Abstract
This paper describes cultural relevance in physical activity intervention research with underrepresented populations. Seventy-one extant studies which tested interventions to increase physical activity among underrepresented adults were included. Verbatim descriptions of efforts to enhance cultural relevance of study designs and interventions were extracted and then content analyzed. We found strategies to enhance cultural relevance of interventions as soliciting input from population members, linking intervention content with values, addressing language and literacy challenges, incorporating population media figures, using culturally relevant forms of physical activity, and addressing specific population linked barriers to activity. Methodological approaches included specialized recruitment and study locations, culturally relevant measures, underrepresented personnel, and cost-awareness study procedures to prevent fiscal barriers to participation. Most reported activities were surface matching. Existing research neither compared the effectiveness of cultural relevance approaches to standardized interventions nor addressed economic, education, geographic, or cultural heterogeneity among groups.
Keywords: health promotion, exercise, minority groups, minority health
Introduction
Health inequities persist despite dramatic scientific advances over the past decades. In the United States, certain underrepresented racial/ethnic groups in general have poorer health than the population at large and are at increased risk for chronic diseases such as type 2 diabetes and cardiovascular disease [1, 2]. Physical activity (PA) has been shown to help prevent or delay the onset of these diseases as well as reduce or eliminate the risk of disease-related complications [3]. Underrepresented adults have significantly lower PA rates than the general population [4].
The need to increase PA among underrepresented populations has led to extensive research testing interventions. Researchers have called for efforts to increase the cultural relevance of interventions to targeted underrepresented populations to increase the interventions’ impact and sustainability [5–9]. The extent to which a study is culturally relevant for a particular underrepresented population can widely vary. The modification may be as simple as delivering interventions in locations where underrepresented participants congregate to having participants be involved in every aspect of design and implementation.
Cultural relevance may be viewed as having components of surface structure and/or deep structure [8]. Surface-structure involves matching study content to observable characteristics of the population through the use of personnel, locations, images, and language that are familiar to the target population [8]. Deep-structure matching goes further to incorporate the cultural beliefs, values, norms, and world view of population into the intervention [8]. In this regard, the design and implementation of a PA intervention might take into account such factors as the importance of religion and family, beliefs about exercise, and views regarding ideal body type. Depending on the study, strategies to address cultural relevance may focus on project personnel, the content of the intervention, or on the participants’ experiences of the process of participating in the study [10].
Although many possible strategies are available for increasing the cultural relevance of PA intervention studies, the extent to which investigators are actually matching methods and interventions to particular underrepresented target populations is unclear, and to date, no comprehensive review has been published that summarizes attempts to make PA intervention studies more culturally relevant [9, 11]. Nor has any previous review summarized researchers’ descriptions of cultural relevance aspects of their studies which they believed influenced intervention effectiveness.
This paper provides the results of a content analysis of published reports of underrepresented-targeted PA intervention studies to address the following questions:
What strategies have investigators reported to enhance cultural relevance of PA studies with regard to study design characteristics?
What strategies have investigators reported to enhance the cultural relevance of PA intervention content in extant research?
How have investigators interpreted the effectiveness of their cultural relevance efforts?
Method
In this report, the term underrepresented group refers specifically to those individuals living in the United States who have any of the following backgrounds or identities: African-American, Native American, Latino, Latino American, Asian, Asian American, Pacific Islander, Native Alaskan, or Native Hawaiian [12]. At present, no standardized terminology exists when referring to designs and interventions that intentionally take the target population’s race, ethnicity, and culture into consideration. Such efforts are variously described in the literature as cultural/ethnic/racial/minority adapted, aligned, anchored, appropriate, based, centered, compatible, competent, concordant, congruent, informed, matched, oriented, relevant, responsive, sensitive, shaped, syntonic, targeted, and tailored [6, 8, 9, 12–14]. Given the lack of standard use of these terms, this project uses cultural relevance when referring to any attempts to make research designs or interventions appropriate for underrepresented participants.
Content analysis was selected to address the research questions because it was an unobtrusive, cost-effective means of indirectly assessing researcher behavior by examination of their written communications. Content analysis also permitted examination of studies conducted years or decades ago.
Sample
The sample for the project was published reports of studies testing PA interventions in underrepresented adults. This project used primary studies from the sample of studies examined in a previously published comprehensive meta-analysis [12] and more recently published papers.
Search Strategies
For the parent study, multiple strategies were employed to ensure a comprehensive search [12]. An expert health sciences librarian used broad search terms for MEDLINE, PsychINFO, Cochrane Controlled Trials Register, EMBASE, Database of Abstracts of Reviews of Effectiveness, Healthstar, Dissertation Abstracts International, Sport Discus, CINAHL, Combined Health Information Database, and Educational Resources Information Center. Because search terms for underrepresented-specific studies are inconsistently applied, these terms for were not used to narrow the search. Searches were updated in early 2014 to locate more recent studies.
Searches were also conducted in the National Institutes of Health Research Portfolio Online Reporting Tool database as well as the mRCT database of clinical trials registries of 14 active and 16 archived registries. Author searches were conducted on the first three author names on eligible studies. Ancestry searches were performed on eligible studies and review papers. Hand searches were completed in 114 journals that frequently publish PA intervention reports.
Potential studies were reviewed by extensively trained research specialists to determine eligibility using a staged eligibility process. Although a time consuming process, these activities were necessary to ensure a comprehensive review.
Inclusion Criteria
Research reports distributed in English after 1959 were selected if they included motivational, behavioral, or educational interventions designed to change PA behavior. Intervention could include motivation, behavioral, or education strategies specifically designed to increase PA. Studies in which the intervention consisted solely of supervised exercise sessions were excluded. Studies were included regardless of interventionist characteristics, mode of delivery (e.g., face-to-face, mailed materials), physical setting (e.g., community center, clinic), and social setting (e.g., individual subjects, families, groups). Studies were included regardless of the extent of their descriptions of attempts to increase cultural relevance to capture the variations in cultural relevance descriptions.
Projects with predominantly underrepresented adults age 18 or older were included in this study. Studies of children and youth were excluded because different interventions would be necessary to match their developmental state. The parent meta-analysis focused on healthy adults, so studies of chronically ill adults were not part of the present analysis.
Abstracts from conference presentations were excluded because of the lack of descriptive content due to word limits. Studies with at least five subjects were included regardless of designs because design is not an important construct in relation to cultural relevance. To examine the range of completed trials, no inclusion criteria about statistical significance of findings was applied.
Data Extraction and Synthesis
The sampling unit for the project was individual published research reports. To characterize the sample, descriptive information was recorded from each report that included year of publication, sample size, percent underrepresented participants, gender distribution, and subjects’ mean age.
The context unit for the content analysis was a sentence or series of sentences. To address the first two research questions content was recorded which described one or multiple cultural relevance strategies employed in research methods or interventions. To address the third research question, content in the discussion sections of primary studies was reviewed to record how investigators interpreted the effectiveness of cultural relevance interventions. The recording unit for the analysis was any single strategy to increase the cultural relevance of research methods or interventions. To generate a data set for content analysis, each study was carefully read to identify context units. Authors were not contacted for additional information to avoid recall bias and bias related to social desirability.
Open-ended analysis was used to identify dominant themes and subject matter. Emergent coding was used establish categories based on a preliminary review of the text, and these categories were used to group related text from different studies into clusters [15–17]. To facilitate analysis, sorting, and grouping of text, relevant content was copied verbatim from each article into a Microsoft Word document. This approach permitted transformation of raw data into manageable content categories that were still grounded in the original text [18].
