Abstract
Spouses whose partner has an alcohol use disorder can experience considerable psychological distress. Yet, due to social, financial, relationship, and psychological barriers they often remain hidden, and underserved. To partially reduce treatment barriers for this population, this study evaluated the short-term efficacy of a self-paced, web-delivered coping skills training program for women experiencing distress as a result of living with a partner with an Alcohol Use Disorder. Participants (N = 89) were randomly assigned to either 8-weeks of an Internet-administered Coping Skills Training Program (iCST), or an 8-week Delayed Treatment Control (DTC). Participation in, and satisfaction with iCST was high. At the end of the 8-week access/delay period, iCST participants exhibited a significantly higher level of coping skills relative to DTC, d = 1.02, 95% CI [.64, 1.51], and reported significantly fewer depressive symptoms, d = −.65, 95% CI [−1.21, −.35], and situational anger, d = −.70, 95% CI [−1.62, −.64]. Moreover, iCST appeared to prevent an increase in symptoms among those with low baseline symptom levels; DTC did not. Skill acquisition appeared to partially mediate changes observed. Online coping skills training may be an effective way of reaching and helping a large number of this frequently underserved population.
Keywords: spouses, alcohol use disorders, web-based treatment, coping skills training, women
Approximately 7.7 million adults in the U.S. are currently married to or living with a partner with an Alcohol Use Disorder (AUD; National Institute on Alcohol Abuse and Alcoholism, 2006). The majority of this population has a male partner (73%), is female, and does not have an SUD of its own. As used here, “partner” refers to the person with the SUD; “spouse” refers to the individual married to, or living with the person with the SUD. This spouse population can experience considerable psychological distress, much of which appears directly related to the extent of problems brought on by the partner’s drinking (e.g., Rychtarik & McGillicuddy, 1997). As such, it is at greater risk for medical and mental health conditions, and incurs overall higher healthcare costs than the population without a substance-abusing partner (e.g., Dawson, Grant, Chou, & Stinson, 2007; Ray, Mertens, & Weisner, 2007). Yet, these spouses remain largely hidden and underserved. The large majority has a partner who does not seek treatment (Hasin, Stinson, Ogburn, & Grant, 2007); professional help for their own needs is not widely available, and third party coverage can be limited (Center for Substance Abuse Treatment, 2004). Fear of the partner’s retribution, family turmoil, stigmatization, and financial and time constraints also are often reported, anecdotally, as barriers to spouse help seeking.
The self-help group Al-Anon is widely available for the spouse, but evidence of Al-Anon’s reach, and its efficacy remain limited (Timko, Young, & Moos, 2012). Empirically supported, professionally administered coping skills training interventions have increasingly been found to improve spousal coping, and relieve spousal distress (see O’Farrell & Clements, 2012), yet are not widely available. Moreover, Al-Anon, and professionally based interventions suffer from some of the same service and accessibility barriers noted above.
To partially address access barriers, this study evaluated the short-term efficacy of a web-based coping skills training program for women whose partner has an AUD. Web-based interventions have the potential to reduce accessibility, relationship, psychological, and time barriers, and could reach a potentially larger portion of this underserved group than face-to-face interventions (Rychtarik, McGillicuddy, & Barrick, 2013). This study tested whether an Internet-based Coping Skills Training (iCST) intervention, relative to a Delayed Treatment Control (DTC) condition, would increase coping skills and reduce depressive symptoms at the end of site access. It also explored (a) whether skill acquisition mediated the intervention effect, (b) iCST-DTC differences on secondary spouse outcomes of anger, anxiety, and stress, (c) condition differences on tertiary and ancillary measures of partner drinking, spouse and partner help seeking, contact days, and relationship violence, and (c) iCST usage and its relationship to outcome. The intervention’s effect on DTC participants, once provided access, also is discussed.
