Abstract
Objective
Food insecurity may be a modifiable and independent risk factor for worse control of medical conditions, but it has not been explored among veterans. We determined the prevalence of, and factors independently associated with, food insecurity among veterans in the Veterans Aging Cohort Study (VACS).
Methods
Using data from VACS from 2002–2008, we determined the prevalence of food insecurity among veterans who have accessed health care in the Veterans Health Administration (VA) as defined by “concern about having enough food for you or your family in the past month.” We used multivariable logistic regression to determine factors independently associated with food insecurity and tests of trend to measure the association between food insecurity and control of hypertension, diabetes, HIV, and depression.
Results
Of the 6,709 veterans enrolled in VACS, 1,624 (24%) reported being food insecure. Food insecurity was independently associated with being African American, earning <$25,000/year, recent homelessness, marijuana use, and depression. Being food insecure was also associated with worse control of hypertension, diabetes, HIV, and depression (p<0.001).
Conclusion
Food insecurity is prevalent and associated with worse control of medical conditions among veterans who have accessed care in the VA.
Food insecurity is a household-level economic and social condition of limited or uncertain access to adequate food.1 In 2012, approximately 49 million people lived in U.S. households experiencing food insecurity. Being food insecure is more common among those in racial/ethnic minority groups and low-income individuals, as well as individuals with functional limitations or disabilities that could prevent individuals from gaining access to, preparing, and even consuming foods.2 It is an independent risk factor for poor intermediate health outcomes, including worse glycemic control in adults with diabetes, higher viral load in adults with human immunodeficiency virus (HIV), and worse depressive symptoms.3–13 Food insecurity may impact chronic disease self-management through varied mechanisms: reliance on inexpensive foods that are generally poor for glycemic control, competing demands between food and health-care expenditures, and decreased adherence to medications that should be taken with food.3–6
Few studies have examined the prevalence of and risk factors for food insecurity among veterans. According to data from the 2008 U.S. Department of Agriculture's Food Security Survey, 15.2% of veterans reported food insecurity compared with 16.8% of the general population.1 This survey may, however, reflect an underestimation of food insecurity among veterans given its target population of noninstitutionalized individuals contacted by telephone. Other large population-based studies have not specifically examined prior military service as a correlate of food insecurity,5,14 and some studies have even excluded veterans because they were a small portion of the study cohort.15 Given that individuals who use the Veterans Health Administration (VA) health-care system are more likely to be of a racial/ethnic minority group, poor, homeless, or disabled, they may be at an increased risk for food insecurity and, thus, experience worse health outcomes. We have previously reported that, among HIV-infected individuals receiving care in the VA health-care system, food insecurity is associated with worse HIV outcomes, including lower CD4 counts and higher viral load.3 A recent study found that military service impacts soldiers' food environment and food security, which then influences eating behavior and food choices both during military service and following discharge.16 Further, there are significant and persistent disparities in health and health care among veterans compared with the general population.17
To our knowledge, no study has empirically studied the prevalence of food insecurity and its correlates among the Veteran population receiving medical care within the VA health-care system. We therefore examined the prevalence of and health outcomes associated with food insecurity among a multisite sample of veterans enrolled in the Veterans Aging Cohort Study (VACS), using clinical and administrative data to define health outcomes.
METHODS
Sample and setting
We analyzed baseline data on 6,709 subjects enrolled in VACS. VACS is an observational cohort of HIV-infected and HIV-uninfected individuals that began in 2002 and is designed to examine the role of alcohol and comorbid medical and psychiatric disease in determining clinical outcomes in HIV infection.3,7 A full description of the study and measures collected is provided elsewhere.18 Briefly, VACS assesses patients using a combination of self-reported, administrative, and clinical data from eight VA infectious disease and general medical clinics (Atlanta, Georgia; Baltimore, Maryland; Bronx, New York; Manhattan/Brooklyn, New York; Houston, Texas; Los Angeles, California; Pittsburgh, Pennsylvania; and Washington, D.C.). Overall, 58% of HIV-infected patients at the eight sites were enrolled, with only 9% of those approached refusing to participate. HIV-negative controls, in a 1:1 ratio, were recruited from general medicine clinics at the same medical centers and were matched based on age, race/ethnicity, and gender. All participants were engaged in the VA health-care system. Data collected include sociodemographic factors; comorbid conditions; measures of patients' health and habits, including drug and alcohol use; homelessness; and health behaviors. The study sample for these analyses included the subset of VACS participants who completed a baseline survey from 2002 to 2008.
