Abstract
Aims
To determine whether chronic life stress is differentially associated with quality of life (QoL) for Blacks vs. Hispanics with Type 2 Diabetes.
Methods
We assessed self-reported chronic stress and QoL in 125 patients with Type 2 diabetes who self-identified as either non-Hispanic Black or Hispanic. Separate cross-sectional two-way interaction models (stress × race/ethnicity) with physical and mental health as outcomes were examined.
Results
The two-way interaction predicted mental (b = 3.12, P = .04) but not physical health. Simple slopes analyses indicated that under conditions of high stress, Blacks (b = −4.4, P < .001), but not Hispanics, experienced significantly lower levels of mental health. In exploratory analyses, we examined a three-way interaction (stress × race/ethnicity × social support) with physical and mental health as outcomes. Results indicated the three-way interaction predicted mental (b = .62, P = .01) but not physical health. Simple slopes analyses indicated that under conditions of high stress, high levels of social support improved mental health for Hispanics (b = 1.2, P < .001), but not for Blacks.
Conclusions
Black patients with Type 2 diabetes may be particularly vulnerable to the deleterious effects of high chronic stress. Social support buffers effects of stress on mental health in Hispanics but not Blacks, which suggests differences in the use and/or quality of social support between Hispanics and Blacks. Longitudinal investigations that examine race/ethnicity, stress, social support, and QoL should help clarify the processes that underlie these observed relations.
Keywords: diabetes, race/ethnicity, social support, stress
Introduction
Nearly 26 million Americans are living with diabetes [1] with type 2 diabetes accounting for 90–95% of all diagnosed cases [2]. Patients with diabetes frequently experience impaired quality of life (QoL) due to diabetes-related distress and complications and comorbidities associated with this chronic disease. Black and Hispanic adults are two to three times more likely to have type 2 diabetes [3] and to suffer from diabetes-related distress [4], complications [5,6] and poor QoL [7] compared to non-Hispanic Whites. Blacks and Hispanics also encounter more severe chronic life stress (e.g., access to fewer economic resources and racial/ethnic discrimination) compared to non-Hispanic Whites [8,9], which may exacerbate the impact of diabetes on QoL. Several studies have found that exposure to chronic stress increases the risk of being diagnosed with diabetes [10–13] and contributes to poor glucose control [14]. However, the majority of studies of the effects of chronic stress in diabetes patients have been conducted in predominantly Caucasian samples, the findings from which may not generalize to other racial/ethnic groups. Additionally, most investigations that have included non-Caucasian patients have combined Blacks and Hispanics into one category and compared them to Whites, which ignores the possibility that Blacks and Hispanics with diabetes may be differentially susceptible to the effects of chronic stress. A couple of notable studies have examined the role of stress in Blacks and Hispanics separately [14,15] but are limited by a focus on one type of life stress (e.g., discrimination) and a restricted range of outcomes (e.g., diabetes-related distress). Evidence from large-scale epidemiological studies demonstrating that Blacks and Hispanics experience divergent health outcomes despite similar socioeconomic disadvantages [16], a phenomenon known as the Hispanic Paradox [17,18], underscores the importance of examining whether the effects of chronic stress vary by race/ethnicity.
To our knowledge, no studies to date have examined whether exposure to a range of chronic stress domains predicts key outcomes such as mental and physical QoL in Black and Hispanic diabetes patients and whether race/ethnicity moderates this relationship. Understanding the relationship between chronic stress and QoL in Black and Hispanic diabetes patients will help to determine the need for stress reduction interventions in these groups and identify which patients are most likely to benefit from such interventions. Additionally, evaluating effects of a broad range of chronic life stressors beyond diabetes distress may inform culturally appropriate stress-reduction interventions for Black and Hispanic patients. In the present study we tested: a) whether chronic stress predicted QoL in Blacks and Hispanics with type 2 diabetes; and b) whether the relationship between chronic stress and QoL was moderated by race/ethnicity.
