Abstract
Objective:
Three-year changes in well-being were studied among family caregivers of an epidemiologically derived sample of stroke survivors from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study and compared to matched noncaregivers.
Methods:
Family caregivers of REGARDS participants who experienced a stroke event completed telephone interviews assessing depressive symptoms, mental and physical health quality of life (QOL), life satisfaction, and leisure satisfaction at approximately 9, 18, 27, and 36 months after the stroke (n = 235). For each stroke caregiver, a family member of a stroke-free REGARDS participant was enrolled as a matched noncaregiving control (n = 235) and completed similar interviews.
Results:
Multilevel longitudinal models found that caregivers showed poorer well-being at 9 months poststroke than controls on all measures except physical health QOL. Significant differences were sustained for 22 months after the stroke event for depressive symptoms, 31 months for mental health QOL, and 15 months for life satisfaction. For leisure satisfaction, differences were still significant at 36 months poststroke. Caregiving effects were similar across race and sex.
Conclusions:
Stroke caregiving is associated with persistent psychological distress, but life satisfaction, depression, and mental health QOL became comparable to noncaregivers by 3 years after stroke. Caregiver leisure satisfaction was chronically lower than in noncaregivers. Intervention for stroke caregivers should recognize both the strains faced by caregivers and their capacity for successful coping over time.
Most studies of family caregivers of stroke survivors report that caregivers experience negative effects on their well-being.1,2 Most of this research has been cross-sectional and conducted within 1 year of the stroke3 and uses convenience samples. Population-based samples allow for a better estimation of the public health effects of stroke caregiving. Including a demographically matched comparison group controls for differences in health and well-being due to factors such as age, sex, and race.4
The purpose of this study was to examine long-term differences in well-being between a population-based sample of family caregivers of stroke survivors and demographically matched noncaregiving controls. The analyses focused on the following questions: (1) Do stroke caregivers and matched noncaregivers differ in well-being, and what is the magnitude of such effects? (2) How do differences in well-being between caregivers and noncaregivers change over time? (3) Do caregiving, race, and sex affect the trajectories of well-being changes?
METHODS
Participants.
The Reasons for Geographic and Racial Differences in Stroke (REGARDS) study is a national, epidemiologic investigation of stroke incidence and mortality that enrolled 30,239 participants 45 years of age or older from 2003 to 2007.5,6 Large samples of both African American and white men and women were recruited. Follow-up surveillance interviews are conducted every 6 months by telephone and include queries about possible stroke events. Medical records are then examined by adjudicators to confirm incident stroke events. Once stroke survivors are identified by REGARDS they are recruited, along with a primary family caregiver, to participate in the ancillary Caring for Adults Recovering from the Effects of Stroke (CARES) project.7–10
The present analyses are based on 235 family caregivers of REGARDS stroke survivors and a matched control sample of 235 noncaregivers who were also recruited through the REGARDS project. After the CARES project was initiated in 2005, REGARDS participants who reported a stroke event were potentially eligible to participate. Stroke survivors were eligible if they were community-dwelling 9 months after the stroke event and had a family member or close friend who was willing to participate in the project and who had served as an informal caregiver after the stroke event. Only individuals who identified themselves as black or white were enrolled into REGARDS because of their specific interest in that racial comparison.
The matched noncaregiving control sample was recruited by asking each REGARDS participant at their REGARDS baseline interview who would most likely be their caregiver if they needed one in the future. Second, after we enrolled a stroke survivor and family caregiver from REGARDS, we identified a list of REGARDS participants similar to each stroke survivor in CARES on age, sex, race, and relationship with their potential caregiver. That is, if the index stroke survivor was being cared for by a spouse, we identified a stroke-free control from REGARDS who reported that he or she would be cared for by his or her spouse. Third, we randomly selected potential controls from the list of eligible matches and attempted to contact them until we successfully enrolled a matched control case. We contacted the stroke-free control's family member, and after confirming that this person was not already a caregiver for any disabled family member, we enrolled him or her as the matched noncaregiving control to that particular stroke caregiver. Thus, the noncaregiving controls were matched to the stroke caregivers on sex, race, age (±5 years), coresidence, and relationship status, but were not caregivers themselves. Each participant received $20 per interview for participation.
Standard protocol approvals, registrations, and patient consents.
All REGARDS participants provided consent to participate and contact their family members. Caregivers and noncaregiving controls also provided consent. All procedures were reviewed and approved by the Institutional Review Board of the University of Alabama at Birmingham.
Procedures.
