Abstract
Peritraumatic dissociation consistently predicts posttraumatic stress disorder (PTSD). Avoidant coping may serve as a mechanism through which peritraumatic dissociation contributes to PTSD symptoms. Path analysis was used to examine whether avoidant coping assessed 6-weeks following a motor vehicle accident mediated the relationship between in-hospital peritraumatic dissociation and 6-month (n = 193) and 12-month (n = 167) chronic PTSD symptoms. Results revealed that, after controlling for age, gender, depression and 6-week PTSD symptoms, avoidant coping remained a partial mediator between peritraumatic dissociation and chronic PTSD symptoms 6- and 12-months post-accident. Post-hoc multigroup analyses suggested that 6-months post-trauma, the mediation was significant in females, but not in males. Gender-specific results were not significant 12-months post-trauma. Interventions targeted at reducing avoidant coping in high dissociators may aid in reducing PTSD symptoms.
Although previous research has estimated that 60% of men and 50% of women have experienced a traumatic event in their lifetime, rates of posttraumatic stress disorder (PTSD) in the general population are relatively low (~ 7– 8%; Kessler et al., 2005). In order to identify trauma victims most likely to develop PTSD symptoms (PTSS), research has attempted to determine variables that reliably predict PTSS. Peritraumatic dissociation (PD) has been consistently associated with PTSD in a variety of trauma populations (for a review see Lensvelt-Mulders et al., 2008). PD is defined as an immediate reaction to overwhelmingly stressful events, consisting of disturbances in memory, depersonalization and derealization, alterations in time perception, and a sense of detachment from others and one’s surroundings (Marmar et al., 1994). Women report higher levels of PD than men (Tolin & Foa, 2006), and this may help explain the higher PTSD rates in women versus men. PD may protect an individual from immediate overwhelming emotions (van der Hart, Nijenhuis, Steele, & Brown, 2004); however, it may also preclude long-term recovery by preventing emotional processing of the event (Marmar et al., 1994; Ehlers & Clark, 2000).
Meta-analyses have found PD to be related to PTSD with moderate effect sizes (Breh & Seidler, 2007; Lensvelt-Mulders et al., 2008). However, several studies have found that PD does not correlate with PTSS severity above and beyond initial PTSS (see van der Veldon & Wittmann, 2008 for a review). Despite this, PD remains a key risk factor for the disorder (Lensvelt-Mulders et al., 2008), and understanding how PD is related to subsequent PTSS can inform theory and aid in the design of early interventions for at-risk trauma victims (Breh & Seidler, 2007). Avoidant coping, a variable that has been associated with PD and PTSS (Bal, van Oost, Bourdeaudhui & Crombez, 2003; Wong, Looney, Michaels, Palesh, & Koopman, 2006), may serve as a mechanism through which initial PD relates to subsequent PTSS.
Avoidant coping is a passive, emotion-focused way of coping, which may prove counterproductive as the individual makes no attempt to alter the threatening environment or his/her response to the environment (Lazarus, 1993). A positive relationship between avoidant coping and PTSS has been well documented in both cross-sectional and prospective studies (Krause, Kaltman, Goodman, & Dutton, 2008; Ullman, Townsend, Filipas, & Starzynski, 2007). During the acute phase of responding to a trauma, emotional responses and coping behaviors dynamically interact (Folkman & Lazarus, 1988). High PD may invoke avoidant coping because these two reactions share commonalities (e.g., distancing, detachment, compartmentalization: Collins & French, 1998), which serve to prevent the incorporation of fragmented, disorganized traumatic memories into existing cognitive schemas (Engelhard, van den Hout, Kindt, Arntz, & Schouten, 2003). Recent research by Regambal & Alden (2009) suggested a direct link between peritraumatic cognitive processing (including PD) and subsequent maladaptive coping strategies, and reported an indirect link between peritraumatic cognitive processing and intrusive memories through maladaptive coping.
In high dissociators, subsequent attempts to deny, distract, or disengage oneself from traumatic memories may maintain the fragmented memory and prevent habituation (Foa, Steketee, & Rothbaum, 1989). Though initial avoidant coping may be protective by allowing one to garner resources, long-term avoidant coping may render victims unable to translate the threat into one that is controllable (Bryant & Harvey, 1995; Rachman, 1990). This is in line with cognitive models of PTSD (Ehlers & Clark, 2000) purporting that PTSD results when incomplete initial processing of the event renders a sense of current threat. This threat is then unable to be discounted due to the activation of additional maladaptive cognitive and emotional responses.
