Abstract
Objectives
Smartphone applications (apps) are increasingly used to facilitate casual sexual relationships, increasing the risk of sexually transmitted diseases (STDs). In STD investigations, traditional contact elicitation methods can be enhanced with smartphone technology during field interviews.
Methods
In 2013, the Monroe County Department of Public Health conducted a large, multi-infection STD investigation among men who have sex with men (MSM) using both index case and cluster interviews. When patients indicated meeting sexual partners online, disease intervention specialists (DISs) had access to smartphone apps and were able to elicit partners through access to inboxes and profiles where traditional contact information was lacking. Social network mapping was used to display the extent of the investigation and the impact of access to smartphones on the investigation.
Results
A total of 14 index patient interviews and two cluster interviews were conducted; 97 individuals were identified among 117 sexual dyads. On average, eight partners were elicited per interview (range: 1–31). The seven individuals who used apps to find partners had an average of three Internet partners (range: 1–5). Thirty-six individuals either had a new STD (n=7) or were previously known to be HIV-positive (n=29). Of the 117 sexual dyads, 21 (18%) originated either online (n=8) or with a smartphone app (n=13). Of those originating online or with a smartphone app, six (29%) partners were located using the smartphone and two (10%) were notified of their exposure via a website. Three of the new STD/HIV cases were among partners who met online.
Conclusion
Smartphone technology used by DISs in the field improved contact elicitation and resulted in successful partner notification and case finding.
Representing about 2% of the U.S. population, men who have sex with men (MSM) are most affected by human immunodeficiency virus (HIV) in the United States, comprising 63% of new infections in 2010. Nationally, from 2008 to 2010, a 12% increase in new HIV infections was identified among MSM, with a 22% increase among MSM aged 13–24 years.1 Increases in syphilis have also been observed among MSM; in 2012, 75% of primary and secondary syphilis was among MSM.2 Recent increases in syphilis among MSM have been reported in major U.S. cities, with high rates of HIV coinfection.3 Having syphilis or other sexually transmitted diseases (STDs) can increase the likelihood of HIV transmission.4
The Internet has been identified as a tool for initiating and facilitating sexual partnerships and has been implicated in STD outbreaks.5 A 2006 meta-analysis estimated that 40% of MSM have used the Internet to find sex partners, and 30% of those have actually had sex with a partner they found on the Internet.6 Results from this meta-analysis and other studies have further demonstrated that MSM who use the Internet to find partners were more likely to engage in risky sexual behavior, such as multiple partners and unprotected anal intercourse, than those who did not seek partners online.6–9
Recently, mobile technology has expanded rapidly, providing Internet access beyond the personal computer, and social media have become a prominent part of daily life. Many free or low-cost smartphone applications (apps) have been developed specifically for MSM to easily filter for preferences, view profiles, and contact potential sexual partners. These apps may be attractive to MSM due to perceptions of privacy and anonymity in seeking partners.8 Apps such as Grindr and Jack'd differ from traditional Internet dating sites by their global positioning system (GPS) capability, which identifies immediately available partners based on proximity. This ability to easily identify and locate partners may impact sexual health and behavior by increasing access to potential partners and opportunities to engage in sexual behavior. Whether or not the use of apps leads to more or riskier sexual behavior is not clear. One study found that app users had significantly more lifetime sexual partners and were more likely to have a history of at least one STD compared with non-app users, but the two groups did not differ in other important aspects, such as frequency of unprotected anal intercourse, HIV/STD testing behavior, or HIV status.10 Almost half (46%) of participants in a recent study of young MSM in Los Angeles, California, recruited from the Grindr platform reported UAI, and most of those reporting unprotected anal intercourse (70%) had a low perception of risk of acquiring HIV.11
In Monroe County, New York, Internet and smartphone app use has increasingly been identified in investigations of newly reported HIV/STDs by local public health disease intervention specialists (DISs). Partner notification of newly reported HIV/STDs can be hindered when index patients only have online identifiers (e.g., screen names and e-mail addresses) of their partners, and they cannot be located using traditional contact methods. Internet partner notification (IPN) guidelines have been provided by the National Coalition of STD Directors.12 IPN is conducted when only a screen name is known by the index patient. The IPN DISs create health department profiles on commonly used websites. The IPN DIS sends a scripted message to the partner with instructions to contact the DIS. The goal of IPN is for the partner to contact the DIS by phone so that the DIS can notify the partner of his exposure via phone rather than via Internet. The use of the Internet to augment traditional partner notification has been shown to effectively reach partners for examination and treatment if required.13,14 Other literature has shown high acceptability of IPN among MSM at risk for STDs/HIV.15 Less information is available about using the Internet and/or social media to assist in identifying and locating partners for follow-up. A recent report from Wisconsin described how Facebook was used to find partners in a syphilis cluster, resulting in two additional partners located and one notified via Facebook.16
We describe a large, multi-infection STD investigation among mostly black MSM in which the use of smartphone technologies in the field increased the yield of partners elicited and subsequently notified and tested. The network was displayed graphically to further assist in identifying important members of the social network.