Method
Participants
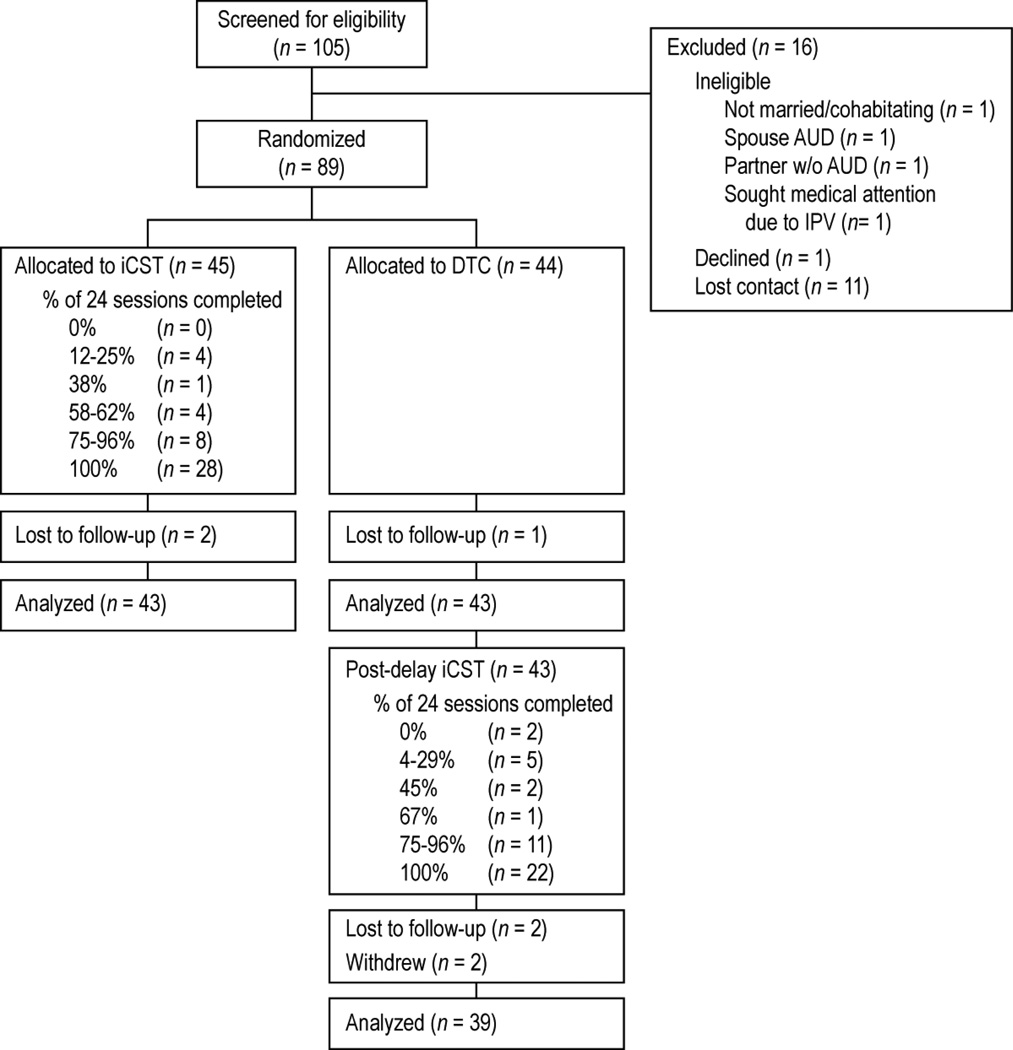
Participants were 89 women responding to media advertisements, or a professional referral for StopSpinningMyWheels.org, a web-based, self-administered program for women with problem-drinking partners. The women (a) were at least 18 years of age, (b) were currently married, or living with their partner, (c) reported partner recent problematic alcohol use (score ≥ 5) on the participant-administered Alcohol Use Disorder Identification Test—Consumption items (AUDIT-C; Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998), and a positive partner alcohol diagnosis on the Family History Assessment Module (Janca, Bucholz, & Janca, 1992), (d) were not suicidal, (e) had no substance use, or unremitted psychotic disorder of their own as assessed by the Structured Clinical Interview for Diagnosis (First, Spitzer, Gibbon, & Williams, 1996), and (f) did not fear for their life, or seek past-year medical help due to partner violence. See Figure 1 for consort flowchart; see Table 1 for sample demographic and baseline characteristics.
Figure 1.
Study design and participant flow.
Table 1.
Spouse, and Spouse-Reported Partner Characteristics by Treatment Condition
| iCST | DTC | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n = 45 | n= 44 | ||||||||
| Characteristic | M | SD | % (n) | M | SD | % (n) | t | X2(df) | p |
| Spouse | |||||||||
| Age | 49.09 | 9.66 | 49.68 | 10.62 | −.28 | .78 | |||
| Years of education | 15.11 | 2.30 | 15.55 | 2.44 | −.87 | .39 | |||
| Race/ethnicity | .24 (2) | .84m | |||||||
| White | 93 (42) | 91(40) | |||||||
| Black | 4(2) | 7(3) | |||||||
| Hispanic | 2 (1) | 2(1) | |||||||
| Full/Part-time employment | 76 (34) | 70(31) | .29 (1) | .59 | |||||
| Occupational statusa | 5.71 | 2.07 | 6.09 | 1.72 | −.94 | .35 | |||
| Married | 87 (39) | 84 (37) | .12 (1) | .73 | |||||
| Years living together | 16.96 | 10.82 | 18.08 | 13.01 | −.44 | .66 | |||
| Percentage of days with partner contactb | 94.09 | 12.57 | 97.16 | 5.46 | −1.30 | .20 | |||
| Self-help group attendance everc | 44(20) | 46(20) | .01 (1) | .92 | |||||
| Self-help group attendance past 8 weeksc | 2(1) | 9(4) | 1.97 (1) | .20m | |||||
| Professional help everd | 38(17) | 50(22) | 1.35 (1) | .25 | |||||
| Professional help past 8 weeksd | 31(14) | 36(16) | .28 (1) | .60 | |||||
| SSIe | 3.00 | .30 | 2.87 | .33 | 1.87 | .07 | |||
| BDI-II | 13.24 | 10.86 | 12.52 | 10.10 | .34 | .74 | |||
| STAXI-II, State Anger | 19.31 | 6.23 | 18.68 | 4.96 | .27 | .78 | |||
| STAXI-II, Anger Expression Index | 37.31 | 7.65 | 37.52 | 7.55 | .10 | .72 | |||
| DASS Anxiety | 4.91 | 6.75 | 2.70 | 3.61 | 1.86 | .07 | |||
| DASS Stress | 9.42 | 7.95 | 9.18 | 6.80 | −.07 | .95 | |||
| IPV | |||||||||
| Initiated any IPV episodef | 11 (5) | 9 (4) | .10 (1) | 1.00n | |||||
| Any severe IPV against partnerg | 4 (2) | 7 (3) | .24 (1) | .68n | |||||
| Minor IPV only against partnerh | 9 (4) | 5 (2) | .67 (1) | .68n | |||||
| Partneri | |||||||||
| AUDIT-C | 9.80 | 1.73 | 9.00 | 2.17 | −1.71 | .09 | |||
| FHAM alcohol symptomsj | 10.64 | 3.68 | 10.45 | 3.66 | .24 | .81 | |||
| Years of problem drinking | 20.53 | 12.79 | 22.28 | 12.43 | −.66 | .51 | |||
| Drug dependence diagnosisk | 16 (7) | 9 (4) | .86 (1) | .34 | |||||
| Professional help everl | 47(21) | 39(17) | .59 (1) | .44 | |||||
| Professional help past 8 weeksl | 11(5) | 14(6) | .13 (1) | .72 | |||||