Measurements
Food insecurity.
To capture the broadest domain of food insecurity—uncertainty about food access—VACS incorporated the first question of the 18-item Household Food Insecurity Access Scale (HFIAS) in the baseline patient survey: “In the past 4 weeks, have you been concerned about having enough food for you or your family?” HFIAS is a previously validated scale designed to assess household food insecurity in multiple international settings.19 Participants who answered “yes” were categorized as being food insecure.
Covariates.
We selected candidate covariates based on prior literature on factors associated with food insecurity and health outcomes.3–6,20 Variables used in the study included age (continuous), gender (male/female), race/ethnicity (white/African American/Hispanic/other), income (<$25,000/year vs. ≥$25,000/year), education (≤high school vs. >high school), married or long-term partner, unemployment, recent homelessness, and site of enrollment. We assessed current alcohol consumption using the three-item Alcohol Use Disorders Identification Test-Consumption (AUDIT-C).21,22 People were classified as having unhealthy alcohol use if their total score on the AUDIT-C was ≥4 drinks/day (or ≥3 drinks/day for women and aged ≥65 years). If participants reported that they drank ≥6 drinks in one sitting at least once a month, they were classified as engaging in heavy episodic drinking.23 Those self-reporting opioid, marijuana, cocaine, or stimulant use, defined according to whether or not a participant reported using more than 1–3 times/month in the past year, were considered as having recent drug use. We assessed multicollinearity using variance inflation factors, which were all <4, indicating that multicollinearity was not complicating our analyses.
Additionally, we examined the association between food insecurity and various clinical conditions, including hypertension, diabetes, HIV, and depression, given that such associations have been reported in other populations.5,11,24 Hypertension was defined as a systolic blood pressure ≥140 millimeters of mercury (mmHg), diastolic blood pressure ≥90 mmHg, or having International Classification of Diseases-Ninth Revision (ICD-9) administrative codes for hypertension. Diabetes was defined using ICD-9 codes. We used the Patient Health Questionnaire-9 (PHQ-9) to assess active depressive symptoms.25 The PHQ-9 is a modified version of the Primary Care Evaluation of Mental Disorders that specifically addresses major depressive disorder. A cutoff score of ≥10 has a sensitivity of 88% and a specificity of 88% for a clinical diagnosis of depression.
HIV status was ascertained from the medical record. Among HIV-infected patients, we compared the VACS Index Score for those with and without food insecurity. The VACS Index Score is a validated index of overall medical health that is predictive of morbidity and mortality and incorporates both HIV and non-HIV biomarkers. It is calculated using the patient's age, CD4 cell count, HIV ribonucleic acid and hemoglobin levels, renal and hepatic function, and hepatitis C virus serostatus.26,27 The VACS Index Score ranges from 0 to 164 points, with higher scores indicating greater burden of disease and higher risk of morbidity and mortality (each additional five points indicates approximately a 20% increased risk of five-year mortality).27,28 We calculated body mass index (BMI) based on weight and height as recorded in the electronic medical record during routine clinical care. Obesity was defined as having a BMI ≥30 kilograms per meter squared (kg/m2). All clinical measures used the laboratory value closest to the baseline survey date.
Control of medical conditions.
Among those with hypertension, we categorized hypertension control as poorly controlled (≥160 mmHg systolic blood pressure or ≥100 mmHg diastolic blood pressure), minimally controlled (>140–<160 mmHg systolic blood pressure or >90–<100 mmHg diastolic blood pressure), and well-controlled (≤140 mmHg systolic blood pressure or ≤90 mmHg diastolic blood pressure). Among those with diabetes, we categorized diabetes control as having a glycosylated hemoglobin A1c (HgBA1c) of 5–7 units (adequately controlled), >7 units (inadequately controlled), and <5 units (tightly controlled). Among HIV-infected patients, we used the VACS Index Score to examine overall control of medical conditions. Because there are no set cutoffs for the VACS Index Score that indicate severity of disease, we examined VACS Index Scores by quartile, with the highest quartile scores indicating a worsening of overall medical condition. Finally, we used PHQ-9 scores to define control of depression, where a higher PHQ-9 score measures worse control of depression: 10–14 indicates moderate depression, 15–19 indicates moderately severe depression, and 20–27 indicates severe depression.25
Analysis
Subjects with and without food insecurity were first compared on baseline sociodemographic and clinical characteristics. We evaluated those characteristics associated with food insecurity using t-tests and chi-square tests as appropriate for continuous and categorical variables. We next examined factors associated with food insecurity using multivariable logistic regression by adjusting for all covariates associated with food insecurity with p<0.2 in unadjusted analyses. To examine the control of medical conditions, we examined the prevalence of food insecurity by severity of hypertension, diabetes, HIV, and depression using chi-square tests and tests of trends as appropriate. We considered p<0.05 to be statistically significant.