Subjects, Materials, and Methods
Patients and Procedures
Adult patients with diabetes (n = 125) who self-identified as non-Hispanic Black or Hispanic were enrolled from outpatient clinics at Bellevue Hospital Center in New York City. After providing written informed consent, patients completed self-report questionnaires with the help of a research assistant if needed. Patients’ medical records were reviewed to confirm the diagnosis of diabetes.
Study Assessments
Chronic stress was assessed using The Global Perceived Stress Scale (GPSS), developed for the Jackson Heart Study – an epidemiologic study of cardiovascular diseases in Blacks [19]. The GPSS is an eight-item questionnaire adapted from Kohn and MacDonald’s Survey of Recent Life Experiences [20], Cohen et al.’s Perceived Stress Scale [21], and Sarason et al.’s Life Events Scale [22] that measures the perception of stress experienced over a prior period of twelve months in the following domains: employment, relationships, neighborhood of residence, caring for others, legal problems, medical problems, experiences of racism and discrimination, and meeting basic needs. Participants rated each domain on the GPSS on a four-point scale ranging from (1 = “not stressful”; 4 = “very stressful”). A cumulative stress score was calculated by recoding each item rated as moderately or very stressful to a ‘1’ and summing across all 8-items, for a maximum cumulative stress score of 8. Internal consistency for the scale in this sample was α = .76.
Health-related QoL was assessed with the Short Form-12 (SF-12), a validated and widely-used self-report measure [23]. The SF-12 yields eight subscales representing various domains of functioning, which are combined to create Physical Component Summary (PCS) and Mental Component Summary (MCS) measures. Each subscale contributes to both summary measures, but physical functioning, physical role limitation, bodily pain and general health are weighted more heavily in the PCS score, whereas mental health, emotional role limitation, social function and vitality are weighted more heavily in the MCS score. PCS and MCS scores are transformed based on U.S. normative data to a mean of 50 and standard deviation of 10, where higher scores reflect better functioning. Internal consistency for the scale in this sample was α = .91.
Participants completed self-reported assessments of age, sex, marital status, education (years), and income. These variables were included as covariates in all analyses. Income was adjusted for differences in household size using an equivalence scale, dividing net income by the square root of household size [24].
Data Analyses
We conducted hierarchical regression analyses, centering predictor variables around their grand mean to facilitate the interpretation of main effects in models containing interaction terms (e.g., [25]). The predictors were entered into the regression model in the following two steps: (1) stress, race/ethnicity, and control variables (age, sex, marital status, education, and income); and (2) the interaction of stress and race/ethnicity. Variables in the regression models were free of extreme outliers, and we confirmed that distributions were appropriate for regression analyses.
Results
Table 1 displays sample demographics and characteristics. Patients were largely low-income and reported experiencing moderate or severe stress in an average of two of the eight assessed life domains. Black and Hispanic patients did not differ with respect to self-reported mental or physical health, chronic stress, or social support.
Table 1.
Participant Characteristics
| Variable | Blacks (n= 64) | Hispanics (n = 61) | Statistic | P |
|---|---|---|---|---|
| Mental Health | 59.3 (12.0) | 57.4 (14.0) | t(113)=0.99 | 0.32 |
| Physical Health | 51.8 (12.4) | 47.8 (12.7) | t(113)=1.31 | 0.19 |
| Stress | 2.1 (1.7) | 1.8 (1.8) | t(121)=0.10 | 0.92 |
| Social Support | 38.4 (7.4) | 36.8 (8.2) | t(132)=1.30 | 0.20 |
| Marital Status (% married) | 19.0 | 29.3 | X²(1)=1.75 | 0.19 |
| Age (years) | 57.4 (10.3) | 58.6 (9.8) | t(123)=0.22 | 0.83 |
| Sex (% female) | 32.8 | 55.7 | X²(1)=6.67 | 0.01 |
| Income ($) | 13,647 (11,437) | 11,678 (11,861) | t(98)=0.62 | 0.53 |
| Education (years) | 13.2 (3.3) | 10.6 (3.9) | t(123)=3.67 | <.001 |
Data are presented as Mean (SD) unless otherwise indicated.
