Abstract
Background
Skeletal anchorage using dental implants, miniplates, miniscrews and microscrews provides an absolute anchorage for tooth movement. Miniscrew and microscrew implants have many benefits such as ease of placement and removal and immediate orthodontic force application.
Methods
Fifteen subjects in the permanent dentition with an overjet ≥6 mm received treatment with the 0.018-inch pre-adjusted edgewise appliance system (Roth prescription) and extraction of all first premolars. Titanium orthodontic implants were placed in both the upper quadrants and were immediately loaded with elastic chain from the implant head to the sectional arch wire.
Result
The overall success rate of immediate loaded titanium orthodontic micro implants (OMI) in the present study was 83.33%, with a mean chairside time of 15.33 min of placing two implants in each patient. Peri-implant inflammation was the only complication observed. Most failures were in the initial part of the study. There was no significant difference in the success rate of implants based on sex, side of placement (right or left) and type of malocclusion.
Conclusion
The OMIs used in the present study proved to be effective and well tolerated in producing immediate orthodontic anchorage for the retraction.
Keywords: Orthodontic micro implants, Retraction, Anchorage
Introduction
Orthodontic treatment is a complex process, requiring a method that balances the orthodontic biomechanics of an individual patient. Anchorage control is the cornerstone of the orthodontic force system. Anchorage is provided by the teeth that resist the forces of reaction generated by the active components of the appliance. Any unwanted tooth movement must be controlled; else the underlying malocclusion will worsen during tooth alignment.
Anchorage is a challenging aspect of orthodontic treatment. Conventional anchorage methods generally rely on patient compliance, result in unwanted reciprocal tooth movements and are a limiting factor in patients with compromised dentition. In an effort to overcome some of these problems, skeletal anchorage has been increasingly incorporated into orthodontic treatment.
Various forms of sliding mechanics have replaced closing loop arches, with the increased use of pre-adjusted appliance. Sliding mechanics have the benefits of minimal wire-bending time and adequate space for activations. The retraction of four incisors after canine retraction is accepted as a method to minimize the mesial movement of the posterior teeth segment, whereas en masse retraction of six anterior teeth may create anchorage problems. In addition, the tipping action built into anterior brackets in pre-adjusted appliances may produce problems of anchorage. These problems may be overcome to some extent by the use of a transpalatal arch and extraoral appliances. Intraoral anchorage devices may provide inadequate anchorage, whereas extraoral appliances provide a suitable anchorage but are dependent on patient compliance. Skeletal anchorage using dental implants, miniplates, miniscrews and microscrews provides an absolute anchorage for tooth movement. By using microscrew implants in the mechanics of en masse retraction of six anterior teeth, treatment time can be reduced effectively and clinicians can move teeth to satisfy the treatment goal without patient compliance for anchorage devices.
The aim of the present study was to clinically evaluate immediate loading of titanium orthodontic micro implants (OMI) in the maxillary arch for anchorage control for en masse retraction of maxillary anterior segment in conjunction with the pre-adjusted edgewise appliance orthodontic therapy.
The objectives were to study the following aspects of titanium orthodontic micro implants for anchorage control:
-
(i)
The clinical chairside time required for placement of OMI.
-
(ii)
Patient tolerance to the surgical procedure of OMI placement.
-
(iii)
OMI failure, if any.
-
(iv)
Patient tolerance to immediate loading of the OMI.
-
(v)
Ease of removal of the OMI at the scheduled end of therapy.
Material and methods
The subject material consisted of 15 patients seeking orthodontic treatment for correction of protrusion of maxillary anterior teeth. All patients had an overjet ≥6 mm and a minimum age of 12 years at the beginning of treatment (to ensure optimal patient compliance) and no congenitally missing teeth (except for the third molars). There was no history of digit sucking, mouth breathing or previous orthodontic treatment. Maximum anchorage was predicted on the need to restrict mesial movement of posterior teeth so that the excessive overjet could be resolved through complete retraction of the upper anterior teeth en masse.