Results
Comprehensive searching located 54,893 possible reports for the parent study [12]. This large number of potential studies was considered because reliable search strategies to locate intervention studies specifically focused on underrepresented subjects are not available. Although 358 reports were eligible for the parent project because they included an intervention to increase PA in healthy adults and reported PA behavior outcomes, only 60 of those studies met the inclusion criteria for the present project; 11 newer studies were also included in this project [19–89]. Although searches went as far back as 1960, the earliest study eligible for this project was published in 1990. In fact, only 10 eligible papers were published prior to 2000. Forty reports indicate the studies were funded.
Sample sizes were generally modest, with a median sample size of 31 for treatment groups and 39 for comparison groups. Subjects were exclusively female in 30 studies, and the median percent of women across all studies was 100%. The median participant age was 44.19 years.
The most frequently studied group was African Americans, follow by Latinos. African Americans constituted the majority of the participants in 30 studies (over 75% of the sample in 24 studies, entire sample in 21 studies). Latinos were the predominant participants in 8 studies, and they constituted the entire sample in 13 studies. More Latino focused studies were published in recent years than in earlier years. Three studies targeted entirely Native American Indian subjects, and two studies targeted entirely Native Hawaiian or Samoan subjects.
Descriptions of strategies to make designs and interventions culturally relevant varied from just a few words to several sentences. Table 1 summarizes the strategies to enhance cultural relevance identified in the studies analyzed for this project. Twenty-one eligible studies did not report any strategy to increase the cultural relevance of the study.
Table 1.
Examples of Strategies to Enhance Cultural Relevance of Physical Activity Intervention Research
| Category | Theme | Examples |
|---|---|---|
| Research team members | Underrepresented group member researchers | Underrepresented member principal/co-investigator |
| Underrepresented group member staff | Underrepresented group member project staff as recruiters, interventionists, and data collectors | |
| Recruiting or training culturally competent staff | ||
| Church members as interventionists | ||
| Methodology features | Recruitment | Recruitment through churches, health care facilities, schools, businesses, community events, worksites, |
| Recruit via target audience mass media | ||
| Use of recruiter from underrepresented group | ||
| Recruitment by church staff or members | ||
| Involve group members in designing recruitment | ||
| Study location | Target population community centers or businesses | |
| Intended participant churches or schools | ||
| Measures | Measures in appropriate language | |
| Measures administered by underrepresented staff | ||
| Cost awareness | Provide childcare | |
| Conduct study in participants’ neighborhood | ||
| Study site near subway or bus station | ||
| Provide transportation costs | ||
| Interventions | Input from members to design interventions | Advisory council or groups |
| Focus groups | ||
| Survey members | ||
| Intervention materials reviewed by underrepresented advisers | ||
| Underrepresented group member-linked values | Families and social interactions | |
| Interrelationships among physical, spiritual, and psychological health | ||
| Convey information valuing experience and intuition | ||
| Use group concepts, stories, metaphors | ||
| Language and literacy issues | Interventions and measures in participants’ language | |
| Project personnel speak participants’ language | ||
| Reduce reading level of project materials | ||
| Use graphical project materials over written text | ||
| Media | Target group specific celebrities, role models, and well-known personalities | |
| Target group articles from group publications | ||
| PA form | Group-linked exercise forms such as dance | |
| Underrepresented group linked barriers to PA | Address family responsibilities as a barrier to PA | |
| Address fatalism as a barrier to PA | ||
| Address self-esteem as a barrier to PA |
Research Team Members
Involving underrepresented members on the research team was a commonly used strategy. Underrepresented members participated as investigators, interventionists, and other project personnel.
Investigators
The reported level of participation of an underrepresented investigator varied from naming an underrepresented co-investigator [27, 70] to much more extensive participation such as involving underrepresented members from initial planning stages of developing the project, conducting a needs assessment, developing interventions, recruiting participants, designing data collection instruments, and the like [23, 75, 83]. Very few papers reported whether the research team included members of the underrepresented group. Millard [27] noted that their research team included several people with professional training in cultural awareness, including medical anthropologists.
Project staff
Employing underrepresented group members as project staff was a common strategy [22, 35, 36, 57, 58, 78]. Depending on the study, project staff varied from volunteers from neighborhoods, communities, or churches to paid professionals such as dieticians and nurses. Underrepresented project staff could be involved in any phase of the research. For example, interventions were often delivered by group members [19, 26, 27, 33, 36, 38, 46, 56, 60, 61, 65, 66, 69–72, 76–78, 85, 88]. In some church-based projects, church members were trained to deliver interventions [38, 63, 69, 78]. Training project staff to achieve cultural competence was also reported [54, 55].
Methodology Features
Investigators used research design decisions to facilitate successful trials. Most specified design modifications were related to successfully engaging or retaining subjects across longitudinal studies.
Recruitment
The most frequently employed strategy to increase recruitment of members of a specific group was to target locations or activities frequented by members of the group. Churches were often used as recruitment sites [38, 40, 55, 63, 69–71, 78, 85]. Church pastors, church members, and promotoras were involved in recruitment [38, 56, 63, 70, 71, 78, 85]. The second most common site of recruitment was health care facilities and services that are designed to serve underrepresented adults [24, 28, 34, 37, 45, 57, 64, 65, 84–86, 89, 90].
Other recruitment sites included schools such as traditional public schools, English as a second language programs, and vocational training classes [34–36, 46, 55, 85]. Some investigators recruited at local businesses frequented by potential subjects, such as beauty salons [61] and grocery stores [34, 54, 55, 61, 71]. Worksites with strong potential subject representation were selected for recruitment [33, 35, 42, 52, 61]. Other studies recruited through ethnic civic, social, and fraternal organizations [23, 45, 54, 55, 71]. Another strategy used was snowball sampling among family and friends of participants [37, 65, 89].
Recruitment on a wider scale was attempted in several studies. Some investigators recruited at community events such as health fairs [23, 26, 61, 69, 85, 87, 89], whereas others used targeted mass-mailings and newspaper announcements and flyers specifically aimed at potential participants [23, 34, 45, 54, 55, 67, 71, 76, 87]. Some investigators targeted a particular region or community [27, 28, 38, 58, 76, 77, 85]. A few studies involved underrepresented members in designing or implementing recruitment strategies [23, 26, 27, 36, 40, 67, 71].
Study Site Strategies
Several studies were conducted at specific locations to facilitate engagement. Just as they functioned for recruitment, local churches were also commonly used for intervention delivery and data collection [24, 35, 38, 40, 49, 55, 56, 63, 69–71, 78, 85]. Other underrepresented-specific sites for intervention delivery included community settings [41, 58, 86] such as underrepresented group member owned or frequented fitness centers [22, 28, 55, 57, 71], and hospitals serving underrepresented communities [37, 41, 54, 65]. Quinn employed church members to follow participants across the study to avoid attrition [78].
Measures
Some attention in selecting measures was apparent. Strategies included using measures in the native language of participants [30, 46, 75]. Another strategy was having group member staff administer measures [35]. Measuring constructs related to ethnicity such as acculturation was also reported to enhance the cultural relevance of studies [71].
Cost Considerations
Some investigators designed projects with an awareness that limited participant incomes would hinder or prevent their study participation. Childcare expenses were managed in several projects [36, 54, 55, 85, 91]. Some study locations were selected for proximity to subway or bus lines or participants’ transportation expenses were covered by the study [27, 36, 37]. Churches and community clinics were used because they were more likely to be within easy traveling distance for subjects [37]. One project took cost into consideration when recommending PA behaviors [68].