Effects of chronic stress on quality of life and moderating role of race/ethnicity
Mental health
As shown in Table 2, results of regression analyses indicated a significant main effect of stress on mental health QoL (b = −.28, P < .01) and a significant two-way interaction (race/ethnicity × stress) (b = 3.12, P = .04). For a more specific test of these results, we conducted simple slope analyses [25], which revealed that stress predicted mental health for Blacks (b = −4.4, P < .001), but not for Hispanics, (b = −1.3, P = .23). Thus, Blacks experienced significantly lower levels of mental health under conditions of high vs. low stress, whereas Hispanics’ mental health remained stable across levels of stress (see Figure 1).
Table 2.
Results of Regression Analyses Predicting Level of Physical and Mental Health From Stress, Ethnicity, and Social Support
| Step 1* | Step 2 | Step 3 | Step 4 | Step 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Variable | b | β | b | β | b | β | b | β | b | β |
|
| ||||||||||
| Physical health | ΔR2 = .13 | ΔR2 = .00 | ΔR2 = .00 | ΔR2 = .00 | ΔR2 = .00 | |||||
| Stress | −.28 | −.04 | ||||||||
| Race/Ethnicity (R/E) | −3.52 | −.14 | ||||||||
| Stress × R/E | .45 | .05 | ||||||||
| Social Support | −.09 | −.06 | ||||||||
| Stress × Social Support | −.04 | −.04 | ||||||||
| R/E × Social Support | −.03 | −.08 | ||||||||
| Stress × R/E × Social Support | −.21 | −.80 | ||||||||
| Mental health | ΔR2 = .2† | ΔR2 = .04‡ | ΔR2 = .02 | ΔR2 = .04 | ΔR2 = .06† | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Stress | −2.76‡ | −.37‡ | ||||||||
| Race/Ethnicity (R/E) | −1.27 | −.05 | ||||||||
| Stress × R/E | 3.12‡ | 1.49‡ | ||||||||
| Social Support | .29 | .18 | ||||||||
| Stress × Social Support | .24‡ | .22‡ | ||||||||
| R/E × Social Support | .13 | .06 | ||||||||
| Stress × R/E × Social | .62* | .44‡ | ||||||||
R/E = Race/Ethnicity.
Age, sex, marital status, education, and income were entered as covariates in step 1.
P < .01.
P < .05.
Figure 1.
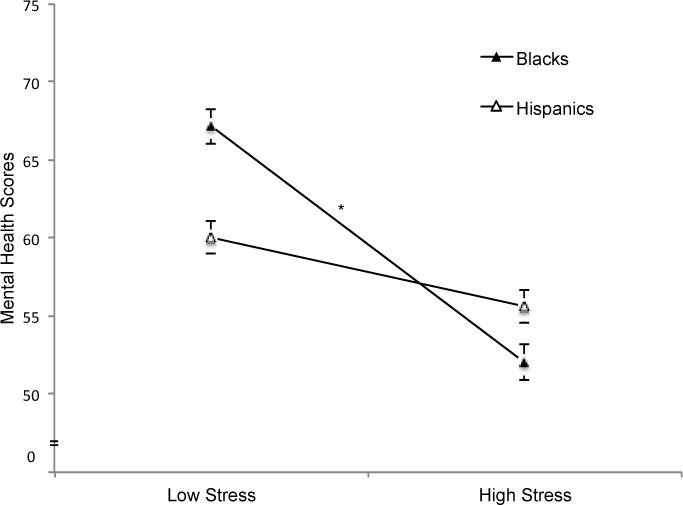
Test for a non-zero slope of the two-way interaction effect of ethnicity and stress on mental health scores. Values depict estimates at ±1 SD for stress. Error bars represent standard error of the mean.
*Slope is significantly different from zero (P < .05).