RESULTS
Among 6,709 subjects, 1,624 (24%) reported food insecurity (Table 1). Subjects who were food insecure were significantly more likely than those who were food secure to be of a racial/ethnic minority group (85% vs. 76%, p<0.001), low income (86% vs. 66%, p<0.001), unemployed (83% vs. 64%, p<0.001), and recently homeless (28% vs. 8%, p<0.001). Those who were food insecure were also more likely than those who were food secure to report using marijuana (12% vs. 8%, p<0.001), cocaine (12% vs. 7%, p<0.001), and opioids at least 1–3 times a month (8% vs. 4%, p<0.001) and to meet criteria for unhealthy alcohol use (42% vs. 38%, p=0.002) and heavy episodic drinking (30% vs. 24%, p<0.001). Food-insecure individuals were also more likely than food-secure individuals to be HIV-positive (52% vs. 49%, p=0.02), depressed (41% vs. 15%, p<0.001), and have a lower mean BMI (25.8 kg/m2 vs. 26.5 kg/m2, p<0.001). Food-insecure participants were less likely to have hypertension (32% vs. 37%, p<0.001) than hose who reported being food secure but about equally likely to have diabetes (22% vs. 24%, p=0.09) (Table 1).
Table 1.
Veterans Aging Cohort Study participants by food-insecure status, 2002–2008 (n=6,709)
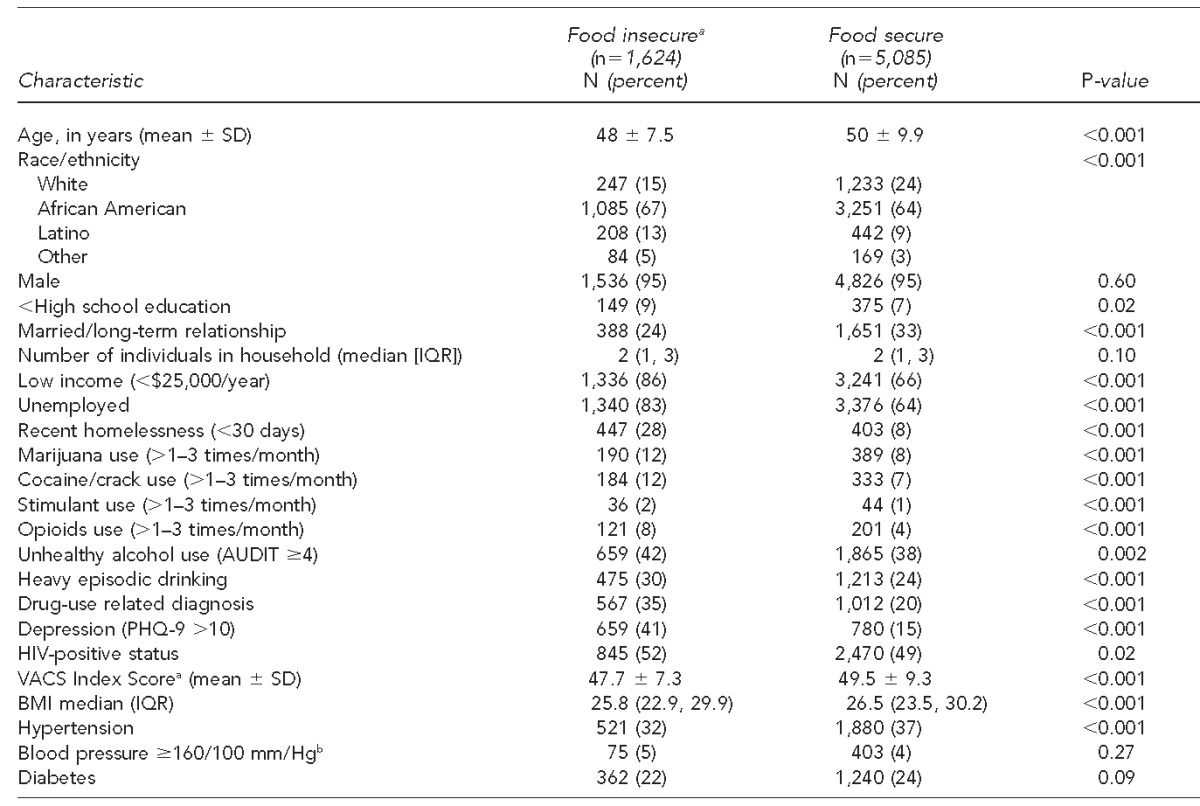
aFood insecurity is a household-level economic and social condition of limited or uncertain access to adequate food.