Intervention Characteristics
Six major themes were identified with respect to strategies to match the intervention to the underrepresented group: soliciting input from members in designing interventions; linking the intervention to group values; addressing problems of language and literacy; using specific media and media personalities; suggesting socially and culturally acceptable forms of PA; and addressing cultural beliefs, norms, and values that may act as barriers to increased PA. It should be noted that while several studies indicated that interventions were culturally relevant, the authors but did not provide details about the content [35, 48, 66, 71, 75]. For example, one study indicated that a culturally sensitive exercise counseling intervention included materials that were designed to address African-American socio-cultural concerns about exercise, but the authors did not describe the specific content addressing those concerns [71].
Input from Underrepresented Informants to Design Interventions
Several studies involved underrepresented group members in designing interventions or procedures [22, 30, 37, 38, 57, 61, 75, 76]. In some cases, input was obtained using focus or advisory groups [28, 29, 35, 36, 56, 57, 60, 61, 69, 75, 89]. In one study, this involvement was so pervasive that participants directed actual sessions via interactive approaches, designed project social activities, and developed the study logo and name [61]. Another study used indirect information from the population via existing literature to design culturally relevant interventions [69].
Underrepresented Group-linked Values
Several studies included families in interventions or incorporated social support by friends and family into interventions [33, 35, 36, 55, 61, 66, 77, 92]. Some interventions emphasized the importance of families as a reason for maintaining a healthy lifestyle [65].
While many studies were conducted in churches, studies did not always link interventions to spirituality; the church merely served as a convenient location for interacting with participants. Faith components of interventions were alluded to in some interventions [35, 40, 54], whereas in others the interrelationships among physical, psychological, and spiritual health were overtly emphasized and described [35, 70].
Several interventions conveyed information in a manner consistent with experience and intuition as ways of knowing, as compared to empiricism as the source of knowledge. These interventions used testimonials or narrative forms of information [36]. Others used underrepresented role models to convey the importance of PA [29, 35, 89].
The manner of intervention delivery and who delivered the interventions could contribute to cultural relevance of interventions. Underrepresented group member interventionists could have used communication strategies and cultural metaphors that would make interventions culturally relevant. This was alluded to in a few studies [35, 65]. Corsino [23] emphasized in their study that using food names specific to certain regions in Latin America acknowledged cultural differences among the participants.
Language and Literacy
In populations in which language difference was an issue, investigators provided study materials in the native language and project staff were conversant in that language [22, 23, 25, 27, 28, 30, 34, 38, 42, 46, 74, 77, 80, 85]. Several studies reported using measures in the language most familiar to participants [38, 42, 57, 71, 74, 75, 77, 80, 85]. Use of interventionists who were of the same group as participants was another method of overcoming language barriers [19, 23, 25–27, 33, 36, 56, 60, 61, 65, 66, 69–72, 76, 85, 88]. To overcome problems related to literacy, investigators sometimes relied on graphical content or lowered the reading level of written content for all subjects [28, 56, 65, 75, 80, 91].
Media Approaches
Media used to promote physical activity may be more compelling if study participants can identify with or relate the images and content. Several studies used media with content and images that would resonate with the target population [22, 24, 28, 35, 36, 55, 63, 65, 71, 72, 88]. Walcott-McQuigg included articles from magazines popular with the target group in the intervention [88]. Nichols used materials depicting women who resembled the population of study [72]. Leeman-Castillo used a computerized multimedia program that matched images of role models to the user’s characteristics [24]. Because narrative approaches may be more persuasive for some underrepresented participants, studies also used anecdotes or testimonials from members of the target group as a method of social interaction to promote PA [35, 55].
Culturally Matched PA
Samples will be more likely to undertake PA if it is in a form that is culturally acceptable, popular, and available to those with limited financial resources. For example, walking may not be an acceptable form of exercise in the Latino community because it is viewed as indicative of low socioeconomic status [85]. A number of interventions in the project sample incorporated culturally specific forms of PA [19, 23, 49, 53, 65, 66, 68, 70, 71, 77, 80, 91]. One dance intervention integrated physical, mental, and spiritual health as common in the underrepresented group [70].
Culture-linked Barriers to PA
Cultural values, norms, and belief systems within a particular population may function as barriers to PA behavior change, and a number of interventions in the sample addressed these issues [19, 35, 46, 54, 85]. Because of the pre-eminent importance of family for some groups, multiple family obligations and commitments can often limit time available for PA. This barrier was addressed in the studies by Albright [19], Collins [46], and Fitzgibbon [54]. An intervention to counter the high rates of diabetes in the Cherokee nation included efforts to overcome the pervasive, fatalistic perception within tribe members that developing diabetes was inevitable [35]. Collins addressed low self-esteem in Latina women that undermines their motivation to improve their physical health [46]. Staten noted that within the Latino community, countering erroneous, culturally ingrained beliefs about the causes of diabetes was necessary so that individuals were more likely to make changes in their health behaviors [85].
Cultural Relevance Efforts and Intervention Effectiveness as Interpreted by Authors
Most authors provided some interpretation in the discussion section regarding the effectiveness of their attempts to increase cultural relevance. Authors emphasized the importance of community member involvement in devising recruitment strategies [26, 40, 67], and in designing and delivering interventions [22, 25, 29, 30, 35, 60, 61, 63, 69–71, 75, 78]. Several researchers interpreted their interventions as effective because they addressed shared meanings and values, including faith themes [54, 69, 70, 85, 91].
The social context of PA behavior change was addressed by several authors who described the importance of family and social support to enhance PA and others who noted family and social obligations may hinder PA [33, 34, 46, 61, 66, 71]. The economic circumstance of some underrepresented populations was acknowledged by many authors. For example, they noted common barriers to PA which were difficult to address in research studies such as economic instability in families, inadequate resources to access safe exercise facilities, and unsafe environments for exercise [35, 36, 49, 61, 76, 77, 83, 85, 89, 91]. Authors did not propose viable solutions to these complex problems.
Although authors appeared to believe their interventions were effective because of cultural relevance of interventions, a few authors noted that research comparing culturally relevant and standard interventions is lacking. For example, Kumanyika noted that research testing the impact of interventionist characteristics on effectiveness is needed [65]. Other investigators noted future research should examine differences within underrepresented groups [59, 70, 80].