| PDAm | 23.20 | 35.72 | 27.32 | 36.53 | −.59 | .56 | |||
| DDDm | 8.23 | 6.04 | 7.85 | 6.69 | .27 | .79 | |||
| IPV | |||||||||
| Initiated any IPV episodef | 11 (5) | 9 (4) | .10 (1) | 1.00n | |||||
| Any severe IPV against spouseg | 0 (0) | 7 (3) | 3.17 (1) | .12n | |||||
| Minor IPV only against spouseh | 16 (7) | 7 (3) | 1.70 (1) | .32n | |||||
Note.iCST = Internet-based Coping Skills Training; DTC = Delayed Treatment Control; SSI = Spouse Situation Inventory; BDI-II = Beck Depression Inventory, Second Edition; STAXI-II = State Trait Anger Expression Inventory, Second Edition; DASS = Depression Anxiety and Stress Scales; AUDIT-C = Alcohol Use Disorders Identification Test consumption items; FHAM = Family History Assessment Module for alcohol dependence; PDA = Percentage of Days Abstinent; DDD = Drinks per Drinking Day; IPV = Intimate Partner Violence (physical). Raw means and SDs are presented; to reduce skew and accommodate outliers, analysis results for some variables are on based on square root (BDI-II, DASS, DDD), negative inverse (STAXI), reflected square root (AUDIT-C), and arcsine (PDA) transformations.
Hollingshead and Redlich (1958) coded 1 (low status) to 9 (high status), n = 44 each for CST and DTC;
Days on which spouse reported having contact with the partner in the past 8 weeks;
Al-Anon, Nar Anon, or other self-help group attendance related to the partner’s substance use disorder;
Individual therapy, or professionally-led family group program attendance related to the partner’s substance use disorder;
n = 44 each, for iCST and DTC;
an IPV episode is a time delimited period of physical IPV separated by several hours or days;
across IPV episodes, and regardless of initiator, severe violence reported included hitting with a fist, slamming against a wall, kicking, and choking;
across IPV episodes, and regardless of initiator, minor violence reported included grabbing, pushing, shoving, slapping, pulling/twisting hair, and throwing something;
as reported by the spouse;
positivealcohol use disorder symptoms out of 19 over the past 12 months;
From the drug dependence module of the FHAM.
Partner professional substance abuse treatment through either an individual therapist, or formal inpatient or outpatient program;
during the last week of the baseline period; for PDA n = 43 and n = 40, for iCST and DTC, respectively; for DDD n = 41 and n = 40, respectively;
Fisher’s exact test (two-tailed), or the Freeman-Halton extension of Fisher’s exact test for 2 X 3 contingency tables. The p values are based on t-tests for continuous measures; chi square tests of independence for categorical measures.
Procedure
Following online and phone baseline assessments, participants were randomly assigned either to 8-week iCST access, or to the DTC. A biased coin (p = .75), urn randomization procedure was used to help balance conditions on sample size, education (< 12 years; ≥ 12 years), partner past three months treatment history (Yes; No), and past three months participant Al-Anon attendance (Yes; No). At the end of the 8-week access/delay period, online and phone assessments were again administered. Phone interviewers were blind to access condition assignment. DTC participants were given 8-week access to iCST on completion of their postdelay assessment, and readministered the postaccess assessment. The study was designed a priori to detect a moderate iCST-DTC effect on depressive symptoms at p < .05, power = .80.
