Abstract
Methamphetamines are the second most commonly used illicit drug worldwide and cost the United States health-care system ∼$23.4 billion annually. Use of this drug affects multiple organ systems and causes a variety of clinical manifestations. Although there are commonly known sequelae of methamphetamine abuse such as “meth mouth,” there is limited evidence regarding maxillary sinus manifestations. The following cases highlight the initial evaluation and management of two methamphetamine abusers with loculated purulent collections within the maxillary sinus as a result of methamphetamine abuse. Our aim was to delineate the otolaryngologic symptoms associated with the patients' methamphetamine abuse. Computed tomography and magnetic resonance imaging studies revealed loculated purulent collections within the maxillary sinus of probable odontogenic origin in both patients. Methamphetamine abuse leading to rampant caries and poor oral hygiene may predispose individuals for craniofacial infections and fluid collections. These cases illustrate the development of maxillary sinusitis and maxilla mucoceles that have been associated with methamphetamine use.
Keywords: Abscess, abuse, cyst, intranasal, maxillary, methamphetamine, odontogenic, route, sinus
Behind cannabis, methamphetamines are the second most commonly used illicit drug worldwide.1 The estimated toll on the United States Health care-system is ∼$23.4 billion annually.2 They affect multiple organ systems and cause a variety of clinical manifestations including cardiac arrhythmias, tachycardia, arousal, hallucinations, euphoria, and increased body temperature.3–5
Methamphetamine-type substances stimulate the central nervous system by modulating dopamine and norepinephrine release and reuptake at nerve terminals.6 These drugs also stimulate α-adrenergic receptors within the salivary gland vasculature, causing vasoconstriction and reduction of salivary flow. Repetitive abuse can therefore result in hyposalivation, ultimately leading to an increase in the retention of cariogenic organisms. Notable sequelae of methamphetamine abuse specific to otolaryngology include dental caries, bruxism, trismus, and nasal septal necrosis and perforation.7–12 However, there is limited evidence regarding craniofacial manifestations. The following case highlights two young female patients who are methamphetamine abusers with maxillary sinus manifestations.
CASE REPORTS
Case 1
A 27-year-old woman presented with a history of intermittent amphetamine use, recurrent facial and sinus fluid collections, and poor dentition. One month before our initial evaluation, she presented to a neighboring emergency department (ED) with similar symptoms. At that time she was diagnosed with a nasal abscess and was discharged without intervention secondary to lack of insurance. After that visit, she experienced a “popping” sensation with subsequent purulent discharge and temporary relief of headaches and sinus pressure.
The patient's symptoms worsened several days later, and she returned to the ED complaining of fever, nausea, frontal headache, sinus pressure, intermittent tinnitus, diplopia, and photophobia. Clear rhinorrhea was evident, the posterior pharynx was mildly erythematous, and the left hard palate showed swelling in the anterior portion. Her urinalysis was positive for opiates and cannabis and her white blood cell (WBC) count was slightly elevated at 10. Magnetic resonance imaging (MRI) and maxillofacial computed tomography (CT) revealed a 31 × 26 ×-34 mm rim enhancing radicular cyst originating from the maxillary second incisor and canine teeth showing restricted diffusion with protrusion into the nasal cavity and incorporation of dental roots, causing alveolar ridge thinning (Fig. 1 panel A). An additional 16 × 12-mm radicular cyst was seen along the left maxillary bone measuring originating from left maxillary second incisor and canine teeth (Fig. 1 panel B). There was associated bone destruction of the alveolar ridge, protrusion into the nasal cavity, and involvement of dental roots most likely odontogenic in origin.
Figure 1.

(Panel A) Axial view of T2 weighted magnetic resonance imaging (MRI) revealed a cystic lesion (3.1 × 2.6 × 3.4 cm) between the nasal cavity and right maxillary sinus with restricted diffusion. The lower part of the cyst involved the palate bone and root of the right maxillary second incisor and canine teeth. Compression causing lateral displacement of the medial wall of the right maxillary sinus was also noted. Another cyst with similar signal characteristics was identified along the left hard palate with the inferior part of the cyst involving the left maxillary second incisor and canine teeth. Both were considered radicular cysts. (Panel B) Coronal computed tomography (CT) scan with right maxillary sinus abscess (2.8 × 2.3 × 2.4 cm) with protrusion into the nasal cavity, incorporation of dental roots, and alveolar ridge thinning (A). Left maxilla abscess (1.7 × 1.4 cm) with associated bone destruction of the alveolar ridge and protrusion into the nasal cavity (B).