An initial baseline CARES interview was conducted by telephone for the caregivers approximately 9 months after the stroke event. After explaining the study and screening for eligibility, trained research interviewers obtained data on demographic information, physical health, and psychosocial functioning. Similar interviews were completed through 2013 at 18, 27, and 36 months poststroke. Noncaregiving controls were given a baseline interview, then 3 corresponding follow-up interviews every 9 months thereafter. The medical records for the suspected stroke events were examined by at least 2 trained adjudicators to verify the date of the stroke and determine key descriptive data on the stroke. In terms of site, 54% were left hemisphere, 41% right hemisphere, and 5% bilateral. For type of stroke, 92% were ischemic and 8% were hemorrhages. Most stroke survivors (86%) were hospitalized after their stroke events, and the average length of those hospitalizations was 8.54 days (SD = 12.8).
The participants analyzed in this article are the family caregivers of the stroke survivors in comparison to the matched noncaregiving controls.
Demographic variables.
Age was the number of days between the participant's stated date of birth and the date of the baseline interview. Education in years was based on self-report. Sex and race (African American vs white) and married/unmarried status were dichotomous variables based on self-report. Region was analyzed based on the categories used in the stratified sampling design (Stroke Belt, Stroke Buckle, nonbelt). Annual income was coded as a categorical variable as indicated in table 1.
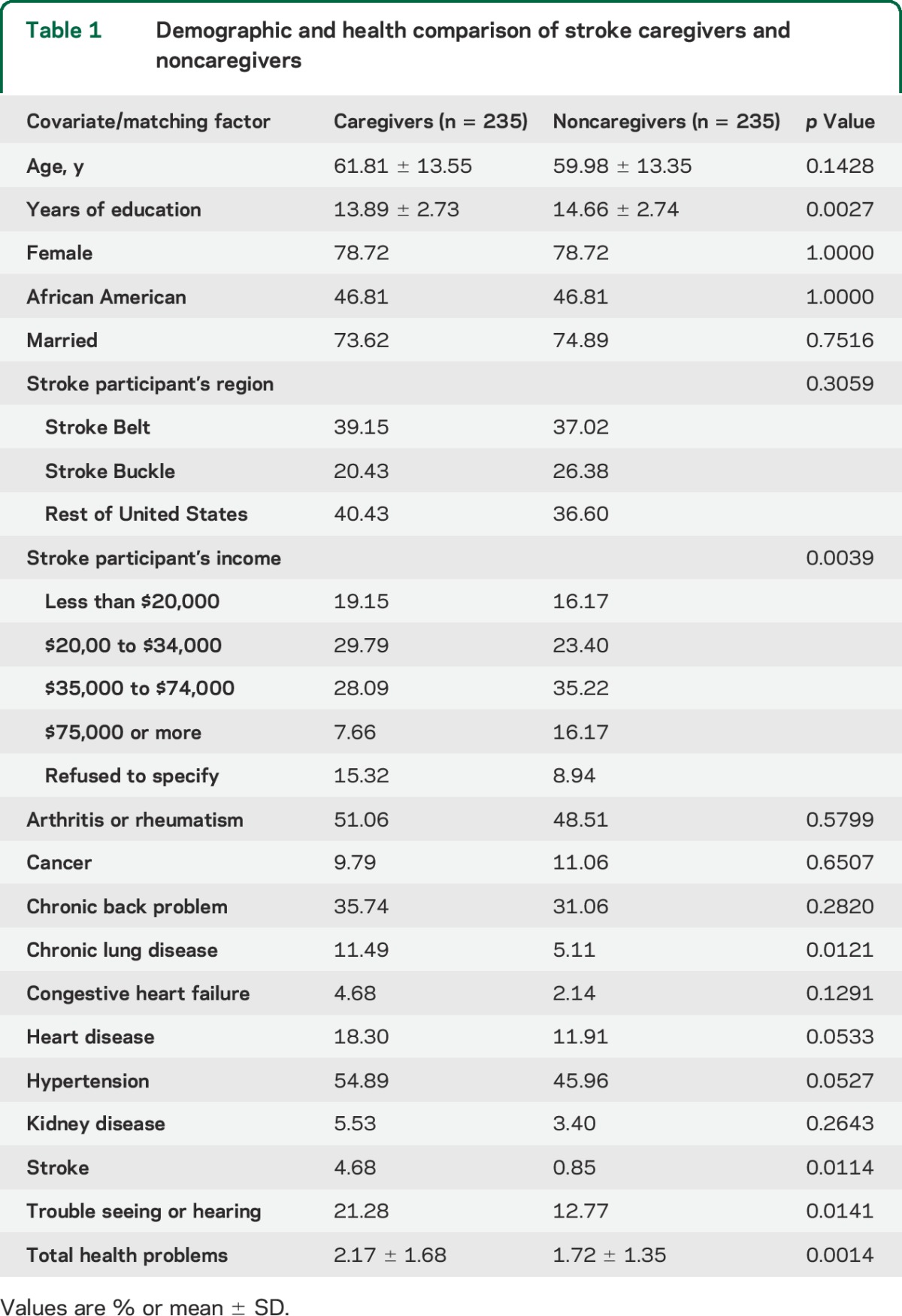
Table 1.
