Abstract
We collected 325 nasal swabs from freshly slaughtered previously healthy pigs from October 2012 through January 2014 in a slaughterhouse near Lomé in Togo. Influenza A virus genome was detected by RT-PCR in 2.5% to 12.3% of the pooled samples, and results of hemagglutinin subtyping RT-PCR assays showed the virus in all the positive pools to be A(H1N1)pdm09. Virus was isolated on MDCK cells from a representative specimen, A/swine/Togo/ONA32/2013(H1N1). The isolate was fully sequenced and harbored 8 genes similar to A(H1N1)pdm09 virus genes circulating in humans in 2012–2013, suggesting human-to-swine transmission of the pathogen.
Keywords: influenza virus, H1N1, pandemic, Togo, swine, interspecies transmission
Introduction
Comparatively little is known about influenza virus circulation in Africa, and even less is known about swine influenza virus on the continent. Before the emergence of the H1N1 pandemic virus in 2009 ([H1N1]pdm09 virus), few investigations into the presence of influenza virus in Africa had occurred. Swine influenza antibodies have recently been detected in Uganda (Kirunda et al., 2014) and in Nigeria (Adeola et al., 2010). Adeola et al isolated swine influenza viruses in Nigeria and showed antigenic cross-reactivity with human H1 and H3 viruses (Adeola et al., 2009). However, no sequence data were available, making the comparison with viruses circulating in other parts of the world difficult.
Subsequent to A(H1N1)pdm09 becoming pandemic in humans it was detected in swine on La Réunion Island in 2009 (Cardinale et al., 2012), in Cameroon in 2010 (Njabo et al., 2012), and in Nigeria in 2010 (Meseko et al., 2014). We carried out a large-scale active surveillance study of animal influenza in Togo from 2009 through 2014 with close to 10 000 avian and swine swabs tested for the presence of influenza virus genome. As observed in the neighboring Benin and Côte d’Ivoire, none of the animal swabs collected in Togo through 2012 had been positive for influenza A virus, nor had any animal serum tested positive for influenza A virus antibodies (Couacy-Hymann et al., 2012). Again from 2011 through 2014, no avian samples tested positive for influenza virus genome or antibody in the 3 countries (Fuller et al., 2014). However in swine, influenza virus genome was detected, demonstrating that influenza activity in the region is not completely absent and likely transient when present.
Material and Methods
We collected 325 nasal swabs from freshly slaughtered pigs in a slaughterhouse near Lomé in Togo. From October 2012 through January 2014, 10 to 42 samples were collected once a month. Each pig was clinically examined prior to slaughter, and none of the pigs showed respiratory symptoms. Trained personnel collected the samples and the study complied with INRA, St Jude Children’s Research Hospital, Laboratoire vétérinaire de Lomé, and international guidelines on animal welfare. The samples were collected in viral transport media as described (Couacy-Hymann et al., 2012) and then stored on ice during sampling and transportation to the laboratory (< 2hours). Swabs were then stored at −80°C in Lomé (Togo), shipped to Toulouse (France) in a dry shipper (−196°C), and stored at −80°C in Toulouse before further processing.
The samples were pooled by 5 (in sampling order: 50 µl aliquots from 5 swabs (5 pigs) per pool tube) to reduce the screening cost. RNA was extracted by using the QIAmp viral RNA minikit (QIAGEN), and influenza A–specific one-step real-time RT-PCR was carried out by using M52C/M253R influenza A primers and the QuantiFast SYBR® Green RT-PCR Kit (QIAGEN) according to the instructions of the manufacturer as previously described (Couacy-Hymann et al., 2012).
Influenza A virus genome was detected in 8 out of 65 positive pools: in samples collected in February, from June through September, and in November 2013. Subtyping real-time RT-PCR assays for HA detected only the A(H1N1)pdm09 virus genes in all the positive pools (WHO, 2009).