Despite theoretical support for the dynamic interplay of PD, coping, and PTSS, most empirical studies of these constructs have assessed PD retrospectively (Marx & Sloan, 2005; Wong et al., 2006), and only two cross-sectional studies have examined mechanisms through which PD was related to PTSS. Gershuny, Cloitre, and Otto (2003) reported that peritraumatic fears mediated the relationship between PD and PTSD in a sample of undergraduate trauma victims. Similarly, self-reported memory fragmentation, thought suppression, and acute PTSS mediated the relationship between PD and PTSD in females who suffered from pregnancy loss (Engelhard et al., 2003). Although these results are suggestive, PTSD was assessed via self-report, PD and panic symptoms were assessed retrospectively, and the cross-sectional designs limited conclusions regarding causality. As PD occurs during and soon after a trauma, intervening to reduce PD is not practical; however, avoidant coping lends itself easily to intervention, as it is an ongoing process that occurs during the days, weeks, and months following a trauma. Therefore, if avoidant coping at 6-weeks post-trauma serves as a mechanism for the relationship between PD and PTSS, this will inform the timing and content of interventions as well as identify individuals reporting higher levels of PD as those most likely to benefit from such intervention.
The present study assessed the extent to which avoidant coping mediated the relationship between PD and PTSS in a sample of individuals exposed to a potentially traumatic event (a motor vehicle accident resulting in admission to a trauma unit). It was hypothesized that higher in-hospital PD would be associated with higher levels of avoidant coping 6-weeks post-trauma, and that both PD and avoidant coping would be associated with higher 6- and 12-month chronic PTSS. It was also predicted that avoidant coping would mediate the relationship between PD and chronic PTSS at both time points. Exploratory post hoc analyses were also conducted to determine whether the mediational model differed by gender.
Method
Participants
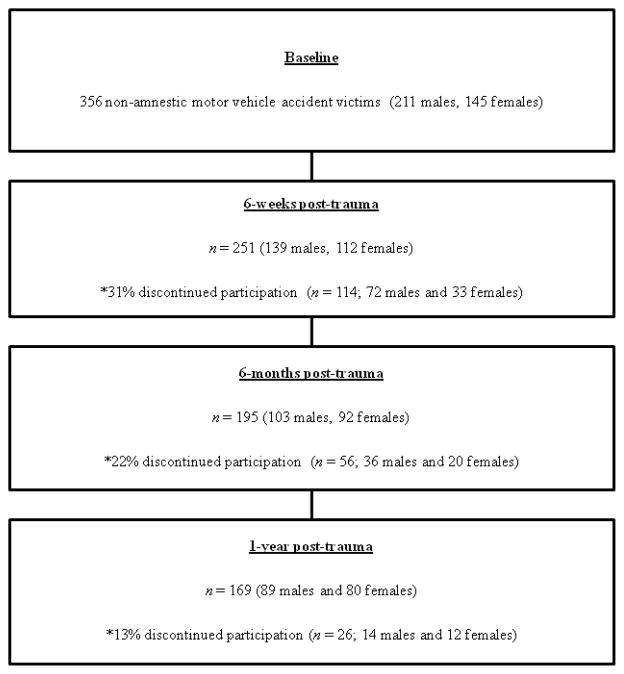
Three-hundred fifty-six non-amnesic adult motor vehicle accident victims were recruited from one of two trauma centers in Akron, OH (see Figure 1). To be eligible for participation, participants must have been fluent in English, over the age of 18, and lived within 30 miles of the hospital. To exclude severe traumatic brain injury, participants had to score a 14 or 15 on the Glasgow Coma Scale (Teasdale & Jennett, 1974). Potential participants were also required to score at least 25 on the Mini Mental Status Exam (Folstein, Folstein & McHugh, 1975) to ensure that they were lucid enough to give informed consent. As the aim of the study was to examine the range of responses to a potentially traumatic event, and not to restrict analyses to those individuals meeting a DSM-IV classified trauma, endorsement of PTSD criterion A was not necessary for inclusion.
Figure 1.
Flow diagram of participant progress throughout the four waves of the present study.
The average age of the participants was 38.7 (SD = 16.22, range = 18–81). The sample was 88% Caucasian, 10% African American, and 2% other (e.g., Hispanic, mixed races/ethnicities). At all follow-up assessments (6-weeks and 6- and 12-months), a greater number of males dropped out of the study than females (all ps < .001 at 6-weeks, and 6- and 12-months). Participants who dropped out of the study at the 6- (p = .01) and 12-month (p = .001) assessments also had reported higher levels of PD than participants who were retained. There were no other significant differences in demographic or study variables between participants who dropped out and those who were retained.
Measures
Peritraumatic dissociation
Participants completed the self-report Peritraumatic Dissociative Experiences Questionnaire (PDEQ; Marmar, Weiss, & Metzler, 1997) based on their experiences and feelings “during the accident and immediately afterward”. Possible scores range from 10–50. Internal consistency for the PDEQ was high (Cronbach’s alpha (α) = .77).
Coping
The Brief COPE (Carver, 1997) subscales of denial, behavioral disengagement, and self-distraction were summed to create the construct of avoidant coping (Wong et al, 2006; Ullman et al., 2007). Possible scores range from 6–24. Internal consistency was high for both the full scale (α = .87), and the abbreviated 6-item avoidant coping scale (α = .81 calculated with the Spearman-Brown prophecy formula; Nunnally, 1970).
