Abstract
Objective
The World Health Organization (WHO) reports that nonsmokers experience disease and death due to secondhand smoke (SHS) exposure in the home. We estimated the total excess burden and costs to society due to SHS exposure in U.S. public housing.
Methods
We quantified the public health burden for outcomes causally related to SHS exposure for nationally representative never-smoking residents in U.S. public housing using (1) WHO-recommended health outcomes and methodology, (2) publicly available and other large databases, and (3) published estimates of morbidity and mortality rates. We used published estimates of direct medical and nonmedical care costs and the value of productivity losses to estimate SHS-related societal costs for disease and death. We estimated the public health and economic burden for two serum cotinine limits of detection (LODs): 0.05 nanograms per milliliter (ng/mL) and 0.015 ng/mL.
Results
In 2011, an estimated 37,791 never-smoking child and adult U.S. public housing residents experienced illness and death due to SHS exposure at home based on an LOD=0.05 ng/mL (50,967 residents at LOD=0.015 ng/mL). Costs incurred by society for these illnesses and deaths totaled $183 million (LOD=0.05 ng/mL) and $267 million (LOD=0.015 ng/mL) annually. Of the total costs, direct costs (medical and nonmedical) accounted for $128 million and $176 million for LOD=0.05 ng/mL and LOD=0.015 ng/mL, respectively. Medical care accounted for the majority of direct costs—$110 million at LOD=0.05 ng/mL and $153 million at LOD=0.015 ng/mL. Adverse respiratory health outcomes accounted for approximately one-half (56% at LOD=0.05 ng/mL and 52% at LOD=0.015 ng/mL) of total societal costs.
Conclusion
Implementing smoke-free policies in all U.S. public housing could save lives and decrease SHS-related morbidity and mortality in never-smoking residents, resulting in annual societal savings of $183 million at LOD=0.05 ng/mL and $267 million at LOD=0.015 ng/mL.
An estimated 15%–18% of U.S. children are exposed to secondhand smoke (SHS) at home.1 SHS is a major cause of disease, and there is no safe level of SHS exposure.1,2 Children and nonsmoking adults living below the federal poverty level (FPL) are more likely to be exposed to SHS than those in higher socioeconomic status households.3 Children are especially vulnerable because their exposure patterns and developmental status enhance absorption of environmental toxicants.4 Additionally, because many elderly people with limited mobility live in public housing, they may spend more time indoors, be exposed to more SHS, and suffer more severe adverse health outcomes than the general population.2 People with disabilities comprise nearly one-third of the public housing population and have greater SHS exposure than those without a disability.5,6 Because SHS migrates, residents of multiunit housing who do not allow smoking in their home are at risk for SHS exposure if other residents in their building smoke.7 SHS migration has implications for nonsmoking public housing residents, as 88% of public housing is multiunit.8
The World Health Organization (WHO) reports that there is sufficient evidence of causal relationships between SHS and adverse health outcomes, including lung cancer, heart disease, and asthma in adults; and low birthweight (LBW) (i.e., birthweight ≤2,500 grams), sudden infant death syndrome (SIDS), and lower respiratory infections (LRIs)—including respiratory syncytial virus, bronchitis, otitis media (OM), and asthma—in children.2
Smoke-free policies significantly reduce adverse health outcomes caused by SHS.9–13 In 2009 and 2012, the U.S. Department of Housing and Urban Development (HUD) encouraged public housing authorities to implement smoke-free policies in subsidized housing.14,15 Recent research suggests that smoke-free policies are supported by a majority of never- and former-smoking subsidized housing residents and are associated with cessation or lower rates of smoking among smokers.16,17 Recent data indicate that in 2013, more than 300 housing authorities had instituted smoke-free policies.18,19
The health and economic consequences of childhood SHS exposure in the United States are well documented,20–28 but similar analyses are not available for nonsmoking adults. While there are published estimates of the U.S. public health burden associated with SHS exposure in adults and state-level economic studies on SHS that include nonsmoking adults, information on the national aggregate costs of SHS-related health effects in adults is sparse.29–36
A recent study estimated SHS-related costs in all government-subsidized housing using state-level estimates.37 However, to our knowledge this is the first study to estimate the public health and economic burden of SHS in public housing based on nationally representative and other large-scale databases, including biomarker data. Quantifying the burden of SHS for residents may provide incentives to institute smoke-free policies in public housing.
METHODS
We used methods described by the WHO to estimate the annual public health burden for new cases (i.e., incidence) of SHS-attributable illness and death for adult and child never-smoker U.S. public housing residents.2,38 When the number of incident cases was unavailable, we used self-reported (asthma) or treated (OM and LRI) prevalence rates. We based population-attributable fractions (PAFs) and attributable burdens for each health outcome on WHO estimates of relative risk (RR). We then estimated annual societal economic burdens for each health outcome and overall using previously described methods.39
Public housing never smokers
We estimated the number of adult never smokers by multiplying the national percentage of adult never smokers with a household income ≤200% FPL by the number of adults living in public housing (Personal communication, Lydia Taghavi, HUD, February 2012). We used the national prevalence of middle school and high school never smokers from the 2009 National Youth Tobacco Survey to estimate the number of never smokers among public housing adolescents because data stratified by family income or housing type were not available. We defined adults and adolescents aged 11–17 years as never smokers if they reported lifetime consumption of ≤99 cigarettes and either had not smoked (adults) or used any tobacco products (adolescents) in the past 30 days. All children <11 years of age were considered never smokers. We used the proportion of adult never smokers receiving government housing assistance in the 2010 National Health Interview Survey (NHIS) as a proxy for the proportion of adult public housing never smokers. However, government housing assistance is overreported in NHIS; therefore, we further limited NHIS never-smoker data extracted to those who reported both government-subsidized housing and a household income ≤200% FPL.40
Exposure to SHS
We used the national percentage of current nonsmokers with detectible serum cotinine levels who participated in the 2007–2008 and 2009–2010 cycles of the National Health and Nutrition Examination Survey (NHANES) to estimate the proportion of adults and children exposed to SHS. Because NHANES participants are not asked if they live in government-assisted housing, we used SHS-exposed nonsmokers in NHANES with a reported income ≤130% FPL guidelines as a proxy for the nonsmoking public housing population. We classified adults ≥20 years of age with a serum cotinine concentration >the limit of detection (LOD) but ≤10 nanograms per millimeter (ng/mL) who did not report being a current cigarette smoker or having used any nicotine-containing products within the previous five days as nonsmokers.3 We defined SHS-exposed nonsmoking adolescents as those aged 12–19 years who reported no smoking in the previous 30 days, no use of any nicotine-containing product within the previous five days, and a serum cotinine level >LOD but ≤10 ng/mL. All children aged 3–11 years were classified as SHS-exposed if their cotinine level was >LOD but ≤10 ng/mL. Serum cotinine is not measured in NHANES participants <3 years of age. SHS exposure prevalence for these children was assumed to be the same as in children aged 3–11 years.41 We present results based on the current serum cotinine LOD=0.015 ng/mL as well as the historically important LOD=0.05 ng/mL to allow comparisons with previous work.
Disease status
We derived incidence, prevalence, and mortality rates for both adult and child health outcomes causally related to SHS exposure from sources listed in Tables 1 and 2. We multiplied each disease/mortality rate by the relevant number of never smokers living in public housing to estimate the number of never-smoking residents with each health outcome of interest. We estimated the public health burden attributable to SHS for each health outcome by calculating a PAF using the RR estimated by WHO (Tables 1 and 2).2 We used SAS® version 9.2 and SUDAAN® release 10.0 to calculate population-based estimates.42,43
Table 1.