The virus isolated from Madin-Darby canine kidney (MDCK, ATCC) cells inoculated with a representative specimen was A/swine/Togo/ONA32/2013(H1N1). The full genome of the isolate was amplified by RT-PCR and sequenced on a 3130XL Applied Biosystems capillary sequencer at the Plateau de Génomique GeT-Purpan, UDEAR UMR 5165 CNRS/UPS, CHU PURPAN, Toulouse, France. The sequences were submitted to GenBank and can be found under the following accession numbers: [KM386876-KM386883].
Results
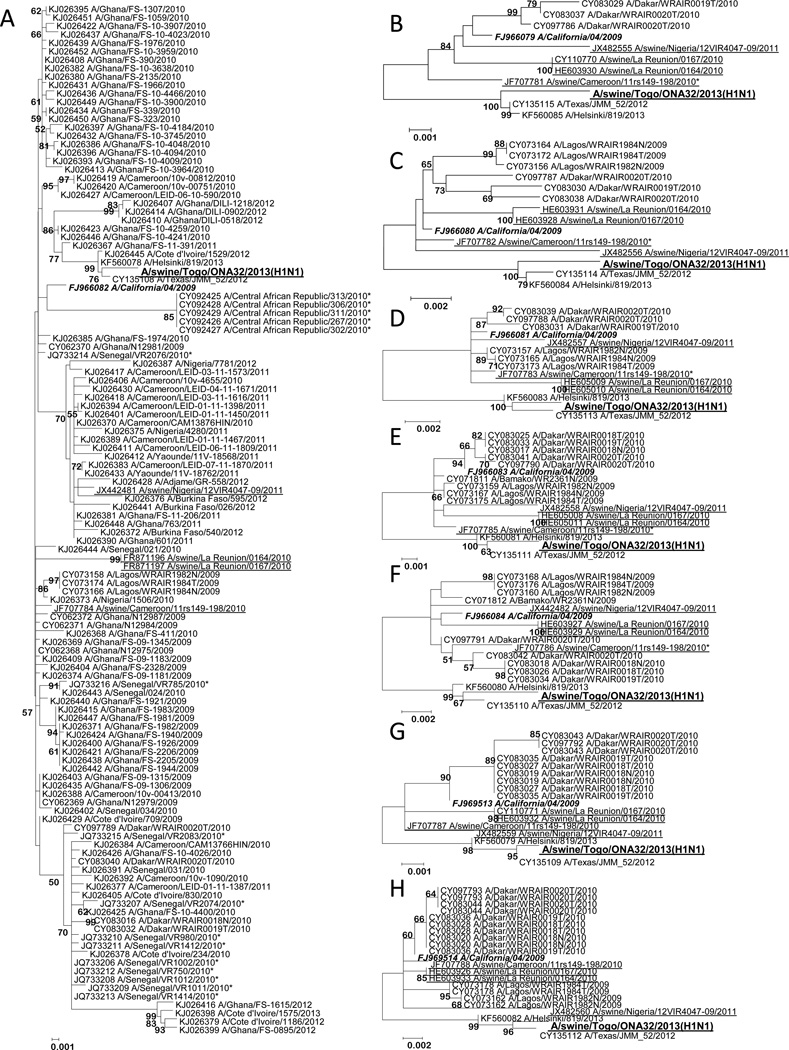
The virus harbored 8 genes clustering with A(H1N1)pdm09 virus genes (Figure). The sequences of A/swine/Togo/ONA32/2013(H1N1) were compared gene-by-gene with those of the closest blast hit for which a full genome was available (A/Texas/JMM_52/2012[H1N1]), with all the sequences from human (H1N1)pdm09 viruses from West and Central Africa available on GenBank, and with all the African swine (H1N1)pdm09 virus sequences available on GenBank. For the 8 genes, A/swine/Togo/ONA32/2013(H1N1) grouped with A/Texas/JMM_52/2012(H1N1) with high supporting bootstrap values (92, 97, 100, 100, 98, 99, 99, and 100 for HA, PB2, PB1, PA, NP, NA, M, and NS, respectively; Figure A to H). Interestingly, the HA gene sequence of A/Côte d’Ivoire/1529/2012 was also closely related to that of A/swine/Togo/ONA32/2013(H1N1) and A/Texas/JMM_52/2012(H1N1) (Figure A). The full genome sequence of this Ivorian strain was not available on GenBank for further comparison. The analysis of molecular markers of drug resistance showed that A/swine/Togo/ONA32/2013(H1N1) is likely sensitive to neuraminidase inhibitors (i.e., it harbors 275H on its NA protein) but resistant to the M2 inhibitors amantadine and rimantadine (i.e., S31N substitution observed on its M2 protein). Unique amino acid mutations (as determined by comparison with all available (H1N1)pdm09 sequences on GenBank) were identified for A/swine/Togo/ONA32/2013(H1N1): Q313H in NA, and S31G in PB1.