METHODS
Index patient interviews
In New York State, HIV, syphilis, gonorrhea, and chlamydia are the four STDs that are reportable under New York Public Health Law 2101.17 At the Monroe County Department of Public Health (MCDPH) STD/HIV Program, all reports of newly diagnosed HIV, early syphilis, and a subset of gonorrhea and chlamydia cases are referred to DISs for interview. DISs interview index patients to confirm treatment status, educate about STDs and risk reduction to prevent future disease, provide necessary community referrals, and elicit -partners for notification of exposure. Case and interview data are entered into a local electronic health record, where all new and historical STD diagnoses are tracked. These data are also submitted to the New York State Department of Health.
During partner elicitation, DISs ask the index patient if he/she knows the HIV status of each of his/her sexual partners. Named partners are checked against the local electronic health record for any past HIV/STD diagnoses. When an index patient names a partner known to MCDPH to be HIV-positive (i.e., previously known HIV-positive, or PKP), and the index patient indicates that he/she did not know his/her partner's status, the PKP partner is assigned to be reinterviewed by DISs; the index patient is not informed of the partner's HIV status but is encouraged by DISs to be tested. The purpose of the reinterview is to discuss risk-reduction methods, relay the importance of disclosing HIV status to the person's sexual partners, and elicit additional sexual partners who may require notification of their exposure to HIV.
Cluster interviews
Cluster interviews are conducted with uninfected partners of index patients to elicit additional information about the index patient and to identify others in the social network who may benefit from testing.18 MCDPH STD/HIV Program policy requires cluster interviews of uninfected partners of all new cases of early syphilis; cluster interviews are occasionally conducted for other diseases at the discretion of program management.
Smartphone assessment and implementation
To address the changing landscape of social and sexual networks through Internet use, and to improve STD partner elicitation and notification, the New York State Department of Health released “Internet-based Partner Services Guidelines for State, County, and Local Health Departments” in 2009.19 In 2010, MCDPH gained county approval to search sexually explicit websites for patient and partner locating and identifying information, and in 2012 extended approval to the field with the use of county-issued smartphones by DISs during field interviews.
The use of smartphones by Monroe County DISs has aided in partner elicitation by providing DISs with the ability to search various dating/hookup websites and apps in real time with index patients to identify previous sexual partners. During case interviews, clients are able to use the DIS's smartphone to log on to their accounts on various websites and apps to find their sexual partners, and retrieve inbox messages containing traditional locating information, such as phone numbers and addresses. Because notifications cannot happen via GPS apps, the only way for partners to be reached is by accessing profiles during field encounters with the original patient. In addition, smartphone availability in the field has been beneficial to DISs in locating non-app Internet profiles for IPN. Prior to smartphone access, DISs would elicit a screen name during an interview and, upon returning to the office, search the website and find that screen name did not exist. Access to websites in the field allows staff to confirm the spelling of screen names and the identity of the profile with the index patient. Smartphone access has also been helpful in confirming traditional locating information by accessing search sites and maps with the index patient.