Treatment Conditions
Internet-based Coping Skills Training (iCST)
Participants in iCST received (a) 8-week access to StopSpinningMyWheels.org, a 24-session, self-paced, online skill training website, and (b) randomization to one of two site coaches (professional counselors) who could, at the participant’s discretion, be consulted either by phone, secure email, or chat. Participants received a brief initial coach phone call to instruct them in accessing the site; additional brief contacts occurred at Weeks 1, 3, and 6 to assess access problems, encourage site use, and remind of the coach’s availability. Site content was adapted from the face-to-face, Coping Skills Training (CST) reported in Rychtarik and McGillicuddy (2005), and focused on reducing participant distress. Sessions, administered sequentially, averaged 17 min (range: 4 to 32 min). Participants initially were introduced, via videos, to five different women (portrayed by actresses) who described their history and struggles living with a partner with an AUD. These women were then followed in remaining sessions as they struggled and coped with problem situations related to their partner’s drinking. Problem situations were from Form A of the Spouse Situation Inventory (SSI; Rychtarik & McGillicuddy, 1997). The videos, instructional narration, animated presentations, quizzes, and personal journaling, then trained participants to (a) focus on their own needs, (b) manage negative thinking, (c) problem solve situations, (d) use functional analysis of self and partner behavior, and (e) communicate with greater consistency and clarity.
Delayed Treatment Condition (DTC)
Participants in DTC received access to the program site after an 8-week delay, and upon completion of the postdelay assessment.
Measures
Online measures
The score on The Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996) was the primary outcome measure. Secondary spouse outcome measures included the State Anger subscale, and Anger Expression Index of the State-Trait Anger Expression Inventory, (STAXI-2; Spielberger, 1999), and the Anxiety and Stress subscales of the Depression, Anxiety, Stress Scales (DASS; Lovibond & Lovibond, 1995). The Client Satisfaction Questionnaire (CSQ-8; Attkisson & Greenfield, 2004) assessed site satifaction.
Phone measures
The Spouse Situation Inventory (SSI, Forms A and B; Rychtarik & McGillicuddy, 1997) was administered to assess skill acquisition. This role-play measure consists of 24 representative alcohol-related problem-situation vignettes experienced by women with partners with an AUD (e.g., partner drunkenness, violence, impact on children/family), and possesses good levels of reliability and generalizability. Form A was administered at baseline; Form B administered at postaccess/delay. Responses were audio recorded, and scored on a 1 (not effective at all) to 6 (extremely effective) scale by a trained rater using standardized scoring criteria, and blind to access condition assignment. A second blind rater independently scored a subset of SSI responses; interrater ICCs were .74 and .78 for Forms A and B, respectively. The Alcohol and Drug Use (Sobell & Sobell, 1996), and Intimate Partner Violence (IPV) Timeline (Fals-Stewart, Birchler, & Kelley, 2003) interviews were administered to the spouse to assess, respectively, her reports of the partner’s alcohol use, and her physical IPV victimization and perpetration in the 90-day baseline, and the 56-day access/delay periods. Weekly percentage of days abstinent (PDA) from alcohol, and weekly number of standard alcoholic drinks per drinking day (DDD) in the last week of baseline, and in the access/delay period served as baseline and postaccess/delay partner-drinking measures, respectively; abstinent weeks were coded “0” DDD. Ancillary timeline outcomes were prevalence of spouse and partner treatment, spouse self-help, IPV episodes, and minor (e.g., push, grab, slap), and severe (e.g., hit with fist, choke, threatened with knife) IPV behaviors, and percentage of days the spouse had contact with the partner.
Site usage, coach contacts, and satisfaction in iCST
Participants in iCST averaged 20.38 (SD = 6.03) sessions, 7.04 (SD = 1.28) weeks to complete all 24, and 13.67 (SD = 5.18) out of 17 possible journal entries. Sessions and journal entries were highly correlated, r(40) = .71, p < .001. To avoid redundancy, only proportion of sessions completed was used in site usage analyses. Coach phone contacts were audio recorded, and coaches provided written notes of all contacts, or attempted contacts (i.e., voice mail, email). A trained rater categorized each coach note by content (i.e., administrative [e.g., initial, 1, 3, and 6-week check-ins], technical [e.g., lost password], or clinical [e.g., help with applying site material to one’s own life], and type (i.e., live phone, voice mail, or e-mail). No participant used online chat. A second rater independently rated coach notes on a random 20% participant sample. Interrater Kappas were .82, and .87 for content and type, respectively. The average number of administrative, technical, and clinical coach contacts was 4.73 (SD = 2.96; Mdn = 4), 2.58 (SD = 2.58; Mdn = 2), and 1.18 (SD = 2.16; Mdn = 0), respectively. Thirty-eight percent had at least one clinical contact. A separate experienced rater rated, for each participant, overall coach competence, 0 (inadequate) to 6 (flawless), from audios of live phone contacts; a second rater independently rated a random 20% sample; at least one live recording was available from 84% of participants; interrater ICC = .60. The competence scale, adapted from Young & Beck (1980), reflected interpersonal warmth, ease in eliciting feedback, and, in clinical contacts, treatment fidelity. Median competence ratings were 4 (Very Good) and 3 (Good) for the respective coaches. Satisfaction with iCST was high, CSQ-8 item M = 3.51 (out of 4), SD = .48.