bAmong those with HIV infection
cAmong those with hypertension
SD = standard deviation
IQR = interquartile range
AUDIT = Alcohol Use Disorders Identification Test
PHQ-9 = Patient Health Questionnaire-9
HIV = human immunodeficiency virus
VACS = Veterans Aging Cohort Study
BMI = body mass index
mm/Hg = millimeters of mercury
In adjusted analyses, compared with white individuals, African Americans had increased odds of being food insecure (adjusted odds ratio [AOR] = 1.56, 95% confidence interval [CI] 1.31, 1.86), as did Latinos (AOR=2.12, 95% CI 1.66, 2.72) and those in other racial/ethnic minority groups (AOR=1.94, 95% CI 1.36, 2.76) (Table 2). Those with an income <$25,000/year (AOR=2.50, 95% CI 2.10, 2.98) and those who were recently homeless (AOR=3.18, 95% CI 2.77, 3.79) had more than twofold higher odds of being food insecure compared with those with higher incomes or who were adequately housed. Food insecurity was independently associated with marijuana use (AOR=1.36, 95% CI 1.10, 1.68) and meeting criteria for depression (AOR=3.00, 95% CI 2.60, 3.46). It was not independently associated with heavy episodic drinking or using cocaine, opioids, or amphetamines. HIV status was also not independently associated with food insecurity.
Table 2.
Risk factors for food insecurity in Veterans Aging Cohort Study participants, 2002–2008 (n=6,709)
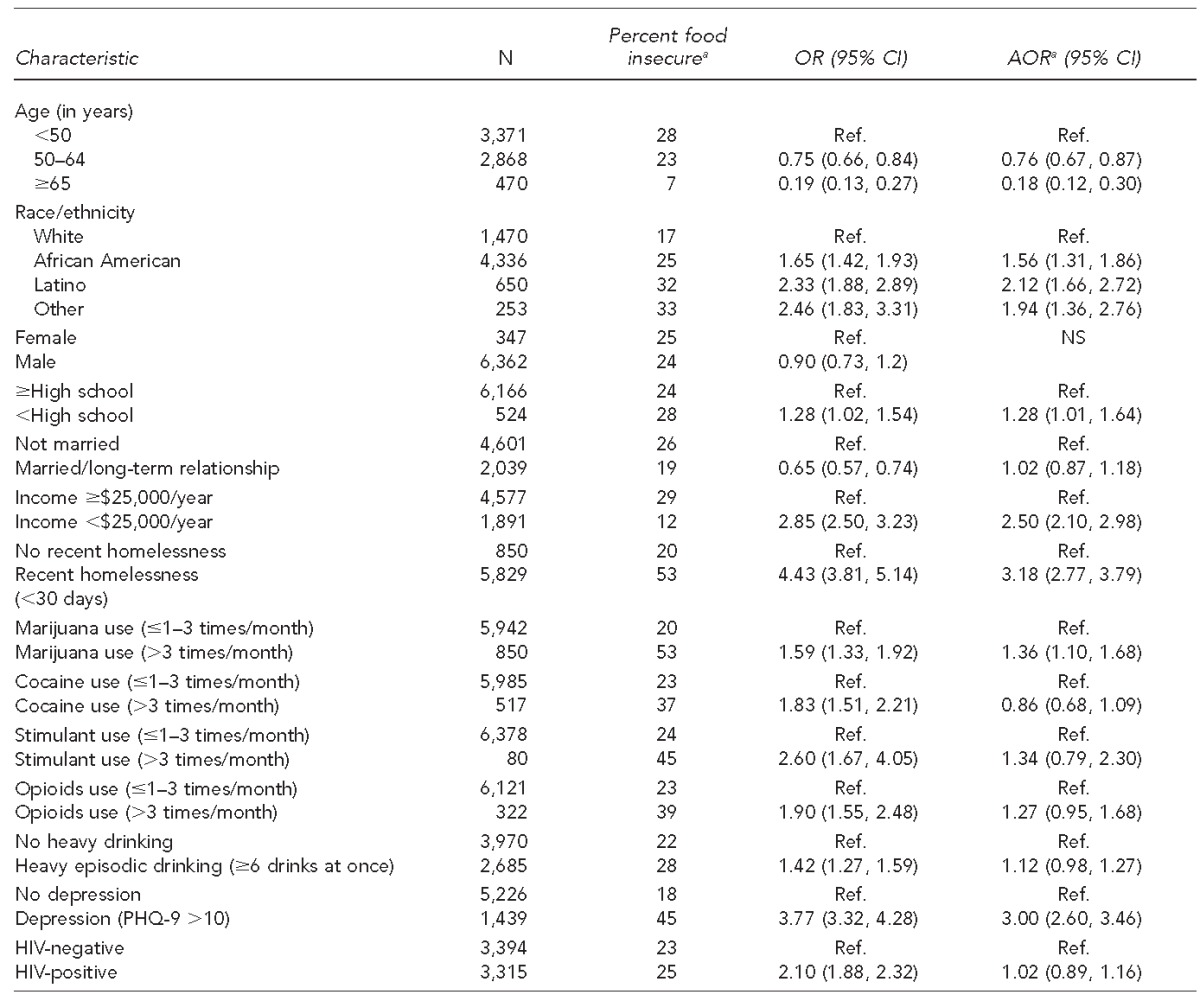
aFood insecurity is a household-level economic and social condition of limited or uncertain access to adequate food.
OR = odds ratio
CI = confidence interval
AOR = adjusted odds ratio
Ref. = reference group
NS = not significant
PHQ-9 = Patient Health Questionnaire-9
HIV = human immunodeficiency virus