RESULTS
Investigation
From February to May 2013, MCDPH conducted a large investigation using both traditional interviews of newly reported cases and cluster interviews of uninfected members of the social network. Smartphone access to websites and apps enhanced the investigation. -Adam4Adam, Jack'd, Facebook, and Black Gay Chat Live (BGC) were all accessed by DISs during this investigation.
The first case reported was a new case of gonorrhea in a PKP patient. The interview with this patient yielded three partners: one PKP person and two partners who tested negative for all STDs. The index patient indicated using Jack'd to meet two of his three partners. One of the partners named by the index patient was identified by physical description and screen name only. The index patient indicated that his partner used the Jack'd app and Adam4Adam and BGC websites. Initial attempts to notify the partner via IPN were unsuccessful. MCDPH DIS staff searched Facebook for the screen name used on Adam4Adam and BGC and found a profile with a similar screen name and the same picture used on BGC. The Facebook screen name matched the nickname used on other sites and provided a last name. During an internal staff meeting, two DIS staff recognized the nickname and last name from a previous investigation. They used the alias search function in the electronic health record to identify the person's legal name and full locating information. The partner was found to have been previously tested.
A second partner acquired through the Internet named by the index patient was well known to the STD/HIV program staff and had previously been named by multiple PKP patients in other investigations during the past year. This partner was located, notified, and tested negative for all STDs after this initial exposure; however, due to his known sexual history and risk behaviors, a cluster interview was conducted yielding an additional eight sex partners. He indicated using the Jack'd app to meet one of his eight partners; the partner he met on the Jack'd app was located, notified, and subsequently diagnosed newly HIV-positive. Of his remaining seven partners, four were PKP, two tested negative, and one was unable to be located.
The decision to cluster interview this HIV-negative partner was particularly productive. Two of the named partners in the cluster interview were assigned for interview. Both of these partners indicated using apps to meet new partners. As a direct result of this effort, two new HIV cases and one person who was coinfected with syphilis and chlamydia were identified. The network investigation continued to expand with the interviews of the newly identified cases and ultimately resulted in a total of 16 interviews.
During one of the HIV interviews, the only information the index patient had was the partner's screen name on Jack'd. The DIS asked if the index patient had any messages in his inbox on the app. The patient's cell phone was inoperable due to an uncharged battery. Therefore, the DIS used his county-issued smartphone and the patient was able to log into the app using his own log-in information and password. The patient and DIS reviewed the messaging inbox together and found a cell phone number for the partner. When the DIS called the cell phone number, he was able to obtain the partner's full legal name and date of birth and made a plan to meet with the partner to notify him of his exposure to HIV. This partner tested positive for HIV and was linked to specialty care. Knowledge of and access to the app was essential in locating, notifying, and engaging this partner in testing and care for HIV immediately.
Profile pages on apps and websites can consist of date of birth, age, physical description, nicknames, sexual orientation, HIV status, place of employment, and photographs. Information found on profiles is valuable to make connections and further identify partners for whom only marginal contact information is available. In one instance, the only information given for a partner was a profile name on Jack'd. DIS searched social media websites and found the same screen name used on Facebook and a photograph that matched the description of the partner given by the index patient, as well as the name of the high school the partner attended. Because Monroe County DIS staff have collaborative relationships with many local high school nurses, DISs were able to work with the school nurse to identify the partner. The partner was then located and notified of his HIV exposure.