Annual SHS-attributable morbidity and mortality of adult never smokers residing in U.S. public housing, 2011
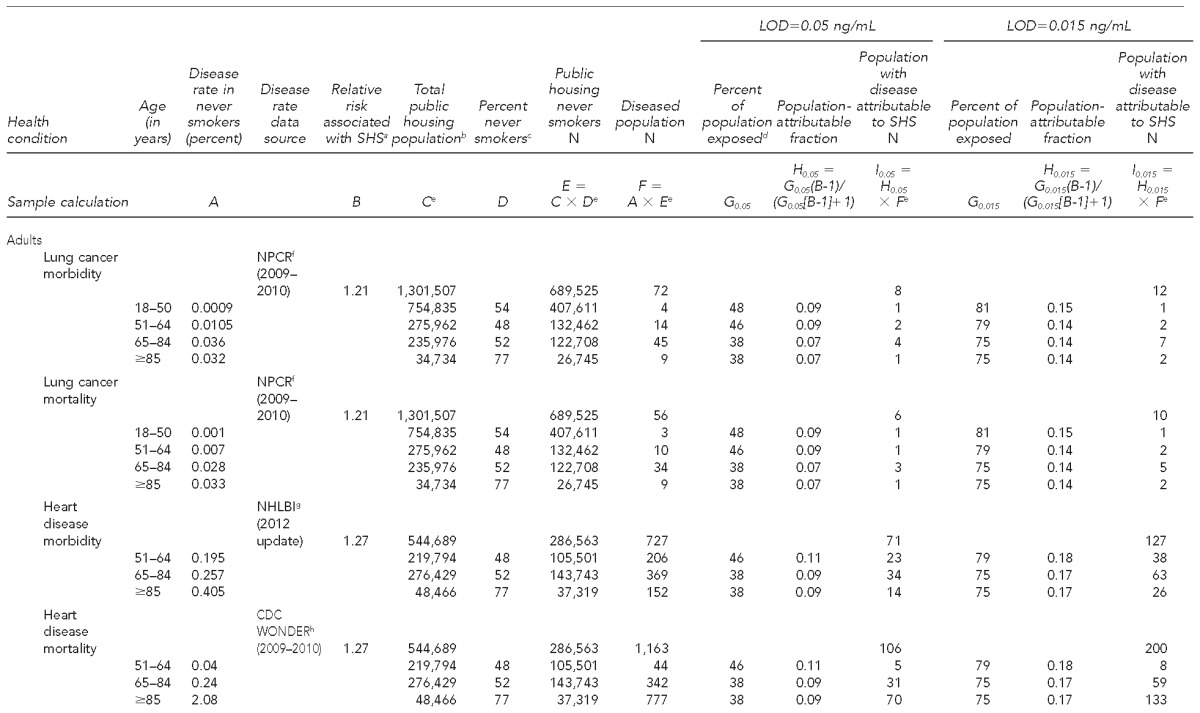
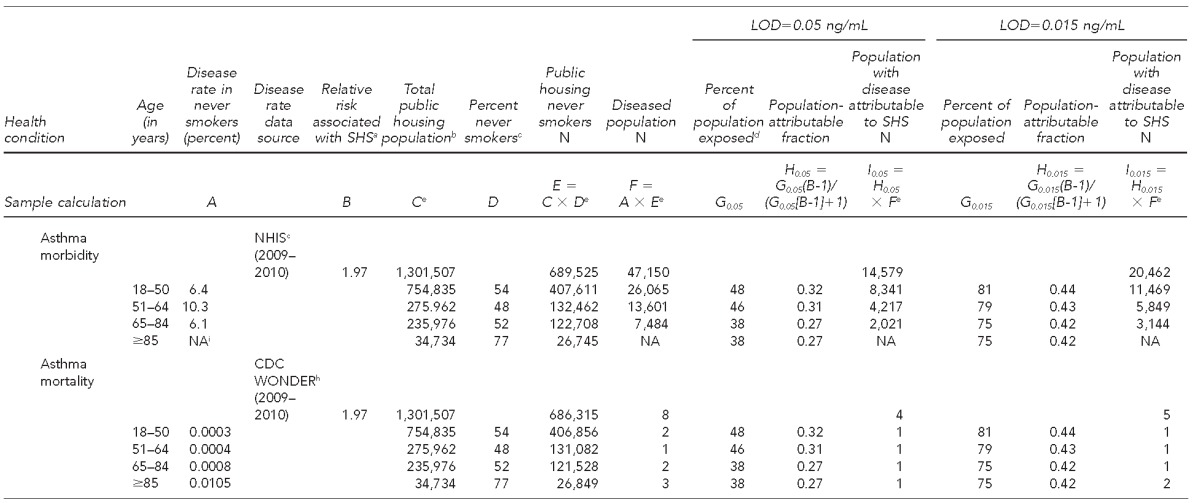
aÖberg M, Jaakkola MS, Prüss-Üstün A, Schweizer C, Woodward A. Second-hand smoke: assessing the burden of disease at national and local levels. Geneva: World Health Organization; 2010.
bUnpublished data: personal communication, Lydia Taghavi, U.S. Department of Housing and Urban Development, February 2012
cData extracted from: Centers for Disease Control and Prevention (US). National Health Interview Survey 2009 data release [cited 2014 Feb 11]. Available from: URL: http://www.cdc.gov/nchs/nhis/nhis_2009_data_release.htm
dData extracted from: National Center for Health Statistics (US). National Health and Nutrition Examination Survey questionnaires, datasets and related documentation [cited 2014 Mar 10]. Available from: URL: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm
eSummed values may not add to totals due to rounding.
fCenters for Disease Control and Prevention (US). CDC WONDER: National Program of Cancer Registries Early Release publication information data: incidence 1999–2010 [cited 2014 Feb 25]. Available from: URL: http://wonder.cdc.gov/wonder/help/cancernpcr.html
gRoger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011;123:e18-e209.
hCenters for Disease Control and Prevention (US). CDC WONDER: underlying cause of death 1999–2013 [cited 2014 Apr 1]. Available from: URL: http://wonder.cdc.gov/wonder/help/ucd.html
iInsufficient sample size to obtain a reliable estimate
SHS = secondhand smoke
LOD = limit of detection
ng/mL = nanograms per milliliter
NPCR = National Program of Cancer Registries
NHLBI = National Heart, Lung, and Blood Institute
CDC = Centers for Disease Control and Prevention
WONDER = Wide-ranging Online Data for Epidemiologic Research
NHIS = National Health Interview Survey
NA = not applicable
Table 2.