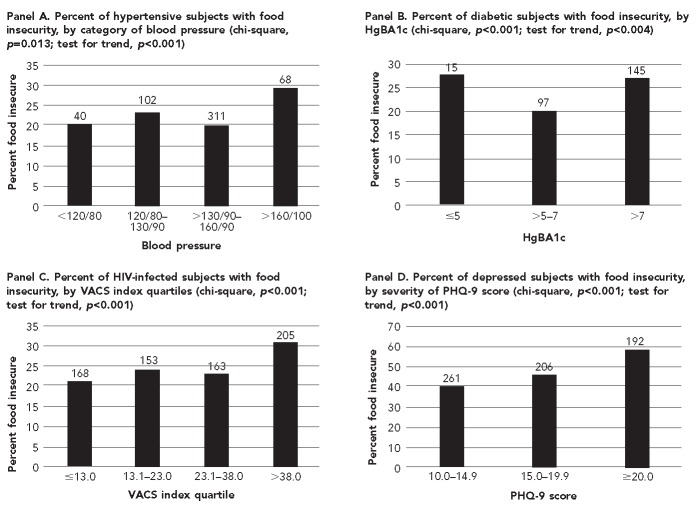
Figure. Severity of chronic conditions by food insecuritya for Veterans Aging Cohort Study participants, 2002–2008
aFood insecurity is a household-level economic and social condition of limited or uncertain access to adequate food.
HgBA1c = glycosylated hemoglobin A1c
HIV = human immunodeficiency virus
VACS = Veterans Aging Cohort Study
PHQ-9 = Patient Health Questionnaire-9
Among those with hypertension, individuals with poor blood pressure control were more likely to be food insecure than those whose systolic blood pressure was <160 mmHg. Having a higher blood pressure was associated with higher rates of food insecurity (test of trend, p=0.013) (Figure, Panel A). Food insecurity was independently associated with poor blood pressure control even after adjusting for individuals' race, age, and gender (AOR=1.59, 95% CI 1.17, 2.17) (data not shown). Among those with diabetes, individuals with tight diabetes control (HgBA1c <5, 29.4%) (Figure, Panel B) or who had evidence of inadequate diabetes control (HgBA1c >7, 27.1%) were more likely to be food insecure than those whose diabetes was controlled (HgBA1c 5–7, 20.0%, p<0.001). Food insecurity was independently associated with inadequate diabetes control even after adjusting for subjects' race, age, and gender (AOR=1.58, 95% CI 1.17, 2.13) but not with tight diabetes control (AOR=1.68, 95% CI 0.87, 3.23) (data not shown). Among HIV-infected individuals, those with food insecurity had higher VACS Index Scores (test for trend, p<0.001) (Figure, Panel C). Similarly, higher rates of food insecurity were seen in those with more severe depressive symptoms (test of trend, p<0.001) (Figure, Panel D).