All patients received treatment with the 0.018-inch Roth prescription pre-adjusted edgewise appliance system and extractions of upper and lower first premolars. Once the initial leveling and aligning was complete, segmental (canine to canine) 0.017 × 0.025-inch stainless steel arch wire, with distal end of arch wire bent mesially (distal to canines), was fixed to engage the elastic chain in the upper arch. Titanium orthodontic implants (1.3 mm in diameter and 8 mm in length) were surgically inserted between the roots of the first molar and the second premolar in both upper quadrants.
All patients were made to rinse with 0.02% chlorhexidine immediately prior to the surgical procedure to reduce the intraoral bacterial load. Topical anesthesia was used prior to infiltration anesthesia to reduce needle prick pain. 0.5 ml of 2% lignocaine with 1:80,000 adrenaline was sufficient for this simple surgical procedure, to insert the Titanium orthodontic implants. The aim was not to achieve profound anesthesia of the teeth, instead get numbness of soft tissue only. It was prudent for the teeth to have some sensitivity, as the patient's complaint of discomfort in the event of bone drill contacting the roots of the teeth would be an indicator to redirect the drill away from the roots.
Speed-reduction contra angle hand piece with constant normal saline irrigation was used to make the original entry into the bone. A round bur (0.9 mm diameter) was used to first make a small indentation on the bony surface. Small indentation on the bone surface prevented slippage of pilot drill. The diameter of the pilot drill end was 1 mm. The drill was used to penetrate the mucosa, attached gingiva and underlying bone without a surgical flap. A slow drill speed (400–500 RPM) with constant normal saline irrigation for reducing the heat and to keep the surgical site lubricated was used. A long hand driver was used for driving the OMI perpendicular to the bone surface.
The OMI's were checked for stability and were immediately loaded with elastic chain from the implant head to the sectional arch wire. The elastic chains were calibrated to deliver 150 g of force on each side, for en masse retraction of the upper anterior teeth. Conventional mechanics were used for the lower arch.
Follow-up appointments were scheduled after 24 h and 7 days of placement of the OMI and subsequently every 3–5 weeks until the desired amount of tooth movement had been achieved. After the space-closure phase, customary orthodontic treatment proceeded without interruption. On achieving appropriate angulation and inclination of teeth and optimum overjet and overbite, debonding and debanding of the cases was done and implants removed. Implant removal was done without the use of local anesthesia, by un-screwing the OMI with the long hand screw driver.
The data were obtained by clinical evaluation of the implants at each appointment and by self-administered questionnaire, for assessment of the patient's perception, level of motivation for and experiences with the OMIs.
Five clinical variables were investigated. The variables were divided into two categories: host factors and environmental management factors. Host factors were related to age, sex and side of screw placement i.e. right or left. Environmental management factors were oral hygiene and inflammation around the screw implants.
Mobility of OMI's was checked with cotton tweezers at each appointment after placement. There were 2 groups: yes (mobile) and no (not mobile) based on the presence or absence of any discernible mobility. If there was any discernible mobility, the screw implant was considered to have failed.
Each patient received a retrospective questionnaire which included a 10-point visual analog scale (VAS) concerning discomfort caused by the OMI surgery, not by the adjustment of the orthodontic appliances. They were asked whether they experienced any of the following forms of discomfort after implantation: pain (time course and intensity), swelling, difficulty in chewing, speech difficulty and difficulty in tooth brushing. The VAS was a 10-cm line with anchors at each end of the line that read “no pain (or discomfort)” (0 cm) and “pain (or discomfort) as much as it could be” (10 cm). Those who experienced pain were asked as to when it occurred: immediately after implantation, after 1 h, at 12 h or between 1 and 14 days.
Results
The present study had 15 patients, 60% were females and 40% males. The mean age of the patients' was 15.05 years (SD ± 2.27). The mean age for females was 14.95 years (SD ± 2.49) and 15.1 years (SD ± 1.84) for males. There was one additional appointment to place two OMIs with a mean chairside time of 15.33 min (SD ± 1.78) for each patient.
Five patients reported swelling at the end of 1 h and only one at the end of 7 days (Fig. 1). Three patients reported difficulty of speech in the first hour after placement of OMI. Only one patient reported difficulty in chewing by the end of 12 h. Five patients reported difficulty in brushing at the end of 12 h and only one continued to have this difficulty at the end of 24 h and after seven days. Five patients complained of pain in the first hour after OMI insertion, of which only one reported pain at the end of 12 h. The highest VAS score at the end of 1 h was 50, with an average of 12. At 12 h after placement of OMI only one had a VAS score of 20.