Physical health
As shown in Table 2, there was no significant main effect of stress on physical health QoL (b = −.28, P = .73) and no significant two-way interaction (race/ethnicity × stress) (b = .45, P = .77).
Exploratory analyses related to the moderating role of ethnicity on the relationship between chronic stress and QoL
In exploratory analyses, we examined a three-way interaction between race/ethnicity, chronic stress, and social support predicting mental health. The three-way model was motivated by the need for understanding third variables that may clarify the relationship between stress and race/ethnicity and also by evidence supporting a buffering role of social support between stress and diabetes-related outcomes [26,27]. Social support was assessed using the Interpersonal Support Evaluation List (ISEL), which includes four sub-scales (appraisal, belonging, self-esteem, and tangible support) and provides an overall measure of perceived support [28]. The three-way interaction model was run by entering the two-way interaction variables as described above and adding the following steps: (3) social support; (4) the remaining two-way interactions; and (5) the three-way interaction between stress, race/ethnicity, and social support.
As shown in Table 2, the three-way interaction was statistically significant for mental but not physical health QoL. Figure 2 shows that under conditions of low stress, social support did not affect mental health for Hispanics (b = −.48, P = .14), nor for Blacks (b = .45, P =.29). Further, these two slopes did not differ significantly from each other (t = −1.74, P =.09). At high stress levels, social support had a protective effect on mental health for Hispanics (b = 1.2, P < .001), but was unrelated to mental health for Blacks (b = −.00, P = .99). These two slopes differed significantly from each other (t = 2.23, P =.03). Thus, as evidenced by the positive slope for Hispanics, mental health scores improved for this group in the presence of high social support under conditions of high stress. On the other hand, Blacks’ mental health remained unchanged in the presence of social support at high levels of stress.
Figure 2.
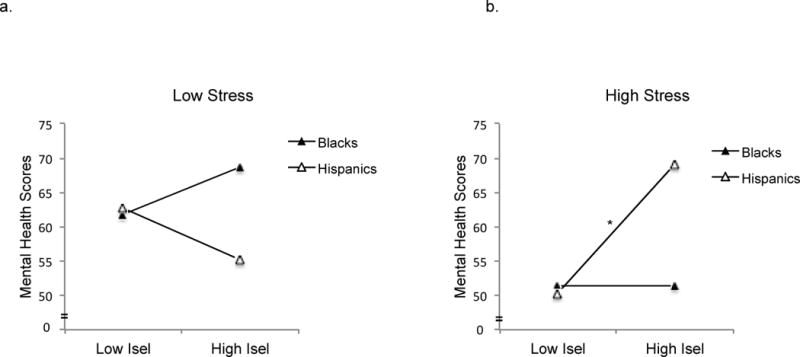
Test for a non-zero slope of the three-way interaction effect of race/ethnicity × stress × social support on mental health scores. Results are shown separately for participants who experienced (a) low and (b) high life stress. Values depict estimates at ±1 SD for stress and social support. Error bars represent standard error of the mean.
*Slope is significantly different from zero (P < .001)
Discussion
This study examined the relationship between chronic stress and mental and physical QoL in Black and Hispanic patients with type 2 diabetes. Results indicated that stress was related to poorer mental health but only for Blacks, not Hispanics. Exploratory analyses suggested that social support played a buffering role in protecting Hispanics, but not blacks, from experiencing poorer mental health in the face of high stress. No relationships were found between chronic stress and physical health.
The finding that Blacks experienced significantly poorer mental health under conditions of high stress points to stress as an important risk factor for mental health-related QoL in these patients. Lower scores on the mental health subscale of the SF-12 are highly correlated with depression [23], a costly emotional and economic burden for sufferers, family members, and society. These results underscore the potential utility for stress-reduction interventions for Black patients with diabetes who appear to be at greatest risk for psychopathology in the face of high chronic stress, and who thus may experience significant therapeutic gains from such treatment approaches. Results for Hispanics, who appeared to be buffered from experiencing poorer mental health under conditions of high stress, converge with epidemiological findings in support of the Hispanic Paradox, whereby Hispanics experience a morbidity/mortality advantage relative to other minority populations and non-Hispanic Whites [18].