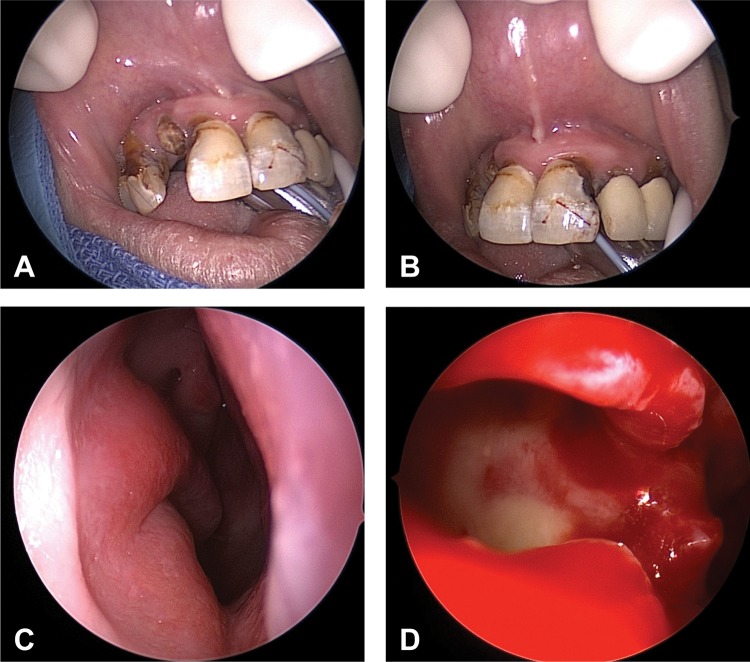
The patient underwent surgery to drain the abscesses. A right medial maxilla inferior antral window, septoplasty, and left inferior antral window were performed given the inferior location of the mucoceles in relation to the natural os. Gross surgical findings included a markedly deviated septum to the left, right medial maxilla bulging into the nasal cavity, marked mucopurulence in the right maxillary sinus, and no evidence of fistula formation from mouth to nose (Fig. 2). Initial intraoperative right maxillary sinus culture revealed 1+ WBC polymorphonuclear cells and 2+ Gram-negative rods. Additional culture results yielded 3+ streptococcus milleri group (anginosus group), 1+ Staphylococcus aureus coagulase positive, and 3+ anaerobic Gram-negative rods β-lactamase positive. Pathological examination showed marked signs of chronic inflammation and fibrosis without evidence of malignancy. The patient made a full recovery from surgery and was seen in follow-up 2 weeks after discharge with no issues.
Figure 2.
(A) Multiple caries are present with significant erosion of the right lateral incisor. (B) Eroding gumline in the central incisors, left lateral incisor, and canine. (C) Endoscopic view of right nasal cavity showing bulging of right maxilla into nasal cavity. (D) Endoscopic view of right maxillary sinus showing mucopurulence after right medial maxilla inferior antral window during maxillary antrostomy.
Case 2
A 21-year-old woman with a history of intravenous heroin use with inhaled methamphetamine use presented to the ED with intermittent right upper molar pain for the past year. She reported an increase in severity of pain a few days before admission with associated right facial swelling. On examination the patient had right facial swelling over her cheek and preauricular region with no erythema or fluctuance. The patient had tenderness to palpation of the right maxillary canine with no periodontal erythema or swelling. No buccal induration or fluctuance was noted bilaterally. Her WBC count was within normal limits and urine toxicology was positive for amphetamines, cannabinoids, and opiates. Maxillofacial CT (Fig. 3) showed a 13-mm hypodense rim-enhancing fluid collection abutting and wrapping around the buccal surface of the maxillae bilaterally. Inflammatory stranding in the soft tissues overlying the maxilla, left cheek, and mandibular region in addition to bilateral retroantral fat pads suggested an abscess of odontogenic origin.
Figure 3.

Hypodense rim-enhancing fluid collection abutting and wrapping around the buccal surface of maxilla bilaterally. There is inflammatory stranding in the soft tissues overlying maxilla, left cheek, and mandibular region and of the bilateral retroantral fat pad.
The patient was given broad-spectrum antibiotics as an inpatient. She was in the process of being evaluated for surgical intervention; however, she left against medical advice to “smoke” therefore was prescribed a short dose of clindamycin.
DISCUSSION
This article describes two cases of patients with known methamphetamine use and maxillary sinus manifestations. Odontogenic manifestations including dental trauma, periodontal disease, and tooth extractions have all been associated with increased risk of maxillary sinusitis.13–15 Both patients were determined to have abscesses of odontogenic origin. The etiology was more apparent in the 27-year-old patient given her poor dentition, periodontal disease, and eroding gumline. These patients' histories of methamphetamine use likely predisposed them to sinus involvement because of the close proximity of the maxillary teeth with the sinus.