Summary
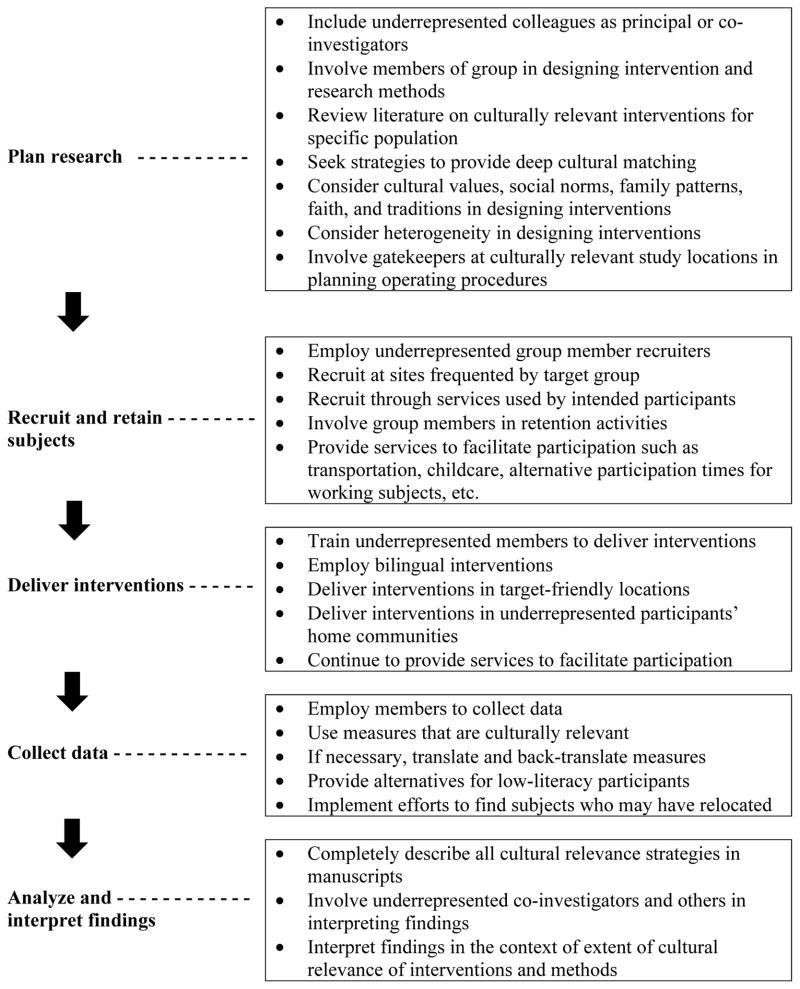
Diverse strategies were used to recruit and retain underrepresented participants as well as deliver interventions which were culturally relevant. Researchers interpreted their strategies as being effective to improve PA in the completed studies. To provide a concise summary of strategies for researchers to use in planning future studies, data from the content analysis are also presented in relation to the different phases of research: planning, recruitment, intervention delivery, data collection, and interpretation of study findings (Figure 1).
Figure 1.
Strategies to enhance cultural relevance at each stage of the research process
Discussion
In the research reports included in this content analysis, surface matching predominated in the strategies for increasing the cultural relevance of PA interventions for underrepresented adults [11, 81]. Typical strategies included employing underrepresented group project staff. Studies were often conducted in locations frequented by members of groups, for example, a number of studies involving African Americans were conducted in churches. For studies involving non-native English speakers, interventions and evaluations were conducted in the participants’ native language. Much less evidence was found for deep structure matching to values and belief systems [8]. The cultural values explicitly mentioned in the few reports describing these features included family and social interaction, spirituality, fatalism, and testimonial narrative information about PA behavior [8, 93].
Although little overt evidence for deep structure matching was found in the studies analyzed, it must be considered that such matching could nevertheless have occurred. In studies in which the interventionists were members of the same underrepresented group as participants, interventionists could share or at least relate to some of the same beliefs and values as participants and might either consciously or unconsciously embed historical social references into their communications. Use of underrepresented interventionists would increase the likelihood of positive social interactions, expressiveness, and sharing of testimonial or experiential type information, as compared to empiricism as a way of knowing [8]. None of the reports explicitly described interventionists’ approaches to interacting with study participants, so the possibility that underrepresented interventionists contributed to deep-structure matching remains speculative. Also, using matched project staff would serve to increase credibility and trustworthiness and decrease concerns about mistreatment by authority figures, health care providers, and government officials [5, 8].
Researchers may have overtly incorporated deep structure matching into studies but simply failed to describe those efforts in the published reports [94–96]. Incomplete reporting of intervention content in published journal articles is well-documented [97–99]. It is possible that underrepresented investigators may view making interventions cultural relevant as the normative standard so that these aspects of interventions do not need to be mentioned in reports [11]. It is possible that research teams with underrepresented investigators design interventions which are more culturally relevant than studies without such investigators. Very few studies reported whether members of underrepresented groups were principal or co-investigators. The problem with vague or incomplete descriptions about cultural relevance is that in cases of unsuccessful interventions, readers are unsure whether the failure was related to content. When interventions are successful, a lack of details regarding culturally relevant content will prevent their successful implementation in practice [11].
All interventions are culturally influenced [100, 101]. Traditional PA interventions are based on shared values and worldviews of majority populations in North America and Western Europe [102]. For example, values of individualism are evident in interventions based on the assumption that the individual is the basic unit of society and thus that individuals will be motivated act to improve their personal health [93, 103]. Future research which makes these cultural attributes visible is essential to determine their impact on intervention effectiveness. The greater attention paid to strategies to engage underrepresented participants over strategies to effectively increase PA behavior may partially account for the limited effectiveness of interventions [11].
Our previous meta-analysis of 60 of the 71 studies included in this project found that PA interventions overall had only a modest, non-clinically significant effect on increasing PA behavior in underrepresented populations (standardized mean difference effect size of 0.172 for treatment vs. control comparisons at outcome and 0.312 for treatment pre- post-intervention comparisons) [12]. Significant heterogeneity in the relative effectiveness of interventions was detected across studies; however, moderators of effect size, including cultural relevance, were not reported in the previous work [12]. Meta-analyses of mental health treatments have shown that effect sizes are larger when treatments are culturally relevant [102, 104–106], suggesting that modifications to increase cultural relevance can have a positive effect on outcomes. Whether culturally relevant content has a clinically significant impact on PA behavior remains to be determined, as the comparative effectiveness of culturally relevant PA interventions versus standard interventions in underrepresented populations has not been extensively investigated [6, 95]. Another unknown is the extent of cultural relevance necessary to achieve PA behavior change [107]. Can interventions designed for the general population simply have cultural content added in certain key areas? Or must a culturally relevant intervention be designed completely ab initio for the target group in question?
Another issue that remains unaddressed is the impact of heterogeneity within underrepresented groups on effectiveness of culturally relevant interventions. Audience segmentation strategies are typically used to increase cultural relevance [108]. However, by classifying individuals into broad racial/ethnic categories, investigators may make erroneous assumptions about the group as a whole and miss important cultural distinctions among subgroups [5, 100]. Basing interventions on assumed common attributes can be viewed as a form of stereotyping that may ultimately damage efforts to create effective interventions [100]. Even among subgroups, culture is experienced differently among individuals [8, 103]. None of the studies in the present analysis described cultural tailoring with content matched to each subject on the basis of individually assessed cultural characteristics [103]. The level of disaggregation necessary to create effective interventions while still remaining feasible for widespread adoption remains unclear [103].
Education, income, and geographic heterogeneity within underrepresented groups has not been adequately studied. Sample sizes in future studies need to be adequate to allow for exploratory analyses of intervention effectiveness by variations within underrepresented groups. Future research should address spiritual heterogeneity, extant research has focused on Christian spirituality. A related topic is the need to balance economic realities, such as the fiscal sustainability of walking as a form of exercise, with the potential preference and cultural meaning forms of exercise, such as organized dance classes, which may be less economically sustainable.
Observations and conclusions in this project were limited by the information in the research reports. Although researchers may possess detailed procedure manuals that fully describe cultural relevance, this information is often not made available to research consumers, so conclusions must perforce be drawn from information provided in published reports. This analysis focused only on studies involving healthy adults. Whether studies conducted with chronically ill adults would differ with respect to cultural relevance content is not known. Unfortunately, no standardized language is yet available to describe cultural relevance approaches. This limits attempts to summarize strategies across primary research. Despite these limitations, this was the first project to summarize cultural relevance strategies in extant PA research.
