Abstract
The putative causes of bruxism are multifactorial and there are no definite measures for bruxism management. The aim of this study was to evaluate the efficacy of biofeedback therapy on sleep bruxism, compared with occlusal splint. Twenty-four volunteers with sleep bruxism were divided into two groups: the GTB group that were treated with biofeedback therapy (n = 12) and the GTO group that were treated with occlusal splint (n = 12). A mini pressure sensor integrated with a monitoring circuit by use of a maxillary biofeedback splint was fabricated. To foster the relaxation of the masticatory muscles and the nervous system, the wireless device received signals from bruxism events and vibrations alerted the bruxer when the threshold was exceeded. Total episodes and average duration of bruxism events during 8 hours of sleep were analyzed with the monitoring program (TRMY1.0). After 6 and 12 weeks, the episodes (P = 0.001) and duration (P < 0.05) in the GTB group declined dramatically. In contrast, there were no significant differences in the GTO group after the treatment (P > 0.05). Furthermore, the episodes had significant differences between the GTB group and the GTO group after the same period of treatment (P = 0.000). The results suggest that biofeedback therapy may be an effective and convenient measure for mild bruxers, when compared with occlusal splint therapy. The mini wireless biofeedback method may be of value for the diagnosis and management of bruxism in the future.
Keywords: sleep bruxism, biofeedback, occlusal splint, miniaturization, vibration, wireless technology
Introduction
Bruxism is an oral parafunction characterized by clenching and grinding of teeth during wakefulness or sleep. Awake bruxism (AB), often known as tooth clenching, is mainly associated with anxiety, life stress including work pressure and family responsibilities[1]-[4], and a number of psychopathological symptoms[5]. In geriatric patients, awake bruxism is frequently observed in frontotemporal dementia, and normal pressure hydrocephalus which characteristically shows frontal lobe dysfunction and can be regarded as a frontal neurological sign of various disorders[6]. Sleep bruxism (SB), which mostly occurs during night, is an oromandibular behavior defined as a stereotyped movement characterized by tooth grinding and/or clenching[7],[8]. According to the International Classification of Sleep Disorders Version 2 (ICSD-2), SB is classified as a sleep related movement disorder usually associated with sleep arousals[9]. Both AB and SB may be also associated with various movements and degenerative disorders, such as oromandibular dystonia and Huntington's disease[10].
The prevalence of SB in the adult population is estimated to be approximately 8–10%[11]. The major negative impacts of bruxism on health include tooth attrition and destruction[12]; risk factors associated with increased mechanical and/or technical complications in prosthodontic rehabilitation[13]; contribution to (not simple cause-effect relationship) chronic masticatory myofascial pain[14],[15]; exacerbation of temporomandibular disorders or induction of temporal tension headache; grinding sounds that may interfere with the sleep of family or life partners[16],[17].
Generally speaking, the putative etiology of SB has multiple factors including genetic factors, some drugs and medications, psychosocial factors, and central nervous system or combined factors[18],[19]. Information about genetic predisposition to SB stems mostly from studies based on questionnaires or analyses of monozygotic twin populations, some drugs (alcohol, caffeine, and tobacco) and medications (e.g., selective serotonin re-uptake inhibitors, benzodiazepines, and dopaminergic drugs), which have relationship with the etiopathogenesis of SB[20]. At present, sleep arousal, autonomic sympathetic-cardiac activation, neurotransmitters and other central factors play major roles in the genesis of SB. Psychosocial components, such as anxiety and stress may be risk factors for SB[21]. Treatment modalities for bruxism involve reversible occlusal correction, behavioral changes and pharmacological approaches[22]. The most common method of reversible occlusal adjusting for many bruxers is the use of occlusal appliance. However, the inherent effect of an occlusal splint has been found to be the protection of tooth wear rather than the alleviation of bruxism behavior itself[23]. One of the behavioral approaches is the biofeedback method for bruxism; the efficacy has been reported by many researchers. The majority of these devices rely on electromyography (EMG) of the masticatory muscles[24],[25].
However, there are some disadvantages of EMG biofeedback devices, i.e., the EMG signals can be affected by electrode position, posture and skin resistance. It is also difficult for bruxers to tolerate the device well while asleep with the electrodes attached on masseter and/or temporalis muscles[26]. So far, there is no approach that is effective for bruxism management. The purpose of this study is to evaluate the efficacy of biofeedback therapy on SB via a mini wireless biofeedback device contrasted with occlusal splint. We sought to determine whether the awareness of clenching or grinding of teeth can alleviate the episodes of bruxism behavior itself after several weeks of training and learning in bruxers.