Figure.
Severity of chronic conditions by food insecuritya for Veterans Aging Cohort Study participants, 2002–2008
aFood insecurity is a household-level economic and social condition of limited or uncertain access to adequate food.
HgBA1c = glycosylated hemoglobin A1c
HIV = human immunodeficiency virus
VACS = Veterans Aging Cohort Study
PHQ-9 = Patient Health Questionnaire-9
DISCUSSION
In a large multisite study, one-quarter of veterans receiving care in the VA health-care system reported food insecurity in the past 30 days, which was significantly more than the general U.S. population or as reported in prior studies.1 Being poor, of a racial/ethnic minority, unemployed, or recently homeless was independently associated with food insecurity, risk factors similar to those reported in the general population. Food insecurity was also independently associated with marijuana use and depression, as has been shown in other studies. Unlike previous studies, we did not see a statistically significant association between food insecurity and illicit drug use, but our study may have been underpowered to detect such an association.8,29
Similar to past studies, but using more stringent methods to characterize the medical diagnoses and measures of control, we found that food insecurity was associated with worse control of hypertension, diabetes, HIV disease, and depression.5,7,11–13,30,31 The high rate of food insecurity among a veteran population with access to health care and medications raises several interesting issues. The first is that it supports the hypothesis that food insecurity may be a path to poor health outcomes above and beyond lack of access to medical care and medications. The association with food insecurity and inadequate diabetes control may imply that people have inadequate nutrition contributing to more episodes of hypoglycemia.4 Episodic underconsumption may lead to periods of binging, which is linked to insulin resistance, or eating less expensive foods that are calorie dense with little nutritional value. These explanations support the nonlinear relationship between food insecurity and hemoglobin Alc. Similarly, the high sodium and low potassium content of highly processed foods, common in the diets of food-insecure adults, may worsen blood pressure control.5
For HIV and depression, where disease management is less clearly subject to variations in diets, food insecurity may be associated with medication nonadherence.8 Another plausible biologic mechanism for the relationship between food insecurity and various diseases is that food may impact the pharmacokinetics of medications. Because we did not assess the use of specific medication regimens, we cannot infer the effect of particular regimens on the association between food insecurity and disease control. Further research needs to be conducted to explore the mechanisms of the association between food insecurity and disease control to tailor interventions to improve the health outcomes for food-insecure patients. Studies from resource-poor settings indicate that supplementing the diet with micronutrients can improve the health outcomes of individuals with HIV.32
Our findings suggest that interventions addressing food insecurity in veteran populations accessing the VA health-care system will need to examine the intertwined nature of food insecurity and homelessness in this population. Currently, the VA has programs focused on food insecurity related to homelessness and has allocated $3.4 billion to homeless veterans' health care and $800 million to specialized homeless programs, including access to quality food sources. These efforts include enrolling veterans into programs such as the Supplemental Nutrition Assistance Program that provides food stamps. However, these programs may no longer be available and are not currently meeting the nutritional needs of these veterans and their families.33
Limitations
This study was subject to several important limitations. For one, no conclusions about cause and effect can be derived from this study due to its cross-sectional design. For example, it is possible that worse disease outcomes contribute to food insecurity. Also, individuals with more advanced disease and poor functional health status are less able to obtain food or lack an adequate ability to store and cook food. And out-of-pocket health-care expenditures, including medications, can also deplete resources and may lead to food insecurity.34 These effect-cause relationships deserve further exploration in future studies.
Additionally, our measurement for food insecurity was a single item of the HFIAS that captured only one aspect of food insecurity—anxiety and uncertainty about food supply. Therefore, we lacked accurate information about other components of food insecurity, including insufficient food intake or quality of food, as well as the duration, frequency, or extent of food insecurity. While the item that we used to assess food insecurity has not been validated among individuals accessing the VA health-care system, validation studies have demonstrated that it is able to distinguish food-secure from food-insecure households across different cultural contexts, and it has been used in populations with similar demographic and clinical characteristics. Such information would further define the impact of food insecurity on health outcomes among veterans.