Annual SHS-attributable morbidity and mortality of child never smokers residing in U.S. public housing, 2011
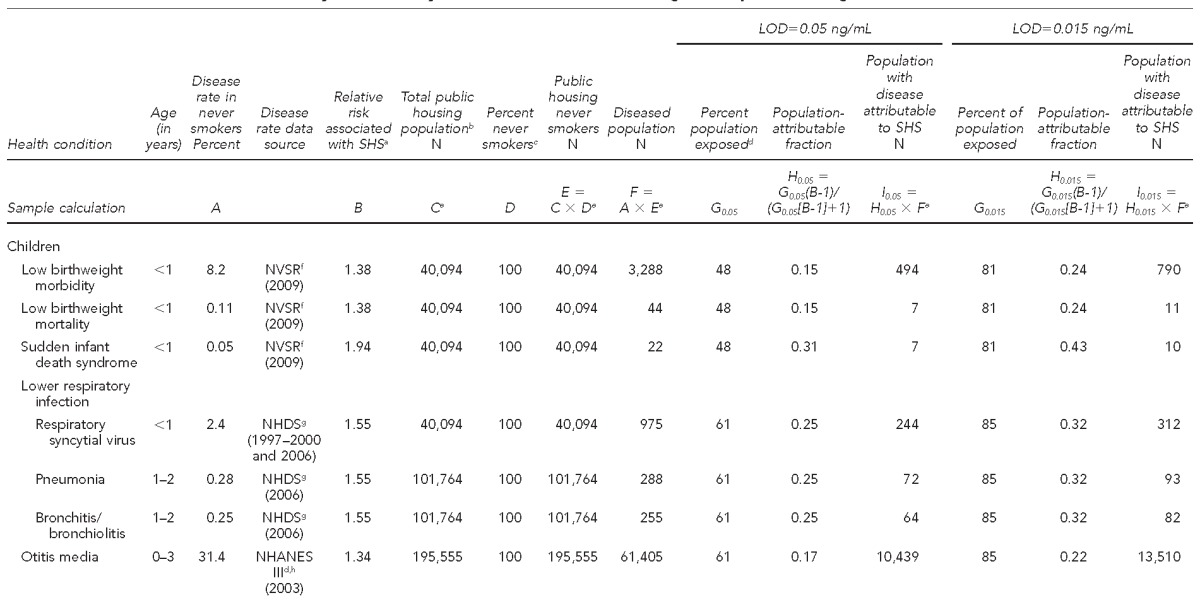
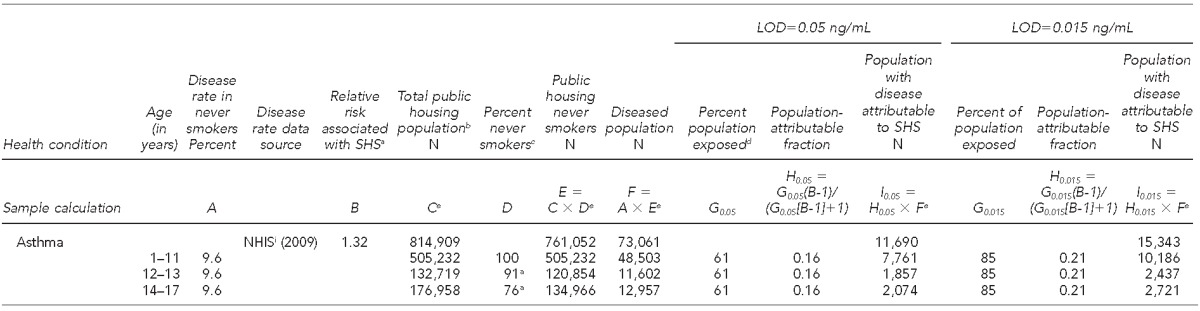
aÖberg M, Jaakkola MS, Prüss-Üstün A, Schweizer C, Woodward A. Second-hand smoke: assessing the burden of disease at national and local levels. Geneva: World Health Organization; 2010.
bUnpublished data: personal communication, Lydia Taghavi, U.S. Department of Housing and Urban Development, February 2012
cData extracted from: Centers for Disease Control and Prevention CDC (US), Office on Smoking and Health. National Youth Tobacco Survey (NYTS) 2009 [cited 2012 Jun 15]. Available from: URL: http://www.cdc.gov/tobacco/data_statistics/surveys/nyts/index.htm. The NYTS captures smoking status by status in school (i.e., middle or high school). For children >11 years of age, we assumed children aged 12–13 years were in middle school and those aged ≥14 years were in high school.
dData extracted from: National Center for Health Statistics (US). National Health and Nutrition Examination Survey III questionnaires, datasets and related documentation [cited 2014 Mar 10]. Available from: URL: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm
eSummed values may not add to totals due to rounding.
fHamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2009. Natl Vital Stat Rep 2010 Dec 21;59:1-19. Also available from: URL: http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_02.pdf [cited 2014 Feb 19].
gNational Center for Health Statistics (US). National Hospital Discharge Survey, 1997–2000 and 2006 [cited 2015 Feb 4]. Available from: URL: http://www.cdc.gov/nchs/nhds/nhds_publications.htm
hPublished estimate in: Auinger P, Lanphear BP, Kalkwarf HJ, Mansour ME. Trends in otitis media among children in the United States. Pediatrics 2003;112:514-20.
iNational Center for Health Statistics (US). 2009 National Health Interview Survey public-use data release. Hyattsville (MD): NCHS; 2010.
SHS = secondhand smoke
LOD = limit of detection
ng/mL = nanograms per milliliter
NVSR = National Vital Statistics Report
NHDS = National Hospital Discharge Survey
NHANES III = National Health and Nutrition Examination Survey III
NHIS = National Health Interview Survey
Estimates of costs of health outcomes
We conducted a literature search using PubMed, Google, and Google Scholar to identify treatment costs for each health outcome considered in our analysis. Keywords included “asthma,” “cost,” “cardiovascular disease,” “coronary heart disease,” “coronary artery disease,” “economic burden,” “ischemic heart disease,” “lower respiratory infection,” “low birthweight,” “lung cancer,” “myocardial infarction,” “otitis media,” “respiratory syncytial virus,” “secondhand smoke,” “smoke inhalation,” and “sudden infant death syndrome.” We took a societal perspective and included all costs for treatment of the health outcomes, regardless of who accrued the cost. Depending on costs considered in the source studies used, we accounted for direct costs (i.e., medical costs including hospitalizations, physician's visits, and medications; and nonmedical costs including travel and paid childcare) and/or productivity losses (e.g., caregiver time lost from work or school due to a patient's illness)(Table 3).44
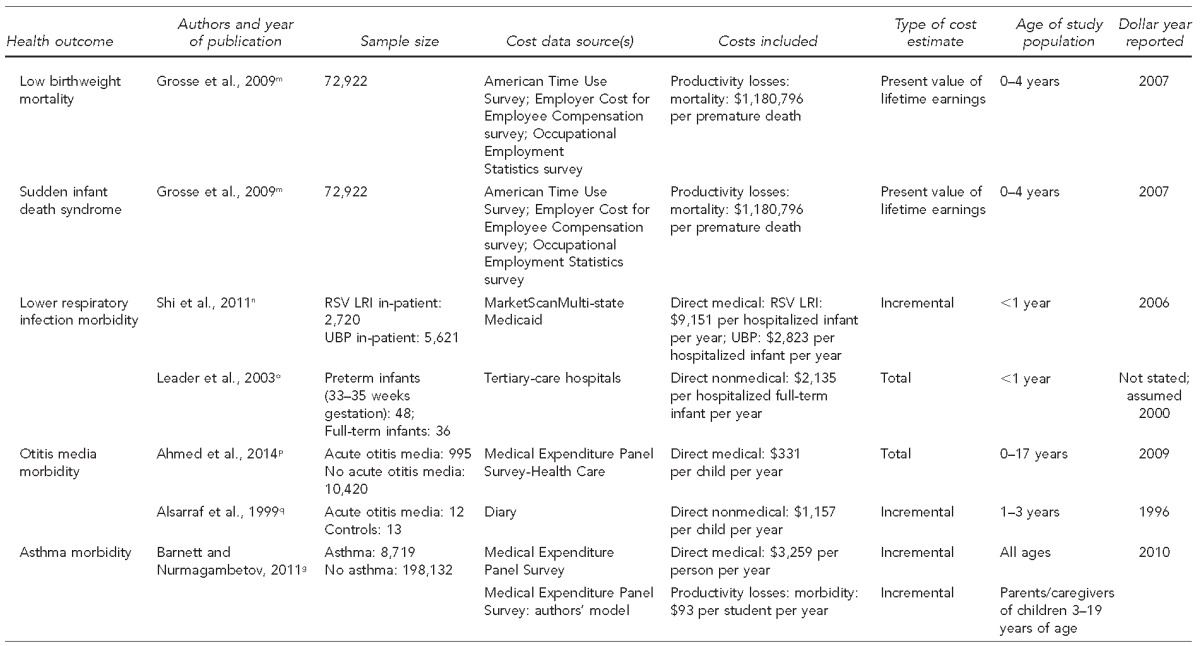
Table 3.