Materials and methods
Mini wireless biofeedback device
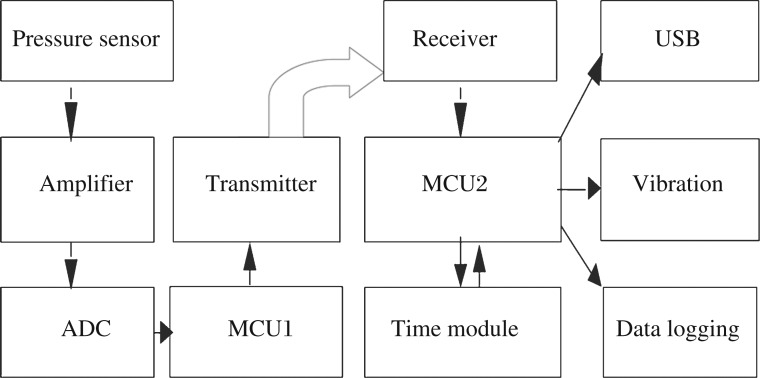
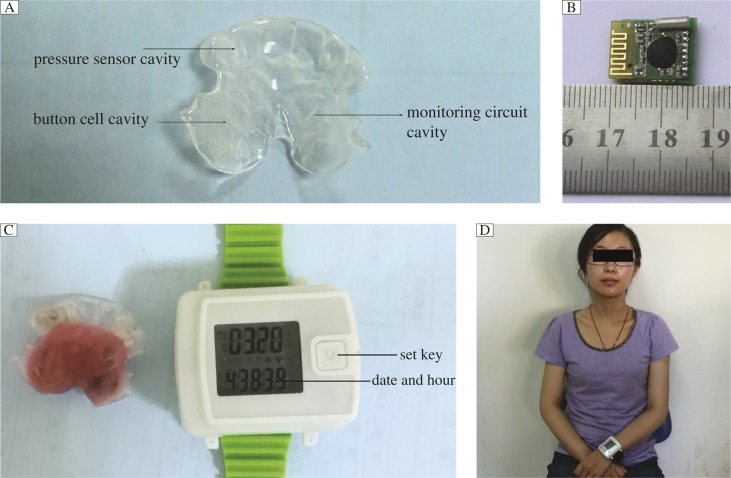
The configuration of the proposed system used for monitoring and vibration is shown in Fig. 1. The pressure sensor (HU-101, SaiYing Electronics Technology Development Inc. Bengbu, China) was embedded 0.5–1 mm below the surface of a maxillary biofeedback splint (Jing Yi Denture Co. Ltd., Nanjing, China) at the point contacted by the mandibular canine in the intercuspal position. A stabilization splint, which covers the maxillary or mandibular full dental arch, is rather large[11],[27]. In consideration of the bruxer's comfort, the design of a biofeedback splint (Fig. 2A) is different from a traditional anterior or stabilization splint. An anterior splint is small and covers some of the anterior teeth. Because the button cell (CR2025, Panasonic, Indonesia, 20 mm×2.5 mm) and mini monitoring circuit (18 mm×16 mm×5 mm, Fig. 2B) are designed to be packed into the splint, it is essential to extend the margin of the splint to the lingual surface of bilateral maxillary premolars.
Fig. 1. The mini wireless biofeedback system.
The signals were transformed from the analog-to-digital converter (ADC) to microcontroller unit (MCU1 and MCU2, MSP430F4152, Texas Instrument, USA), which has ultra lower power consumption with active mode of 200 μA, 1 Mhz and 2.2 v.
Fig. 2. Mini wireless biofeedback device.
A: The margin of the biofeedback splint extends to the lingual surface of the bilateral maxillary second premolars. The cavity design for placement of the pressure sensor, monitoring circuit and button cell. B: Mini-monitoring circuit (18 mm×16 mm×5 mm). C: A maxillary biofeedback splint with pressure sensor, monitoring circuit and button cell embedded(left), a watch style vibration device (right). D: A bruxer with the maxillary biofeedback splint for monitoring and the wireless vibration device. Use of photo was permitted by the study subject.