Demographic and health comparison of stroke caregivers and noncaregivers
Health and disease history.
Participants were asked in the CARES interviews if they had ever been told by a doctor or health professional that they had arthritis or rheumatism, cancer, chronic back problems, chronic lung disease, congestive heart failure, heart disease, hypertension, kidney disease, stroke, and trouble with hearing. Total number of health problems was the sum of these conditions.
Well-being.
Depressive symptoms were measured with the 20-item Center for Epidemiologic Studies–Depression scale (CES-D).11 Frequency of each symptom was rated on a 0 (rarely) to 3 (most of the time) scale. Higher scores indicate greater depression.
The 12-item Short Form Health Survey assessed health-related quality of life (QOL) measured by the Physical Component Summary (PCS) and Mental Component Summary (MCS) scores. These measures have been standardized to have a mean of 50 and a SD of 10 in the adult US population,12 with higher scores representing better health.
Life satisfaction was assessed using the Life Satisfaction Index–Z,13 (LSI-Z) which obtains levels of agreement with 13 general statements about life. Items were summed, with higher scores indicating greater life satisfaction.
The Leisure Time Satisfaction scale (LTS) measures satisfaction with time spent doing leisure activities.14 Six items targeted activities such as hobbies, quiet time, and church attendance. Participants were asked “over the past month, how satisfied are you with the amount of time you have been able to spend….” Three-point rating scales (0 = not at all, 1 = a little, 2 = a lot) are used, with higher scores indicating higher LTS.
Cronbach α was greater than 0.77 for all of the well-being measures used in the study.
Statistical analyses.
Caregivers and noncaregivers were compared on demographic and health data collected at the 9-month assessment. Multilevel longitudinal models were then used to estimate linear trajectories over time and to test for statistically significant differences (p < 0.05) between caregivers and noncaregivers on CES-D, LSI-Z, MCS, PCS, and LTS.
We identified 602 possible stroke participants through REGARDS. We contacted 469, with the remaining individuals unreachable (116), not contacted because chart data were insufficient to support a stroke diagnosis (6), or the stroke occurred too long before our 9 months assessment window (11). Of the 469 contacted, 73 refused, and 161 were ineligible, leaving 235 stroke survivor–caregiver dyads. We identified multiple potential noncaregiving controls for each stroke participant. Of 3,474 potential noncaregiver controls, 688 were contacted. Of these, 379 refused or did not answer subsequent return calls, and 74 were ineligible, leaving 235 noncaregiving controls.
A total of 652 caregiver and 756 control interviews were completed and included in the analyses. Of the 470 participants, 231 (49.15%) completed all 4 longitudinal assessments, and 389 (82.77%) completed at least 2 of the 4 possible interviews. The longitudinal models included all available data. There was no imputation of missing data, although models did include partial data from participants who did not complete all 4 telephone interviews.15
Dates of each longitudinal interview and, for the stroke caregivers, the date of stroke, were used to calculate indicators of time for the longitudinal models. Differences between dates were calculated in days and converted to months. For caregivers, the initial interview was approximately 9 months after the stroke date by design, but the precise timing of this interview was determined and used in the analyses. For noncaregivers, a value of 9.0 months was assumed for the first CARES interview, and differences between interview dates were then used to measure the precise timing of the follow-up interviews. This months-since-stroke variable was then centered at 9 months by subtracting 9.0. The stroke case variable was coded as caregiver = 0 and noncaregiving control as −1. The analytic models, therefore, included (1) a main effect for stroke case that constituted a direct caregiver vs control contrast at 9 months after stroke, (2) a main effect for time that tested whether the linear increase or decrease across time in the caregiving group was significantly different from zero, and (3) a stroke case by time interaction, which tested whether the linear rate of change over time differed between caregivers and controls. In more expansive models, we included interaction effects for race by time, sex by time, and 3-way interactions including stroke case (e.g., stroke case by race by time), to assess whether there were differences in rates of change over time by sex or race. Person-specific changes over time were estimated at the within-person level and then modeled as effects of between-subject predictors at a second, higher-order level.15
Restricted maximum likelihood estimates of model parameters were obtained using SAS PROC MIXED.16 Race, sex, age, education, and number of health problems measured at the 9-month interview were included as time-invariant covariates. We did not include a time-variant covariate for caregiver health because the measure of health conditions was based on diagnosed conditions at baseline and our goal was to evaluate subsequent changes in well-being. For outcome measures that differed significantly between caregivers and noncaregivers, covariate-adjusted means were calculated at each time point in the longitudinal trajectory. Standardized effect sizes were obtained by obtaining the difference in covariate-adjusted means between caregivers and noncaregivers and dividing this difference by the overall SD from the initial interview.17 We also compared the adjusted means at each month and reported the first month that these differences were no longer statistically significant.