Figure. Nucleotide-level, maximum likelihood–derived phylogenetic trees of the 8 gene segments of the A/swine/Togo/ONA32/2013(H1N1) isolate.
Partial gene sequences are indicated with a “*” symbol after the strain name. The gene sequences of A/swine/Togo/ONA32/2013(H1N1) (in large bold font) were compared to all West and Central African human (H1N1)pdm09 sequences available on GenBank, as well as to the closest blast hit for which a full genome was available (A/Texas/JMM_52/2012[H1N1], whose gene segments shared consistently <99.4% identity with A/swine/Togo/ONA32/2013(H1N1) gene segments), to a 2013 representative virus, A/Helsinki/819/2013, and to the recommended vaccine strain (A/California/4/2009[H1N1]) (in bold italic font). Swine viruses are underlined. The number of bootstrap replications was set to 500, and bootstrap values above 50 are labeled on major tree branches for reference. Phylogenetic trees of the A) hemagglutinin (HA); B) polymerase basic 2 (PB2); C) polymerase basic 1 (PB1); D) polymerase acidic (PA); E) nucleoprotein (NP); F) neuraminidase (NA); G) matrix (M); and H) non-structural protein (NS) gene segments are shown.
In conclusion, phylogenetic analyses showed that A/swine/Togo/ONA32/2013(H1N1) was more closely related to (H1N1)pdm09 viruses that were circulating in humans in the region and worldwide in 2012–2013 than to (H1N1)pdm09 viruses circulating in swine, suggesting that human-to-swine transmission of the pathogen occurred.
Discussion
Swine populations have been surveyed every month in Togo since 2009 within the framework of a large-scale animal influenza surveillance project, with no influenza A virus detected in nasal swabs and no influenza A antibodies in swine sera (Couacy-Hymann et al., 2012). We have previously hypothesized that the combination of climate and animal density factors might be responsible for what appeared to be the absence of influenza virus in the backyard sector of Côte d’Ivoire, Benin, and Togo (Couacy-Hymann et al., 2012). Lowen et al, indeed, showed in a laboratory setting and in the guinea pig model that the lower the temperature and relative humidity, the higher the rate of aerosol transmission (Lowen et al., 2007). In addition, Meseko et al detected swine influenza virus in Nigeria throughout the 2 years of their study, with higher isolation rates from November through January, when the dry Harmattan wind is present (Meseko et al., 2014). In the present study, we did not detect significantly more influenza virus in the Harmattan season (November through January in Togo as in Nigeria) than during the rest of the year. This finding could be explained by a much lower animal density in Togo than in Nigeria: 1.2 million tons of pork meat was produced in Africa in 2012, with 10 100 tons in Togo and 249 000 tons in Nigeria (www.faostat.org). Data collected over a longer period of time would be necessary to properly test the seasonality hypothesis. To better assess swine influenza virus prevalence in Togo, a surveillance of younger animals would be informative. In the Nigerian study, 78% of the swine influenza–positive samples were, indeed, from weaners and growing pigs (Meseko et al., 2014), which are thought to be more susceptible to infection; but we tested older pigs sampled at a slaughterhouse.