The wireless transmitter sent the signals of bruxism events per second and the signals were received by a watch style device. When the value exceeded the threshold, as clenching or grinding of teeth occurred during sleep, the watch vibrated to inform the bruxer of the abnormal movement of teeth and induce voluntary relaxation of the masticatory muscles and nervous system (Fig. 2C and 2D).
Software for analysis of bruxism events
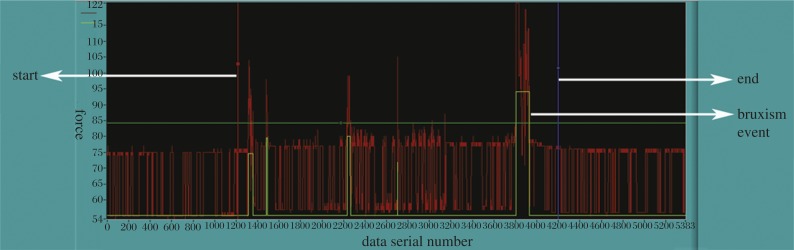
The software (TRMY 1.0, Nanjing Jing Tong Ren Biological Technology Co., Ltd, Nanjing, China) was developed in Labwindows 8.5 (National instruments, USA). The analysis of bruxism events through the USB of the vibration device included the value of bite force, the occurring time (year/month/day/hour/minute/second) and the duration in specific intervals, as showing in Fig. 3.
Fig. 3. A result sample of monitoring device.
The irregular red lines demonstrate bite forces during sleep, the area between a red and blue line (the white arrow) is the interval for analysis, the green rectangles represent episodes of bruxism events.
Validation of the mini wireless biofeedback device
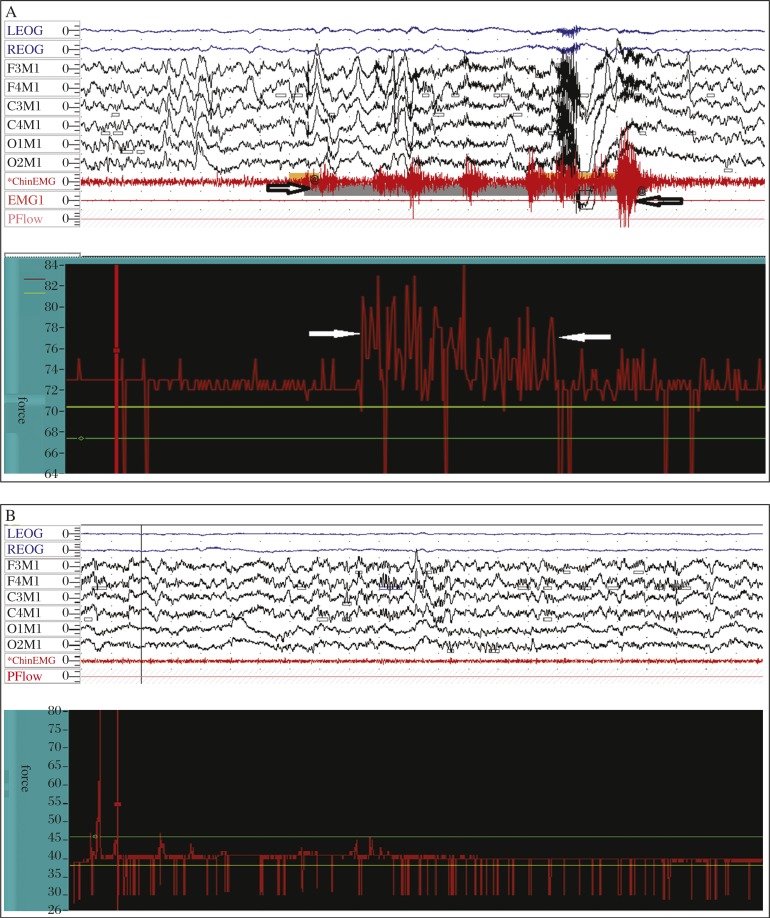
The patent of the mini biofeedback device was approved by State Intellectual Property Office of China in 2012[28]. For evaluating the validity of the device, the authors simultaneously compared the device with polysomnography (PSG, Alice 5 Diagnostic Sleep System, Philips Respironics. Inc, USA) in bruxers. The PSG was provided by the Department of Oral and Maxillofacial Surgery, Affiliated Hospital of Stomatology, Nanjing Medical University. The sensitivity was 88.1% and the specificity was 84.5% in detection of bruxism events (Fig. 4A and 4B) (109 detections for PSG and 96 detections of bruxism events for monitoring device. Bruxism was diagnosed as previously described[21],[29]).