Network data
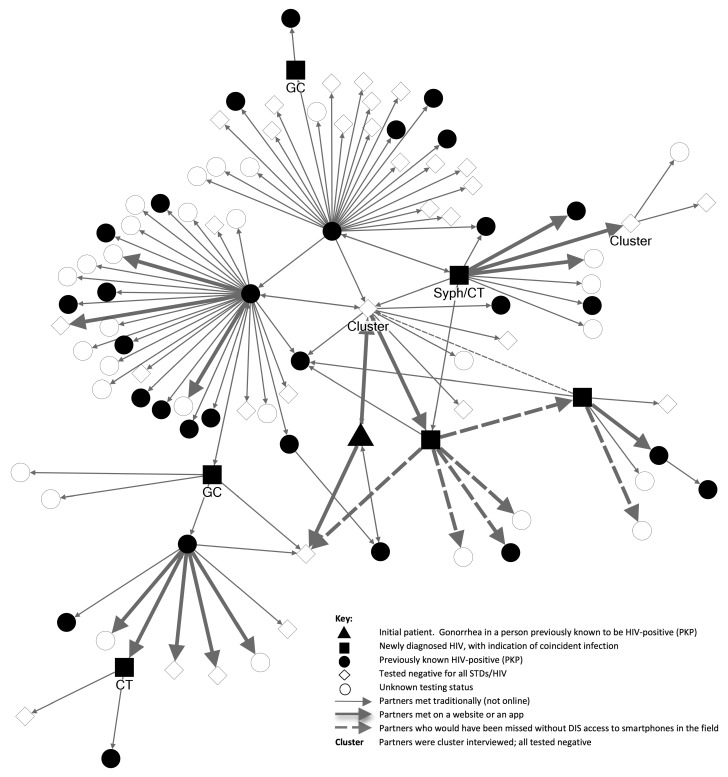
Line lists of the individuals and the sexual dyads in this social network were created in Microsoft® Excel® documenting demographics, partner dispositions, and test results. We used NodeXL20 to visualize the extent of the investigation (Figure).
Figure.
Social network diagram of new cases and contacts, by STD and HIV infection status, and method of meeting, in Monroe County, New York, 2013
STD = sexually transmitted disease
HIV = human immunodeficiency virus
DIS = disease intervention specialist
PKP = previously known HIV-positive
GC = gonorrhea
Syph = syphilis
CT = chlamydia
Ninety-seven unique individuals were named during the course of this investigation. Most were male (98%), black (81%), and <30 years of age (54%) (Table 1). Sixteen interviews were conducted: 14 index patient interviews and two cluster interviews of people testing negative for STDs. A total of 117 sexual dyads were identified, with an average of seven partners elicited per interview (range: 1–31) (Table 2).
Table 1.
Demographics of individuals named in a large, multi-infection STD investigation among men who have sex with men in Monroe County, New York, 2013
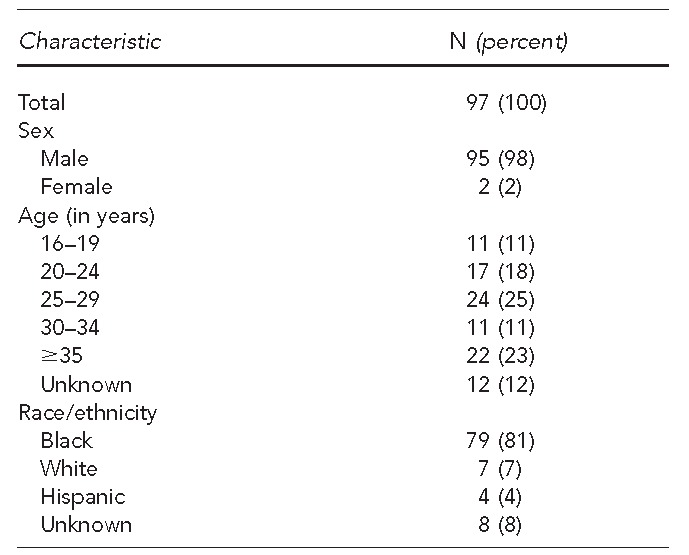
STD = sexually transmitted disease
Table 2.