Finally, this study was conducted among veterans who have accessed the VA health-care system; further studies would need to explore the prevalence of and risk factors for food insecurity in the general population of veterans, including those who have never accessed health care in the VA system.
CONCLUSION
In a large, multisite study, food insecurity was common in veterans who have accessed the VA health-care system and was associated with worse disease control across multiple medical conditions. Longitudinal studies with detailed measures of food insecurity are needed to better understand the relationships between food insecurity and health outcomes and to inform specific interventions to reduce health inequities among veterans.
Footnotes
The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The Veterans Aging Cohort Study (VACS) is funded by the National Institute on Alcohol Abuse and Alcoholism (#U01-AA-13566 and #U10-AA-13566); the National Institute on Aging (NIA) (#K23-AG00826); and the Robert Wood Johnson Generalist Faculty Scholar Award, an interagency agreement among the NIA, National Institute of Mental Health, and Veterans Health Administration Health Services Research & Development Research Enhancement Award Program (REAP) PRIME Project (#REA-08-266). Emily Wang receives salary support from a career development award from the National Heart, Lung, and Blood Institute (#K23-HL103720) and the Yale Clinical Center of Investigation's Clinical & Translations Science Awards Grant (#UL1 RR024139). The Institutional Review Boards at the Veterans Health Administrations in Atlanta, Georgia; Baltimore, Maryland; Bronx, New York; Manhattan/Brooklyn, New York; Houston, Texas; Los Angeles, California; Pittsburgh, Pennsylvania; and Washington, D.C., approved the study, and all participants provided written informed consent prior to enrollment.
REFERENCES
- 1.Nord M, Andrews M, Carlson S. Washington: Department of Agriculture (US); 2009. Household food security in the United States, 2008. Economic Research Report No. (ERR-83) [Google Scholar]
- 2.Coleman-Jensen A, Nord M, Singh A. Washington: Department of Agriculture (US); 2013. Household food inecurity in the United States in 2012. Economic Research Report No. (ERR-155) [Google Scholar]
- 3.Wang EA, McGinnis KA, Fiellin DA, Goulet JL, Bryant K, Gilbert CL, et al. Food insecurity is associated with poor virologic response among HIV-infected patients receiving antiretroviral medications. J Gen Intern Med. 2011;26:1012–8. doi: 10.1007/s11606-011-1723-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seligman HK, Jacobs EA, Lopez A, Sarkar U, Tschann J, Fernandez A. Food insecurity and hypoglycemia among safety net patients with diabetes. Arch Intern Med. 2011;171:1204–6. doi: 10.1001/archinternmed.2011.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants [published erratum appears in J Nutr 2011;141:542] J Nutr. 2010;140:304–10. doi: 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Melchior M, Caspi A, Howard LM, Ambler AP, Bolton H, Mountain N, et al. Mental health context of food insecurity: a representative cohort of families with young children. Pediatrics. 2009;124:e564–72. doi: 10.1542/peds.2009-0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiser SD, Fernandes KA, Brandson EK, Lima VD, Anema A, Bangsbert DR, et al. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52:342–9. doi: 10.1097/QAI.0b013e3181b627c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiser SD, Frongillo EA, Ragland K, Hogg RS, Riley ED, Bangsberg DR. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. J Gen Intern Med. 2009;24:14–20. doi: 10.1007/s11606-008-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vogenthaler NS, Hadley C, Lewis SJ, Rodriguez AE, Metsch LR, del Rio C. Food insufficiency among HIV-infected crack-cocaine users in Atlanta and Miami. Public Health Nutr. 2010;13:1478–84. doi: 10.1017/S1368980009993181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vogenthaler NS, Hadley C, Rodriguez AE, Valverde EE, del Rio C, Metsch LR. Depressive symptoms and food insufficiency among HIV-infected crack users in Atlanta and Miami. AIDS Behav. 2011;15:1520–6. doi: 10.1007/s10461-010-9668-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22:1018–23. doi: 10.1007/s11606-007-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siefert K, Heflin CM, Corcoran ME, Williams DR. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. J Health Soc Behav. 2004;45:171–86. doi: 10.1177/002214650404500204. [DOI] [PubMed] [Google Scholar]