Fig. 4. The images of polysomography (PSG) and the monitoring device.
A: The comparison of a polysomography and the monitoring device; the PSG demonstrates a bruxism event, which consisted of a series of EMG activities, with the amplitude reaching 20% maximum voluntary contraction (MVC), and the duration is more than 2 seconds. In contrast, the monitoring device demonstrates a series of serrations with the amplitude of force exceeding 20% of the maximum bite force (relative to the baseline) during intercuspal position and the duration was no less than 3 seconds. B: Demonstration of the EMG amplitude of masseter muscle during sleep with no remarkable changes, while the monitoring device also presented the baseline value of bite force without significant changes during sleep simultaneously.
Experiment protocol subjects
Twenty-four outpatients with a diagnosis of SB were recruited between December 2011 and May 2013 from the Department of General Dentistry, Affiliated Hospital of Stomatology, Nanjing Medical University. The subjects were assignedto the GTB group (9 females, 3 males, mean age 26.6±5.0 years) and the GTO group (10 females, 2 males, mean age 24.7±5.5 years) using a random number table.
The inclusion criteria were: bruxers between the ages of 20–40 years, > six month history of bruxism (according to American Academy of Sleep Medicine (AASM) clinical diagnostic criteria for SB[21]) which was confirmed by clinical examination and bed-partner or families and no history of psychological and neurotic diseases. Patients undergoing treatment for temporomandibular disorders and patients with organic nerve disease were excluded from the experiment. Excluded treatments included botulinum toxin injection and/or use of other drugs to reduce masseter and temporalis muscle hyperactivity because of some effects that are similar with biofeedback therapy for management of bruxism and may interfere with the results of this study. Enrollment of participants and the experimental procedures in this study were conducted in accordance with the Declaration of Helsinki (revised in Edinburgh 2000). All subjects signed an informed consent form to participate in a protocol that had been approved by the Ethics Committee of Affiliated Hospital of Stomatology, Nanjing Medical University.
Experimental procedure
Dental impressions for each of the participants in GTB and GTO were taken for manufacturing the maxillary biofeedback splint designed as Fig. 2A. A baseline of episodes, duration, and a biting force value for each bruxer was determined without vibration during the first three nights by setting the threshold to the maximum. The threshold was set to a normal value, which was determined by using the mean value of the biting force, calculated in specific intervals (e.g., one minute, one hour and 8 hours) via TRMY 1.0, and the duration of ≥ 3s[30]. When the threshold was exceeded, the bruxers in the GTB group would become conscious of clenching or grinding of teeth during sleep and relax themselves via alleviating the tension of the masticatory muscles and nervous system. In contrast, the GTO group were treated with a maxillary biofeedback splint without vibration by setting the threshold to the maximum value during the treatment period. Six and 12 weeks after therapy in each group, the episodes and duration of bruxism events were monitored and recorded again by use of the mini wireless monitoring device during 8 hours of sleep for data collection.
Statistical analysis
The total episodes and durations of bruxism events during 8 hours of sleep were analyzed after 6 and 12 weeks of therapy. Within each group, the difference between pre- and post-treatment, and the efficacy of biofeedback therapy versus occlusal splint treatment between GTB and GTO were assessed by univariate ANOVA. The multiple comparisons of the post-hoc test were performed with Tukey HSD test to determine which groups had significant differences between and within GTB and GTO in SPSS version 19.0 (IBM SPSS Statistics, Chicago, IL, USA). A probability value of P < 0.05 was considered statistically significant.
Results
Total episodes and duration of bruxism events in GTB and GTO at the beginning
The average total episodes of bruxism events during 8 hours of sleep were 10.2±2.8 (range, 7 to 16) times in GTB at the beginning. In GTO, the average total episodes of bruxism events were 11.9±5.7 (range, 4 to 21) times. The duration of bruxism events in GTB ranged from 5 to 40 seconds (mean,17.3±9.6 s). In GTO, the duration ranged from 6 seconds to 24 s; the average duration was 14.8±5.5 seconds. There were no significant differences between GTB and GTO, both in total episodes (P = 0.883) and duration of bruxism events (P = 0.907). For the occurrence times, bruxism events were observed throughout the sleep.