Partners elicited and testing positive for STD/HIV, by interview type, in a large, multi-infection investigation among men who have sex with men in Monroe County, New York, 2013
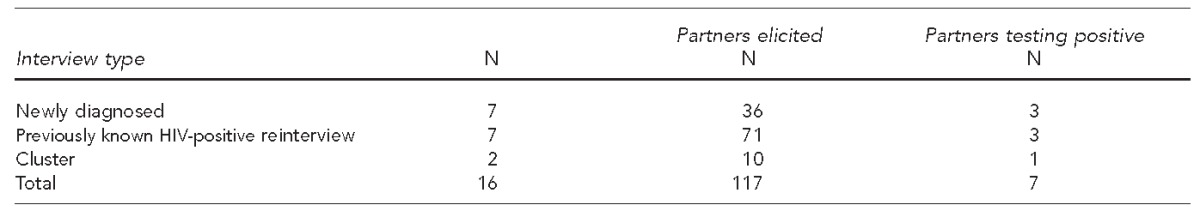
STD = sexually transmitted disease
HIV = human immunodeficiency virus
A total of 21 dyads (18%) were facilitated with an app or a website. Jack'd was the most commonly identified app in this network (n=14, 67%) followed by Adam4Adam (n=5, 24%). Among the seven index patients who admitted to using apps or websites to find partners, an average of three (range: 1–5) Internet partners were named. Access to the app/website in the field provided additional information to initiate partner notification in six (29%) of the partners, and two (10%) were actually notified of their exposure on the website itself (data not shown).
One new case of HIV infection among Internet partners was identified. As previously described, this new case would not have been tested and diagnosed at the time without real-time access to the Jack'd app with the index patient. Overall, eight individuals and 10 connections would have remained unknown in this network without information gleaned from accessing the smartphone. The Figure shows the partners who would have been missed without DIS smartphone access in the field.
As a result of partner notification and testing in this network, seven new cases of disease were diagnosed (Table 3). Thirty-one (32%) people were notified of their exposure and tested negative for all STDs/HIV. In this network, 30 PKP individuals were sexually active with negative partners, often times without disclosing their HIV-positive status; only one PKP patient was diagnosed with a new STD infection in this investigation. There were 30 people whose HIV/STD status remained unknown, and 15 of those people were out of the Monroe County jurisdiction and were referred to the appropriate jurisdiction when possible. Of the remaining unknowns, three were notified of their exposure and refused testing, four were partners for whom only marginal information was given by the index patient, two were notified via Adam4Adam.com with no further contact or update, and the rest were not located by the DIS (data not shown).
Table 3.
STD/HIV in a large, multi-infection investigation among men who have sex with men in Monroe County, New York, 2013
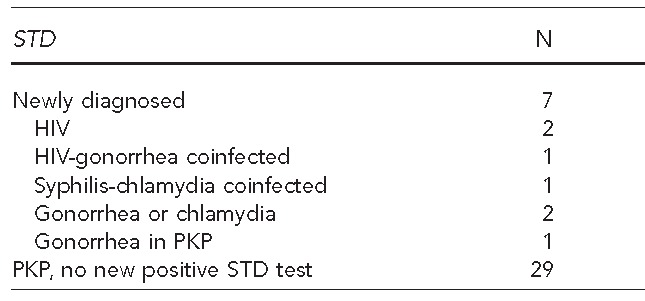
STD = sexually transmitted disease
HIV = human immunodeficiency virus
PKP = previously known HIV-positive
DISCUSSION
This investigation demonstrates the extent to which apps and websites were used for meeting sexual partners in this social network, and how having access to smartphones in the field enhanced partner elicitation during STD/HIV interviews. Allowing patients to log into their social networking or dating site accounts in real time with the DIS improved recall and provided additional locating or contact information for partners. Access to smartphones in the field can be used to augment partner services investigations; the technology serves as an additional tool and should not be used in place of traditional partner notification procedures.
Risk-reduction messages need to be relevant and tailored to the patient regardless of how partners are met. Often, messaging around condom use and changing sexual behaviors to less risky behaviors can be tailored to patients who meet partners via apps and online. These messages help patients create a profile that lets potential partners know they are looking for safe sex encounters only.
The decision to provide smartphones to Monroe County DISs for use during field interviews was made after DISs reported difficulty in getting valid contact information for Internet partners. Recognizing the changing use of technology in finding partners and hoping to obtain the most relevant information to identify and locate partners during the index patient interview, staff suggested that having real-time access to the websites/apps during the interview would allow them to verify screen names or find traditional contact information on the patient's accounts.
STD/HIV program managers made the case to health department administrators for access to smartphones by providing data such as the number of interviews conducted, the number of partners named, and the number named by using the Internet. Management also planned to use these data to determine how the technology was being used and whether or not performance was improved. Staff members were oriented to the phones and taught how to introduce its use during the interview; confidentiality and technology security policies were reinforced.