PTSS
The Clinician Administered PTSD Scale (Blake et al., 1995) assesses diagnostic levels of PTSD and continuous PTSS. Participants completed the Clinician Administered PTSD Scale based on symptoms experienced in the past month consequent to their motor vehicle accident. Continuous PTSS scores were calculated by summing the frequency and intensity values of each item (range of possible scores: 0–136). This measure demonstrated high internal consistency (alpha at 6-weeks = .91; at 6-months = .90; at 12-months = .91).
Current depression, alcohol and substance use
The Structured Clinical Interview for the DSM-IV (First, Gibbon, Spitzer, & Williams, 1996) was administered to assess diagnostic levels of current depression, current alcohol and/or substance abuse, and whether participants received help for mental health issues. Presence versus absence for each variable was coded dichotomously. Individuals that met sub-threshold depressive criteria were included in the absence group, although analyses were also run with sub-threshold participants included in the diagnostic group; no differences in results were found.
Injury severity
The injury severity score (Baker, O’Neill, Haddon, Long, 1974) is calculated by determining the extent of injury to six different body regions, then squaring and summing the scores from the three most severely injured body regions. Injury severity scores can range from 1 to 75, and were obtained from participants’ medical charts.
Procedure
The study protocol was approved by the human subjects review boards of Kent State University, Summa Health System, and Akron General Hospital. The study was described to eligible participants, and written informed consent was provided by interested participants. Participants completed a demographics questionnaire and the PDEQ in-hospital at a median of 25 (SD = 54.43) hours post-trauma. Follow-up assessments occurred in participants’ homes. Six-weeks post-trauma, participants completed the Brief COPE. Six-weeks and 6- and 12-months post-trauma, PTSS were assessed with the Clinician Administered PTSD Scale, and depression, alcohol abuse, and substance abuse were assessed with the Structured Clinical Interview for the DSM-IV. Interviews were conducted by trained master’s level clinical psychology graduate students. Given the duration and labor-intensive nature of the study, a number of interviewers were required to administer these standardized assessments. However, results from one-way ANOVAs on Clinician Administered PTSD Scale Scores by interviewer revealed no differences between interviewers on scoring, and controlling for interviewer did not change the present results. Further, inter-rater reliability on a randomly selected 10% of audiotaped PTSS scores demonstrated strong agreement between continuous PTSS at 6-weeks (r = .98, p < .001), and 6- (r = .97, p < .001) and 12- (r = .98, p < .001) months post-trauma. Perfect agreement was demonstrated for PTSD diagnostic rates (Kappa = 1.0) at 6-weeks, and 6- and 12-months. Participants were reimbursed $25.00 per assessment for their participation.
Missing Data
To include data from retained participants, missing values were imputed for 8.5% and 1.7% of data points at 6-and 12-months post-trauma, respectively, by estimation maximization in EQS (Bentler, 2004). Four participants with missing depression data were deleted from analyses without imputing due to the categorical nature of these data.
Data Analyses
Preliminary analyses were conducted with Statistics Package for the Social Sciences Version 16 (SPSS 2006). To test for possible control variables, Pearson Product moment correlations were conducted between continuous variables, and Spearman Rho correlations were conducted between continuous and categorical variables. One-way ANOVAs and chi square analyses examined gender differences and differences between depressed and nondepressed participants on the variables of interest. Additional analyses were conducted to determine the potential impact of substance and alcohol abuse and treatment seeking behaviors. Path analyses were conducted in AMOS using maximum likelihood estimation. Model fit was assessed using the Comparative Fit Index (CFI) and the Tucker-Lewis Index (TLI), with fit indices above .90 indicating a good model fit, and the χ2 test, with a value below .05 indicating a good model fit. The root mean square error of approximation (RMSEA) was also calculated for model fit; values below .06 are found to support a good model fit. Given Kraemer and colleagues (2008) recent criticisms of the Baron and Kenny (1986) guidelines for mediation, the current mediation analyses adhered to practices outlined by Preacher and Hayes (2004). Bootstrapping was used to estimate the standard errors and 95% bias-corrected confidence intervals of the indirect effect. In order for partial mediation to be supported, the mediator must be associated with both the predictor and the outcome after controlling for covariates, and the confidence interval of the indirect effect must not include zero. An alpha level of .05 (two-tailed) was used to determine significance in all analyses.
Hypothesized Model
The hypothesized model (Figure 2) was designed to test whether 6-week avoidant coping mediated the relationship between in-hospital PD and 6- and 12-month chronic PTSS after controlling for gender, age, 6-week PTSS and depression. Whereas model fit estimates and all direct path estimates were derived from analyses involving the model depicted in Figure 2, an adapted model was also conducted to isolate the indirect effect of interest from the control variables measured at 6-weeks. The adapted model represented PD, gender, age, 6-week depression and PTSS as exogenous variables, which resulted in avoidant coping serving as the sole indirect effect in the model. Consequently, indirect path estimates and confidence intervals were derived from this adapted model, which allowed for testing the significance of the indirect path from PD to PTSS specifically through avoidant coping.