RESULTS
Demographic characteristics of caregivers and controls.
Demographic variables in table 1 confirm that caregivers and noncaregivers did not differ significantly on the variables that were used for matching. Caregivers and noncaregivers also did not differ significantly on marital status and region. Caregivers had significantly lower educational attainment and income than noncaregivers, and were more likely to report a history of chronic lung disease, stroke, trouble seeing or hearing, and more total health problems.
Well-being measures over time for caregivers and controls.
Results from the longitudinal models are shown in table 2, and some are illustrated in the figures. For depressive symptoms, there were significant effects for caregiver/noncaregiver, time, sex, age, education, and health. Being a caregiver, being a woman, having lower age and education, and having more health problems were associated with significantly higher depressive symptoms at 9 months after stroke. A significant time by caregiver/noncaregiver interaction effect was also found, illustrated in figure 1. Caregivers have significantly higher depression scores at 9 months than noncaregivers, but this difference diminished over time because depressive symptoms significantly decreased over time for the caregivers, The magnitude of the difference in depressive symptoms at the 9-month assessment was 0.28 standard deviation units (SDUs) and decreased to 0.01 SDUs at 36 months. The difference between caregivers and noncaregivers was significant until 22 months after the stroke.
Table 2.
Multilevel models of well-being over time
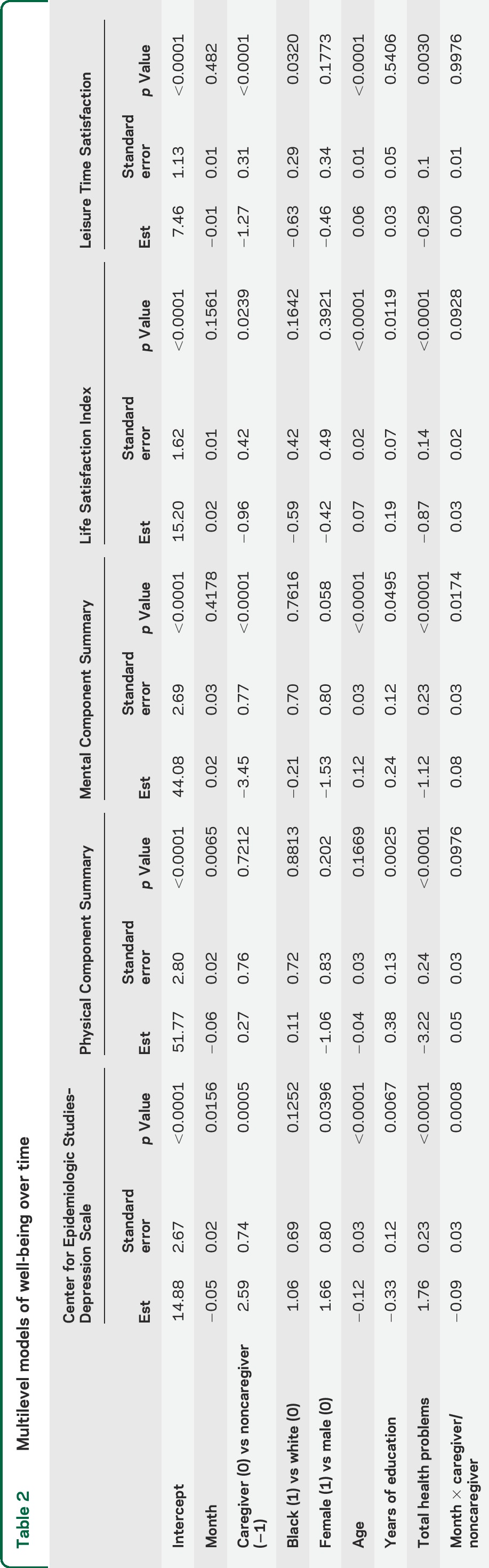
Figure 1. Model-based covariate-adjusted linear trajectories for Center for Epidemiologic Studies–Depression scale (CESD).