Fig. 1.
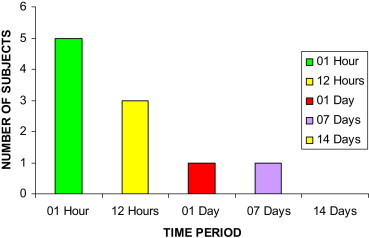
Swelling post OMI insertion.
The overall success rate was 83.33% for all implants with a mean period of force application of 14 months. When the OMI's failed, new ones were placed into a neighboring area. Only one patient had two failed OMIs on the same side. The success rate of OMI's on the right side was 78.95% compared to 88.24% on the left side. The success rate of patients with good oral hygiene was 100%, it was 73% for those with fair oral hygiene and 50% for those with poor oral hygiene. 81.81% of implants succeeded in females compared to 85.71% in males. 90.9% of implants placed in patients with Class I malocclusion succeeded, compared to 80% in Class II division 1 malocclusion. Two implants failed on the first day and four after seven days (Table 1).
Table 1.
Success rate and number of OMI according to clinical variables.
| Clinical variable | Success rate % | Success/total implant (n) |
|---|---|---|
| Oral hygiene | ||
| Good | 100 | 20/20 |
| Fair | 73 | 11/14 |
| Poor | 50 | 1/2 |
| Sex | ||
| Female | 81.81 | 18/22 |
| Male | 85.71 | 12/14 |
| Side of placement | ||
| Right | 78.95 | 15/19 |
| Left | 88.24 | 15/17 |
| Type of Malocclusion | ||
| Class I | 90.9 | 10/11 |
| Class II div 1 | 80.0 | 20/25 |
Avoidance of use of head gear was the most important motivating factor to opt for orthodontic implants with a mean response of 9.23 followed by potential for faster treatment, with a mean response of 8.46 (Table 2).
Table 2.
Pretreatment patient questionnaire: motivating factors (0, least important to 10, most important).
| Motivating factor | Mean response | SD |
|---|---|---|
| To avoid using head gear | 9.23 | 0.64 |
| Potential for faster treatment | 8.46 | 0.80 |
| Potential for better treatment | 8.31 | 1.01 |
| Opportunity to try something new | 8.15 | 1.30 |
| Opportunity to contribute to science | 6.61 | 1.05 |
Fourteen of the fifteen patients found the orthodontic implant “good idea”, none found the head gear “good idea”. One patient found the orthodontic implant “medieval”, whereas 12 patients found the head gear “medieval” (Table 3). During treatment 86.67% patients were glad they got OMI's (Table 4) and after treatment 93.33% patients found that OMI's worked well (Table 5, Figs. 2–4).
Table 3.
Pretreatment patient questionnaire: initial perceptions.
| Descriptive words | Implants | Headgear |
|---|---|---|
| Pretty cool | 13 | 0 |
| Strange | 3 | 11 |
| Medieval | 1 | 12 |
| Cutting edge | 12 | 0 |
| Good idea | 14 | 0 |
Table 4.
During-treatment patient questionnaire.
| Question | Number | % |
|---|---|---|
| Are you glad you got the OMIs? | 13 | 86.67 |
| Do you think the OMIs are working well? | 12 | 80.00 |
| Did it hurt to have the OMIs placed? | 5 | 33.33 |
| Is it more difficult to clean around the OMIs vs the braces? | 5 | 33.33 |
| Have the OMIs hurt during treatment? | 1 | 6.67 |
| Do the OMIs bother you? | 4 | 26.67 |
Table 5.
After-treatment patient questionnaire.
| Question | Number | % |
|---|---|---|
| Do you think the OMIs worked well? | 14 | 93.33 |
| Are you glad you got the OMIs? | 13 | 86.67 |
| Did you enjoy participating in the study? | 14 | 93.33 |
| Did removing the OMIs hurt? | 2 | 13.33 |
Fig. 2.

a: Pre-treatment extraoral photographs, b: Post-treatment extraoral photographs.