Figure 2.
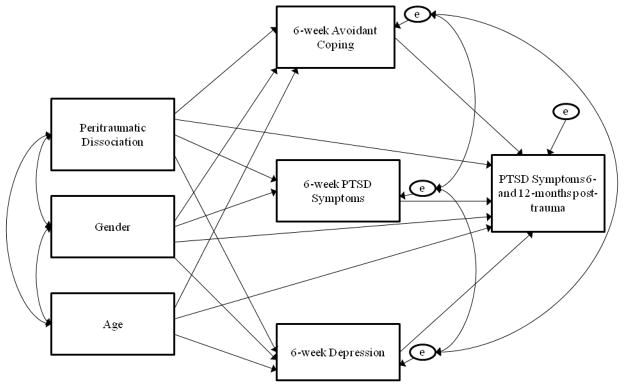
Hypothesized model examining the development of 6-month and 12-month PTSD Symptoms. This model was examined twice for each outcome (6- and 12-month PTSD Symptoms).
Note. Peritraumatic dissociation was assessed with the Peritraumatic Dissociative Experiences Questionnaire; Avoidant coping was assessed with the Brief COPE; PTSD symptoms were assessed with the Clinician Administered PTSD Scale; Depression was assessed with the Structured Clinical Interview for the DSM-IV.
Exploratory post-hoc analyses
Post-hoc multigroup analyses were conducted within AMOS to determine whether the hypothesized model performed equivalently across genders. The first step in these analyses involved estimating the hypothesized path model with no constraints across gender; all regression coefficients, correlations, and means were free to take on different values for men and women. This unconstrained model was then compared to models in which various constraints across gender were used. Comparison of the χ2 statistics of the two models determined the degree to which the constrained model parameters differed for men and women. A significant χ2 difference statistic indicated that the constraints worsened the overall fit, meaning that the genders significantly differed on the relevant model parameters. If this test was significant and revealed a better fit for the unconstrained model, it suggested that that the mediating role of avoidant coping may not be equal across genders. Though the initial multigroup analysis was performed on the proposed model (Figure 2), an adapted model was also conducted (as previously mentioned) to isolate the indirect effect of interest, and test the significance of the path from PD to PTSS through avoidant coping.
Results
Preliminary Analyses
Twenty-four participants met PTSD diagnostic criteria (9.6%) at 6-weeks, 13 (6.6%) met at 6-months, and 15 (8.5%) met at 12-months post-trauma. Relatively low rates may reflect the fact that participants were not required to meet criterion A to be included in the study. Whereas, by definition, all participants satisfied criterion A1 of PTSD due to suffering severe injuries from a potentially threatening motor vehicle accident, 67.2% met criterion A2 (subjective sense of fear, helplessness, or horror). Given relatively low rates of diagnostic PTSD levels, the present paper focused on continuous PTSS as the primary outcome variable. Diagnostic rates of depression following the motor vehicle accident were also relatively low: 31 participants (12%) met criteria at 6-weeks, 26 (13%) at 6-months, and 18 (11%) at 12-months post-trauma.
Bivariate correlations revealed statistically significant relationships among all key continuous study variables (PD, avoidant coping, and 6-week, 6-and 12-month PTSS. One-way ANOVAs also revealed statistically significant gender differences and differences between depressed and nondepressed participants on key continuous study variables (see Table 1), except for the relationship between gender and avoidant coping.
Table 1.
Descriptive Statistics and Results of One-Way ANOVA’s
| Total M (SD) |
Males M (SD) |
Females M (SD) |
F | Depressed M (SD) |
Non-Depressed M (SD) |
F | |
|---|---|---|---|---|---|---|---|
| Peritraumatic Dissociation | |||||||
| In-hospital (n = 356) | 23.58 (7.82) | 22.74 (7.67) | 24.80 (7.90) | 6.04** | - | - | - |
| Avoidant Coping | |||||||
| 6-weeks (n = 251) | 9.97 (3.29) | 9.65(3.67) | 10.24 (3.33) | 1.73 | 12.17(3.76) | 9.67(3.12) | 16.54*** |
| PTSD Symptoms | |||||||
| 6-weeks (n = 251) | 25.56 (20.79) | 20.88 (15.86) | 31.38 (24.49 | 16.54*** | 54.00 (26.65) | 21.48 (16.19) | 90.48*** |
| 6-months (n = 193) | 20.33 (19.05) | 14.78 (14.38) | 26.54 (21.64) | 20.38*** | 47.11 (26.46) | 16.21 (13.71) | 84.37*** |
| 12-months (n = 167) | 19.52 (20.33) | 14.40 (13.15) | 24.61 (25.20) | 10.97** | 48.19 (26.33) | 15.68 (16.39) | 54.15*** |
Note. Peritraumatic dissociation was assessed with the Peritraumatic Dissociative Experiences Questionnaire; Avoidant coping was assessed with the Brief COPE; PTSD symptoms were assessed with the Clinician Administered PTSD Scale; Depression was assessed with the Structured Clinical Interview for the DSM-IV.
p < .01.
p < .001.