Opportunities for future research in the area of PA behavior change are enormous. Whether making interventions more culturally relevant can lead to clinically significant, persistent increases in PA is a question yet to be adequately addressed. Identifying a causal relationship between the presence of culturally relevant content and increased PA will require rigorous designs with appropriate comparison groups [9, 100]. To address the question of whether interventions must be specifically tailored to a specific underrepresented group, primary studies are needed that compare culturally relevant general interventions to those interventions specifically created with a particular underrepresented group in mind. The relative contributions of surface and deep structure strategies also need to be investigated as do methods for overcoming cultural, social, and psychological barriers to increasing PA [7, 9, 11]. Regardless of the area of investigation, detailed descriptions of cultural relevance strategies will be necessary to permit critical assessment of findings and allow implementation in practice [11].
Conclusion
In the United States, racial and ethnic underrepresented groups disproportionately suffer from chronic illnesses. If these racial/ethnic disparities in health status are not addressed, their burden on public health will continue to increase, as currently underrepresented individuals are projected to account for nearly 50% of the total U.S. population by 2050 [109]. Reducing health disparities validates the need for more research to identify effective interventions to modify health behaviors known to affect disease risk, including PA behavior. Because receptivity to health messages is strongly influenced by beliefs, values, life experiences, cultural history, and group identity, a central aspect of this research must be to identify those cultural relevance characteristics that yield the most significant improvements in PA behavior for any given population.
Acknowledgments
Financial support provided by a grant from the National Institutes of Health (R01NR009656) to Vicki Conn, principal investigator.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Vicki S. Conn, Email: conn@missouri.edu, University of Missouri, School of Nursing, S317 School of Nursing, University of Missouri, Columbia, MO 65211 573 882 0231 (office), 573 884 4544 (fax).
Keith Chan, Email: chankc@missouri.edu, University of Missouri, School of Nursing, S323 School of Nursing, University of Missouri, Columbia, MO 65211, 573 882 0231, 573 884 4544.
JoAnne Banks, Email: wallacejb@wssu.edu, Winston Salem State University, Division of Nursing, 601 Martin Luther King Jr. Drive, Winston-Salem, NC 27110, 336-750-3086 (office), 336 750 2599 (fax).
Todd M. Ruppar, Email: ruppart@missouri.edu, University of Missouri, School of Nursing, S423 School of Nursing, University of Missouri, Columbia, MO 65211, 573 884 5153 (office), 573 884 4544 (fax).
Jane Scharff, Email: jane.scharff@montana.edu, University of Missouri, School of Nursing, S318 School of Nursing, University of Missouri, Columbia, MO 65211, 573 882 0231 (office), 573 884 4544 (fax).
References
- 1.Agency for Healthcare Research and Quality. Disparities in healthcare quality among racial and ethnic minority groups. 2011 Retrieved from http://www.ahrq.gov/research/findings/nhqrdr/nhqrdr10/minority.html.
- 2.Liao Y, Bang D, Cosgrove S, et al. Surveillance of health status in minority communities - racial and ethnic approaches to community health across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. Morbidity and Mortality Weekly Report. 2011;60:1–41. [PubMed] [Google Scholar]
- 3.Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33:e147–167. doi: 10.2337/dc10-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Minority health surveillance - REACH U.S. 2009. 2012 Retrieved from http://www.cdc.gov/features/dsreachus/
- 5.Kreuter MW, McClure SM. The role of culture in health communication. Annual Review of Public Health. 2004;25:439–455. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- 6.Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: examples from parent training. Clinical Psychology: Science and Practice. 2006;13:295–310. doi: 10.1111/j.1468-2850.2006.00042.x. [DOI] [Google Scholar]
- 7.Mitrani V. Reducing health disparities for Hispanics through the development of culturally tailored interventions. Hispanic Health Care International. 2009;7:2–4. doi: 10.1891/1540-4153.7.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethnicity & Disease. 1999;9:10–21. [PubMed] [Google Scholar]
- 9.Whitt-Glover MC, Kumanyika SK. Systematic review of interventions to increase physical activity and physical fitness in African-Americans. American Journal of Health Promotion. 2009;23:S33–56. doi: 10.4278/ajhp.070924101. [DOI] [PubMed] [Google Scholar]
- 10.Sue S, Zane N, Nagayama Hall GC, Berger LK. The case for cultural competency in psychotherapeutic interventions. Annual Review of Psychology. 2009;60:525–548. doi: 10.1146/annurev.psych.60.110707.163651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumanyika SK, Yancey AK. Physical activity and health equity: evolving the science. American Journal of Health Promotion. 2009;23:S4–7. doi: 10.4278/ajhp.23.6.s4. [DOI] [PubMed] [Google Scholar]
- 12.Conn VS, Phillips LJ, Ruppar TM, Chase JA. Physical activity interventions with healthy minority adults: meta-analysis of behavior and health outcomes. Journal of Health Care for the Poor and Underserved. 2012;23:59–80. doi: 10.1353/hpu.2012.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aten JD, Boan D. Toolkit: Culturally Adapting and Implementing Evidence-Based Practices for Disaster and Humanitarian Settings. Humanitarian Disaster Insitute; Wheaton College, Wheaton, IL: 2013. [Google Scholar]
- 14.Sanders Thompson VL, Cavazos-Rehg PA, Jupka K, et al. Evidential preferences: cultural appropriateness strategies in health communications. Health Education Research. 2008;23:549–559. doi: 10.1093/her/cym029. [DOI] [PubMed] [Google Scholar]
- 15.Coffey AJ, Atkinson PA. Making Sense of Qualitative Data. Sage Publications; Thousand Oaks, California: 1996. [Google Scholar]
- 16.Weber RP. Basic Content Analysis. Sage Publications; Thousand Oaks, California: 1990. [Google Scholar]
- 17.Patton MQ. Qualitative Research and Evaluation Methods. Sage Publications; Thousand Oaks, California: 2002. [Google Scholar]
- 18.Berg BL. Qualitative Research Methods for the Social Sciences. Allyn and Bacon; Boston: 2001. [Google Scholar]
- 19.Albright CL, Pruitt L, Castro C, et al. Modifying physical activity in a multiethnic sample of low-income women: one-year results from the IMPACT (Increasing Motivation for Physical ACTivity) project. Annals of Behavioral Medicine. 2005;30:191–200. doi: 10.1016/j.apnr.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 20.Flannery K, Resnick B, Galik E, et al. The Worksite Heart Health Improvement Project (WHHIP): feasibility and efficacy. Public Health Nursing. 2012;29(5):455–466. doi: 10.1111/j.1525-1446.2012.01023.x. [DOI] [PubMed] [Google Scholar]