The three-way interaction between stress, ethnicity, and social support points to potential differences in use and/or effects of social support between Blacks and Hispanics. Although no prior studies have directly tested this hypothesis, some evidence and theory suggest that the buffering effects of social support may be particularly robust in Hispanics [29,30]. For example, Hispanics are more likely than Blacks to have recently immigrated to the U.S. from Spanish-speaking nations. As such, Hispanics are more likely to face language barriers, and thus may rely more heavily on close family networks than Blacks [31]. In essence, Hispanics, compared to Blacks, may make greater use of social support.
One additional or alternative explanation could be that Blacks and Hispanics are affected by social support differently. For example, some research cautions that social support can reach a threshold, whereby perceived social support confers diminishing returns because reciprocal expectations and demands of social networks exceed capacity, thus creating stress [32]. It may be, then, that Blacks have a lower threshold than Hispanics and that more moderate, instead of high, levels of social support are adaptive for Blacks. Although we did not find evidence in support of this hypothesis in our data (i.e., no curvilinear trend was found when examining low, moderate, and high levels of social support in Blacks; and Hispanics had significantly higher mental health, compared to Blacks, at moderate levels of social support), this explanation cannot be ruled out due to potential confounds. For instance, the threshold model may hold in the context of different domains of social support. We were primarily interested in perceived social support, which predicts of a range of important outcomes [28] but does not directly index availability (i.e., actual support) or quality of social support, both of which may vary between Blacks and Hispanics and have been associated with unique outcomes [33]. Although definitive conclusions cannot be drawn about the buffering role of social support between Blacks in Hispanics, results suggest potential differences in utilization and or quality of support and highlight the importance of assessing distinct support domains (e.g., perceived vs. availability vs. quality) in future studies.
Given the significant findings for mental health and compelling epidemiological evidence in support of the Hispanic Paradox, null results for the main effect of stress and interaction between stress and ethnicity predicting physical health were surprising. However, evidence from correlational and experimental studies suggests that divergent findings for the relationships between stress and physical and mental health are not atypical [34,35]. Still, why would both the two- and three-way interactions predict mental but not physical health?
First, our findings may be explained by a diathesis-stress model whereby physical deterioration, in particular, occurs only after cumulative psychological stressors exceed a threshold. The measure of stress used in this study indexed stress severity over the previous 12 months, not cumulative stress over the lifespan—arguably, a more robust predictor of physical health [36]. Longitudinal investigations that measure the relationship between stress and physical health over the life course are needed to test this hypothesis. Second, null findings may be further explained by protective factors that were not assessed in this study (e.g., emotional intelligence and coping skills), which mitigate the effects of stress (i.e., differential susceptibility hypothesis: [37]). These explanations, however, should be considered with caution as null results are subject to a range of interpretations.
Several limitations of the current study merit further investigation. First, results are cross-sectional which restricts causal conclusions about the relationships between race/ethnicity, stress, social support, and mental health. For example, the directional model proposed considered stress and social support as predictors of mental health. One alternative hypothesis could be that poor mental health leads to increased stress and/or lower social support. Our measure of stress captured stress experienced over the course of 1 year prior to the assessment, as opposed stress during the moment of assessment, which renders this alternative explanation less likely. Additionally, our directional model is consistent with evidence from experimental and longitudinal studies, which demonstrate that stress predicts mental health instead of the other way around [38, 39]. Still, future investigations should test this model using a longitudinal design in which stress and social support are measured prospectively and at multiple time points.
Second, although adding the three-way interaction to the hierarchical regression analyses predicting mental health explained significant variance (P < .001), the variance explained was only 6%. Future studies should assess additional variables such as sociocultural attitudes and behaviors that may differ between Blacks and Hispanics [40], to clarify other conditions under which the two-way interaction between stress and race/ethnicity is significant.