After implementation, a review of partner elicitation performance data demonstrated an increase in the number of Internet partners from 22 of 1,472 (1.5%) partners named in 2012 to 61 of 1,603 (3.8%) partners named in 2013 through the use of smartphones in the field. In addition to tracking performance data, the electronic health record maintained by the STD/HIV program contributed to the project's success. Fields in the patient record were customized to collect screen names or Internet aliases. By connecting screen names to patient records, staff can search the master patient index in the electronic health record not only by first and/or last name, but also by screen name. This -electronic health record search will allow staff to locate previously named partners when they are known only by a screen name in future investigations. Following the investigation, 168 screen names were added to patient records in the electronic health record in 2013, and DISs continue to link screen names to patient records in the electronic health record as they become known.
An additional strength of this study was the integration of STD and HIV services in this local health department. The initial patient in this investigation was reported as a new case of gonorrhea. Because local STD and HIV records are integrated in the electronic health record, surveillance staff members immediately identified this case as a PKP and elevated this referral for investigation. Integrating STD and HIV prevention programs allows for appropriate, comprehensive services to be delivered to patients and their partners and optimizes the use of limited health department resources.21 As indicated previously, Monroe County DISs only work a subset of new gonorrhea and chlamydia cases due to high volumes. Knowing the HIV status of a newly reported STD case ensures that PKPs with new STDs are prioritized and interviewed, and their partners notified of their exposure in a timely manner.
While resource constraints in local or state health jurisdictions may only allow for interviews of newly diagnosed HIV cases, the Monroe County STD/HIV Program has prioritized the reinterview of PKPs and assigns occasional cluster interviews outside the early syphilis protocol. The data from this network demonstrate that both approaches, in addition to index case interviews, can result in case finding. A previous study of a sexual network in Atlanta also demonstrated that interviewing only infected people can miss key individuals in a network.22
One limitation of current IPN guidelines is the lack of guidance related to notification on apps. At this time, there are guidelines for creating profiles on dating websites for the purpose of partner notification,12 but there is no guidance for conducting partner notification on apps. We were able to use apps in this case as a tool to gather additional information on partners to locate them offline, but in cases where we could not locate partners, notification on the app could be beneficial.
CONCLUSION
Smartphone technology used by DISs in the field improved contact elicitation and resulted in successful partner notification and case finding. The experiences of this investigation demonstrate the need for local health departments to equip DISs with the necessary tools to enhance partner services. To remain effective, public health will need to keep pace as technology continues to evolve.
Footnotes
The authors thank Kimberly Smith and Alaisha Reid of the Monroe County Health Department HIV/STD Program for their contributions to the partner services interviews of this investigation.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) HIV among gay and bisexual men [cited 2014 Oct 6] Available from: URL: http://www.cdc.gov/hiv/risk/gender/msm.