From October 2010 through January 2014, Togo reported sporadic influenza virus activity in humans to the World Health Organization (WHO). (H1N1)pdm09 was reported in the country in October and November 2010, from February through April 2011 and from June through August 2011, in February and July 2012 and from September through November 2012, and from April through July 2013 and October through December 2013 (WHO). Nzussouo et al reported that (H1N1)pdm09 occurrence in most of West Africa was delayed compared to that of the rest of the world (Nzussouo et al., 2012). The first countries in West Africa to report (H1N1)pdm09 circulation were Côte d’Ivoire in April 2009 and Ghana in August 2009 (WHO). Taken together, these data show (i) circulation of (H1N1)pdm09 virus in humans since at least 2010; (ii) low influenza virus activity (or reporting) without seasonality: a transmission event from human to swine is possible in Togo. The sporadic circulation of (H1N1)pdm09 in humans since 2010 might explain why no swine influenza virus was detected before 2013 in Togo although human-to-swine spillover was observed much earlier in many other countries. The absence of seasonality in human influenza reports in Togo is also in agreement with the irregular occurrence of the disease in swine.
The results of our phylogenetic analyses of A/swine/Togo/ONA32/2013(H1N1) genome suggest a human origin of the virus. Human-to-swine and swine-to-human transmission of influenza virus have been frequently reported (Brockwell-Staats et al., 2009), and proven human-to-swine transmission of (H1N1)pdm09 occurred several times in America at the early stages of the 2009 pandemic (Howden et al., 2009; Pereda et al., 2010; Weingartl et al., 2010). In Cameroon, Larison et al recently studied the virus spillover from human to swine and found that free roaming of pigs is a significant risk factor. They hypothesized that virus transmission to swine may occur via consumption of human feces, which contains infectious particles (Larison et al., 2014). However, this mode of transmission seems relatively unlikely in the Togolese context, swine production in Togo consists of small farms and free range pigs, with little to no importation from abroad, a setup unfavorable for sustained swine influenza virus transmission (Saenz et al., 2006). Taken together, the literature and our phylogenetic analyses results support the hypothesis of human-to -swine transmission of (H1N1)pdm09 in Togo; however, epidemiological studies are warranted to show the transmission route definitively.
Since the (H1N1)pdm09 virus emerged in April-May 2009 in human and swine populations, it has evolved in both hosts. Interestingly, in humans, the virus just underwent a little genetic drift but no significant antigenic drift, and the WHO recommended the same virus strain be used for the seasonal vaccine composition in February 2014 as was used in 2009: A/California/7/2009 (H1N1)pdm09-like virus (WHO). In contrast, (H1N1)pdm09 virus evolved considerably in swine not only with mutations but also with numerous reassortment events. In the United States, co-circulation and multiple reassortments between endemic and pandemic swine influenza viruses have been identified since 2009 (Corzo et al., 2013; Ducatez et al., 2011). These reassortant viruses harbored pandemic matrix and endemic hemagglutinin and neuraminidase gene segments, with diverse combinations for the other 5 gene segments (Ducatez et al., 2011). Since then, swine endemic/pandemic reassortant influenza viruses have worried public health authorities because H3N2 influenza variants (H3N2v) with pandemic matrix gene and swine endemic H3N2 backbone emerged in 2011 and caused sporadic and relatively mild human infections. To date, 340 human cases have been reported (CDC, 2013). (H1N1)pdm09 virus also underwent generic reassortments in European swine populations: Moreno et al identified an H1N2 influenza virus with an endemic swine neuraminidase (N2) gene segment on an (H1N1)pdm09 backbone in 2010 in Italy (Moreno et al., 2011); several pandemic/endemic reassortment events were also found in swine populations in Germany (Lange et al., 2013; Starick et al., 2011; Starick et al., 2012). However, Asia seems to be the continent on which (H1N1)pdm09 has evolved the most, with the first report of a virus harboring a swine Eurasian neuraminidase gene segment on an (H1N1)pdm09 backbone (Vijaykrishna et al., 2010), followed by many other complex reassortment combinations (Liang et al., 2014). The A/swine/Togo/ONA32/2013(H1N1) identified in the current study harbored a pure (H1N1)pdm09 genotype, suggesting that human-to-swine transmission of the pathogen occurred, which is a more likely event than an importation of a swine influenza virus into the country. Surveillance studies need to be continued in the region to better understand the virus transmission and evolution and the interspecies transmission.