Third, the present study is limited by reliance on self-report measures and a single measure of social support. Although we applied standardized inventories that have been used extensively in previous investigations, some of these measures are subject to retrospective and recall bias. Future research utilizing methods that minimize recall bias (e.g., daily diary assessments of stress) and comprehensively assess social support (e.g., inventories and/or peer assessments that index a range of social support domains) would enhance our understanding of the effects of race/ethnicity, stress, and social support on QoL.
Finally, Hispanics and Blacks were treated as undifferentiated groups, which ignores potentially large cultural differences within these groups (e.g., Dominicans, Puerto Ricans for Hispanics and Caribbeans, Africans for Blacks) that may influence outcomes. Future studies would do well to examine these groups separately in order thoroughly understand the role of stress and the absence of social support as risk factors for diminished QoL, which may be influenced by culture.
In conclusion, despite the fact that diabetes is most prevalent in Blacks and Hispanics and that chronic life stress is a recognized predictor of diabetes onset and severity, a dearth of research has examined the effects of chronic stress on QoL in Blacks and Hispanics with diabetes. This is especially unfortunate given that Blacks and Hispanics face higher life stress (e.g., discrimination and socioeconomic disadvantages) compared to non-Hispanic Whites. No studies that we are aware of have examined the association between chronic stress across a range of domains and QoL in Blacks and Hispanics and whether this relationship varies by race/ethnicity. Our study reports several novel findings regarding the relationships between stress, ethnicity, and social support. First, only Black patients with type 2 diabetes, not Hispanics, experienced poorer mental health under conditions of high stress. Second, the three-way interaction indicated that under conditions of high stress, social support had no influence on mental health for Blacks, but improved mental health for Hispanics. These findings were not explained by differences in levels of stress or social support between Blacks and Hispanics and suggest possible differences in stress coping and the utilization and/or effects of social support between these groups.
Overall, results point to the possible utility of stress reduction and tailored social support interventions aimed at teaching diabetes patients how to use their support networks, for Blacks, and increasing levels of social support for Hispanics with limited social networks. Given the pernicious effects of chronic stress on a range of physical and mental health disorders, future studies are needed that examine the relationships between stress, race/ethnicity, and social support in patients with other chronic diseases.
Acknowledgments
Funding from this study was provided by K24HL111315, awarded to G.O.
A.J.S. analyzed the data and wrote the manuscript. M.J.O collected the data. W.C supervised data analyses. G.O. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. T.M.S. designed and supervised the study, and contributed to analyzing the data and writing the manuscript.
The authors thank Alex Sierra, Oluchi Iheagwara, and Stephanie Grilo in the Center for Healthful Behavior Change for their assistance with this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Parts of this study were presented in abstract form at the 34th Annual Meeting and Scientific Sessions of the Society for Behavioral Medicine, San Francisco, California, 20–23 March 2013.
Competing Interest Statement
The authors have no competing interests to report.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Pre-diabetes in the United States. Atlanta, Ga: U.S. Department of Health and Human Services; 2011. [Google Scholar]
- 2.U.S. Census Bureau. U.S & World Population Clock [article online] Available from http://www.census.gov/popclock/. Accessed 10 December 2013.
- 3.National Diabetes Information Clearinghouse. National diabetes statistics, 2011 [article online] Available from http://www.diabetes.niddk.nih.gov/dm/pubs/statistics. Accessed 10 December 2013.
- 4.Spencer MS, Kieffer EC, Sinco BR, Palmisan G, Guzman RJ, Sherman JA, et al. Diabetes-specific emotional distress among African Americans and Hispanics with Type 2 diabetes. Journal of Health Care for the Poor and Underserved. 2006;17:88–105. doi: 10.1353/hpu.2006.0095. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. African Americans & complications [article online] Available from http://www.diabetes.org/living-with-diabetes/complications/african-americans-and-complications.html. Accessed 10 December 2013.
- 6.U.S. Department of Health and Human Services Office of Minority Health. Diabetes and Hispanic Americans [article online] Available from http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=3&lvlid=62. Accessed 10 December 2013.