Fig. 3.
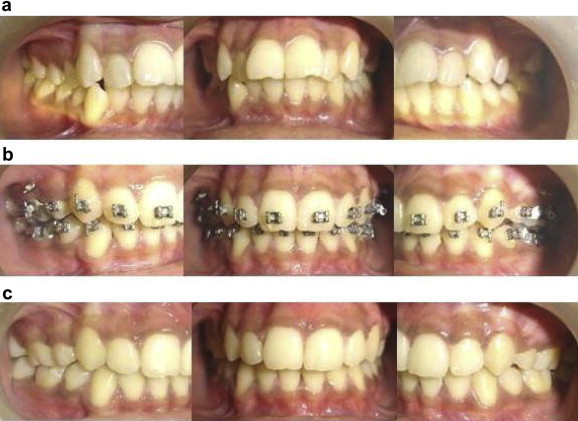
a: Pre-treatment intraoral photographs. b: Intra-treatment with OMI in situ. c: Post-treatment intraoral photographs.
Fig. 4.
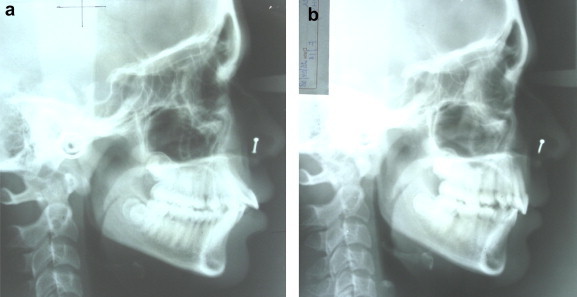
a: Pre-treatment lateral cephalogram, b: Post-treatment lateral cephalogram.
Discussion
Anchorage has been a concern among orthodontists and has created many problems in this field. This problem has arisen because appliances are in balance, meaning that two objects connected by active appliances are subject to equal and opposite forces. Intraoral and extraoral appliances have been used to fulfill the anchorage requirement, but because of side effects and compliance issues, new methods such as implants have been developed to obtain effective anchorage.1 Although, implants do not present the side effects and compliance issues presented by other techniques, they have to be stable and capable of resisting forces that act on the teeth.2
In the present study there was one additional appointment and a mean chairside time of 15.33 min (SD ± 1.78) taken to place two OMI's in a patient, thus the procedure can be conducted at any Armed Forces Orthodontic center without placing additional burden on the resources in terms of additional clinical time of such centers.
The overall success rate in this study of the OMI's was 83.33%, it was higher than the 37.0% reported by Kim and Choi,3 70% by Fritz et al,4 78.6% by Moon,5 and 70.73% reported by Garfinkle et al.6 It was similar to the success rate of 83.9%–85.0% reported by Miyawaki et al,7 81.1% by Kuroda et al,8 and 83.8% by Moon et al.9 However, it was lower than the 80.0%–93.6% reported by Park et al10 and 85.7% by Chen et al.11
All six OMI's failures in this study occurred within two weeks of placement. This was shorter than 1.65 months of Moon et al9 and 3.40 months of Park et al.10 In this study, four of the six failed implants were in the first five patients. In addition, the OMI success rate tended to increase over time from the beginning of the study; this finding indicated a learning curve for the clinician.
Males had a higher success rate than females in the present study, but this was statistically not significant (Table 6). The studies of Moon et al,9 Park et al10 and Miyawaki et al7 have also noted in their studies that sex was not related to the clinical success of the OMI.
Table 6.
Success rate and number of OMI according to clinical variables.