- 21.Olvera N, Bush JA, Sharma SV, et al. BOUNCE: a community-based mother-daughter healthy lifestyle intervention for low-income Latino families. Obesity. 2010;18(Suppl 1):S102–104. doi: 10.1038/oby.2009.439. [DOI] [PubMed] [Google Scholar]
- 22.Ayala GX T San Diego Prevention Research Center. Effects of a promotor-based intervention to promote physical activity: Familias Sanas y Activas. American Journal of Public Health. 2011;101:2261–2268. doi: 10.2105/ajph.2011.300273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corsino L, Rocha-Goldberg MP, Batch BC, et al. The Latino Health Project: pilot testing a culturally adapted behavioral weight loss intervention in obese and overweight Latino adults. Ethnicity & Disease. 2012;22(1):51–57. [PMC free article] [PubMed] [Google Scholar]
- 24.Leeman-Castillo B, Beaty B, Raghunath S, Steiner J, Bull S. LUCHAR: using computer technology to battle heart disease among Latinos. American Journal of Public Health. 2010;100(2):272–275. doi: 10.2105/ajph.2009.162115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marquez B, Wing RR. Feasibility of enlisting social network members to promote weight loss among Latinas. Journal of the Academy of Nutrition & Dietetics. 2013;113(5):680–687. doi: 10.1016/j.jand.2013.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marshall SJ, Nicaise V, Ji M, et al. Using step cadence goals to increase moderate-to-vigorous-intensity physical activity. Medicine & Science in Sports & Exercise. 2013;45(3):592–602. doi: 10.1249/mss.0b013e318277a586. [DOI] [PubMed] [Google Scholar]
- 27.Millard AV, Graham MA, Wang X, et al. Pilot of a diabetes primary prevention program in a hard-to-reach, low-income, immigrant Hispanic population. Journal of Immigrant and Minority Health. 2011;13(5):906–913. doi: 10.1007/s10903-010-9412-y. [DOI] [PubMed] [Google Scholar]
- 28.Ockene IS, Tellez TL, Rosal MC, et al. Outcomes of a Latino community-based intervention for the prevention of diabetes: the Lawrence Latino Diabetes Prevention Project. American Journal of Public Health. 2012;102(2):336–342. doi: 10.2105/ajph.2011.300357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilder B, Schuessler J, Hendricks CS, Grandjean P. Implementing a physical activity program for underserved African-American women. Journal of National Black Nurses Association. 2010;21(2):16–26. [PubMed] [Google Scholar]
- 30.Pekmezi DW, Neighbors CJ, Lee CS, et al. A culturally adapted physical activity intervention for Latinas: a randomized controlled trial. American Journal of Preventive Medicine. 2009;37(6):495–500. doi: 10.1016/j.amepre.2009.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Annesi JJ. Effects of a cognitive behavioral treatment package on exercise attendance and drop out in fitness centers. European Journal of Sport Science. 2003;3:1–16. doi: 10.1080/17461390300073206. [DOI] [Google Scholar]
- 32.Annesi JJ. Relations of changes in exercise self-efficacy, physical self-concept, and body satisfaction with weight changes in obese white and African American women initiating a physical activity program. Ethnicity & Disease. 2007;17:19–22. doi: 10.1016/j.bodyim.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Ard JD, Rosati R, Oddone EZ. Culturally-sensitive weight loss program produces significant reduction in weight, blood pressure, and cholesterol in eight weeks. Journal of the National Medical Association. 2000;92:515–523. [PMC free article] [PubMed] [Google Scholar]
- 34.Avila P, Hovell MF. Physical activity training for weight loss in Latinas: a controlled trial. International Journal of Obesity & Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 1994;18:476–482. [PubMed] [Google Scholar]
- 35.Bachar JJ, Lefler LJ, Reed L, et al. Cherokee Choices: a diabetes prevention program for American Indians. Preventing Chronic Disease. 2006;3:1–9. [PMC free article] [PubMed] [Google Scholar]
- 36.Baranowski T, Simons-Morton B, Hooks P, Henske J, et al. A center-based progam for exercise change among Black-American families. Health Education Quarterly. 1990;17:179–196. doi: 10.1177/109019819001700205. [DOI] [PubMed] [Google Scholar]
- 37.Becker DM, Yanek LR, Johnson WR, Jr, et al. Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation. 2005;111:1298–1304. doi: 10.1161/01.cir.0000157734.97351.b2. [DOI] [PubMed] [Google Scholar]
- 38.Bell AC, Swinburn BA, Amosa H, Scragg RK. A nutrition and exercise intervention program for controlling weight in Samoan communities in New Zealand. International Journal of Obesity. 2001;25:920–927. doi: 10.1038/sj.ijo.0801619. [DOI] [PubMed] [Google Scholar]
- 39.Berry D, Savoye M, Melkus G, Grey M. An intervention for multiethnic obese parents and overweight children. Applied Nursing Research. 2007;20:63–71. doi: 10.1016/j.apnr.2006.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bopp MJ. PhD. University of South Carolina; Columbia, SC: 2005. Evaluation of a Faith-Based Physical Activity Intervention. [Google Scholar]
- 41.Burden RW, Kumar RN, Phillips DL, Borrego ME, Galloway JM. Hyperlipidemia in Native Americans: evaluation of lipid management through a cardiovascular risk reduction program. Journal of the American Pharmaceutical Association. 2002;42:652–655. doi: 10.1331/108658002763029634. [DOI] [PubMed] [Google Scholar]
- 42.Campbell MK, Tessaro I, DeVellis B, et al. Effects of a tailored health promotion program for female blue-collar workers: health works for women. Preventive Medicine. 2002;34:313–323. doi: 10.1006/pmed.2001.0988. [DOI] [PubMed] [Google Scholar]
- 43.Cardinal BJ, Cardinal MK. Changes in exercise behavior and exercise identity associated with a 14-week aerobic exercise class. Journal of Sport Behavior. 1997;20:377–386. [Google Scholar]
- 44.Cardinal BJ, Sachs ML. Effects of mail-mediated, stage-matched exercise behavior change strategies on female adults’ leisure-time exercise behavior. Journal of Sports Medicine and Physical Fitness. 1996;36:100–107. [PubMed] [Google Scholar]
- 45.Chen AH, Sallis JF, Castro CM, et al. A home-based behavioral intervention to promote walking in sedentary ethnic minority women: project WALK. Women’s Health. 1998;4:19–39. [PubMed] [Google Scholar]
- 46.Collins R, Lee RE, Albright CL, King AC. Ready to be physically active? The effects of a course preparing low-income multiethnic women to be more physically active. Health Education and Behavior. 2004;31:47–64. doi: 10.1177/1090198103255529. [DOI] [PubMed] [Google Scholar]
- 47.Cook C, Simmons G, Swinburn B, Stewart J. Changing risk behaviours for non-communicable disease in New Zealand working men--is workplace intervention effective? New Zealand Medical Journal. 2001;114:175–178. [PubMed] [Google Scholar]
- 48.Craft L, Freund KM, Culpepper L, Perna FM. Intervention study of exercise for depressive symptoms in women. Journal of Women’s Health. 2007;16:1499–1509. doi: 10.1089/jwh.2007.0483. [DOI] [PubMed] [Google Scholar]
- 49.Doshi NJ, Hurley RS, Garrison ME, Stombaugh IS, et al. Effectiveness of a nutrition education and physical fitness training program in lowering lipid levels in the Black elderly. Journal of Nutrition for the Elderly. 1994;13:23–33. doi: 10.1300/J052v13n03_02. [DOI] [PubMed] [Google Scholar]