- 2.Centers for Disease Control and Prevention (US) Sexually transmitted disease surveillance, 2012. Atlanta: CDC; 2014. Also available from: URL: http://www.cdc.gov/std/stats12/default.htm [cited 2014 Oct 6] [Google Scholar]
- 3.Centers for Disease Control and Prevention (US) Syphilis & MSM (men who have sex with men)—CDC fact sheet. Atlanta: CDC; 2014. Also available from: URL: http://www.cdc.gov/std/syphilis/stdfact-msm-syphilis.htm [cited 2014 Oct 6] [Google Scholar]
- 4.Centers for Disease Control and Prevention (US) The role of STD detection and treatment in HIV prevention—CDC fact sheet. Atlanta: CDC; 2010. Also available from: URL: http://www.cdc.gov/std/hiv/stds-and-hiv-fact-sheet-press.pdf [cited 2014 Oct 7] [Google Scholar]
- 5.Klaussner JD, Wolf W, Fischer-Ponce L, Zolt I, Katz MH. Tracing a syphilis outbreak through cyberspace. JAMA. 2000;284:447–9. doi: 10.1001/jama.284.4.447. [DOI] [PubMed] [Google Scholar]
- 6.Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sex Transm Dis. 2006;33:576–84. doi: 10.1097/01.olq.0000204710.35332.c5. [DOI] [PubMed] [Google Scholar]
- 7.McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. JAMA. 2000;284:443–6. doi: 10.1001/jama.284.4.443. [DOI] [PubMed] [Google Scholar]
- 8.Garofalo R, Herrick A, Mustanski BS, Donenberg GR. Tip of the iceberg: young men who have sex with men, the Internet, and HIV risk. Am J Public Heath. 2007;97:1113–7. doi: 10.2105/AJPH.2005.075630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White JM, Mimiaga MJ, Reisner SL, Mayer KH. HIV sexual risk behavior among black men who meet other men on the Internet for sex. J Urban Health. 2013;90:464–81. doi: 10.1007/s11524-012-9701-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lehmiller JJ, Ioerger M. Social networking smartphone applications and sexual health outcomes among men who have sex with men. PLoS One. 2014;9:e86603. doi: 10.1371/journal.pone.0086603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Landovitz RJ, Tseng CH, Weissman M, Haymer M, Mendenhall B, Rogers K, et al. Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. J Urban Health. 2013;90:729–39. doi: 10.1007/s11524-012-9766-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Coalition of STD Directors. Internet partner services [cited 2014 Oct 6] Available from: URL: http://www.ncsddc.org/what-we-do/technical-assistance-training-and-health-equity-promotion/internet-partner-services.
- 13.Pioquinto RM, Tupas EA, Kerndt PR, Taylor MM, Holmberg SD, Patel PA. Using the Internet for partner notification of sexually transmitted diseases—Los Angeles County, California, 2003. MMWR Morb Mortal Wkly Rep. 2004;53(6):129–31. [PMC free article] [PubMed] [Google Scholar]
- 14.Ehlman DC, Jackson M, Saenz G, Novak DS, Kachur R, Heath JT, et al. Evaluation of an innovative Internet-based partner notification program for early syphilis case management, Washington, DC, January 2007–June 2008. Sex Transm Dis. 2010;37:478–85. doi: 10.1097/OLQ.0b013e3181e212cb. [DOI] [PubMed] [Google Scholar]
- 15.Mimiaga MJ, Fair AD, Tetu AM, Novak DS, Vanderwarker R, Bertrand T, et al. Acceptability of an Internet-based partner notification system for sexually transmitted infection exposure among men who have sex with men. Am J Public Health. 2008;98:1009–11. doi: 10.2105/AJPH.2006.098467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hunter P, Oyervides O, Grande KM, Prater D, Vann V, Reitl I, et al. Facebook-augmented partner notification in a cluster of syphilis cases in Milwaukee. Public Health Rep. 2014;129(Suppl 1):43–9. doi: 10.1177/00333549141291S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. New York Public Health Law, Art. 21, Title 1, §2101.
- 18.Recommendations for partner services programs for HIV infection, syphilis, gonorrhea and chlamydial infection. MMWR Recomm Rep. 2008;57(RR-9):1–83. [PubMed] [Google Scholar]
- 19.New York State Department of Health. Internet-based partner services guidelines for state, county, and local health departments. Albany (NY): New York State Department of Health; 2009. [Google Scholar]
- 20.Smith M, Milic-Frayling N, Shneiderman B, Mendes Rodrigues E, Leskovec J, Dunne C, et al. NodeXL. San Francisco: The Social Media Research Foundation; 2014. [Google Scholar]
- 21.Centers for Disease Control and Prevention (US), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Atlanta: CDC; 2009. Program collaboration and service integration: enhancing the prevention and control of HIV/AIDS, viral hepatitis, sexually transmitted diseases, and tuberculosis in the United States. [Google Scholar]
- 22.Rothenberg RB, Sterk C, Toomey KE, Potterat JJ, Johnson D, Schrader M, et al. Using social network and ethnographic tools to evaluate syphilis transmission. Sex Transm Dis. 1998;25:154–60. doi: 10.1097/00007435-199803000-00009. [DOI] [PubMed] [Google Scholar]