Chi square analyses revealed that more females suffered from depression than males 6-weeks (χ2 [1, n = 248] = 15.69, p < .001) and 6-months post-trauma (χ2 [1, n = 194] = 4.12, p = .04), but this finding was not significant 12-months post-trauma (χ2 [1, n = 165] = .06, p = .81, ns). Based on these results, age, gender, 6-week PTSS, and depression were retained as covariates in multivariate analyses. Results also revealed that the inclusion versus exclusion of individuals meeting alcohol (n = 20 at 6-weeks; n = 10 at 6-months; n = 14 at 12-months) and/or substance abuse criteria (n = 5 at 6-weeks; n = 7 at 6-months; n = 8 at 12-months) and/or those who sought mental health treatment (n = 49 at 6-weeks; n = 36 at 6-months; n = 46 at 12-months) did not impact the following analyses. Injury severity scores were not significantly related to any study variables and were not retained as covariates to simplify the model.
6-month chronic PTSS
The first model tested whether avoidant coping mediated the relationship between PD and 6-month PTSS after controlling for gender, age, 6-week PTSS and depression (see Table 2). The direct path from age to depression was nonsignificant and not included in the proposed model. Model fit indices revealed that the proposed model fit the data well (χ2 [1, n = 194] = .01, p = .93, CFI = 1.00, TLI = 1.06, RMSEA = .00, 95% CI [0.00, 0.06], p = .94). Direct pathways revealed that PD positively predicted 6-week and 6-month PTSS and predicted 6-week avoidant coping and depression. Furthermore, 6-week avoidant coping and PTSS positively predicted 6-month PTSS. Results also revealed a significant overall indirect path from PD to 6-month PTSS, and after isolating the indirect pathway of PD to PTSS through avoidant coping, findings revealed that 6-week avoidant coping (β = .09, p = .01; 95% CI [0.03, 0.18]) was a significant mediator between PD and 6-month PTSS after controlling for gender, age, and 6-week depression and PTSS.
Table 2.
Direct Path Coefficients Corresponding to the 6-month PTSD Symptom (PTSS) Model
| Avoidant Copinga | 6-week PTSS | 6-week Depression | 6-month PTSS | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Predictors | B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β |
| In-hospital PD | .14(.03) | .30** | .94(.19) | .31** | .01(.00) | .17* | .32(.13) | .19* |
| Gender | .42(.44) | .06 | 9.5(2.81) | .22* | .14(.05) | .20* | 4.23(1.78) | .11* |
| Age | −.05(.01) | −.21* | −.19(.07) | −.14* | - | .00(.05) | .00 | |
| 6- week Depression | - | - | - | 7.67(4.47) | .14 | |||
| 6-week PTSS | - | - | - | .41(.09) | .50** | |||
| Avoidant Copinga | - | - | - | 1.05(.32) | .18** | |||
Note. All path coefficients were derived from bootstrapped estimates; PD = Peritraumatic Dissociation assessed with the Peritraumatic Dissociative Experiences Questionnaire; Avoidant coping was assessed with the Brief COPE; PTSS were assessed with the Clinician Administered PTSD Scale; Depression was assessed with the Structured Clinical Interview for the DSM-IV.
Avoidant Coping was assessed 6-weeks post-trauma.
p < .05.
p < .01.
p < .001.
12-month chronic PTSS
The second model tested whether avoidant coping mediated the relationship between PD and 12-month PTSS after controlling for gender, age, 6-week PTSS and 6-week depression (see Table 3). Model fit indices revealed that the proposed model adequately fit the data (χ2 [1, n = 168] = .10, p = .75, CFI = 1.00, TLI = 1.07, RMSEA =.00, 95% CI [0.00, 0.14], p = .79). PD positively predicted 6-week avoidant coping, and 6- and 12-month PTSS, but PD was not predictive of depression. Six-week avoidant coping and PTSS, but not depression, positively predicted 12-month PTSS. Given that the overall indirect path from PD to 12-month PTSS was significant, we isolated the indirect pathway of PD to 12-month PTSS through avoidant coping. Findings revealed that avoidant coping (β = .03, p = .01; 95% CI [.01 – .08]) again was a significant partial mediator between PD and 12-month PTSS after controlling for gender, age, and 6-week depression and PTSS.
Table 3.