- 7.McCollister KE, Zheng DD, Fernandez CA, Lee DJ, Lam BL, Arheart KL, et al. Racial disparities in quality-adjusted life-years associated with diabetes and visual impairment. Diabetes Care. 2012;35:1692–94. doi: 10.2337/dc11-2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myers HF. Ethnicity- and socio-economic status-related stresses in context: an integrative review and conceptual model. J Behav Med. 2009;32:9–19. doi: 10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- 9.Nuru-Jeter A, Williams CT, LaVeist TA. A methodological note on modeling the effects of race: The case of psychological distress. Stress and Health. 2008;24:337–50. [Google Scholar]
- 10.Rod NH, Gronbaek M, Schnohr P, Prescott E, Kristensen TS. Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study. J Intern Med. 2009;266:467–75. doi: 10.1111/j.1365-2796.2009.02124.x. [DOI] [PubMed] [Google Scholar]
- 11.Heraclides A, Chandola T, Witte DR, Brunner EJ. Psychosocial stress at work doubles the risk of type 2 diabetes in middle-aged women: evidence from the Whitehall II study. Diabetes Care. 2009;32:2230–35. doi: 10.2337/dc09-0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Novak M, Björck L, Giang KW, Heden-Ståhl C, Wilhelmsen L, Rosengren A. Perceived stress and incidence of Type 2 diabetes: a 35-year follow-up study of middle-aged Swedish men. Diabet Med. 2013 Jan;30(1):e8–16. doi: 10.1111/dme.12037. [DOI] [PubMed] [Google Scholar]
- 13.Räikkönen K, Matthews KA, Kuller LH. Depressive symptoms and stressful life events predict metabolic syndrome among middle-aged women. Diabetes Care. 2007;30:872–77. doi: 10.2337/dc06-1857. [DOI] [PubMed] [Google Scholar]
- 14.Faulenbach M, Uthoff H, Schwegler K, Spinas GA, Schmid C, Wiesli P. Effect of psychological stress on glucose control in patients with Type 2 diabetes. Diabet Med. 2012;29:128–31. doi: 10.1111/j.1464-5491.2011.03431.x. [DOI] [PubMed] [Google Scholar]
- 15.LeBron AW, Valerio M, Kieffer E, Sinco B, Rosland A-M, Hawkins J, et al. Everyday Discrimination, Diabetes-Related Distress, and Depressive Symptoms Among African Americans and Latinos with Diabetes. J Immigrant Minority Health. 2013:1–9. doi: 10.1007/s10903-013-9843-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bulatao RA, Anderson NB. Understanding Racial and Ethnic Differences in Health in Late Life: A Research Agenda. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 17.Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am J Public Health. 2013;103:e52–60. doi: 10.2105/AJPH.2012.301103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomson EF, Nuru-Jeter A, Richardson D, Raza F, Minkler M. The Hispanic Paradox and Older Adults’ Disabilities: Is There a Healthy Migrant Effect? International Journal of Environmental Research and Public Health. 2013;10(5):1786–1814. doi: 10.3390/ijerph10051786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Payne TJ, Wyatt SB, Mosley TH, Dubbert PM, Guiterrez-Mohammed ML, Calvin RL, et al. Sociocultural methods in the Jackson Heart Study: conceptual and descriptive overview. Ethn Dis. 2005;15:S6–48. [PubMed] [Google Scholar]
- 20.Kohn PM, MacDonald JE. The Survey of Recent Life Experiences: a decontaminated hassles scale for adults. J Behav Med. 1992;15(2):221–28. doi: 10.1007/BF00848327. [DOI] [PubMed] [Google Scholar]
- 21.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96. [PubMed] [Google Scholar]
- 22.Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the life experiences survey. J Consult Clin Psychol. 1978;46(5):932–46. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- 23.Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Thompson J, Smeeding T. Inequality in the Great Recession—The Case of the United States. In: Jenkins SP, et al., editors. Income Inequality and the Great Recession. Oxford University Press; 2012. [Google Scholar]