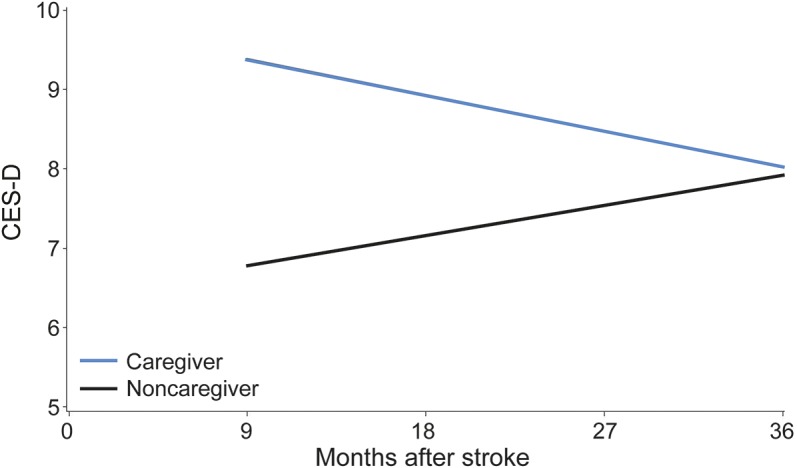
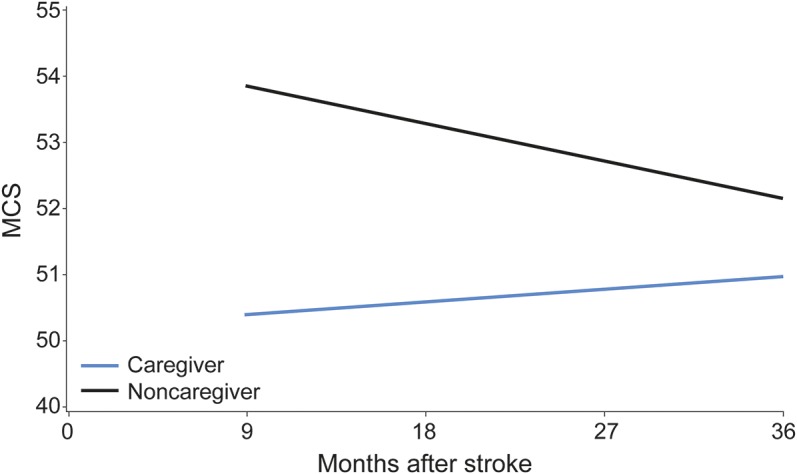
For mental health QOL, there were significant effects for caregiver/noncaregiver, age, education, and health. Being a noncaregiver, having higher age and education, and having fewer health problems were associated with higher mental health QOL at 9 months after stroke. Although scores were stable over time for the caregivers, there was a significant time by caregiver/noncaregiver interaction effect that is shown graphically in figure 2. Caregivers had lower mental health QOL than noncaregivers at 9 months, but this difference diminished over time. The magnitude of difference in mental health QOL at the 9-month assessment was 0.38 SDUs, but decreased to 0.13 SDUs at 36 months and was statistically significant until 31 months after the stroke.
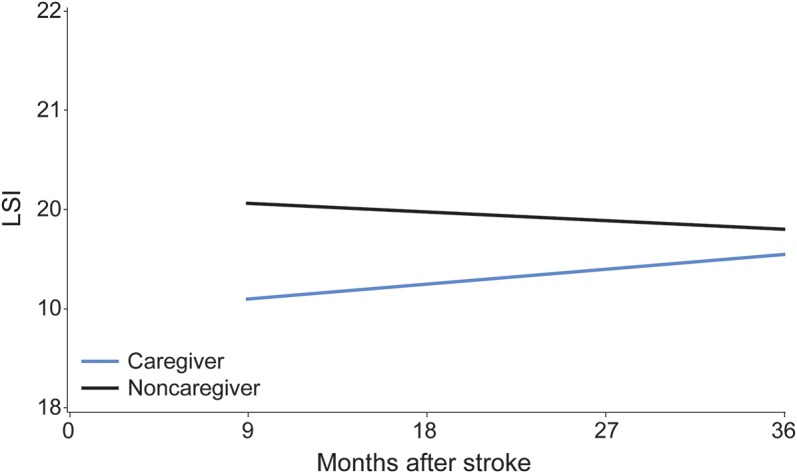
Figure 2. Model-based covariate-adjusted linear trajectories for Life Satisfaction Index–Z (LSI).