Efficacy of GTB and GTO after 6 and 12 weeks of therapy
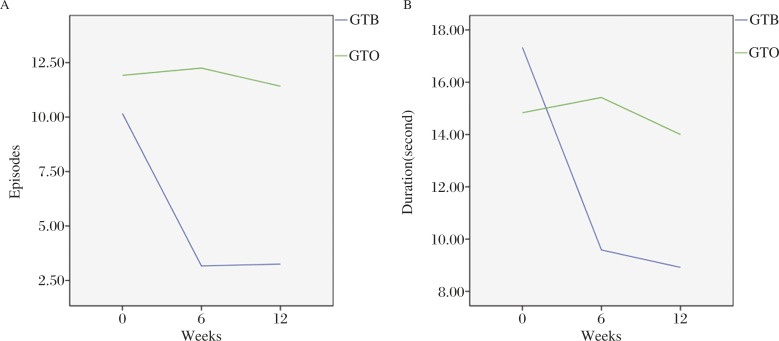
The total episodes and duration in GTB and GTO, before, after 6 and 12 weeks of therapies are illustrated in Fig. 5A and Fig. 5B. The differences in episode and duration before and after in GTB had statistical significance (episodes P = 0.001, duration P = 0.026 and 0.012 respectively). However, there were no significant differences in GTO comparing bruxism events at the baseline with 6 and 12 weeks after occlusal splint therapy (all P>0.05).
Fig. 5. Efficacy of GTB and GTO after 6 and 12 weeks of therapy.
A: The total episodes in GTB declined dramatically from the beginning to the end of 6 and 12 weeks after biofeedback therapy (P = 0.001), while there are no significant differences in GTO (6 weeks, P = 0.998. 12 weeks, P = 0.970). B: The duration in GTB has significant difference between 6 and 12 weeks after biofeedback therapy compared to baseline (6 weeks, P = 0.026, 12wks, P = 0.012), while similar results cannot be found in GTO (P = 0.999).
As shown in Table 1, post 6 and 12 weeks of therapy, the total episodes of bruxism events during 8 hours of sleep in GTB were (3.2±1.2) times and (3.3±1.4) times. The episodes in GTO were (12.3±6.0) times and (11.4±3.7) times, and there were significant differences between GTB and GTO (all P = 0.000) after therapy. The average duration of bruxism events in GTB was (9.6±3.2) seconds and (8.9±2.7) seconds, and the duration in GTO was (15.4±6.0) seconds and (14.0±6.1) s. There were no significant differences (P = 0.172 and P = 0.305) comparing GTB with GTO. Furthermore, there were no significant differences of episodes and duration between 6 and 12 weeks in GTB and GTO (all P>0.05) after biofeedback and occlusal splint therapy.
Table 1. Total episodes and duration of bruxism events during 8 hrs sleep before, 6 and 12 weeks after.
| n | Before | 6 weeks | 12 weeks | F | P | Before | 6 weeks | 12 weeks | F | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Episodes (times) | duration (second) | ||||||||||
| GTB | 12 | 10.2±2.8 | 3.2±1.2 | 3.3 ±1.4 | 14.44 | 0.00 | 17.3±9.6 | 9.6±3.2 | 8.9±2.7 | 3.83 | 0.004 |
| GTO | 12 | 11.9±5.7 | 12.3±6.0 | 11.4±3.7 | 14.8±5.5 | 15.4±6.0 | 14.0±6.1 | ||||
Tukey HSD test, within GTB, 6 weeks vs. before: episodes p = 0.001, duration P = 0.026. 12 weeks vs. before: episodes p = 0.001, duration p = 0.012. Within GTO, 6 weeks vs. before: episodes P = 0.998, duration P = 0.999.12 weeks vs. before: episodes p = 0.970, duration p = 0.999. Between GTB and GTO, 6 weeks: episodes P = 0.000, duration p = 0.172. 12 weeks: episodes p = 0.000, duration P = 0.305.
Sleep quality in GTB and GTO
Pittsburgh Sleep Quality Index (PSQI)[31] is a useful instrument in measuring sleep quality. The sleep quality of each subject was evaluated by PSQI based on the bruxer's self-report. Two in GTB and one in GTO reported some interferences with sleep, and the value of PSQI was higher than five (5–10) according to the survey of PSQI in this study.