Highlights.
-
-
First detection of swine influenza virus in Togo
-
-
2009 H1N1 pandemic influenza virus in pigs in Togo
-
-
Human-to-swine transmission of 2009 H1N1 pandemic influenza virus in Togo
Acknowledgements
This work was supported in part by Contract No. HHSN266200700005C from the U.S. National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, and by the American Lebanese Syrian Associated Charities (ALSAC). We would like to thank Komla Batawui, Lengo kossiwa, Go-Maro Wolali, Pali Magnoudewa, Messan Agbeko, Dogno Koffi, Amindji Amegboh, Agbonon Hypolite, Dackey EdemAlao Funmi, Lengo Kossiwa, Go-Maro Wolali, Dogno Koffi , Pali Magnoudéwa, Kpatina Alfred, Voedjo Koukpealedou, Aketre Yawo, Quentin Langeois, Charlotte Foret, Angélique Teillaud, Josyane Loupias, Brigitte Peralta, Charley Lagarde, Christelle Camus-Bouclainville, Guillaume Croville, Etienne Liais, Renaud Berger, Clément Fage, Florian Grard, and Jean-Benoit Tanis for their excellent technical assistance. We also thank Amanda Ball, James Knowles, Jennifer DeBeauchamp, Jerry Parker, Richard Elia, Pamela McKenzie, and Maureen Tice for help with logistics and data management.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
Conflicts of interest: none.
Authors' contributions
MDF, FA, and RJW designed the study. MDF and FA organized the sample collection. MDF organized the molecular screening, carried out virus isolation and sequencing, and analyzed the data. MDF and RJW drafted the manuscript. All authors read and approved the final manuscript.
Contributor Information
Mariette F. Ducatez, Email: m.ducatez@envt.fr.
Félix Awoume, Email: felixawoume@gmail.com.
Richard J. Webby, Email: richard.webby@stjude.org.
References
- Adeola OA, Adeniji JA, Olugasa BO. Isolation of influenza A viruses from pigs in Ibadan, Nigeria. Veterinaria italiana. 2009;45:383–390. [PubMed] [Google Scholar]
- Adeola OA, Adeniji JA, Olugasa BO. Detection of haemagglutination-inhibiting antibodies against human H1 and H3 strains of influenza A viruses in pigs in Ibadan, Nigeria. Zoonoses and public health. 2010;57:e89–e94. doi: 10.1111/j.1863-2378.2009.01268.x. [DOI] [PubMed] [Google Scholar]
- Brockwell-Staats C, Webster RG, Webby RJ. Diversity of influenza viruses in swine and the emergence of a novel human pandemic influenza A (H1N1) Influenza and other respiratory viruses. 2009;3:207–213. doi: 10.1111/j.1750-2659.2009.00096.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardinale E, Pascalis H, Temmam S, Herve S, Saulnier A, Turpin M, Barbier N, Hoarau J, Queguiner S, Gorin S, Foray C, Roger M, Porphyre V, Andre P, Thomas T, de Lamballerie X, Dellagi K, Simon G. Influenza A(H1N1)pdm09 virus in pigs, Reunion Island. Emerging infectious diseases. 2012;18:1665–1668. doi: 10.3201/eid1810.120398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Situation Summary on Influenza A (H3N2) Variant Viruses (“H3N2v”) 2013 [Google Scholar]
