30:1634–1641. doi: 10.1161/ATVBAHA.110.207316. [DOI] [PMC free article] [PubMed] [Google Scholar]