Data analyses
The prevalence of partner treatment, spouse self-help, and IPV was too low for adequate data analyses. Hence, results on these variables are only descriptive. A square root transformation was used on BDI, DASS, DDD, and number of administrative contacts data; an arcsine transformation was used for PDA, and proportion of completed sessions and journal entries; a negative inverse transformation was used for STAXI-II subscale scores, and coach clinical contacts. SSI data were missing from one subject due to a phone-recording malfunction. Otherwise, missing data did not exceed 5% on primary and secondary spouse measures; missing partner drinking data were due largely to spouse uncertainty, and was not imputed. Access condition differences on spouse primary and secondary outcomes were assessed using intent-to-treat ANCOVA in SAS Proc GLM. SAS Proc Mixed was used for two-level, mixed effects analyses of partner weekly PDA and DDD across the 8-week access/delay period, with random intercepts and linear time slopes, and an unstructured variance-covariance matrix. The baseline value of the dependent variable was a covariate in all analyses; and partialled out of correlations, where applicable. Coach assignment, and variables with baseline iCST-DTC differences approaching significance (see Table 1) were included in an initial set of analyses; none affected outcomes, and were not included in final analyses. Bias-corrected, bootstrapped confidence intervals (CIs; Preacher & Hayes, 2008) were used to explore the indirect (mediating) effect of the SSI on BDI, controlling for respective baseline values. The standardized mean difference (d) in adjusted score means from ANCOVA and mixed models used baseline SD as the divisor; bias-corrected CIs for d were bootstrapped. Tables and figures report adjusted means, or back transformed adjusted means, and bootstrapped SEs. All bootstrapping used 1,000 samples.
Results
Did iCST increase coping skillfulness and decrease depressive symptoms compared to DTC?
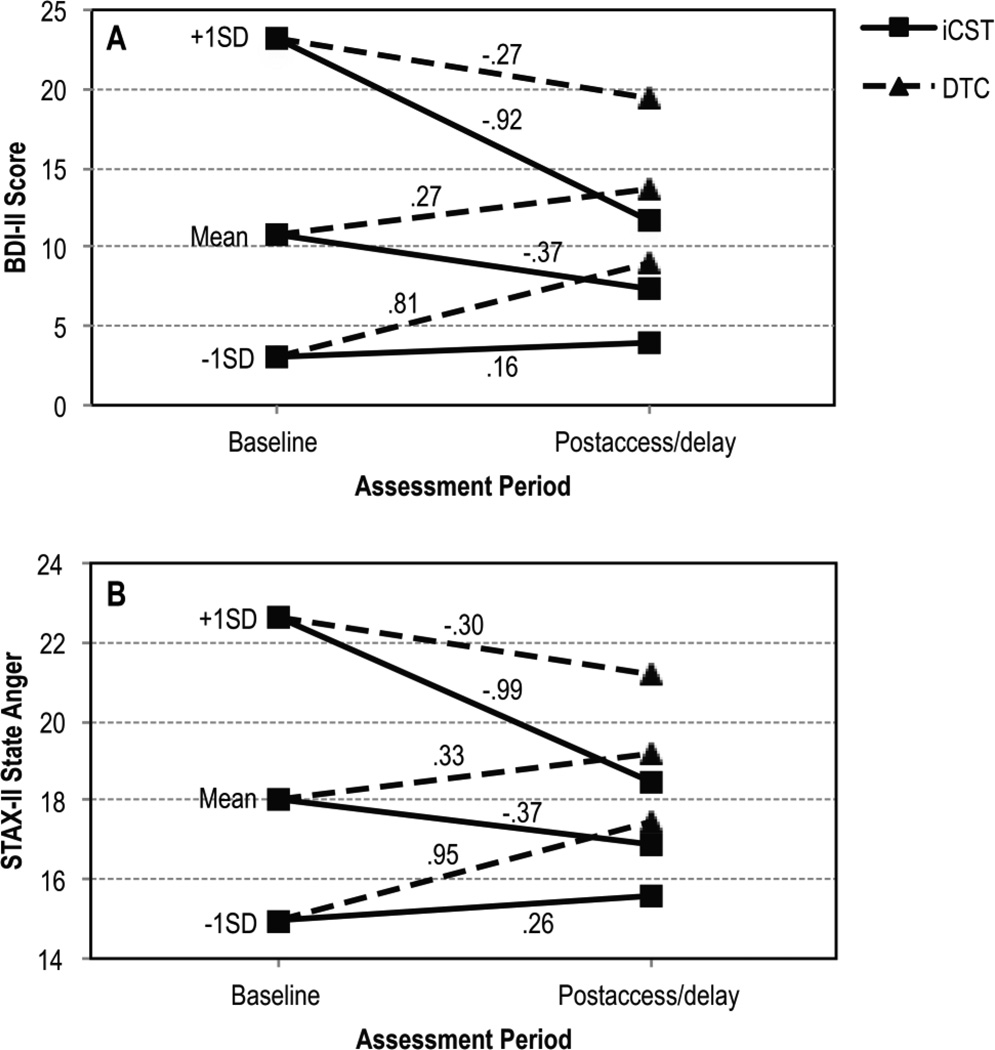
Participants in iCST exhibited greater postaccess skill than did those in DTC (see Table 2). From baseline to postaccess/delay, iCST participants showed a large skill increase, d = 1.06, 95% CI [.57, 1.49], while DTC participants had little change, d = .09, 95% CI [−.22, .37]. At the same time, depressive symptoms were significantly lower in iCST than DTC (see Table 2). As shown in Figure 2A, change in DTC, which largely reflected regression to the mean and other nonsite-specific factors, showed a small decrease at high baseline depression levels, a small increase at the mean baseline level, and a large increase among those with originally low depression scores. In contrast, depressive symptoms in iCST showed a large reduction from high baseline levels, a modest reduction at the mean level, and remained quite stable at low baseline levels—preventing the increasing trajectory at this level seen in DTC. The indirect (mediating) effect of postaccess/delay SSI skill on participant depressive symptoms was significant, r = .28, SE = .15, 95% CI [.003, .62], accounting for 28.3% of the total access condition effect.