- Corzo CA, Culhane M, Juleen K, Stigger-Rosser E, Ducatez MF, Webby RJ, Lowe JF. Active surveillance for influenza A virus among swine, midwestern United States, 2009–2011. Emerging infectious diseases. 2013;19:954–960. doi: 10.3201/eid1906.121637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couacy-Hymann E, Kouakou VA, Aplogan GL, Awoume F, Kouakou CK, Kakpo L, Sharp BR, McClenaghan L, McKenzie P, Webster RG, Webby RJ, Ducatez MF. Surveillance for influenza viruses in poultry and swine, west Africa, 2006–2008. Emerging infectious diseases. 2012;18:1446–1452. doi: 10.3201/eid1809.111296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducatez MF, Hause B, Stigger-Rosser E, Darnell D, Corzo C, Juleen K, Simonson R, Brockwell-Staats C, Rubrum A, Wang D, Webb A, Crumpton JC, Lowe J, Gramer M, Webby RJ. Multiple reassortment between pandemic (H1N1) 2009 and endemic influenza viruses in pigs, United States. Emerging infectious diseases. 2011;17:1624–1629. doi: 10.3201/1709.110338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller TL, Ducatez MF, Njabo KY, Couacy-Hymann E, Chasar A, Aplogan GL, Lao S, Awoume F, Tehou A, Langeois Q, Krauss S, Smith TB. Avian influenza surveillance in Central and West Africa, 2010–2014. Epidemiology and infection. 2014:1–8. doi: 10.1017/S0950268814003586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howden KJ, Brockhoff EJ, Caya FD, McLeod LJ, Lavoie M, Ing JD, Bystrom JM, Alexandersen S, Pasick JM, Berhane Y, Morrison ME, Keenliside JM, Laurendeau S, Rohonczy EB. An investigation into human pandemic influenza virus (H1N1) 2009 on an Alberta swine farm. The Canadian veterinary journal. La revue veterinaire canadienne. 2009;50:1153–1161. [PMC free article] [PubMed] [Google Scholar]
- Kirunda H, Erima B, Tumushabe A, Kiconco J, Tugume T, Mulei S, Mimbe D, Mworozi E, Bwogi J, Luswa L, Kibuuka H, Millard M, Byaruhanga A, Ducatez MF, Krauss S, Webby RJ, Webster RG, Wurapa K, Byarugaba DK, Wabwire-Mangen F. Prevalence of influenza A viruses in livestock and free-living waterfowl in Uganda. BMC veterinary research. 2014;10:50. doi: 10.1186/1746-6148-10-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange J, Groth M, Schlegel M, Krumbholz A, Wieczorek K, Ulrich R, Koppen S, Schulz K, Appl D, Selbitz HJ, Sauerbrei A, Platzer M, Zell R, Durrwald R. Reassortants of the pandemic (H1N1) 2009 virus and establishment of a novel porcine H1N2 influenza virus, lineage in Germany. Veterinary microbiology. 2013;167:345–356. doi: 10.1016/j.vetmic.2013.09.024. [DOI] [PubMed] [Google Scholar]
- Larison B, Njabo KY, Chasar A, Fuller T, Harrigan RJ, Smith TB. Spillover of pH1N1 to swine in Cameroon: an investigation of risk factors. BMC veterinary research. 2014;10:55. doi: 10.1186/1746-6148-10-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang H, Lam TT, Fan X, Chen X, Zeng Y, Zhou J, Duan L, Tse M, Chan CH, Li L, Leung TY, Yip CH, Cheung CL, Zhou B, Smith DK, Poon LL, Peiris M, Guan Y, Zhu H. Expansion of Genotypic Diversity and Establishment of 2009 H1N1 Pandemic-Origin Internal Genes in Pigs in China. Journal of virology. 2014;88:10864–10874. doi: 10.1128/JVI.01327-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen AC, Mubareka S, Steel J, Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS pathogens. 2007;3:1470–1476. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meseko CA, Odaibo GN, Olaleye DO. Detection and isolation of 2009 pandemic influenza A/H1N1 virus in commercial piggery, Lagos Nigeria. Veterinary microbiology. 2014;168:197–201. doi: 10.1016/j.vetmic.2013.11.003. [DOI] [PubMed] [Google Scholar]