Both patients' patterns of methamphetamine abuse, precise duration of use, and route of administration were unknown; however, these variables might have also affected their otolaryngologic manifestations. A previous study with 43 known methamphetamine abusers suggested that intranasal users had worse anterior maxillary dentition compared with those who injected or smoked the drug.16 This phenomenon may be caused by the common blood supply of the anterior maxillary teeth and nasal mucosae via branches of the infraorbital artery.16 Repeated bouts of intranasal methamphetamine could lead to vasoconstriction and subsequent ischemia to the anterior maxillary teeth, given that the abscesses in both patients originated from anterior maxillary rather than posterior maxillary teeth as shown by CT and MRI testing. This may suggest the patients reviewed had a history of intranasal methamphetamine abuse; however, our patients did not present with other common symptoms of intranasal methamphetamine abuse such as anosmia, mucosal atrophy, perforation, or necrosis of nasal septum, dysphagia, and dysphonia.13
Methamphetamine is a sympathomimetic amine that acts on the α-adrenergic receptors of the vasculature of the salivary glands. This causes vasoconstriction and reduced salivary flow, which functions as a buffer to counteract acidity and prevent enamel breakdown.9 Reduced salivary flow is a significant risk factor for caries formation. Deficiency of saliva can lead to prolonged periods of low pH promoting enamel demineralization. It is also known that long-term methamphetamine users admit to not practicing good oral hygiene including brushing their teeth.16 With a lack of plaque control and deficiency of saliva, the mouth becomes a great place for bacteria overproduction, potentially leading to infection, and in these cases, abscess formation.
CONCLUSION
This series represents two patients diagnosed with loculated purulent collections within the maxillary sinus and a history of methamphetamine abuse. The patients' dental caries secondary to their methamphetamine abuse were likely the cause of their abscess development, and physicians should be aware of the craniofacial manifestations for methamphetamine use.
Footnotes
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. United Nations Office on Drugs and Crime. World drug report 2010. 2010. 127 Available online at www.unodc.org/documents/wdr/WDR_2010/World_Drug_Report_2010_lo-res.pdf; accessed March 13, 2014.
- 2. Nicosia N, Pacula RL, Kilmer B, et al. In The Economic Cost of Methamphetamine Use in the United States, 2005. Santa Monica, CA: RAND Corp; Available online at www.rand.org/pubs/monographs/MG829.html; accessed Match 13, 2014. [Google Scholar]
- 3. Boenisch H, Bruess M. The norepinephrine transporter in physiology and disease. In Handbook of Experimental Pharmacology, Vol. 175 Sitte HH, Freissmuth M. (Eds). Heidelberg: Springer Verlag, 485–524, 2006. [DOI] [PubMed] [Google Scholar]
- 4. Cruickshank C, Dyer K. A Review of the clinical pharmacology of methamphetamine. Addiction 104:1085–1099, 2009. [DOI] [PubMed] [Google Scholar]
- 5. Baylen CA, Rosenberg H. A review of the acute subjective effects of MDMA/ecstasy. Addiction 101:933–947, 2006. [DOI] [PubMed] [Google Scholar]
- 6. King G, Ellinwood E. Amphetamines and Other Stimulants. In Substance abuse: A comprehensive textbook, 3rd edition Lowinson JK, Ruiz P, Millman RB, Langdrog JG. (Eds). Baltimore, MD: Williams & Wilkins, 1997. [Google Scholar]
- 7. Bakhshaee M, Khadivi E, Naseri Sadr M, Esmatinia F. Nasal septum perforation due to methamphetamine abuse. Iran J Otorhinolaryngol 25:53–56, 2013. [PMC free article] [PubMed] [Google Scholar]
- 8. Vilensky W. Illicit and licit drugs causing perforation of the nasal septum. J Forensic Sci 27:958–962, 1982. [PubMed] [Google Scholar]
- 9. Curtis EK. Meth mouth: A review of methamphetamine abuse and its oral manifestations. Gen Dent 54:125–129, 2006. [PubMed] [Google Scholar]
- 10. Mooney LJ, Glasner-Edwards S, Rawson RA, Ling W. Medical effects of methamphetamine use. In Methamphetamine Addiction: From Basic Science to Treatment. Roll JM, Rawson RA, Ling W, Shoptaw S. (Eds). New York, NY: Guilford, 117–142, 2009. [Google Scholar]
- 11. Shaner JW. Caries associated with methamphetamine abuse. J Mich Dent Assoc 84:42–47, 2002. [PubMed] [Google Scholar]
- 12. McGrath C, Chan B. Oral health sensations associated with illicit drug abuse. Br Dent J 198:159–162, 2005. [DOI] [PubMed] [Google Scholar]
- 13. Rawson RA, Gonzales R, Marinelli-Casey P, Ang A. Methamphetamine dependence: A closer look at treatment response and clinical characteristics associated with route of administration in outpatient treatment. Am J Addict 14:291–299, 2007. [DOI] [PubMed] [Google Scholar]
- 14. Kretzschmar DP, Kretzschmar JL. Rhinosinusitis: Review from a dental perspective. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96:128–135, 2003. [DOI] [PubMed] [Google Scholar]
- 15. Fagnan LJ. Acute sinusitis: A cost-effective approach to diagnosis and treatment. Am Fam Physician 58:1795–1802, 1998. [PubMed] [Google Scholar]
- 16. Richards JR, Brofeldt BT. Patterns of tooth wear associated with methamphetamine use. J Periodontol 71:1371–1374, 2000. [DOI] [PubMed] [Google Scholar]