Direct Path Coefficients Corresponding to the 12-month PTSD Symptom (PTSS) Model
| Avoidant Copinga | 6-week PTSS | 6-week Depression | 12-month PTSS | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Predictors | B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β |
| In-hospital PD | .15(.03) | .04* | .86(.20) | .28** | .01(.05) | .15+ | .38(.13) | .13** |
| Gender | .24(.50) | .04 | 9.12(3.18) | .21** | .12(.05) | .17* | 2.10(2.46) | .05 |
| Age | −.05(.02) | −.22** | −.18(.07) | −.13** | - | .18(.07) | .14* | |
| 6- week Depression | - | - | - | 4.67(5.52) | .08 | |||
| 6-week PTSS | - | - | - | .50(.11) | .53** | |||
| Avoidant Copinga | - | - | - | .92(.42) | .15* | |||
Note. All path coefficients were derived from bootstrapped estimates. PD = Peritraumatic Dissociation assessed with the Peritraumatic Dissociative Experiences Questionnaire; Avoidant coping was assessed with the Brief COPE; PTSS were assessed with the Clinician Administered PTSD Scale; Depression was assessed with the Structured Clinical Interview for the DSM-IV.
Avoidant Coping was assessed 6-weeks post-trauma.
p < .05.
p < 01.
p < .10.
Post-hoc analyses
6-month chronic PTSS
Multigroup post-hoc analyses were conducted to test whether the mediation model performed equivalently for males (n = 103) and females (n = 92). Due to issues of limited power with smaller samples, these results must be interpreted with caution. Results at 6-months revealed that the unconstrained model was a slightly better fit to the data (χ2 [2, n = 194] = 5.61, p = .08, CFI = .99, TLI = .84, RMSEA =.09, 95% CI [0.00, 0.19], p = .18) than the constrained model (χ2 [5, n = 194] = 13.52, p = .02, CFI = .97, TLI = .82, RMSEA =.09, 95% CI [0.04, 0.16], p = .10) which forced the 3 pathways between PD and avoidant coping, PD and 6-month PTSS, and avoidant coping and 6-month PTSS, to be equal. Analysis of model comparison revealed a marginally significant difference between the constrained versus the unconstrained model (Δχ2 [3, n = 194] = 7.08, p = .07). Given the exploratory nature of these analyses, and to inform future study designs, we conducted post hoc analyses on this finding. Results from the unconstrained model revealed that PD positively predicted PTSS 6- weeks post-trauma for both females (β = .39, p = .02) and males (β = .21, p = .02) but not 6-months post-trauma for females or males. PD was positively related to avoidant coping for females (β = .14, p = .01), but not for males (β = .18, p = .09). Further, avoidant coping positively predicted PTSS at 6-months (β = .29, p = .01) in females but not males. We then isolated the indirect pathway of PD to 6-month PTSS through avoidant coping, and findings revealed that this indirect pathway was significant for females (β = .07, p = .01 [CI 95% = .01 – .08]) but not for males. Therefore, results suggested that avoidant coping served as a significant partial mediator between PD and 6-month PTSS after controlling for age, and 6-week depression and PTSS for females, but not for males.
12-months chronic PTSS
Twelve-months post-trauma (ns = 89 males and 80 females), results revealed a poor fit for both the unconstrained model (χ2 [2, n = 168] = 6.15, p = .05, CFI = .98, TLI = .76, RMSEA =.11, 95% CI [0.01, 0.11], p = .11) and the constrained model (χ2 [5, n = 168] = 12.23, p = .03, CFI = .97, TLI = .83, RMSEA =.09, 95% CI [0.03, 0.16], p = .12). Analysis of model comparison revealed no differences between the unconstrained and the constrained models (Δχ2 [3, n = 168] = 6.08, p = .11), implying that the hypothesized model functioned equivalently for both males and females 12-months post-trauma.
Discussion
Results of this study support prior findings that higher PD was associated with greater avoidant coping 6-weeks post-trauma and with greater 6- and 12-month chronic PTSS. Further, higher levels of avoidant coping were related to greater PTSS at both time points. The present results extend prior findings by demonstrating that avoidant coping acted as a partial mechanism through which initial PD may lead to persistent PTSS in a longitudinal model, after controlling for gender, age, depression, and 6-week PTSS.
Although the analyses were exploratory, and the principle analysis was marginally significant, the finding that avoidant coping mediated the relationship between PD and 6-month PTSS for females but not for males, suggests avenues for further attention. These results are consistent with findings that females experience greater PD and PTSS than males (see Tolin & Foa, 2006). Further, despite the lack of gender differences in avoidant coping in our sample, the interaction of gender and PD was associated with greater risk for chronic PTSS in females than in males. These results provide further support for the utility of PD and for the importance of examining gender differences in studies of PTSS risk factors.
As PD occurs, by definition, during a trauma, interventions designed to reduce PD are difficult to conceptualize. Further, research has suggested that immediate interventions such as critical incident stress debriefing are at best ineffective and, at worse, may increase PTSS (Bisson, Jenkins, Alexander, & Bannister, 1997). Therefore, prevention strategies may be the only way to directly impact PD. Coping, unlike PD, is an ongoing process which lends itself easily to intervention (Aldwin & Yancura, 2004; Olff, Langeland, & Gersons, 2005).