Discussion
The etiology and neurological mechanism that generate SB are not well understood. During the past decades, researchers have focused on central factors rather than peripheral factors (e.g., occlusal factors)[17],[32],[33]. However, occlusal splint for management of bruxism is currently the standard for most dentists. Though a number of reports have been published with descriptions of the efficacy of these reversible occlusal interventions[34], many patients show little improvement in SB after having endured long-term occlusion adjusting therapy. Van der Zaag et al.[35] observed large differences among individuals with stabilization splints. Some of them indeed showed a decrease in bruxism activity (19%–29%), while others showed no change or even an increase (33%–48%). This suggests that the effect of occlusal modification has contributed much more to the protection of natural teeth and less to stopping the behavioral movement of bruxism itself[27].
Due to reasons mentioned above, the use of medications (e.g., botulinum toxin, L-dopa, SSRI, and propranolol) in the management of bruxism has been increasingly studied in recent years. Some drugs have a paralytic effect on masticatory muscles by inhibition of acetylcholine release at the neuromuscular junction, e.g., botulinum toxin[36],[37]. So far, its application in the management of bruxism is mainly described in case reports and in randomized clinical trials (RCT) which have also been recently reported[38]. In short, it was shown that SB did improve with frequently prescribed, non-specific muscle relaxant medicines[39]; the effectiveness of botulinum toxin has been reported for many neurological disorders[40]. Although the maintenance of therapeutic efficacy and the influence of these medicines on bruxism have not been fully understood, its long-term tolerability and the risk of addiction need further attention.
An alternative measure for management of bruxism is behavioral approaches, which has been tried for many years. The biofeedback method uses the concept that bruxers can unlearn their undesired behaviors when a stimulus makes them aware of their adverse muscle activities. This technique has been applied for bruxism during wakefulness as well as for SB. While awake, patients can be trained to control their jaw muscle activities through auditory or visual feedback from a surface EMG.
Auditory, electrical, vibratory and even taste stimuli can be used for SB feedback[24],[25],[41],[42]. The majority of case reports regard the biofeedback method to be an effective measure for the management of bruxism. Among these reports, the better design was a biofeedback device invented by Jadidi et al.[24], which is based on EMG of the temporalis without substantial sleep disturbance. Generally, bruxism diagnosis and biofeedback devices are based on monitoring masticatory muscle activity using surface electromyography. However, the surface EMG signal is affected by many factors such as electrode position, posture and skin resistance. In addition, attachment of multiple electrodes to the bruxer's face by a dentist or the bruxer without causing bruxer discomfort or sleep disruption is not easy or convenient. Several researchers have tried to measure SB activity directly by using an intra-oral appliance. Nishigawa et al.[30] measured bite force using a strain-gauge transducer incorporated into a bite-guard. This device was an analogue pressure sensor with electrical wires connected out of the mouth during sleep. Another patent proposed a device which tracks the position of the jaw using an optical sensing unit, but it required an upper and lower splint, as the light emitter and the detector were separated on each splint[43].
Therefore, despite the number of techniques that have been developed to detect and treat bruxism in the clinic, a practical method is still not available for bruxers to effectively and conveniently use. Compared to other oral devices for monitoring and treating bruxism, the characteristics of the biofeedback device the authors have proposed in this study are as follows: (i) The miniature maxillary biofeedback splint is integrated into one packet. As shown in Fig. 2 the splint covers from the right canine to the left canine with the margin extending to the lingual surface of the bilateral premolars. The design took into consideration both the patient's comfort and adequate cavities for embedding the monitoring circuit. A large splint often feels uncomfortable, compared with a mini one. Moreover, some studies showed that a thick splint can decrease rhythmic masticatory muscle activity (RMMA) in bruxers. However, the effect seems to be transitory[23]. To reduce the thickness of splint's effects on bruxism behavior and the oromandibular motor system, the authors designed the cavities for the pressure sensor, circuit and button cell using a wax model. The thickness of the contact point between the upper and lower canine is about 0.5 mm less than an ordinary resin splint in the intercuspal position, with no obvious contact in the mandibular postural position; (ii) The biofeedback system's operation is based on pressure-orient, which has distinct difference from an EMG-based device. The benefit of EMG is that it is more objective in evaluating bruxism events. However, there are some disadvantages to EMG as mentioned above. The wireless feature addresses the most important considerations, patient comfort and ease of use; (iii) The biofeedback device incorporates monitoring with biofeedback function and the threshold is convenient to modify subject to different circumstances. In many studies, the biofeedback devices relied on audio[44], which has the major disadvantage of sleep disturbance. In the development of this device, accurate vibration time was determined by a watch style device which is worn on the bruxer's wrist. In some cases, the patients may be conscious of bruxism behavior by feeling the vibration of the wrist without substantial waking.