| Clinical variable | Success rate % | Success (n) | Total implant (n) | Significance (chi-square or Fisher exact) |
||
|---|---|---|---|---|---|---|
| Chi-sqr | p value | Outcome | ||||
| Sex | ||||||
| Female | 81.81 | 18 | 22 | 1.1799 | 0.2774 | No difference in success rate between male and female |
| Male | 85.71 | 12 | 14 | |||
| Side of placement | ||||||
| Right | 78.95 | 15 | 19 | 0.5573 | 0.4554 | No difference in success rate between two sides |
| Left | 88.24 | 15 | 17 | |||
| Type of malocclusion | ||||||
| Class I | 90.90 | 10 | 11 | 0.6020 | 0.4378 | No difference in success rate by type of malocclusion |
| Class II div 1 | 80.00 | 20 | 25 | |||
In the present study the success rate of OMI's was better in the over 15 year age group. This was similar to that reported by Park et al,12 who have postulated that the under 15-year-old patient group suffered a lower success rate than the over 15-year-old patient group because they had thin cortical bone and poor bone quality. Park13 insisted that the success rate for the under 20 age group was higher than that of the over 20 age group, but Miyawaki et al7 stated that there was no significant difference in the success rates of the under 20 age group, 20–30 age group and the over 30 age group.
The success rate of OMIs for the left side was higher compared to that on the right side in the present study, but this was statistically not significant (Table 6). The results of the present study were in agreement with the results of Moon et al9 who found no difference in the success rate on either the right or left side. This is not in agreement with the results of Park et al10 who reported that the left side had a significantly higher success rate than the right side. In our opinion, if the OMIs were properly placed in the attached gingiva according to the protocol and if the oral hygiene was well maintained, the chances of soft tissue inflammation around the OMI could be decreased. Therefore, there would be no difference in the success rate between the right and left sides.
In this study three patients reported difficulty of speech in the first hour after placement of OMI. Only one patient reported difficulty in chewing by the end of 12 h. Five patients reported difficulty in brushing at the end of 12 h and only one patient continued to have this difficulty at the end of 24 h and seven days.
The patients already had the orthodontic appliance in situ at the time of placement of OMI; the atraumatic technique of OMI insertion and the small size of the OMI contributed better adaptability and fewer problems for the patient.
Placement, use and retrieval of the OMIs were generally well tolerated procedures. Only two patients reported using over-the-counter post placement analgesics, indicating the highest reported VAS score of 50 and an average of 12 (on a VAS scale of 1–100), as not too severe a pain experience. No patient accepted the offer of local anesthesia before removal of the OMIs.
In most orthodontic treatments, pain generally increases with time, according to measurements at 4 and 24 h and then decreases to normal levels of sensation 7 days after treatment.14–18 A pain assessment of 40–50 on the 100-point VAS scale was shown 1 day after orthodontic treatment.14 Thus, the discomfort is not more with OMI's than with orthodontic treatment.
The patients were pleased with the tangible orthodontic results, 93.33% thought that OMI's worked well. This is in accordance with Koruda & Yamada [19], who have concluded that orthodontic treatment with miniscrew anchorage is simpler and more useful than that with traditional anchorage mechanics.
In the present study, none of the OMI's fractured during placement and removal. Peri-implant inflammation was the only complication observed in the present study. The results of the present study are encouraging and should prove helpful to both clinicians and patients considering OMIs.
In conclusion the overall success rate of immediate loaded titanium OMI's in the present study was 83.33%, with a mean chairside time of 15.33 min for placing two implants in each patient. Peri-implant inflammation was the only complication observed. Most failures were in the initial part of the study. There was no significant difference in the success rate of implants based on sex, side of placement (right or left) and type of malocclusion. OMI's were better tolerated in the above 15 age group. Therefore, OMIs can be used for orthodontic anchorage predictably and consistently in routine orthodontic practice.
To minimize failure, clinicians should attempt to reduce inflammation around the implants. Clinicians should expect to experience a learning curve. The OMIs used in the present study proved to be widely accepted, effective and well tolerated in producing immediate orthodontic anchorage for the retraction.
Conflicts of interest
All authors have none to declare.
Acknowledgment
This paper is based on Armed Forces Medical Research Committee project No. 3757/2007 granted by the office of the Directorate General Armed Forces Medical Services and Defence Research Development Organisation, Government of India.