Source articles for cost data and selected source article study characteristics on SHS-attributable health outcomes in the U.S.
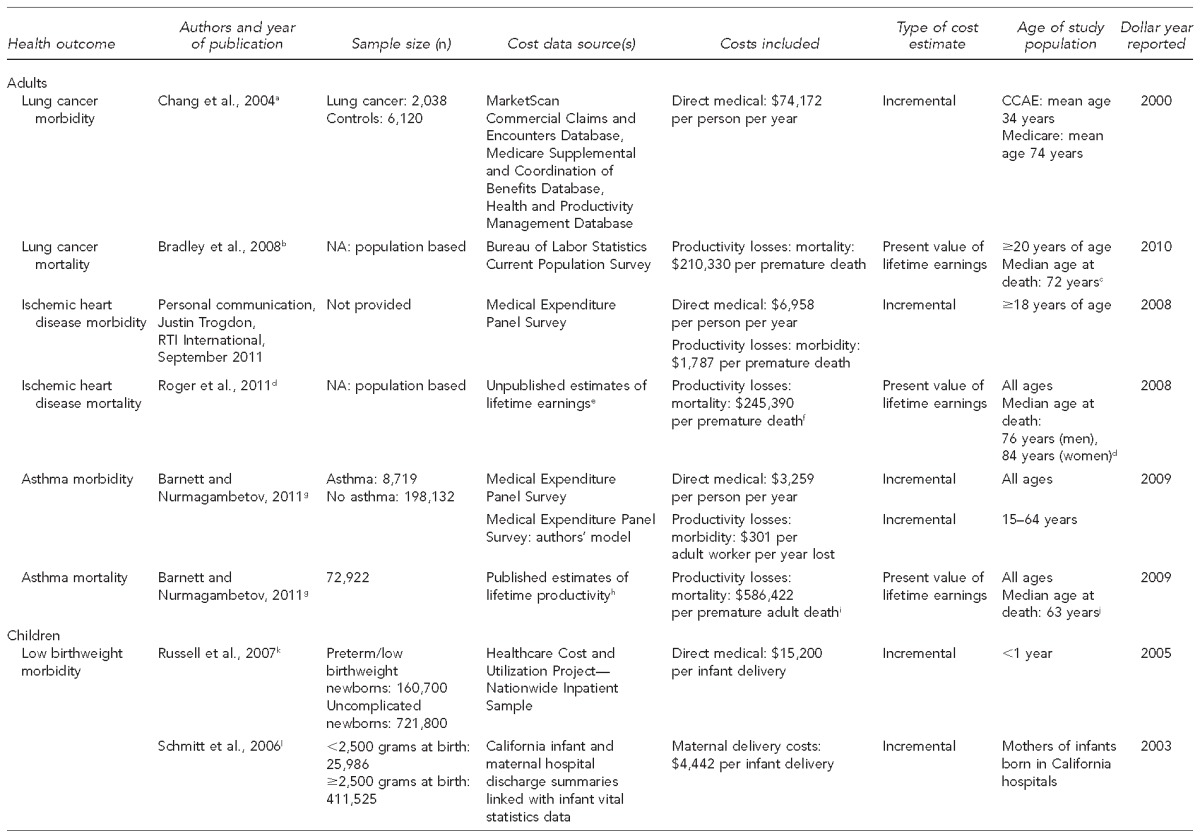
aChang S, Long SR, Kutikova L, Bowman L, Finley D, Crown WH, et al. Estimating the cost of cancer: results on the basis of claims data analyses for cancer patients diagnosed with seven types of cancer during 1999 to 2000. J Clin Oncol 2004;22:3524-30.
bBradley CJ, Yabroff KR, Dahman B, Feuer EJ, Mariotto A, Brown ML. Productivity costs of cancer mortality in the United States: 2000–2020. J Natl Cancer Inst 2008;100:1763-70.
cLung cancer median age at death from Surveillance, Epidemiology, and End Results (SEER) stat fact sheets/lung and bronchus [cited 2014 Mar 12]. Available from: URL: www.seer.cancer.gov
dRoger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011;123:e18-e209.
dKelly BB, Fuster V, editors. Promoting cardiovascular health in the developing world: a critical challenge to achieve global health. Washington: National Academies Press; 2010.
eProvided by the National Heart, Lung, and Blood Institute to the American Heart Association
fCalculated by authors based on published costs due to lost productivity (mortality) in: Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011;123:e18-e209, and the number of ischemic heart disease deaths from: Kochanek KD, Xu J, Murphy SL, Minino AM, Kung H-C. Deaths: final data for 2009. Natl Vital Stat Rep 2011 Dec 29;60:1-117.
gBarnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002–2007. J Allergy Clin Immunol 2011;127:145-52.
hCosts were adapted from data presented in: Grosse SD, Krueger KV, Mvundura M. Economic productivity by age and sex: 2007 estimates for the United States. Med Care 2009;47(7 Suppl 1):S94-103.
iCalculated by the authors based on ages and mortality costs for those aged ≥15 years presented in: Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002–2007. J Allergy Clin Immunol 2011;127:145-52.
jCalculated by the authors from number and age of asthma-related deaths published in: Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002–2007. J Allergy Clin Immunol 2011;127:145-52.
kRussell RB, Green NS, Steiner CA, Meikle S, Howse JL, Poschman K, et al. Cost of hospitalization for preterm and low birthweight infants in the United States. Pediatrics 2007;120:e1-9.
lSchmitt SK, Sneed L, Phibbs CS. Costs of newborn care in California: a population-based study. Pediatrics 2006;117:154-60.
mGrosse SD, Krueger KV, Mvundura M. Economic productivity by age and sex: 2007 estimates for the United States. Med Care 2009;47(7 Suppl 1):S94-103.
nShi N, Palmer L, Chu BC, Katkin JP, Hall CB, Masaquel AS, et al. Association of RSV lower respiratory tract infection and subsequent healthcare use and costs: a Medicaid claims analysis in early-preterm, late-preterm, and full-term infants. J Med Econ 2011;14:335-40.
oLeader S, Yang H, DeVincenzo J, Jacobson P, Marcin JP, Murray DL. Time and out-of-pocket costs associated with respiratory syncytial virus hospitalization of infants. Value Health 2003;6:100-6.
pAhmed S, Shapiro NL, Bhattacharyya N. Incremental health care utilization and costs for acute otitis media in children. Laryngoscope 2014;124:301-5.
qAlsarraf R, Jung CJ, Perkins J, Crowley C, Alsarraf NW, Gates GA. Measuring the indirect and direct costs of acute otitis media. Arch Otolaryngol Head Neck Surg 1999;125:12-8.
SHS = secondhand smoke
CCAE = Commercial Claims and Encounters
NA = not applicable
RSV = respiratory syncytial virus
LRI = lower respiratory infection
UBP = unspecified bronchiolitis/pneumonia
We applied monetary valuations for morbidity-related productivity losses for all adult health outcomes, but only for asthma in children (Table 3). We used only published estimates of data from the United States.45 We valued premature loss of life as the present value of lifetime economic productivity.46,47 We used a human capital approach behind a “veil of ignorance” (i.e., productivity losses due to morbidity were based on annual costs using national average wages).48 We excluded costs associated with premature death when such deaths were rare events and did not contribute substantially to the societal burden resulting from SHS exposure in public housing.
Because excess expenditures better estimate the potential cost savings of policies aimed at reducing adverse health outcomes, we calculated costs for each health outcome by multiplying per-person excess costs by number of never smokers impacted.49 We summed these costs to derive total aggregated costs for all health outcomes. We used the personal consumption health care expenditure index to adjust direct medical costs and the gross domestic product index to adjust productivity losses and nonmedical direct costs to 2011 dollars.