Table 2.
Adjusted means, SEs, and main site access condition effects at the end of the 8-week site access/delay period for spouse primary, secondary, and partner-related tertiary outcomes.
| iCST |
DTC |
|||||||
|---|---|---|---|---|---|---|---|---|
| Outcome measure | M | SE | M | SE | F(1,83) | p | d |
d 95% CI |
| Spouse Primary | ||||||||
| SSI | 3.28 | .05 | 2.96 | .05 | 26.01a | <.001 | 1.02 | [.64, 1.51] |
| BDI-II | 7.32 | 1.2 | 13.64 | 1.39 | 10.71 | .002 | −.65 | [−1.21, −.35] |
| Spouse Secondary | ||||||||
| STAXI-II State Anger | 16.90 | .39 | 19.14 | .61 | 10.54 | .002 | −.70 | [−1.62, −.64] |
| STAXI-II Anger Expression |
35.10 | .99 | 35.48 | .92 | .14 | .71 | −.06 | [−.41, .26] |
| DASS-Anxiety | 1.81 | .37 | 2.98 | .73 | 2.52 | .12 | −.32 | [−.74, .01] |
| DASS-Stress | 7.34 | .99 | 8.35 | 1.18 | .48 | .49 | −.14 | [−.55, .22] |
| Partner-related tertiary | ||||||||
| PDA | 18.34 | 3.52 | 20.02 | 4.01 | .05b | .81 | −.03 | [−.31, .20] |
| DDD | 6.49 | .89 | 5.92 | .69 | .18c | .67 | .08 | [−.26, .40] |
Note: iCST = Internet-based Coping Skills Training; DTC = Delayed Treatment Control; d = standardized mean difference (iCST – DTC); CI = confidence interval of d; SSI = Spouse Situation Inventory; BDI-II = Beck Depression Inventory, Second Edition; STAXI-II S-Ang = State Anger subscale of the State Trait Anger Expression Inventory, Second Edition; STAXI-II AXI = Anger Expression of the State Trait Anger Expression Inventory, Second Edition; DASS = Depression Anxiety and Stress Scales; PDA = Weekly Percentage of Days Abstinent; DDD = weekly average Drinks per Drinking Day. All analysis models controlled for the baseline value of the dependent variable. Analyses of BDI-II, STAXI-II, and DASS subscales were conducted on square root, negative inverse, and square root transformed scores, respectively. Analyses of PDA and DDD were conducted on arsine and square root transformed values, respectively. Means for PDA and DDD are at the midpoint of the access/delay interval. Except for SSI scores, which were not transformed, means presented are back-transformed, with bootstrapped SEs.d values are based on iCST-DTC differences in adjusted means of transformed scores, where applicable, divided by the baseline SD; dbootstrap confidence intervals are bias-corrected.
Ns = 43 each in iCST and DTC for BDI-II, STAXI-II, and DASS variables; iCST-DTC respective Ns = 42 and 43 for SSI, 41 and 42 for PDA, and 40 and 39 for DDD.
dfs = 1,82;
dfs = 1, 76.9;
dfs = 1, 72.7.
Figure 2.
Change from baseline to postaccess/delay on Beck Depression Inventory-II (A) and State Trait Anger Expression Inventory-II, State Anger (B) scores. Change is shown at baseline + 1 SD, mean, and -1 SD levels. Means are back transformed adjusted means. iCST = Internet-based Coping Skills Training; DTC = Delayed Treatment Control. Numbers above the lines are standardized mean differences between postaccess/delay and baseline; d 95% CIs on the BDI-II for iCST at the three respective baseline levels were [−1.32, −.57], [−.76, −.01], and [−.40, .59]; respective d CIs for DTC were [−.61, −.05], [−.76, −.01], and [.35, 1.21]. Respective d CIs on State Anger for iCST were [−1.52, −.65], [−.77, −.18], and [−.002, .61]; respective d CIs for DTC were [−.77, .12], [−.05, .70], and [.64, 1.62].
What were the effects of site access condition on secondary spouse outcomes?
State anger was significantly less in iCST than DTC; anger-expression, anxiety, and stress did not differ between conditions (see Table 2). The pattern of change in state anger closely mirrored that for depressive symptoms (see Figure 2B). Moderate to strong depression-anger associations at baseline and postaccess/delay, rBDI-State Anger = .45 and .58, respectively, may have accounted, in part, for some similarity in change patterns.