References
- 1.Costa A., Raffaini M., Melsen B. Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg. 1998;13:201–209. [PubMed] [Google Scholar]
- 2.Favero L., Brollo P., Bressan E. Orthodontic anchorage with specific fixtures: related study analysis. Am J Orthod Dentofac Orthop. 2002;122:84–94. doi: 10.1067/mod.2002.124870. [DOI] [PubMed] [Google Scholar]
- 3.Kim Y.H., Choi J.H. The study about retention of miniscrews used for intraoral anchorage. J Korean Dent Assoc. 2001;39:684–687. [Google Scholar]
- 4.Fritz U., Ehmer A., Diedrich P. Clinical suitability of titanium microscrews for orthodontic anchorage-preliminary experiences. J Orofac Orthop. 2004;65:410–418. doi: 10.1007/s00056-004-0408-x. [DOI] [PubMed] [Google Scholar]
- 5.Moon C.H. vol. 3–4. Narae Publishing Inc; Seoul: 2002. (Clinical Use and Failure of Skeletal Anchorage System). 14–79. [Google Scholar]
- 6.Garfinkle J.S., Cunningham L.L., Beeman C.S., Kluemper G.T., Hicks E.P., Kimf M.O. Evaluation of orthodontic mini-implant anchorage in premolar extraction therapy in adolescents. Am J Orthod Dentofac Orthop. 2008;133:642–653. doi: 10.1016/j.ajodo.2006.04.053. [DOI] [PubMed] [Google Scholar]
- 7.Miyawaki S., Koyama I., Inoue M., Mishima K., Sugahara T., Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofac Orthop. 2003;124:373–378. doi: 10.1016/s0889-5406(03)00565-1. [DOI] [PubMed] [Google Scholar]
- 8.Kuroda S., Sugawara Y., Deguchi T., Kyung H.M., Yamamotoc T.T. Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfort. Am J Orthod Dentofac Orthop. 2007;131:9–15. doi: 10.1016/j.ajodo.2005.02.032. [DOI] [PubMed] [Google Scholar]
- 9.Moon C.H., Lee D.G., Lee H.S., Im J.S., Baek S.H. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod. 2008;78:101–106. doi: 10.2319/121706-515.1. [DOI] [PubMed] [Google Scholar]
- 10.Park H.S., Jeong S.H., Kwon O.W. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofac Orthop. 2006;130:18–25. doi: 10.1016/j.ajodo.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 11.Chen C.H., Chang C.S., Hsieh C.H. The use of microimplants in orthodontic anchorage. J Oral Maxillofac Surg. 2006;64:1209–1213. doi: 10.1016/j.joms.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 12.Park Y.C., Kim J.K., Lee J.S. Shin Hung International; Seoul: 2005. (Atlas of Contemporary Orthodontics). 01–104:145–161. [Google Scholar]
- 13.Park H.S. Clinical study on success rate of microscrew implants for orthodontic anchorage. Korea J Orthod. 2003;33:151–156. [Google Scholar]
- 14.Bergius M., Berggren U., Kiliaridis S. Experience of pain during an orthodontic procedure. Eur J Oral Sci. 2002;110:92–98. doi: 10.1034/j.1600-0722.2002.11193.x. [DOI] [PubMed] [Google Scholar]
- 15.Erdinc A.M., Dincer B. Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod. 2004;26:79–85. doi: 10.1093/ejo/26.1.79. [DOI] [PubMed] [Google Scholar]
- 16.Leavitt A.H., King G.J., Ramsay D.S., Jackson D.L. A longitudinal evaluation of pulpal pain during orthodontic tooth movement. Orthod Craniofac Res. 2002;5:29–37. doi: 10.1034/j.1600-0544.2002.01158.x. [DOI] [PubMed] [Google Scholar]
- 17.Firestone A.R., Scheurer P.A., Burgin W.B. Patients' anticipation of pain and pain-related side effects and their perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1999;21:387–396. doi: 10.1093/ejo/21.4.387. [DOI] [PubMed] [Google Scholar]
- 18.Sergl H.G., Klages U., Zentner A. Pain and discomfort during orthodontic treatment: causative factors and effects on compliance. Am J Orthod Dentofac Orthop. 1998;114:684–691. doi: 10.1016/s0889-5406(98)70201-x. [DOI] [PubMed] [Google Scholar]
- 19.Kuroda S., Yamada K. Class II malocclusion treated with miniscrew anchorage: comparison with traditional treatment mechanics outcomes. Am J Orthod Dentofacial Orthop. 2009;135:302–309. doi: 10.1016/j.ajodo.2007.03.038. [DOI] [PubMed] [Google Scholar]