RESULTS
In 2011, exposure to SHS resulted in morbidity or mortality in 37,791 (at LOD=0.05 ng/mL) and 50,967 (at LOD=0.015 ng/mL) never-smoking U.S. public housing residents. SHS caused the premature death of 14 (at LOD=0.05 ng/mL) and 21 (at LOD=0.015 ng/mL) infant U.S. public housing residents, and 116 (at LOD=0.05 ng/mL) and 215 (at LOD=0.015 ng/mL) adult U.S. public housing residents (Table 4).
Table 4.
Estimates of annual public health burden and societal costs of SHS-attributable health outcomes for child and adult never smokers in U.S. public housing, 2011
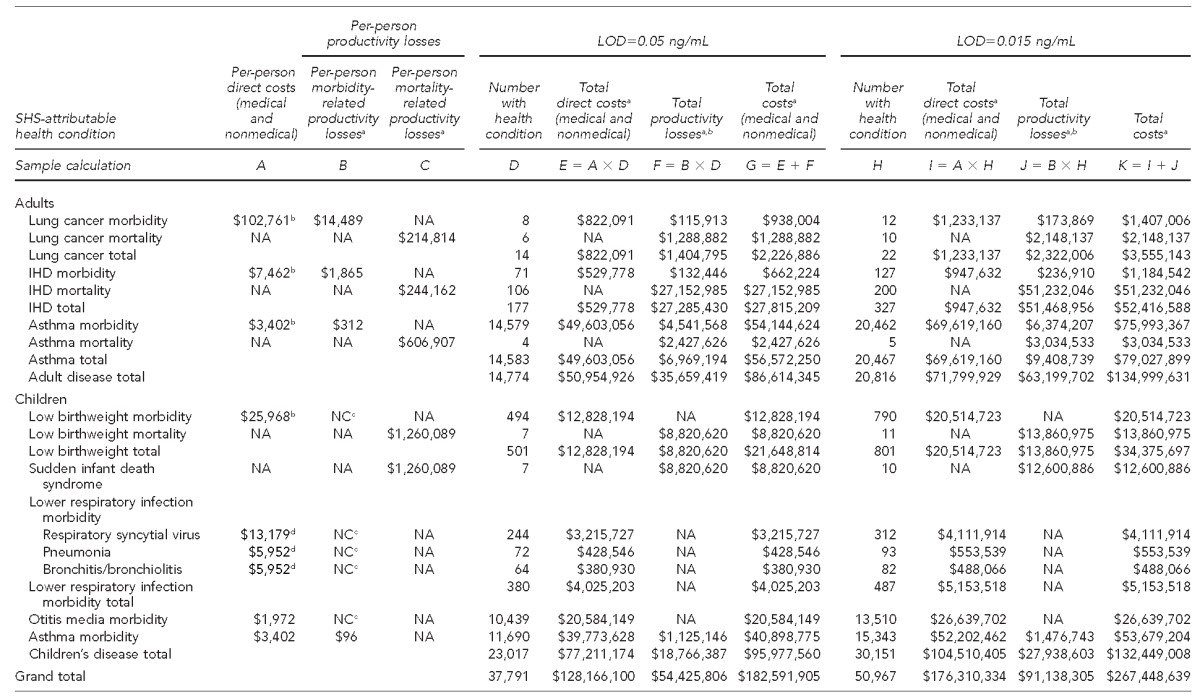
aSummed dollar amounts may not add to totals due to rounding.
bIncludes direct medical costs only
cEstimate was not found in published data.
dIncludes direct medical and nonmedical costs
SHS = secondhand smoke
LOD = limit of detection
IHD = ischemic heart disease
ng/mL = nanograms per milliliter
NA = not applicable
NC = not considered
Annual costs attributable to SHS in U.S. public housing were approximately $183 million (at LOD=0.05 ng/mL) and $267 million (at LOD=0.015 ng/mL) in 2011. Direct medical costs alone accounted for about $110 million (at LOD=0.05 ng/mL) and $153 million (at LOD=0.015 ng/mL) of total costs (calculations not shown). Asthma ranked highest in total SHS-attributable costs for both adults and children at both LODs. Productivity losses accounted for $54 million (at LOD=0.05 ng/mL) and $91 million (at LOD=0.015 ng/mL). The average total per-person cost due to SHS exposure in never-smoking U.S. public housing residents was an estimated $4,832 (at LOD=0.05 ng/mL) and $5,247 (at LOD=0.015 ng/mL) (calculations not shown).
Adults
SHS-related morbidity and mortality in adult U.S. public housing never smokers accounted for about $87 million (at LOD=0.05 ng/mL) and $135 million (at LOD=0.015 ng/mL) in 2011 (Table 4). Direct medical care accounted for approximately 59% (at LOD=0.05 ng/mL) and 53% (at LOD=0.015 ng/mL) of total adult costs (calculations not shown), with asthma and IHD responsible for virtually all SHS-related morbidity and mortality in adults; asthma alone accounted for 99% (at LOD=0.05 ng/mL) and 98% (at LOD=0.015 ng/mL) of the health burden, and 65% (at LOD=0.05 ng/mL) and 59% (at LOD=0.015 ng/mL) of costs for adults (calculations not shown). Lung cancer ranked highest in annual per-person direct medical care costs ($102,761) and morbidity-related productivity losses ($14,489).50,51 However, because it is a rare condition relative to asthma and IHD, lung cancer contributed little (3% for both LODs) to the total economic burden for adults (calculations not shown).
Children
Health-care, productivity, and nonmedical direct costs for children exposed to SHS in U.S. public housing totaled $96 million (at LOD=0.05 ng/mL) and $132 million (at LOD=0.015 ng/mL) (Table 4), or 53% (at LOD=0.05 ng/mL) and 50% (at LOD=0.015 ng/mL) of total societal costs (calculations not shown). Direct costs accounted for 80% (at LOD=0.05 ng/mL) and 79% (at LOD=0.015 ng/mL) of the total economic burden for children (calculations not shown). Asthma together with OM affected 96% of children who had SHS-attributable health outcomes (11,690 [at LOD=0.05 ng/mL] and 15,343 [at LOD=0.015 ng/mL] for asthma and 10,439 [at LOD=0.05 ng/mL] and 13,510 [at LOD=0.015 ng/mL] for OM) (Table 4), and incurred nearly two-thirds of total costs for children ($61 million [at LOD=0.05 ng/mL] and $80 million [at LOD=0.015 ng/mL]) (calculations not shown). Of infants who lived in U.S. public housing and died from SIDS or LBW-related factors, 31% (at LOD=0.05 ng/mL) and 43% (at LOD=0.015 ng/mL) of deaths from SIDS and 15% (at LOD=0.05 ng/mL) and 24% (at LOD=0.015 ng/mL) of deaths from LBW-related factors were attributable to SHS (calculations not shown). Although the number of infants in U.S. public housing expected to have died from SHS-attributable deaths was small (14 [at LOD=0.05 ng/mL] and 21 [at LOD=0.015 ng/mL] out of 40,094 infants), these deaths accounted for 18% (at LOD=0.05 ng/mL) and 20% (at LOD=0.015 ng/mL) of total annual SHS-attributable costs for children in U.S. public housing (calculations not shown).
DISCUSSION
The annual economic burden of SHS-attributable illness and death of never smokers in U.S. public housing totaled approximately $183 million (at LOD=0.05 ng/mL) and $267 million (at LOD=0.015 ng/mL). The benefits of reducing SHS exposure in U.S. public housing include lower out-of-pocket expenditures for medical care, lower apartment clean-up costs, and fewer productivity losses for employers and society.52,53 To our knowledge, this study is the first to estimate both the national public health burden and the economic impact of SHS on never-smoking U.S. public housing residents using nationally representative and other large-scale databases, and including biomarker data. Our results may help frame the problem of SHS exposure in U.S. public housing by quantifying the public health burden and associated monetary costs.