- 50.Dutton GR, Martin PD, Welsch MA, Brantley PJ. Promoting physical activity for low-income minority women in primary care. American Journal of Health Behavior. 2007;31:622–631. doi: 10.5993/ajhb.31.6.7. [DOI] [PubMed] [Google Scholar]
- 51.Early JL, Apovian CM, Aronne LJ, et al. Sibutramine plus meal replacement therapy for body weight loss and maintenance in obese patients. Obesity. 2007;15:1464–1472. doi: 10.1038/oby.2007.175. [DOI] [PubMed] [Google Scholar]
- 52.Elliott-Loyd MB. PhD. Georgia State University; Atlanta, GA: 1998. The Effect of an 18-Week Walking Program on Body Composition in Black and White Sedentary, Overweight Females (Black Women, White Women, Exercise) [Google Scholar]
- 53.Engels HJ, Gretebeck RJ, Gretebeck KA, Jimenez L. Promoting healthful diets and exercise: efficacy of a 12-week after-school program in urban African Americans. Journal of the American Dietetic Association. 2005;105:455–459. doi: 10.1016/j.jada.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 54.Fitzgibbon ML, Stolley MR, Ganschow P, et al. Results of a faith-based weight loss intervention for black women. Journal of the National Medical Association. 2005;97:1393–1402. [PMC free article] [PubMed] [Google Scholar]
- 55.Fitzgibbon ML, Stolley MR, Schiffer L, et al. A combined breast health/weight loss intervention for Black women. Preventive Medicine. 2005;40:373–383. doi: 10.1016/j.ypmed.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 56.Goldfinger J, Arniella G, Wylie-Rosett J, Horowitz C. Project HEAL: peer eduction leads to weight loss in Harlem. Journal of Health Care for the Poor and Underserved. 2008;19:180–192. doi: 10.1353/hpu.2008.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harralson TL, Emig JC, Polansky M, et al. Un corazon saludable: factors influencing outcomes of an exercise program designed to impact cardiac and metabolic risks among urban Latinas. Journal of Community Health. 2007;32:401–412. doi: 10.1007/s10900-007-9059-3. [DOI] [PubMed] [Google Scholar]
- 58.Harvey-Berino J, Rourke J. Obesity prevention in preschool Native-American children: a pilot study using home visiting. Obesity Research. 2003;11:606–611. doi: 10.1038/oby.2003.87. [DOI] [PubMed] [Google Scholar]
- 59.Hong K, Li Z, Wang HJ, Elashoff R, Heber D. Analysis of weight loss outcomes using VLCD in black and white overweight and obese women with and without metabolic syndrome. International Journal of Obesity. 2005;29:436–442. doi: 10.1038/sj.ijo.0802864. [DOI] [PubMed] [Google Scholar]
- 60.Kanders BS, Ullmann-Joy P, Foreyt JP, et al. The Black American Lifestyle Intervention (BALI): the design of a weight loss program for working-class African-American women. Journal of the American Dietetic Association. 1994;94:310–312. doi: 10.1016/0002-8223(94)90374-3. [DOI] [PubMed] [Google Scholar]
- 61.Karanja N, Stevens VJ, Hollis JF, Kumanyika SK. Steps to soulful living (steps): a weight loss program for African-American women. Ethnicity & Disease. 2002;12:363–371. [PubMed] [Google Scholar]
- 62.Keller C, Trevino RP. Effects of two frequencies of walking on cardiovascular risk factor reduction in Mexican American women. Research in Nursing and Health. 2001;24:390–401. doi: 10.1002/nur.1039. [DOI] [PubMed] [Google Scholar]
- 63.Kennedy BM, Paeratakul S, Champagne CM, et al. A pilot church-based weight loss program for African-American adults using church members as health educators: a comparison of individual and group intervention. Ethnicity & Disease. 2005;15:373–378. [PubMed] [Google Scholar]
- 64.Kochevar AJ, Smith KL, Bernard MA. Effects of a community-based intervention to increase activity in American Indian elders. The Journal of the Oklahoma State Medical Association. 2001;94:455–460. [PubMed] [Google Scholar]
- 65.Kumanyika SK, Shults J, Fassbender J, et al. Outpatient weight management in African-Americans: the Healthy Eating and Lifestyle Program (HELP) study. Preventive Medicine. 2005;41:488–502. doi: 10.1016/j.ypmed.2004.09.049. [DOI] [PubMed] [Google Scholar]
- 66.Kumanyika SK, Wadden TA, Shults J, et al. Trial of family and friend support for weight loss in African American adults. Archives of Internal Medicine. 2009;169:1795–1804. doi: 10.1001/archinternmed.2009.337. [DOI] [PubMed] [Google Scholar]
- 67.Lee RE, McGinnis KA, Sallis JF, et al. Active vs. passive methods of recruiting ethnic minority women to a health promotion program. Annals of Behavioral Medicine. 1997;19:378–384. doi: 10.1007/BF02895157. [DOI] [PubMed] [Google Scholar]
- 68.Martin PD, Rhode PC, Dutton GR, et al. A primary care weight management intervention for low-income African American women. Obesity. 2006;14:1412–1420. doi: 10.1038/oby.2006.160. [DOI] [PubMed] [Google Scholar]
- 69.McNabb W, Quinn M, Kerver J, Cook S, Karrison T. The PATHWAYS church-based weight loss program for urban African-American women at risk for diabetes. Diabetes Care. 1997;20:1518–1523. doi: 10.2337/diacare.20.10.1518. [DOI] [PubMed] [Google Scholar]
- 70.Murrock CJ. PhD. Case Western Reserve University; Cleveland, OH: 2007. Dance and Physical Activity in African American Women. [Google Scholar]
- 71.Newton RL, Jr, Perri MG. A randomized pilot trial of exercise promotion in sedentary African-American adults. Ethnicity & Disease. 2004;14:548–557. [PubMed] [Google Scholar]
- 72.Nichols GJ. PhD. University of Maryland; College Park, MD: 1995. Testing a Culturally Consistent Behavioral Outcomes Strategy for Cardiovascular Disease Risk Reduction and Prevention in Low Income African American Women. [Google Scholar]
- 73.Nicklas BJ, Dennis KE, Berman DM, et al. Lifestyle intervention of hypocaloric dieting and walking reduces abdominal obesity and improves coronary heart disease risk factors in obese, postmenopausal, African-American and Caucasian women. Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58:181–189. doi: 10.1093/gerona/58.2.m181. [DOI] [PubMed] [Google Scholar]
- 74.Nies MA, Artinian NT, Schim SM, Wal JS, Sherrick-Escamilla S. Effects of lay health educator interventions on activity, diet, and health risks in an urban Mexican American community. Journal of Primary Prevention. 2004;25:441–455. doi: 10.1023/b:jopp.0000048111.94285.27. [DOI] [Google Scholar]
- 75.Parikh P, Simon EP, Fei K, et al. Results of a pilot diabetes prevention intervention in East Harlem, New York City: Project HEED. American Journal of Public Health. 2010;100(Suppl 1):S232–239. doi: 10.2105/ajph.2009.170910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Plescia M, Herrick H, Chavis L. Improving health behaviors in an African American community: the Charlotte Racial and Ethnic Approaches to Community Health project. American Journal of Public Health. 2008;98:1678–1684. doi: 10.2105/ajph.2007.125062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Poston WS, 2nd, Haddock CK, Olvera NE, et al. Evaluation of a culturally appropriate intervention to increase physical activity. American Journal of Health Behavior. 2001;25:396–406. doi: 10.5993/ajhb.25.4.5. [DOI] [PubMed] [Google Scholar]
- 78.Quinn MT, McNabb WL. Training lay health educators to conduct a church-based weight-loss program for African American women... including commentary by Kaplan S. Diabetes Educator. 2001;27:231–238. doi: 10.1177/014572170102700209. [DOI] [PubMed] [Google Scholar]