Early interventions designed to moderate maladaptive coping (especially in females who experience high PD) may aid in preventing and/or reducing subsequent PTSS. Replication of this finding may lend further support for the efficacy of addressing maladaptive coping behaviors specifically in high dissociators. Interventions that encourage the use of approach coping may buffer the risk of developing PTSS by encouraging victims to actively cope with trauma-related thoughts (Jex, Bliese, Buzzell, & Primeau, 2001) and repair the fragmented memories created by the trauma.
The present results extend prior findings by not only suggesting mechanisms through which PD relates to PTSS, but also by highlighting the need for exploring additional mediating and moderating variables (e.g., gender) that may interact with risk factors to predict subsequent PTSS. Further, in contrast to prior research that incorporated retrospective reports of dissociation that may be less reliable (Marshall & Schell, 2002), the present study included an assessment of PD shortly after the traumatic event. PTSS were also assessed via gold-standard interview rather than via questionnaire. Finally, previous studies examined mediators of the relationship between PD and PTSS with cross-sectional designs. The longitudinal design of the present study provides further evidence for a possible causal relationship between PD and PTSS. Though identification of individuals at the highest risk for PTSS may not be determined until weeks post-trauma after the coping process has been established, this method may efficiently capture those individuals relatively early on who are likely to develop chronic PTSS.
A level of caution should be exercised when viewing the present results in light of some limitations, including the use of a number of interviewers, and not correcting significance levels for multiple testing. Though a relatively homogenous sample of motor vehicle accident victims contributes to the study’s internal validity, it is unknown whether these results would generalize to victims of other types of traumas. Further, given the relatively low endorsement of avoidant coping and PTSS in this sample, it is unclear whether these results would generalize to a more symptomatic sample. As mentioned, our lower rates of diagnostic PTSD may reflect the fact that we did not require endorsement of criterion A as an inclusionary criterion; it is unclear whether the results would apply to samples of trauma victims that all endorsed criterion A. Future studies should assess whether avoidant coping remains a mediator between PD and PTSS in a more symptomatic sample (e.g., a clinical, treatment-seeking sample), as a more complex set of mediators may better serve to explain this relationship when PTSS are experienced to a greater degree.
Further, our sample suffered from a high rate of participant attrition, and a greater number of male participants and participants with high PD discontinued participation. This differential drop out may have especially impacted our post-hoc findings given that the mediation results were nonsignificant in males 6-months post-trauma. It is unclear whether avoidant coping would have remained a partial mediator in male participants who experienced higher levels of dissociation, had sufficient numbers been retained. Alternatively, it is possible that the overall results would have been more robust if more males and higher dissociators had remained in the study. Despite these limitations, results from this study provide support for the utility of PD as an early risk factor for persistent PTSS, and for avoidant coping as a possible mechanism by which chronic PTSS results from PD.
References
- Aldwin C, Yancura LA. Coping and health: A comparison of the stress and trauma literatures. In: Schnurr PP, Green BL, editors. Physical health consequences of exposure to extreme stress. Washington, D.C: American Psychological Association; 2005. pp. 99–126. [Google Scholar]
- Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma-Injury Infection and Critical Care. 1974;14:187–196. Retrieved from http://journals.lww.com/jtrauma/pages/default.aspx. [PubMed] [Google Scholar]
- Bal S, van Oost P, De Bourdeaudhuij I, Crombez G. Avoidant coping as a mediator between self-reported sexual abuse and stress-related symptoms in adolescents. Child Abuse and Neglect. 2003;27:883–897. doi: 10.1016/So145-2134(03)00137-6. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The Moderator-Mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bentler PM. EQS 6 Structural Equations Program Manual. Encino, CA: Multivariate Software, Inc; 2004. [Google Scholar]
- Bisson JI, Jenkins PL, Alexander J, Bannister C. Randomized controlled trial of psychological debriefing for victims of acute burn trauma. British Journal of Psychiatry. 1997;171:78–81. doi: 10.1192/bjp.171.1.78. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupeck DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Breh DC, Seidler GH. Is peritraumatic dissociation a risk factor for PTSD? Journal of Trauma and Dissociation. 2007;8:53–69. doi: 10.1300/J229v08n01_04. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG. Avoidant coping style and post-traumatic stress following motor vehicle accidents. Behavior Research and Therapy. 1995;33:631–635. doi: 10.1016/0005-7967(94)00093-Y. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Collins FE, Ffrench CH. Dissociation, coping strategies, and locus-of-control in a non-clinical population: Clinical implications. Australian Journal of Clinical and Experimental Hypnosis. 1998;26:113–126. Retrieved from http://www.ozhypnosis.com.au/ [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:319–345. doi: 10.1016/S0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- Engelhard IM, van den Hout MA, Kindt M, Arntz A, Schouten E. Peritraumatic dissociation and posttraumatic stress after pregnancy loss: a prospective study. Behaviour Research and Therapy. 2003;41:67–78. doi: 10.1016/S0005-7967(01)00130-9. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Personality Disorders, (SCID-II) Washington, D.C: American Psychiatric Press, Inc; 1997. [Google Scholar]