U.S. public housing residents have higher levels of exposure to SHS than the national population and a majority support policies aimed at eliminating SHS where they live.16,54 Because U.S. public housing is owned by public housing authorities, there are fewer barriers to implementing a smoke-free policy compared with voucher-assisted or privately owned housing (e.g., Section 8) (Personal communication, Barry Steffen, HUD, February 2012). The health benefits of a smoke-free policy for children would be substantial because they receive most of their exposure to SHS in the home and have a higher intake of SHS than adults.1,2 An effective U.S. public housing smoke-free policy would result in 130 (at LOD=0.05 ng/mL) and 236 (at LOD=0.015 ng/mL) fewer lives lost annually in never smokers. Even if never smokers are routinely exposed to SHS outside of the home, evidence suggests that a temporary respite from SHS may reduce adverse health outcomes such as IHD in adults.29
A recent study estimated $521 million in annual societal cost savings if smoking was banned in all government-subsidized U.S. housing. Our estimate of the annual societal direct medical costs ($110 million [at LOD=0.05 ng/mL] and $153 million [at LOD=0.015 ng/mL]) incurred due to SHS in U.S. public housing only is within the range ($50–$181 million) estimated by King et al.37 However, several differences between the two studies are worth noting. First, we provide both aggregated and health outcome-specific estimates of the public health and economic burdens; King et al. provided neither the public health burden nor health outcome-specific costs. Whereas King et al. relied on data based on self-report, we used biomarker data to determine the proportion of never smokers exposed to SHS. We calculated our estimates using both the current and previous LOD for detecting cotinine in serum (0.015 ng/mL and 0.05 ng/mL, respectively). While not explicitly stated, we assume King et al. used the previous LOD in their analysis. King et al. estimated SHS-attributable fire-related and apartment renovation costs, which were not included in our study. We used costs of illness or death from nationally representative or large-scale databases with national data when available. In contrast, the King et al. study used state-adjusted costs based on Minnesota health-care claims data. Finally, King et al. did not account for productivity losses, which were 40% (at LOD=0.015 ng/mL) and 43% (at LOD=0.05 ng/mL) of the total economic burden in our study.
Our estimate is higher than a previous estimate of the national annual per-person cost of productivity losses due to SHS-related death ($373,159 [at LOD=0.05 ng/mL] and $351,172 [at LOD=0.015 ng/mL] in 2011 dollars vs. $158,000 in 2006 dollars per premature death).55 This difference might be because (1) the prevalence of smoking in low-income families is higher than the national average3,56 and (2) public housing has a higher percentage of infants and children than the national population.57,58 Premature death in the young exacts high societal costs.46
Our cost-of-illness study did not include the implementation costs of smoke-free policies. We speculate these costs would be outweighed by the societal benefits of such policies. However, there is scant information on the costs or cost-effectiveness of implementing or enforcing smoke-free policies.59 Widespread adherence to a smoke-free policy in U.S. public housing would reduce adverse outcomes and societal costs from SHS exposure for both former and current smokers, which would greatly increase its benefits. Moreover, if barriers could be reduced in implementing smoke-free policies in voucher-assisted (i.e., Section 8) homes, there would be substantial additional savings produced by HUD-recommended smoke-free policies.
Limitations
Our study had several limitations. First, the RR estimates we used were not based exclusively on SHS exposures occurring solely in the home.2 Serum cotinine measurements reflect recent SHS exposure, regardless of location. Thus, we may have overestimated the health and economic impact of SHS exposure in the home. However, young children, the elderly, and the disabled comprise a substantial proportion of public housing residents and likely spend more time at home.5,57 Thus, the effect of exposures occurring outside the home for these groups may be small. Additionally, SHS exposure inside the home likely, but not necessarily, results in higher exposure levels than exposure due to migration between apartments. For example, it is unclear whether exposure from smoke that migrates from an apartment with one or more heavy smokers to a nonsmoker's apartment is higher or lower than the exposure experienced by never smokers with infrequent exposure to cigarette smoke in their home. Recent studies report that residents living in nonsmoking multiunit housing have higher cotinine levels and are more likely to smell smoke in their buildings than are residents of single-family homes.60,61 These findings suggest that the proportion of people exposed to SHS in our analysis is likely higher than the values we used.
When available, we used the incremental cost of each SHS-caused disease. However, these data were not available for all health outcomes of interest (e.g., OM). Moreover, this approach has been criticized because comorbidities or related health outcomes may account for a substantial portion of total excess costs, leading to double counting of effects and, thus, overestimation of true excess costs.62,63 On the other hand, incorrect coding for patients with comorbidities may lead to an underestimation of SHS-attributable costs.
The use of disease rates and health care based on the general population likely underestimates the amount of disease in the public housing population.64,65 However, we used national disease rates for individuals living in government-assisted housing, where possible, in an attempt to minimize the discrepancy. However, public housing residents may differ in meaningful ways from residents receiving other government housing subsidies. Excluding respiratory syncytial virus, none of the cost estimates we used were derived from studies conducted on low-income populations. Therefore, these costs may not accurately reflect health-care expenditures or the value of productivity losses in the low-income population.66 In particular, nearly half of people in poverty are covered by public insurance or are uninsured,67 which may result in lower reimbursements than for those who have private insurance. Additionally, some of the published estimates we used were quite dated and may not reflect current health-care practices and costs.63 In two cases, OM and LRI, we used morbidity-related productivity loss estimates based on small studies with convenience samples not designed to measure these losses among public housing residents. Finally, although we used a societal perspective, we did not account for all costs that are borne by society (e.g., long-term care, copayments, and other nonmedical direct expenses), as well as the intangible costs of the health effects (e.g., pain and suffering) of SHS exposure.
CONCLUSION
Implementation of smoke-free policies in all U.S. public housing can improve the health of residents and reduce societal costs, including medical costs. Our analysis provides national estimates of the public health and economic burdens associated with SHS exposure in U.S. public housing and quantifies the benefits of implementing a smoke-free policy in all U.S. public housing.
Footnotes
The authors thank Lydia Taghavi, Department of Housing and Urban Development (HUD), for demographic data on the population living in HUD-subsidized public housing; and Peter Ashley, Alastair McFarlane, and Barry Steffen of HUD, and Turnsynbek Nurmagambetov of the Centers for Disease Control and Prevention (CDC) for their review and comments.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Atlanta: Department of Health and Human Services (US), Centers for Disease Control and Prevention, National Center for Chronic Disease, Prevention and Health Promotion, Office on Smoking and Health; 2006. The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. Also available from: URL: http://www.ncbi.nlm.nih.gov/books/NBK44324/pdf/toc.pdf [cited 2012 May 12] [PubMed] [Google Scholar]
- 2.Öberg M, Jaakkola MS, Prüss-Üstün A, Schweizer C, Woodward A. Geneva: World Health Organization; 2010. Second-hand smoke: assessing the burden of disease at national and local levels. WHO Environmental Burden of Disease Series No. 18. Also available from: URL: http://www.who.int/quantifying_ehimpacts/publications/SHS.pdf [cited 2011 Jul 11] [Google Scholar]
- 3.Kaufmann RB, Babb S, O'Halloran A, Asman K, Bishop E, Tynan M, et al. Vital signs: nonsmokers' exposure to secondhand smoke—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2010;59(35):1141–6. [PubMed] [Google Scholar]
- 4.National Research Council (US) Pesticides in the diets of infants and children. Washington: National Academy Press; 1993. [PubMed] [Google Scholar]
- 5.National Center for Health in Public Housing. Demographic facts: residents living in public housing [cited 2011 Aug 1] Available from: URL: http://www.namgt.com/hphr/pdfs/demographicfacts.pdf.