- 79.Racette SB, Weiss EP, Obert KA, Kohrt WM, Holloszy JO. Modest lifestyle intervention and glucose tolerance in obese African Americans. Obesity Research. 2001;9:348–355. doi: 10.1038/oby.2001.45. [DOI] [PubMed] [Google Scholar]
- 80.Resnick B, Luisi D, Vogel A. Testing the Senior Exercise Self-Efficacy Project (SESEP) for use with urban dwelling minority older adults. Public Health Nursing. 2008;25:221–234. doi: 10.1111/j.1525-1446.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 81.Resnick B, Shaughnessy M, Galik E, et al. Pilot testing of the PRAISEDD intervention among African American and low-income older adults. Journal of Cardiovascular Nursing. 2009;24:352–361. doi: 10.1097/jcn.0b013e3181ac0301. [DOI] [PubMed] [Google Scholar]
- 82.Romero Z. MS. University of Texas-Pan American; Edinburg, TX: 2004. Use of Pedometers to Promote Improvement in Selected Physiological Measurements in an Older Female Mexican American Population. [Google Scholar]
- 83.Speck BJ, Hines-Martin V, Stetson BA, Looney SW. An environmental intervention aimed at increasing physical activity levels in low-income women. Journal of Cardiovascular Nursing. 2007;22:263–271. doi: 10.1097/01.jcn.0000278957.98124.8a. [DOI] [PubMed] [Google Scholar]
- 84.Staten L, Gregory-Mercado K, Ranger-Moore J, et al. Provider counseling, health education, and community health workers: the Arizona WISEWOMAN project. Journal of Women’s Health. 2004;13:547–556. doi: 10.1089/1540999041281133. [DOI] [PubMed] [Google Scholar]
- 85.Staten LK, Scheu LL, Bronson D, Pena V, Elenes J. Pasos Adelante: the effectiveness of a community-based chronic disease prevention program. Preventing Chronic Disease. 2005;2:A18. [PMC free article] [PubMed] [Google Scholar]
- 86.Stewart AL, Gillis D, Grossman M, et al. Diffusing a research-based physical activity promotion program for seniors into diverse communities: CHAMPS III. Preventing Chronic Disease. 2006;3:A51. [PMC free article] [PubMed] [Google Scholar]
- 87.The Wisewoman Group. Cardiovascular disease prevention for women attending breast and cervical cancer screening programs: the WISEWOMAN projects. Preventive Medicine. 1999;28:496–502. doi: 10.1006/pmed.1999.0462. [DOI] [PubMed] [Google Scholar]
- 88.Walcott-McQuigg JA, Chen S-P, Davis K, et al. Weight loss and weight loss maintenance in African-American women. Journal of the National Medical Association. 2002;94:686–694. [PMC free article] [PubMed] [Google Scholar]
- 89.Wilbur J, McDevitt JH, Wang E, et al. Outcomes of a home-based walking program for African-American women. American Journal of Health Promotion. 2008;22:307–317. doi: 10.4278/ajhp.22.5.307. [DOI] [PubMed] [Google Scholar]
- 90.Dutton GR. PhD. Louisiana State University; Baton Rogue, LA: 2005. Effects of a Primary Care Weight Management Intervention on Physical Activity in Low-Income African American Women. [Google Scholar]
- 91.Mulvihill MM, Hovell MF, Schade DH, et al. Effects of a culturally tailored diabetes prevention intervention for low SES Latino women on fitness, exercise, BMI, nutrition/exercise knowledge and dietary fat avoidance. Diabetes. 1999;48:A303. [Google Scholar]
- 92.Bouchard C, Leon AS, Rao DC, et al. The HERITAGE family study. Aims, design, and measurement protocol. Medicine & Science in Sports & Exercise. 1995;27:721–729. [PubMed] [Google Scholar]
- 93.Paniagua CT, Taylor RE. The cultural lens of genomics. OJIN: The Online Journal of Issues in Nursing. 2008;13 doi: 10.3912/OJIN.Vol13No01Man05. [DOI] [Google Scholar]
- 94.Conn VS. Unpacking the black box: countering the problem of inadequate intervention descriptions in research reports. Western Journal of Nursing Research. 2012;34:427–433. doi: 10.1177/0193945911434627. [DOI] [PubMed] [Google Scholar]
- 95.Crowder SJ, Broome ME. A framework to evaluate the cultural appropriateness of intervention research. Western Journal of Nursing Research. 2012;34:1002–1022. doi: 10.1177/0193945912451656. [DOI] [PubMed] [Google Scholar]
- 96.Rodriquez M, Bernal G. Frameworks, models, and guidelines for cultural adaptations. In: Bernal G, Rodriquez M, editors. Cultural Adaptations: Tools for Evidence-Based Practice with Diverse Populations. American Psychological Association; Washington DC: 2012. pp. 23–44. [Google Scholar]
- 97.Conn VS, Cooper PS, Ruppar TM, Russell CL. Searching for the intervention in intervention research reports. Journal of Nursing Scholarship. 2008;40:52–59. doi: 10.1111/j.1547-5069.2007.00206.x. [DOI] [PubMed] [Google Scholar]
- 98.Glasziou P, Chalmers I, Altman DG, et al. Taking healthcare interventions from trial to practice. BMJ. 2010;341:c3852. doi: 10.1136/bmj.c3852. [DOI] [PubMed] [Google Scholar]
- 99.Glasziou P, Meats E, Heneghan C, Shepperd S. What is missing from descriptions of treatment in trials and reviews? BMJ. 2008;336:1472–1474. doi: 10.1136/bmj.39590.732037.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: issues for the cultural adaptation and development of psychosocial treatments with Hispanics. Journal of Abnormal Child Psychology. 1995;23:67–82. doi: 10.1007/bf01447045. [DOI] [PubMed] [Google Scholar]
- 101.Bernal G, Domenech Rodriguez MM. Cultural adaptation in context: psychotherapy as a historical account of adaptations. In: Bernal G, Domenech Rodriguez MM, editors. Cultural Adaptations: Tools for Evidence-Based Practice with Diverse Populations. American Psychological Association; Washington, D.C: 2012. pp. 3–22. [Google Scholar]
- 102.Benish SG, Quintana S, Wampold BE. Culturally adapted psychotherapy and the legitimacy of myth: a direct-comparison meta-analysis. Journal of Counseling Psychology. 2011;58:279–289. doi: 10.1037/a0023626. [DOI] [PubMed] [Google Scholar]
- 103.Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Education and Behavior. 2003;30:133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 104.Griner D, Smith TB. Culturally adapted mental health intervention: a meta-analytic review. Psychotherapy. 2006;43:531–548. doi: 10.1037/0033-3204.43.4.531. [DOI] [PubMed] [Google Scholar]
- 105.Huey SJ, Jr, Polo AJ. Evidence-based psychosocial treatments for ethnic minority youth. Journal of Clinical Child and Adolescent Psychology. 2008;37:262–301. doi: 10.1080/15374410701820174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Smith TB, Rodriguez MD, Bernal G. Culture. Journal of Clinical Psychology. 2011;67:166–175. doi: 10.1002/jclp.20757. [DOI] [PubMed] [Google Scholar]
- 107.Miranda J, Bernal G, Lau A, et al. State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology. 2005;1:113–142. doi: 10.1146/annurev.clinpsy.1.102803.143822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rimal RN, Adkins AD. Using computers to narrowcast health messages: the role of audience segmentation, targeting and tailoring in health promotion. In: Thompson TL, Dorsey A, Miller KI, Parrott R, editors. Handbook of Health Communication. Routledge; New York, NY: 2003. pp. 498–499. [Google Scholar]
- 109.United States Cenus Bureau. An older and more diverse nation by midcentury. 2008 Aug 14; Retrieved from http://www.census.gov/newsroom/releases/archives/population/cb08-123.html.