For physical health QOL, there were significant effects for education and health. Higher education and fewer health problems were associated with higher physical health QOL. There were no significant effects for time, caregiving, or time by caregiver interaction.
For life satisfaction, there were significant effects for caregiver/noncaregiver, age, education, and health. Being a noncaregiver, having higher age and education, and having fewer health problems were associated with higher life satisfaction. There were no time or caregiving by time interaction effects for life satisfaction. Life satisfaction over time is illustrated in figure 3. Caregivers had lower life satisfaction by 0.19 SDUs at the 9-month poststroke assessment, and a significant difference persisted up until 15 months after the stroke.
Figure 3. Model-based covariate-adjusted linear trajectories for 12-item Short Form Health Survey Mental Component Scores (MCS).
For leisure time satisfaction, there were significant effects for caregiver/noncaregiver, age, race, and health. Being a noncaregiver, being older, being white, and having fewer health problems were associated with higher leisure time satisfaction. There was no effect for time and no time by caregiver/noncaregiver interaction. The lower leisure satisfaction level for caregivers was persistent at 0.37 SDUs for both 9-month and 36-month assessments.
DISCUSSION
This population-based study confirms and extends previous research1,2 that stroke has a significant initial negative impact on caregiver well-being. Depressive symptoms, life satisfaction, mental health QOL, and leisure time satisfaction were all worse in caregivers at 9 months poststroke than in demographically similar noncaregiving controls. At 9 months after stroke, the caregiver decrease in well-being ranged between 0.19 and 0.38 SDUs. These results are in the low-to-medium effect size range and strongly support the need for services to enhance caregiver well-being, especially during the first year after a stroke.
We did not find significant differences between caregivers and noncaregivers in physical health QOL. Research has rarely evaluated the impact of stroke on caregiver physical health compared with noncaregivers, but broader research on caregiving has suggested that caregiving can be harmful to caregivers' health.18,19 However, recent research has challenged the magnitude of caregiving-related negative health effects20 and whether caregiving is associated with increased mortality risk.21
Stroke caregivers reported lower education and income, and were more likely to report having lung disease, stroke, sensory limitations, and more total health problems than noncaregiving controls. We adjusted for these initial differences but the finding suggests that caregivers may have poorer health than the general population when initiating some kinds of caregiving. Family members of stroke survivors are likely to share risk factors for stroke and other chronic illnesses due to common genes, shared environments, and assortative marriage.22–24 This highlights the importance of using appropriate noncaregiving controls in such research.
When compared with demographically matched noncaregiving controls, stroke caregivers report well-being comparable to noncaregivers within 36 months after stroke. Although stroke caregivers show considerable distress at 9 months after stroke, over time their distress diminishes. Stress and coping theory25,26 suggests that improvements in caregiver well-being could be due to reduction of stressors (e.g., stroke survivor recovery) or improvements in caregiver appraisals and adaptive coping skills with experience.2 These findings contrast with research on Alzheimer caregiving, in which poorer well-being in caregivers compared with noncaregivers remained significant and undiminished over a 2-year follow-up period.27
Leisure time satisfaction remained worse in caregivers than noncaregivers 3 years poststroke. Caregiving may create long-term problems with caregivers' ability to participate in valued activities and interests, and lack of social engagement is a risk factor for worse psychological well-being.1,28 This lack of recovery in leisure activities even with reduced caregiver distress suggests that stroke may lead to sustained changes in lifestyle for caregivers.