- 6.Hall AG, Schumacher JR, Cannell MB, Berry JB, Schiaffino M, Park S. Tobacco use in Florida: comparisons between adults living with and without disabilities. Disabil Health J. 2013;6:213–9. doi: 10.1016/j.dhjo.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Kraev TA, Adamkiewicz G, Hammond SK, Spengler JD. Indoor concentrations of nicotine in low-income, multi-unit housing: associations with smoking behaviours and housing characteristics. Tob Control. 2009;18:438–44. doi: 10.1136/tc.2009.029728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Department of Housing and Urban Development (US) Characteristics of HUD-assisted renters and their units in 2003. Washington: HUD, Office of Policy Development and Research; 2008. Also available from: URL: http://www.huduser.org/portal/publications/pubasst/hud_asst_rent.html [cited 2011 Aug 1] [Google Scholar]
- 9.Herman PM, Walsh ME. Hospital admissions for acute myocardial infarction, angina, stroke, and asthma after implementation of Arizona's comprehensive statewide smoking ban. Am J Public Health. 2011;101:491–6. doi: 10.2105/AJPH.2009.179572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places: a systematic review and meta-analysis [published erratum appears in J Am Coll Cardiol 2009;54:1902] J Am Coll Cardiol. 2009;54:1249–55. doi: 10.1016/j.jacc.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 11.Hahn EJ, York NL, Rayens MK. Smoke-free legislation in Appalachian counties. Am J Public Health. 2010;100:2012–3.s. doi: 10.2105/AJPH.2010.202119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kabir Z, Clarke V, Conroy R, McNamee E, Daly S, Clancy L. Low birthweight and preterm birth rates 1 year before and after the Irish workplace smoking ban. BJOG. 2009;116:1782–7. doi: 10.1111/j.1471-0528.2009.02374.x. [DOI] [PubMed] [Google Scholar]
- 13.Markowitz S. The effectiveness of cigarette regulations in reducing cases of Sudden Infant Death Syndrome. J Health Econ. 2008;27:106–33. doi: 10.1016/j.jhealeco.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 14.Department of Housing and Urban Development (US) Non-smoking policies in public housing. Washington: HUD, Office of Healthy Homes and Lead Hazard Control; 2009. Also available from: URL: http://www.hud.gov/offices/pih/publications/notices/09/pih2009-21.pdf [cited 2011 Sep 12] [Google Scholar]
- 15.Department of Housing and Urban Development (US) Smoke-free policies in public housing. Washington: HUD, Office of Healthy Homes and Lead Hazard Control; 2012. Also available from: URL: http://portal.hud.gov/hudportal/documents/huddoc?id512-25pihn.pdf [cited 2011 Sep 12] [Google Scholar]
- 16.Drach LL, Pizacani BA, Rohde KL, Schubert S. The acceptability of comprehensive smoke-free policies to low-income tenants in subsidized housing. Prev Chronic Dis. 2010;7:A66. [PMC free article] [PubMed] [Google Scholar]
- 17.Pizacani BA, Maher JE, Rohde K, Drach L, Stark MJ. Implementation of a smoke-free policy in subsidized multiunit housing: effects on smoking cessation and secondhand smoke exposure. Nicotine Tob Res. 2012;14:1027–34. doi: 10.1093/ntr/ntr334. [DOI] [PubMed] [Google Scholar]
- 18.American Nonsmokers' Rights Foundation. U.S. laws and policies restricting or prohibiting smoking in private units of multi-unit housing. 2014 [cited 2012 May 23] Available from: URL: http://www.no-smoke.org/pdf/smokefreemuh.pdf.
- 19.The Center for Social Gerontology. Housing authorities/-commissions which have adopted smoke-free policies; 2011 [cited 2012 Oct 12] Available from: URL: http://www.tcsg.org/sfelp/SFHousing Authorities.pdf.
- 20.Aligne CA, Stoddard JJ. Tobacco and children. An economic evaluation of the medical effects of parental smoking [published erratum appears in Arch Pediatr Adolesc Med 1997;151:988] Arch Pediatr Adolesc Med. 1997;151:648–53. doi: 10.1001/archpedi.1997.02170440010002. [DOI] [PubMed] [Google Scholar]
- 21.Cook DG, Strachan DP. Health effects of passive smoking: summary of effects of parental smoking on the respiratory health of children and implications for research. Thorax. 1999;54:357–66. doi: 10.1136/thx.54.4.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DiFranza JR, Aligne CA, Weitzman M. Prenatal and postnatal environmental tobacco smoke exposure and children's health. Pediatrics. 2004;113(4 Suppl):1007–15. [PubMed] [Google Scholar]
- 23.Florence CS, Adams EK, Ayadi MF. Pediatric health care costs attributable to exposure to second-hand smoke: an exploratory analysis. J Health Care Finance. 2007;34:36–43. [PubMed] [Google Scholar]
- 24.Leung GM, Ho LM, Lam TH. The economic burden of environmental tobacco smoke in the first year of life. Arch Dis Child. 2003;88:767–71. doi: 10.1136/adc.88.9.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levy DE, Rigotti NA, Winickoff JP. Medicaid expenditures for children living with smokers. BMC Health Serv Res. 2011;11:125. doi: 10.1186/1472-6963-11-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levy DE, Winickoff JP, Rigotti NA. School absenteeism among children living with smokers. Pediatrics. 2011;128:650–6. doi: 10.1542/peds.2011-1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller T, Rauh VA, Glied SA, Hattis D, Rundle A, Andrews H, et al. The economic impact of early life environmental tobacco smoke exposure: early intervention for developmental delay. Environ Health Perspect. 2006;114:1585–8. doi: 10.1289/ehp.9165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oh SS, Tcheurekdjian H, Roth LA, Nguyen EA, Sen S, Galanter JM, et al. Effect of secondhand smoke on asthma control among black and Latino children. J Allergy Clin Immunol. 2012;129:1478–83. doi: 10.1016/j.jaci.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lightwood J. The economics of smoking and cardiovascular disease. Prog Cardiovasc Dis. 2003;46:39–78. doi: 10.1016/s0033-0620(03)00077-x. [DOI] [PubMed] [Google Scholar]
- 30.Lightwood JM, Glantz SA. Declines in acute myocardial infarction after smoke-free laws and individual risk attributable to secondhand smoke. Circulation. 2009;120:1373–9. doi: 10.1161/CIRCULATIONAHA.109.870691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pope CA, 3rd, Burnett RT, Turner MC, Cohen A, Krewski D, Jerrett M, et al. Lung cancer and cardiovascular disease mortality associated with ambient air pollution and cigarette smoke: shape of the exposure-response relationships. Environ Health Perspect. 2011;119:1616–21. doi: 10.1289/ehp.1103639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Plescia M, Wansink D, Waters HR, Herndon S. Medical costs of secondhand-smoke exposure in North Carolina. NC Med J. 2011;72:7–12. [PubMed] [Google Scholar]
- 33.Waters H. Baltimore: Johns Hopkins Bloomberg School of Public Health; 2006. The economic impact of secondhand smoke in Maryland. Report submitted to the American Cancer Society. [Google Scholar]
- 34.Waters HR, Foldes SS, Alesci NL, Samet J. The economic impact of exposure to secondhand smoke in Minnesota. Am J Public Health. 2009;99:754–9. doi: 10.2105/AJPH.2008.137430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zollinger TW, Saywell RM, Jr, Muegge CM, Przybylski MJ. Estimating the economic impact of secondhand smoke on Indiana in 2007. Indianapolis: Bowen Research Center–Indiana University School of Medicine; 2008. [Google Scholar]