There is no definite method for the management of bruxism with evidence-based tests to date. According to the data from subjects recruited in this study, the GTB results suggest that the total episodes of bruxism events had decreased dramatically, and had statistical significance from the baseline to 6 and 12 weeks after biofeedback therapy during 8 hours of sleep (P = 0.001). Furthermore, the average duration had also declined in the participants from the preliminary night to the end of 6 and 12 weeks study period (P = 0.026 and 0.012). In contrast to GTO, there were no significant differences in episodes and duration (all P>0.05). Meanwhile, there were significant differences in episodes between GTB and GTO after treatment (all P = 0.000). As the splint has the same design of structure and thickness for GTB and GTO, it is reasonable to assume the different efficacy in GTB resulted from the biofeedback method. However, despite having no universal standard for grading the severity of bruxism events at present, it is very important to narrow the results' interpretation. In this study, the total episodes of bruxism events ranged from 4 to 21 times in the baseline, indicating that the participants actually had ‘mild bruxism’. In other words, based on the results of this study, it is difficult to assume that the biofeedback therapy can be effective for all bruxers. The results have similar findings with some other reports, such as Jadidi et al. and Watanabe et al.[24],[40], mentioned above. The occlusal splint therapy in GTO demonstrated the indefinite results in the management of bruxism. The findings after 6 and 12 weeks of therapy are similar with Van der Zaag et al.[35], some of the bruxers have improvement of bruxism events (three bruxers out of twelve have improved their bruxism behaviors). The mean awake time in GTB is about 3–4 times per night without obvious disturbance of sleep, according to the Pittsburgh Sleep Quality Index (PSQI)[31] survey with the bruxers' self-reports (two in GTB and one in GTO have higher scores than five). This study suggests that the efficacy of biofeedback therapy on SB is relative to the bruxers' self-awareness of their behavior in bruxism events and the relaxation self-training, especially on the alleviation of episodes of bruxism events. Whether the putative mechanism of biofeedback lies in GTB is in connection with the relaxation of masticatory muscles or has effects on the central nervous system needs further research.
In conclusion, the mini wireless biofeedback device has proposed an effective, novel, and convenient method for bruxism therapy when contrasted with occlusal splint in this study. The total episodes and average duration were decreased remarkably after 6 and 12 wks therapy. Awareness of clenching or grinding of teeth can alleviate the episodes of bruxism behavior itself after several weeks' training and learning in mild bruxers.
Acknowledgments
We would like to thank Professor XiaoFeng Song and Professor ZhiYu Qian for their kind help with the mini wireless device development. The Bureau of Health of Jiangsu Province supported this study (H200939). A Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD, 2014-37) supported this study.
References
- 1.Winocur E, Uziel N, Lisha T, et al. Self-reported bruxism - associations with perceived stress, motivation for control, dental anxiety and gagging. J Oral Rehabil. 2011;38(1):3–11. doi: 10.1111/j.1365-2842.2010.02118.x. [DOI] [PubMed] [Google Scholar]
- 2.Rao SK, Bhat M, David J. Work, stress, and diurnal bruxism: a pilot study among Information technology professionals in Bangalore city, India. Int J Dent. 2011;2011:650489. doi: 10.1155/2011/650489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Selms MK, Lobbezoo F, Wicks DJ, et al. Craniomandibular pain, oral parafunctions, and psychological stress in a longitudinal case study. J Oral Rehabil. 2004;31(8):738–745. doi: 10.1111/j.1365-2842.2004.01313.x. [DOI] [PubMed] [Google Scholar]