- Moreno A, Di Trani L, Faccini S, Vaccari G, Nigrelli D, Boniotti MB, Falcone E, Boni A, Chiapponi C, Sozzi E, Cordioli P. Novel H1N2 swine influenza reassortant strain in pigs derived from the pandemic H1N1/2009 virus. Veterinary microbiology. 2011;149:472–477. doi: 10.1016/j.vetmic.2010.12.011. [DOI] [PubMed] [Google Scholar]
- Njabo KY, Fuller TL, Chasar A, Pollinger JP, Cattoli G, Terregino C, Monne I, Reynes JM, Njouom R, Smith TB. Pandemic A/H1N1/2009 influenza virus in swine, Cameroon, 2010. Veterinary microbiology. 2012;156:189–192. doi: 10.1016/j.vetmic.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nzussouo NT, Michalove J, Diop OM, Njouom R, Monteiro Mde L, Adje HK, Manoncourt S, Amankwa J, Koivogui L, Sow S, Elkory MB, Collard JM, Dalhatu I, Niang MN, Lafond K, Moniz F, Coulibaly D, Kronman KC, Oyofo BA, Ampofo W, Tamboura B, Bara AO, Jusot JF, Ekanem E, Sarr FD, Hwang I, Cornelius C, Coker B, Lindstrom S, Davis R, Dueger E, Moen A, Widdowson MA. Delayed 2009 pandemic influenza A virus subtype H1N1 circulation in West Africa, May 2009-April 2010. The Journal of infectious diseases. 2012;206(Suppl 1):S101–S107. doi: 10.1093/infdis/jis572. [DOI] [PubMed] [Google Scholar]
- Pereda A, Cappuccio J, Quiroga MA, Baumeister E, Insarralde L, Ibar M, Sanguinetti R, Cannilla ML, Franzese D, Escobar Cabrera OE, Craig MI, Rimondi A, Machuca M, Debenedetti RT, Zenobi C, Barral L, Balzano R, Capalbo S, Risso A, Perfumo CJ. Pandemic (H1N1) 2009 outbreak on pig farm, Argentina. Emerging infectious diseases. 2010;16:304–307. doi: 10.3201/eid1602.091230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saenz RA, Hethcote HW, Gray GC. Confined animal feeding operations as amplifiers of influenza. Vector borne and zoonotic diseases. 2006;6:338–346. doi: 10.1089/vbz.2006.6.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starick E, Lange E, Fereidouni S, Bunzenthal C, Hoveler R, Kuczka A, grosse Beilage E, Hamann HP, Klingelhofer I, Steinhauer D, Vahlenkamp T, Beer M, Harder T. Reassorted pandemic (H1N1) 2009 influenza A virus discovered from pigs in Germany. The Journal of general virology. 2011;92:1184–1188. doi: 10.1099/vir.0.028662-0. [DOI] [PubMed] [Google Scholar]
- Starick E, Lange E, Grund C, Grosse Beilage E, Dohring S, Maas A, Noe T, Beer M, Harder TC. Reassortants of pandemic influenza A virus H1N1/2009 and endemic porcine HxN2 viruses emerge in swine populations in Germany. The Journal of general virology. 2012;93:1658–1663. doi: 10.1099/vir.0.042648-0. [DOI] [PubMed] [Google Scholar]
- Vijaykrishna D, Poon LL, Zhu HC, Ma SK, Li OT, Cheung CL, Smith GJ, Peiris JS, Guan Y. Reassortment of pandemic H1N1/2009 influenza A virus in swine. Science. 2010;328:1529. doi: 10.1126/science.1189132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weingartl HM, Berhane Y, Hisanaga T, Neufeld J, Kehler H, Emburry-Hyatt C, Hooper-McGreevy K, Kasloff S, Dalman B, Bystrom J, Alexandersen S, Li Y, Pasick J. Genetic and pathobiologic characterization of pandemic H1N1 2009 influenza viruses from a naturally infected swine herd. Journal of virology. 2010;84:2245–2256. doi: 10.1128/JVI.02118-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Recommended composition of influenza virus vaccines
- WHO. CDC protocol of realtime RTPCR for influenza A (H1N1) 2009