- 36.Behan DF, Eriksen MP, Lin Y. Economic effects of environmental tobacco smoke. Schaumburg (IL): Society of Actuaries; 2005. [Google Scholar]
- 37.King BA, Peck RM, Babb SD. Cost savings associated with prohibiting smoking in U.S. subsidized housing. Am J Prev Med. 2013;44:631–4. doi: 10.1016/j.amepre.2013.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lewit EM, Baker LS, Corman H, Shiono PH. The direct cost of low birth weight. Future Child. 1995;5:35–56. [PubMed] [Google Scholar]
- 39.Trasande L, Landrigan PJ, Schechter C. Public health and economic consequences of methyl mercury toxicity to the developing brain. Environ Health Perspect. 2005;113:590–6. doi: 10.1289/ehp.7743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Department of Housing and Urban Development (US) Washington: HUD, Office of Policy Development and Research; 2005. Improving housing subsidy surveys: data collection techniques for identifying the housing subsidy status of survey respondents. Also available from: URL: http://www.huduser.org/publications/pdf/datacollect.pdf [cited 2012 Dec 1] [Google Scholar]
- 41.Centers for Disease Control and Prevention (US) Fourth national report on human exposure to environmental chemicals, 2009. Atlanta: CDC; 2009. [Google Scholar]
- 42.SAS Institute, Inc. Cary (NC): SAS Institute, Inc.; 2011. SAS®: Version 9.3. [Google Scholar]
- 43.Research Triangle Institute. Research Triangle Park (NC): Research Triangle Institute; 2008. SUDAAN®: Release 10.0. [Google Scholar]
- 44.Haddix AC, Teutsch SM, Corso PS. Prevention effectiveness: a guide to decision analysis and economic evaluation. 2nd ed. New York: Oxford University Press; 2003. [Google Scholar]
- 45.Wolleswinkel-van den Bosch JH, Stolk EA, Francois M, Gasparini R, Brosa M. The health care burden and societal impact of acute otitis media in seven European countries: results of an Internet survey. Vaccine. 2010;28(Suppl 6):G39–52. doi: 10.1016/j.vaccine.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 46.Grosse SD, Krueger KV, Mvundura M. Economic productivity by age and sex: 2007 estimates for the United States. Med Care. 2009;47(7 Suppl 1):S94–103. doi: 10.1097/MLR.0b013e31819c9571. [DOI] [PubMed] [Google Scholar]
- 47.Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002–2007. J Allergy Clin Immunol. 2011;127:145–52. doi: 10.1016/j.jaci.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 48.Harris J. Double jeopardy and the veil of ignorance—a reply. J Med Ethics. 1995;21:151–7. doi: 10.1136/jme.21.3.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Trogdon JG, Finkelstein EA, Nwaise IA, Tangka FK, Orenstein D. The economic burden of chronic cardiovascular disease for major insurers. Health Promot Pract. 2007;8:234–42. doi: 10.1177/1524839907303794. [DOI] [PubMed] [Google Scholar]
- 50.Chang S, Long SR, Kutikova L, Bowman L, Finley D, Crown WH, et al. Estimating the cost of cancer: results on the basis of claims data analyses for cancer patients diagnosed with seven types of cancer during 1999 to 2000. J Clin Oncol. 2004;22:3524–30. doi: 10.1200/JCO.2004.10.170. [DOI] [PubMed] [Google Scholar]
- 51.Bradley CJ, Yabroff KR, Dahman B, Feuer EJ, Mariotto A, Brown ML. Productivity costs of cancer mortality in the United States: 2000–2020. J Natl Cancer Inst. 2008;100:1763–70. doi: 10.1093/jnci/djn384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.National Center for Healthy Housing. Reasons to explore smoke-free housing. Columbia (MD): National Center for Healthy Housing; 2009. [Google Scholar]
- 53.Live Smoke Free. The benefits of a smoke-free policy [cited 2014 Dec 11] Available from: URL: http://www.mnsmokefreehousing.org/organizations/benefits.html.
- 54.Levy DE, Rigotti NA, Winickoff JP. Tobacco smoke exposure in a sample of Boston public housing residents. Am J Prev Med. 2013;44:63–6. doi: 10.1016/j.amepre.2012.09.048. [DOI] [PubMed] [Google Scholar]
- 55.Max W, Sung HY, Shi Y. Deaths from secondhand smoke exposure in the United States: economic implications. Am J Public Health. 2012;102:2173–80. doi: 10.2105/AJPH.2012.300805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Max W, Sung HY, Shi Y. Who is exposed to secondhand smoke? Self-reported and serum cotinine measured exposure in the U.S., 1999–2006. Int J Environ Res Public Health. 2009;6:1633–48. doi: 10.3390/ijerph6051633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Department of Housing and Urban Development (US) HUD resident characteristics report. Washington: HUD; 2011. [Google Scholar]
- 58.Census Bureau (US) Washington: Census Bureau; 2011. Statistical abstract of the United States: 2012 (131st edition) Also available from: URL: http://www.census.gov/compendia/statab [cited 2012 May 17] [Google Scholar]
- 59.Brownson RC, Hopkins DP, Wakefield MA. Effects of smoking restrictions in the workplace. Annu Rev Public Health. 2002;23:333–48. doi: 10.1146/annurev.publhealth.23.100901.140551. [DOI] [PubMed] [Google Scholar]
- 60.Wilson KM, Klein JD, Blumkin AK, Gottlieb M, Winickoff JP. Tobacco-smoke exposure in children who live in multiunit housing. Pediatrics. 2011;127:85–92. doi: 10.1542/peds.2010-2046. [DOI] [PubMed] [Google Scholar]
- 61.Wilson KM, Torok M, McMillen R, Tanski S, Klein JD, Winickoff JP. Tobacco smoke incursions in multiunit housing. Am J Public Health. 2014;104:1445–53. doi: 10.2105/AJPH.2014.301878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Akobundu E, Ju J, Blatt L, Mullins CD. Cost-of-illness studies: a review of current methods. Pharmacoeconomics. 2006;24:869–90. doi: 10.2165/00019053-200624090-00005. [DOI] [PubMed] [Google Scholar]
- 63.Foster TS, Miller JD, Marton JP, Caloyeras JP, Russell MW, Menzin J. Assessment of the economic burden of COPD in the U.S.: a review and synthesis of the literature. COPD. 2006;3:211–8. doi: 10.1080/15412550601009396. [DOI] [PubMed] [Google Scholar]
- 64.Bryant-Stephens T. Asthma disparities in urban environments. J Allergy Clin Immunol. 2009;123:1199–206. doi: 10.1016/j.jaci.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 65.Cole N, Fox MK, Lin BH. Washington: Department of Agriculture (US), Food Assistance and Nutrition Research Program; 2004. Nutrition and health characteristics of low-income populations: volume II, WIC participants and nonparticipants. EFAN-04014-2. Also available from: URL: http://www.ers.usda.gov/publications/efan-electronic-publications-from-the-food-assistance-nutrition-research-program/efan04014-2.aspx [cited 2011 Dec 2] [Google Scholar]
- 66.Shi N, Palmer L, Chu BC, Katkin JP, Hall CB, Masaquel AS, et al. Association of RSV lower respiratory tract infection and subsequent healthcare use and costs: a Medicaid claims analysis in early-preterm, late-preterm, and full-term infants. J Med Econ. 2011;14:335–40. doi: 10.3111/13696998.2011.578188. [DOI] [PubMed] [Google Scholar]
- 67.Census Bureau (US) Current Population Survey: annual social and economic supplement, 2012 [cited 2014 Feb 4] Available from: URL: https://www.census.gov/hhes/www/cpstables/032013/health/h02_000.htm.