- 13.Heflin CM, Siefert K, Williams DR. Food insufficiency and women's mental health: findings from a 3-year panel of welfare recipients. Soc Sci Med. 2005;61:1971–82. doi: 10.1016/j.socscimed.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 14.Anema A, Vogenthaler N, Frongillo EA, Kadiyala S, Weiser SD. Food insecurity and HIV/AIDS: current knowledge, gaps, and research priorities. Curr HIV/AIDS Rep. 2009;6:224–31. doi: 10.1007/s11904-009-0030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson K, Cunningham W, Andersen R, Harrison G, Gelberg L. Is food insufficiency associated with health status and health care utilization among adults with diabetes? J Gen Intern Med. 2001;16:404–11. doi: 10.1046/j.1525-1497.2001.016006404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith C, Klosterbuer A, Levine AS. Military experience strongly influences post-service eating behavior and BMI status in American veterans. Appetite. 2009;52:280–9. doi: 10.1016/j.appet.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Trivedi AN, Grebla RC, Wright SM, Washington DL. Despite improved quality of care in the Veterans Affairs health system, racial disparity persists for important clinical outcomes. Health Aff (Millwood) 2011;30:707–15. doi: 10.1377/hlthaff.2011.0074. [DOI] [PubMed] [Google Scholar]
- 18.Justice AC, Dombrowski E, Conigliaro J, Fultz SL, Gibson D, Madenwald T, et al. Veterans Aging Cohort Study (VACS): overview and description. Med Care. 2006;44(8 Suppl):S13–24. doi: 10.1097/01.mlr.0000223741.02074.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide. Washington: FANTA; 2007. Aug, [Google Scholar]
- 20.Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127:303–10. doi: 10.1016/j.amjmed.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 21.Babor TF, Ramon de la Fuente J, Saunders J, Grant M. Geneva: World Health Organization; 1992. AUDIT. The Alcohol Use Disorders Identification Test: guidelines for use in primary health care. [Google Scholar]
- 22.Maisto SA, Conigliaro J, McNeil M, Kraemer K, Kelley ME. An empirical investigation of the factor structure of the AUDIT. Psychol Assess. 2000;12:346–53. doi: 10.1037//1040-3590.12.3.346. [DOI] [PubMed] [Google Scholar]
- 23.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158:1789–95. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 24.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363:6–9. doi: 10.1056/NEJMp1000072. [DOI] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 26.Justice AC, Freiberg MS, Tracy R, Kuller L, Tate JP, Goetz MB, et al. Does an index composed of clinical data reflect effects of inflammation, coagulation, and monocyte activation on mortality among those aging with HIV? Clin Infect Dis. 2012;54:984–94. doi: 10.1093/cid/cir989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Justice AC, McGinnis KA, Skanderson M, Chang CC, Gilbert CL, Goetz MB, et al. Towards a combined prognostic index for survival in HIV infection: the role of “non-HIV” biomarkers. HIV Med. 2010;11:143–51. doi: 10.1111/j.1468-1293.2009.00757.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Justice AC, Modur SP, Tate JP, Althoff KN, Jacobson LP, Gebo KA, et al. Predictive accuracy of the Veterans Aging Cohort Study index for mortality with HIV infection: a North American cross cohort analysis. J Acquir Immune Defic Syndr. 2013;62:149–63. doi: 10.1097/QAI.0b013e31827df36c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Werb D, Kerr T, Zhang R, Montaner JSG, Wood E. Methamphetamine use and malnutrition among street-involved youth. Harm Reduct J. 2010;7:5. doi: 10.1186/1477-7517-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21:71–7. doi: 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ma CT, Gee L, Kushel MB. Associations between housing instability and food insecurity with health care access in low-income children. Ambul Pediatr. 2008;8:50–7. doi: 10.1016/j.ambp.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 32.Baum MK, Campa A, Lai S, Sales Martinez S, Tsalaile L, Burns P, et al. Effect of micronutrient supplementation on disease progression in asymptomatic, antiretroviral-naive, HIV-infected adults in Botswana: a randomized clinical trial. JAMA. 2013;310:2154–63. doi: 10.1001/jama.2013.280923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keith-Jennings K, Sherman A. SNAP benefit cuts will affect thousands of veterans in every state [news release] 2013 Oct 28 [cited 2014 Jan 14] Available from: URL: http://www.cbpp.org/cms/index.cfm?fa=view&id=4039.
- 34.Bhargava V, Lee JS, Jain R, Johnson MA, Brown A. Food insecurity is negatively associated with home health and out-of-pocket expenditures in older adults. J Nutr. 2012;142:1888–95. doi: 10.3945/jn.112.163220. [DOI] [PubMed] [Google Scholar]