Race and sex were not significant predictors of the impact of stroke on caregiver well-being or on the longitudinal trajectories after stroke. In previously published analyses with subsets of the current participants, we found that African American stroke survivors had more impairments than white stroke survivors,7,10 consistent with other research.29 However, after adjustment for these differences, African American caregivers had better mental health scores than white caregivers,7 suggesting some heightened resilience to caregiving stress in African American caregivers, which has been noted in previous research.26,30,31
Our project has a number of strengths, including use of a population-based sample of stroke survivors and caregivers, and inclusion of noncaregiving controls matched or covariance adjusted with stroke caregivers on demographic and health variables. The use of a population-based sample enhances the generalizability of the results, although the lack of participants other than whites and African Americans limits generalizability to other racial/ethnic groups. A limitation is that individuals categorized as caregivers were primary caregivers for the stroke survivor after the stroke, but may not have maintained caregiving roles over the duration of the follow-up. While our study began assessing caregivers at 9 months poststroke, there may be higher distress levels in caregivers at previous time points after stroke and this deserves further study.3
Future reports from our group will address individual differences in caregiver well-being over time using a stress process model of caregiving that evaluates changes in stressors, appraisals, social support, and other coping resources.1,28,31,32 In addition, this future work will examine whether race and sex affect individual differences in caregiver stress and coping over time.
Stroke caregivers can experience considerable negative effects on their well-being within the first few years after stroke. Many of these negative effects improve over time, although leisure time satisfaction appears to show a long-lasting pattern of disruption. Efforts to intervene with stroke caregivers should pay attention both to the likely negative effects of caregiving on well-being and the potential for resilience and recovery.
Supplementary Material
ACKNOWLEDGMENT
The authors thank the other investigators, the staff, and the participants of the REGARDS study for their contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
GLOSSARY
- CARES
Caring for Adults Recovering from the Effects of Stroke
- CES-D
Center for Epidemiologic Studies–Depression scale
- LSI-Z
Life Satisfaction Index–Z
- LTS
Leisure Time Satisfaction
- MCS
Mental Component Summary
- PCS
Physical Component Summary
- QOL
quality of life
- REGARDS
Reasons for Geographic and Racial Differences in Stroke
- SDU
standard deviation unit
Footnotes
Editorial, page 1292
AUTHOR CONTRIBUTIONS
William E. Haley: drafting/revising the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data; obtaining funding. David L. Roth: drafting/revising the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data; acquisition of data; statistical analysis; study supervision or coordination; obtaining funding. Martha Hovater: drafting/revising the manuscript for content, including medical writing for content; analysis or interpretation of data; statistical analysis. Olivio J. Clay: drafting/revising the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data; obtaining funding.
STUDY FUNDING
This research project is supported by cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, NIH, Department of Health and Human Services. Additional funding was provided by investigator-initiated grants (R01 NS045789 and R01 NS075047, David L. Roth, PhD, PI) from the National Institute of Neurological Disorders and Stroke, NIH, Department of Health and Human Services.
DISCLOSURE
W. Haley receives funding from National Institute of Neurological Disorders and Stroke R01 NS045789 and R01 NS075047. D. Roth receives funding from National Institute of Neurological Disorders and Stroke R01 NS045789 and R01 NS075047. M. Hovater receives funding from National Institute of Neurological Disorders and Stroke R01 NS045789 and R01 NS075047. O. Clay reports no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Cameron JI, Cheung AM, Streiner DL, Coyte PC, Stewart DE. Stroke survivor depressive symptoms are associated with family caregiver depression during the first 2 years poststroke. Stroke 2011;42:302–306. [DOI] [PubMed] [Google Scholar]
- 2.Visser-Meily A, Post M, van de Port I, Maas C, Forstberg-Warleby G, Lindeman E. Psychosocial functioning of spouses of patients with stroke from initial inpatient rehabilitation to 3 years poststroke: course and relations with coping strategies. Stroke 2009;40:1399–1404. [DOI] [PubMed] [Google Scholar]
- 3.Gaugler JE. The longitudinal ramifications of stroke caregiving: a systematic review. Rehabil Psychol 2010;55:108–125. [DOI] [PubMed] [Google Scholar]