- 25.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 26.Trento M, Passera P, Tomalino M, Bajardi M, Pomero F, Allione A, et al. Group visits improve metabolic control in type 2 diabetes: a 2-year follow-up. Diabetes Care. 2001;24:995–1000. doi: 10.2337/diacare.24.6.995. [DOI] [PubMed] [Google Scholar]
- 27.Keyserling TC, Samuel-Hodge CD, Ammerman AS, Ainsworth BE, Henriquez-Roldan CF, Elasy TA, et al. A randomized trial of an intervention to improve self-care behaviors of African-American women with type 2 diabetes: impact on physical activity. Diabetes Care. 2002;25:1576–83. doi: 10.2337/diacare.25.9.1576. [DOI] [PubMed] [Google Scholar]
- 28.Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, Sarason B, editors. Social support: Theory, research and applications. The Hague: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- 29.Campos B, Shetter CD, Abdou CM, Hobel CJ, Glynn LM, Sandman CA. Familialism, social support, and stress: Positive implication s for pregnant Latinas. Cultur Divers Ethnic Minor Psychol. 2008;14(2):155–62. doi: 10.1037/1099-9809.14.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Menselson T, Rehkopf DH, Kubzansky LD. Depression among Latinos in the United States: a meta-analytic review. J Consult Clin Psychol. 2008;76:355–66. doi: 10.1037/0022-006X.76.3.355. [DOI] [PubMed] [Google Scholar]
- 31.Haxton CL, Harknett K. Racial and gender differences in kin support: A mixed-methods study of African American and Hispanic couples. J Fam Issues. 2009;30(8):1019–40. [Google Scholar]
- 32.Mallinckrodt B, Armer JM, Heppner PP. A threshold model of social support, adjustment, and distress after breast cancer treatment. J Couns Psychol. 2012;59:150–60. doi: 10.1037/a0026549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Serovich JM, Kimberly JA, Mosack KE, Lewis TL. The role of family and friend support in reducing emotional distress among HIV-positive women. AIDS Care. 2001;13:335–41. doi: 10.1080/09540120120043982. [DOI] [PubMed] [Google Scholar]
- 34.van Son J, Nyklíček I, Pop VJ, Blonk MC, Erdtsieck RJ, Spooren PF, et al. The effects of a mindfulness-based intervention on emotional distress, quality of life, and HbA1c in outpatients with diabetes (DiaMind): A randomized controlled trial. Diabetes Care. 2013;36(4):823–30. doi: 10.2337/dc12-1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marshall RP, Jorm AF, Grayson DA, O’Toole BI. Posttraumatic stress disorder and other predictors of health care consumption by Vietnam veterans. Psychiatric Services (Washington, DC) 1998;49(12):1609–11. doi: 10.1176/ps.49.12.1609. [DOI] [PubMed] [Google Scholar]
- 36.Conroy K, Sandel M, Zuckerman B. Poverty grown up: how childhood socioeconomic status impacts adult health. J Dev Behav Pediatr. 2010;31:154–60. doi: 10.1097/DBP.0b013e3181c21a1b. [DOI] [PubMed] [Google Scholar]
- 37.Belsky J, Pluess M. Beyond diathesis stress: Differential susceptibility to environmental influences. Psychol Bull. 2009;135:885–908. doi: 10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- 38.Shallcross AJ, Troy AS, Boland M, Mauss IB. Let it be: accepting negative emotional experiences predicts decreased negative affect and depressive symptoms. Behaviour Research and Therapy. 2010;48(9):921–29. doi: 10.1016/j.brat.2010.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386–89. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- 40.Hasson RE, Adam TA, Pearson JA, Davis NJ, Spruijt-Metz D, Goran MI. Sociocultural and socioeconomic influences on type 2 diabetes risk in African-American and Latino youth. Journal of Obesity. 2013;512914:1–9. doi: 10.1155/2013/512914. [DOI] [PMC free article] [PubMed] [Google Scholar]