- Foa EB, Steketee G, Rothbaum BO. Behavioral and cognitive conceptualizations of post-traumatic stress disorder. Behavior Therapy. 1989;20:155–176. doi: 10.1016/S0005-7894(89)80067-X. [DOI] [Google Scholar]
- Folkman S, Lazarus RS. Coping as a mediator of emotion. Journal of Personality and Social Psychology. 1988;54:466–475. doi: 10.1037//0022-3514.54.3.466. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gershuny BS, Cloitre M, Otto MW. Peritraumatic dissociation and PTSD severity: do event related fears about death and control mediate their relation? Behaviour Research and Therapy. 2003;41:157–166. doi: 10.1016/S0005-7967(01)00134-6. [DOI] [PubMed] [Google Scholar]
- Jex SM, Bliese PD, Bezzell S, Primeau J. The impact of self efficacy on stressor-strain relations: coping style as an explanatory mechanism. Journal of Applied Psychology. 2001;86:401–409. doi: 10.1037/0021-9010.86.3.401. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and Why Criteria Defining Moderators and Mediators Differ Between the Baron & Kenny and MacArthur Approaches. Health Psychology. 2008;27:S101–S108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, Dutton MA. Avoidant coping and PTSD symptoms related to domestic violence exposure: A longitudinal study. Journal of Traumatic Stress. 2008;21:83–90. doi: 10.1002/jts.20288. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. From psychological stress to the emotions: a history of changing outlooks. Annual Reviews of Psychology. 1993;44:1–21. doi: 10.1146/annurev.ps.44.020193.000245. [DOI] [PubMed] [Google Scholar]
- Lensvelt-Mulders G, van der Hart O, van Ochten JM, van Son MJM, Steele K, Breeman L. Relations among peritraumatic dissociation and posttraumatic stress: A meta-analysis. Clinical Psychology Review. 2008;28:1138–1151. doi: 10.1016/j.cpr.2008.03.006. [DOI] [PubMed] [Google Scholar]
- Marmar CR, Weiss DS, Metzler TJ. The peritraumatic dissociative experiences questionnaire. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; 1997. pp. 412–428. [Google Scholar]
- Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL. Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. American Journal of Psychiatry. 1994;151:902–907. doi: 10.1176/ajp.151.6.902. Retrieved from http://ajp.psychiatryonline.org/ [DOI] [PubMed] [Google Scholar]
- Marshall GN, Schell TL. Reappraising the link between peritraumatic dissociation and PTSD symptom severity: Evidence from a longitudinal study of community violence survivors. Journal of Abnormal Psychology. 2002;111:626–636. doi: 10.1037/0021843X.111.4.626. [DOI] [PubMed] [Google Scholar]
- Marx BP, Sloan DM. Peritraumatic dissociation and experiential avoidance as predictors of posttraumatic stress symptomatology. Behaviour Research and Therapy. 2005;43:549–583. doi: 10.1016/j.brat.2004.04.004. [DOI] [PubMed] [Google Scholar]
- Nunnally JC. Introduction to psychological measurement. New York: McGraw-Hill; 1970. [Google Scholar]
- Olff M, Langeland W, Gersons BPR. The psychobiology of PTSD: Coping with trauma. Psychoneuroendocrinology. 2005;30:974–982. doi: 10.1016/j.psyneuen.2005.04.009. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- Rachman S. Fear and courage. 2. New York: Freeman; 1990. [Google Scholar]
- Regambal MJ, Alden LE. Pathways to intrusive memories in a trauma analogue paradigm: A structural equation model. Depression and Anxiety. 2009;26:155–166. doi: 10.1002/da.20483. [DOI] [PubMed] [Google Scholar]
- Teasdale G, Jennett D. Assessment of coma and impaired consciousness. Lancet. 1974;2:81–84. doi: 10.1016/S0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132:959–992. doi: 10.1037/1942-9681.S.1.37. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Townsend SM, Filipas HH, Starzynski LL. Structural models of the relations of sexual assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychology of Women Quarterly. 2007;31:23–37. doi: 10.1111/j.1471-6402.2007.00328.x. [DOI] [Google Scholar]
- van der Hart O, Nijenhuis E, Steele K, Brown D. Trauma-related dissociation: conceptual clarity lost and found. Australian and New Zealand Journal of Psychiatry. 2004;38:906–914. doi: 10.1111/j.1440-1614.2004.01480.x. [DOI] [PubMed] [Google Scholar]
- van der Veldon PG, Wittmann L. The independent predictive value of peritraumatic dissociation for PTSD symptomology after type I trauma: A systematic review of prospective studies. Clinical Psychology Review. 2008;28:1009–1020. doi: 10.1016/j.cpr.2008.02.006. [DOI] [PubMed] [Google Scholar]
- Wong M, Looney E, Michaels J, Palesh O, Koopman C. A preliminary study of peritraumatic dissociation, social support, and coping in relation to posttraumatic stress symptoms for a parent’s cancer. Psycho-oncology. 2006;15:1093–1098. doi: 10.1002/pon. [DOI] [PubMed] [Google Scholar]