- 4.Haley WE, Roth DL, Perkins MM, Kissela B, Howard G. Quality of life after stroke: a prospective longitudinal study. Qual Life Res 2011;20:799–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Howard VJ, Cushman M, Pulley L, et al. The REasons for Geographic and Racial Differences in Stroke study: Objectives and design. Neuroepidemiology 2005;25:135–143. [DOI] [PubMed] [Google Scholar]
- 6.Howard G, Safford MM, Meschia JF, et al. Stroke symptoms in individuals reporting no stroke or transient ischemic attack are associated with a decrease in indices of mental and physical functioning. Stroke 2007;38:2446–2452. [DOI] [PubMed] [Google Scholar]
- 7.Clay OJ, Grant JS, Wadley VG, Perkins MM, Haley WE, Roth DL. Correlates of health-related quality of life in African American and Caucasian stroke caregivers. Rehabil Psychol 2013;58:28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grant JS, Keltner NL, Clay OJ, et al. Does caregiver well-being predict stroke survivor depressive symptoms? A mediation analysis. Top Stroke Rehabil 2013;20:44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haley WE, Allen JY, Grant JS, Clay OJ, Perkins MM, Roth DL. Problems and benefits reported by stroke family caregivers: results from a prospective epidemiological study. Stroke 2009;40:2129–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roth DL, Haley WE, Clay OJ, et al. Race and gender differences in stroke outcomes one year following first-time stroke events. Stroke 2011;42:626–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401. [Google Scholar]
- 12.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–233. [DOI] [PubMed] [Google Scholar]
- 13.Wood V, Wylie ML, Sheafor B. An analysis of a short self-report measure of life satisfaction: Correlation with rater judgments. J Gerontol 1969;24:465–469. [DOI] [PubMed] [Google Scholar]
- 14.Stevens AB, Arguelles S, Belle S, et al. Measurement of leisure time satisfaction in family caregivers. Aging Ment Health 2004;8:450–459. [DOI] [PubMed] [Google Scholar]
- 15.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- 16.Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS for Mixed Models, 2nd ed Cary, NC: SAS Institute; 2006. [Google Scholar]
- 17.Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol Methods 2009;14:43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA 1999;282:2215–2219. [DOI] [PubMed] [Google Scholar]
- 19.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging 2003;18:250–267. [DOI] [PubMed] [Google Scholar]
- 20.Roth DL, Perkins M, Wadley VG, Temple E, Haley WE. Family caregiving and emotional strain: associations with psychological health in a national sample of community-dwelling middle-aged and older adults. Qual Life Res 2009;18:679–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roth DL, Haley WE, Hovater M, Perkins M, Wadley VG, Judd S. Family caregiving and all-cause mortality: findings from a population-based propensity-matched analysis. Am J Epidemiol 2013;178:1571–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liao D, Myers R, Hunt S, et al. Familial history of stroke and stroke risk: the family heart study. Stroke 1997;28:1908–1912. [DOI] [PubMed] [Google Scholar]
- 23.Williams RR, Hunt SC, Heiss G, et al. Usefulness of cardiovascular family history data for population-based preventive medicine and medical research (The Health Family Tree Study and the NHLBI Family Heart Study). Am J Cardiol 2001;87:129–135. [DOI] [PubMed] [Google Scholar]
- 24.Sackett DL, Anderson GD, Milner R, Feinleib M, Kannell WB. Concordance for coronary risk factors among spouses. Circulation 1975;52:589–595. [DOI] [PubMed] [Google Scholar]
- 25.Haley WE, Levine EG, Brown SL, Bartolucci AA. Stress, appraisal, coping, and social support as predictors of adaptational outcome among dementia caregivers. Psychol Aging 1987;2:323–330. [DOI] [PubMed] [Google Scholar]
- 26.Haley WE, Roth DL, Coleton MI, et al. Appraisal, coping, and social support as mediators of well-being in black and white family caregivers of patients with Alzheimer's disease. J Consult Clin Psychol 1996;64:121–129. [DOI] [PubMed] [Google Scholar]
- 27.Roth DL, Haley WE, Owen JE, Clay OJ, Goode KT. Latent growth models of the longitudinal effects of dementia caregiving: a comparison of African-American and white family caregivers. Psychol Aging 2001;16:427–436. [PubMed] [Google Scholar]
- 28.Cameron JI, Stewart DE, Streiner DL, Coyote PC, Cheung AM. What makes family caregivers happy during the first 2 years post stroke? Stroke 2014;45:1084–1089. [DOI] [PubMed] [Google Scholar]
- 29.Kissela B, Schneider A, Kleindorfer D, et al. Stroke in a biracial population: the excess burden of stroke among blacks. Stroke 2004;35:426–431. [DOI] [PubMed] [Google Scholar]
- 30.Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: a 20-year review (1980–2000). Gerontologist 2002;42:237–272. [DOI] [PubMed] [Google Scholar]
- 31.Clay OJ, Roth DL, Wadley VG, Haley WE. Changes in social support and their impact on psychosocial adjustment of African American and white dementia caregivers over a five-year period. Int J Geriatr Psychiatry 2008;23:857–862. [DOI] [PubMed] [Google Scholar]
- 32.Goode KT, Haley WE, Roth DL, Ford GR. Predicting longitudinal changes in caregiver physical and mental health: a stress process model. Health Psychol 1998;17:190–198. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