Did iCST and DTC differ on partner PDA and DDD, help seeking, violence, or contact days?
No PDA or DDD differences emerged (see Table 2). The respective iCST-DTC prevalence of partners in treatment, 9% and 14%, spouse self-help attendance, 7% and 2%, other spouse treatment, 33% and 33%, and the percentage of contact days, 95.12% (SD = 11.06) and 94.03% (SD = 11.34), also did not differ. Nor were respective differences evident in the prevalence of spouse-initiated IPV episodes, 7% and 9%, partner-initiated episodes, 9% and 5%, spouse violence of any type, 7% and 12%, spouse severe violence, 0% and 2%, partner violence of any type, 12% and 7%, or partner severe violence, 0% and 0%. A small PDA increase from Week 1 to Week 8, back-transformed adj Ms = 15.70% (SE = 2.86) and 23.79% (SE = 3.40), respectively, d = .19, 95% CI [.02, .36], approached significance, F(1, 73.9) = 3.46, p = .07, but did not differ by condition, F(1, 72.7) = .14, p = .71. Also, no DDD time, F(1, 68.3) = .83, p = .36, or Condition X Time effect, F(1, 67.3) = .10, p = .75, emerged.
Were sessions completed, and coach contacts related to baseline or postaccess depressive symptoms in iCST?
Table 3 shows intercorrelations among the variables. Depressive symptoms at baseline were not significantly associated with sessions completed or coach contacts during site access. Fewer postaccess depressive symptoms, however, were associated, to a moderate degree, with having completed more sessions, while more depressive symptoms were associated with having had more administrative and, to a lesser extent, clinical contacts. The latter finding for administrative contacts may result from their being negatively associated with sessions completed. In fact, controlling for sessions completed, the depression-administrative contacts association was no longer significant, r(39)partial = .16, 95% CI [−.15, .45], p = .308. Overall, those slow to engage in the site appeared to be more difficult to contact, received more administrative contact attempts and, due to the lower engagement, benefitted less.
Table 3.
Intercorrelations, partial intercorrelations, and 95% confidence intervals among site usage, coach contact, and depressive symptom measures in iCST
| Measure | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Sessions completed (%) | - | −.43** [−.64, −.16] |
.01 [−.28, .30] |
−.08 [−.36, .22] |
−.38* [−.61, −.08] |
| 2. Number of administrative coach contacts | - | −.13 [−.40, .18] |
−.10 [−.38, .20] |
.31* [.00, .56] |
|
| 3. Number of clinical coach contacts | - | .18 [−.12, .45] |
.28† [−.02, .54] |
||
| 4. Baseline BDI-II | - | .44** [.16, .65] |
|||
| 5. Postaccess BDI=II | - |
Note BDI-II = Beck Depression Inventory-II; Sessions completed = arcsine transformed percentage of sessions completed; administrative contacts, and clinical contacts are square-root transformed; and clinical contacts are negative inverse transformed. Correlations between postaccess BDI-II and sessions completed, administrative contacts, and clinical contacts partial out baseline BDI-II.
N = 45; N = 43 for correlations with postaccess BDI-II.
p < .05;
p < .01;
p < .07.
What were DTC participant outcomes following 8-week site access?
With the exception of a significant decrease in stress, former DTC participants exhibited a change pattern identical to those in iCST (detailed results are available from the first author).
Discussion
This study provides initial support for the efficacy of web-based coping skills training for women experiencing distress from their partner’s AUD. Relative to no intervention, iCST increased coping skills, decreased depressive symptoms and anger, and prevented increases in depression and anger among those with initially low baseline levels on these measures. At baseline, the sample fell, on average, within what is often referred to as the subclinical or subsyndromal range of depressive symptoms, and averaged at the 80th percentile of state anger; at postaccess, scores reduced to well within the minimal or normal range on both measures. Subclinical depression is associated with increased psychosocial problems, societal costs, and risk for major depressive and other disorders (Pietrzak et al., 2013). Hence, the results suggest that iCST can produce both clinically relevant and, preventative change. The findings are comparable to the short-term effects found in the face-to-face CST (Rychtarik & McGillicuddy, 2005), from which iCST was adapted. Further research is needed to determine whether long-term maintenance of outcomes in the face-to-face format occurs in iCST, as well.
Differences between iCST and DTC were not found on other secondary spouse outcome measures, which fell within the normal range at baseline. Depression and situational anger appear to most accurately reflect the nature of distress observed in this population. No intervention effect was observed on tertiary or ancillary partner outcomes. This finding was expected because the focus of iCST was on improving the spouse’s functioning, and not specifically on getting the partner to change, or get help. Also, participants may not have had time to implement new skills related to partner communication, which were presented in the later sessions. The small increase in PDA observed in both conditions may reflect regression to the mean, or a reactive effect of some partners knowing of their spouse’s study involvement. Similar findings were observed in Rychtarik and McGillicuddy (2005), where only during long-term follow-up were moderate and large changes in PDA and DDD, respectively, observed.
DTC participants received no coach contacts during the delay period. Hence, one cannot rule out that these contacts, or the mere availability of a coach accounted for some change in iCST. Yet, coach contacts did not appear to be an active change agent. Instead they were associated with more, not fewer, depressive symptoms—reflecting the greater effort required to engage unengaged participants, and the demand for more help among those benefiting less.
The current sample was largely middle aged, highly educated, white, and married, with one third receiving other treatment, perhaps limiting level of distress, and generalizability. Still, the findings suggest that iCST can, at least in the short-term, significantly reduce, and possibly prevent distress among women whose partner has an AUD. Programs such as this may help address treatment barriers for this underserved population. Additional research is needed to study its long-term efficacy, compare it to alternate treatments (e.g., online Al-Anon), better delineate coach effects, assess prospective mediation, and study other key ingredients for change.
Acknowledgments
This research was funded by Grant RC1AA019028 from the National Institute on Alcohol Abuse and Alcoholism. We thank Joan Duquette who provided invaluable and insightful work on StopSpinningMyWheels.org content development, John Messersmith who worked tirelessly on programming, video editing, and technical support, George Gogos, who kept server and support software running, and to the coaching and research technician staff of the Stop Spinning MyWheels project without whom this study would not be possible. Also, special thanks to the staff of Full Circle Studios, LLC of Buffalo, NY for their high quality video production work, and to Brian Danaher, David Kerr, and Christopher Wolfe for their expert consultation on web-design and web-learning.
Further details on methods and results are available from the first author upon request.
References
- Attkisson CC, Greenfield TK. The UCSF Client Satisfaction Scales: I. The Client Satisfaction Questionnaire-8. In: Maruish ME, editor. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment. 3rd Ed. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. pp. 799–812. 2004-14941-027. [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Substance Abuse Treatment and Family Therapy. Treatment Improvement Protocol (TIP) Series, No. 39. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2004. DHHS Publication No. (SMA) 05-4006. [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Chou SP, Stinson FS. The impact of partner alcohol problems on women’s physical and mental health. Journal of Studies on Alcohol. 2007;68:66–75. doi: 10.15288/jsad.2007.68.66. PMID: 17149519. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Birchler GR, Kelley ML. The Timeline Followback Spousal Violence Interview to assess physical aggression between intimate partners: Reliability and validity. Journal of Family Violence. 2003;18:131–142. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P) (Version 2.0) New York: New York State Psychiatric Institute, Biometrics Research Department; 1996. [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Janca A, Bucholz K, Janca I. Family History Assessment Module. Louis, MO: Washington University of Medicine, St.; 1992. [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales (DASS) 2nd Ed. Sydney: Psychology Foundation; 1995. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol use and alcohol use disorders in the United States: Main findings from the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institutes of Health; 2006. U.S. Alcohol Epidemiologic Data Reference Manual (Vol. 8), no. 1, NIH Publication No. (05-5737) [Google Scholar]
- O’Farrell TJ, Clements K. Review of outcome research on marital and family therapy in treatment for alcoholism. Journal of Marital and Family Therapy. 2012;38:122–144. doi: 10.1111/j.1752-0606.2011.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Kinley J, Afifi TO, Enns MW, Fawcett J, Sareen J. Subsyndromal depression in the United States: Prevalence, course, and risk for incident psychiatric outcomes. Psychological Medicine. 2013;43:1401–1414. doi: 10.1017/S0033291712002309. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behaviors Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Ray GT, Mertens JR, Weisner CW. The excess medical cost and health problems of family members of persons diagnosed with alcohol or drug problems. Medical Care. 2007;45:116–122. doi: 10.1097/01.mlr.0000241109.55054.04. [DOI] [PubMed] [Google Scholar]
- Rychtarik RG, McGillicuddy NB. The Spouse Situation Inventory: A role-play measure of coping skills in women with alcoholic partners. Journal of Family Psychology. 1997;11:289–300. doi: 10.1037/0893-3200.11.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rychtarik RG, McGillicuddy NB. Skill training and 12-step facilitation for women with alcoholic partners: Effects on the women’s depression and the partners’ drinking. Journal of Consulting and Clinical Psychology. 2005;73:249–261. doi: 10.1037/0022-006X.73.2.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rychtarik RG, McGillicuddy NB, Barrick C. Reaching women under stress from a partner’s drinking problem: Assessing interest in online help. Journal of Technology in Human Services. 2013;31:185–196. [Google Scholar]
- Sobell LC, Sobell M. Timeline FollowBack (TLFB) Toronto, Ontario: Centre for Addiction and Mental Health; 1996. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory II (STAXI-2) Odessa, FL: PAR/Psychological Assessment Resources; 1999. [Google Scholar]
- Timko C, Young LB, Moos RH. Al-Anon Family Groups: Origins, conceptual basis, outcomes, and research opportunities. Journal of Groups in Addiction & Recovery. 2012;7:279–229. [Google Scholar]
- Young J, Beck AT. Cognitive therapy scale: Rating manual. Bala Cynwyd, PA: Beck Institute for Cognitive Behavior Therapy; 1980. Unpublished manuscript. [Google Scholar]