- 4.Endo H, Kanemura K, Tanabe N, et al. Clenching occurring during the day is influenced by psychological factors. J Prosthodont Res. 2011;55(3):159–164. doi: 10.1016/j.jpor.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Manfredini D, Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain. 2009;23(2):153–166. [PubMed] [Google Scholar]
- 6.Kwak YT, Han IW, Lee PH, et al. Associated conditions and clinical significance of awake bruxism. Geriatr Gerontol Int. 2009;9(4):382–390. doi: 10.1111/j.1447-0594.2009.00538.x. [DOI] [PubMed] [Google Scholar]
- 7.De Laat A, Macaluso GM. Sleep bruxism as a motor disorder. Mov Disord. 2002;17(suppl):S67–S69. doi: 10.1002/mds.10064. [DOI] [PubMed] [Google Scholar]
- 8.Bader G, Lavigne G. Sleep bruxism; an overview of an oromandibular sleep movement disorder. Review Article. Sleep Med Rev. 2000;4(1):27–43. doi: 10.1053/smrv.1999.0070. [DOI] [PubMed] [Google Scholar]
- 9.Thorpy MJ. Classification of sleep disorders. Neurotherapeutics. 2012;9(4):687–701. doi: 10.1007/s13311-012-0145-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chokroverty S. Overview of sleep & sleep disorders. Indian J Med Res. 2010;131:126–140. [PubMed] [Google Scholar]
- 11.Lobbezoo F, van der Zaag J, van Selms MK, et al. Principles for the management of bruxism. J Oral Rehabil. 2008;35(7):509–523. doi: 10.1111/j.1365-2842.2008.01853.x. [DOI] [PubMed] [Google Scholar]
- 12.Tsiggos N, Tortopidis D, Hatzikyriakos A, et al. Association between self- reported bruxism activity and occurrence of dental attrition, abfraction, and occlusal pits on natural teeth. J Prosthet Dent. 2008;100(1):41–46. doi: 10.1016/S0022-3913(08)60135-3. [DOI] [PubMed] [Google Scholar]
- 13.Johansson A, Omar R, Carlsson GE. Bruxism prosthetic treatment: a critical review. J Prosthodont Res. 2011;55(3):127–136. doi: 10.1016/j.jpor.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Velly AM, Gornitsky M, Philippe P. Contributing factors to chronic myofascial pain: a case-control study. Pain. 2003;104(3):491–499. doi: 10.1016/S0304-3959(03)00074-5. [DOI] [PubMed] [Google Scholar]
- 15.Svensson P, Jadidi F, Arima T, et al. Relationships between craniofacial pain and bruxism. J Oral Rehabil. 2008;35(7):524–547. doi: 10.1111/j.1365-2842.2008.01852.x. [DOI] [PubMed] [Google Scholar]
- 16.Fernandes G, Franco AL, Siqueira JT, et al. Sleep bruxism increases the risk for painful temporomandibular disorder, depression and non-specific physical symptoms. J Oral Rehabil. 2012;39(7):538–544. doi: 10.1111/j.1365-2842.2012.02308.x. [DOI] [PubMed] [Google Scholar]
- 17.Koyano K, Tsukiyama Y, Ichiki R, et al. Assessment of bruxism in the clinic. J Oral Rehabil. 2008;35(7):495–508. doi: 10.1111/j.1365-2842.2008.01880.x. [DOI] [PubMed] [Google Scholar]
- 18.Lavigne GJ, Khoury S, Abe S, et al. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35(7):476–494. doi: 10.1111/j.1365-2842.2008.01881.x. [DOI] [PubMed] [Google Scholar]
- 19.Behr M, Hahnel S, Faltermeier A, et al. The two main theories on dental bruxism. Ann Anat. 2012;194(2):216–219. doi: 10.1016/j.aanat.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 20.de la Hoz-Aizpurua JL, Díaz-Alonso E, LaTouche-Arbizu R, et al. Sleep bruxism. Conceptual review and update. Med Oral Patol Oral Cir Bucal. 2011;16(2):e231–e238. doi: 10.4317/medoral.16.e231. [DOI] [PubMed] [Google Scholar]
- 21.Carra MC, Huynh N, Lavigne G. Sleep bruxism: a comprehensive overview for the dental clinician interested in sleep medicine. Dent Clin North Am. 2012;56(2):387–413. doi: 10.1016/j.cden.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 22.Shetty S, Pitti V, Satish Babu CL, et al. Bruxism: A Literature Review. J Indian Prosthodont Soc. 2010;10(3):141–148. doi: 10.1007/s13191-011-0041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klasser GD, Greene CS. Role of oral appliances in the management of sleep bruxism and temporomandibular disorders. Alpha Omegan. 2007;100(3):111–119. doi: 10.1016/j.aodf.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 24.Jadidi F, Castrillon E, Svensson P. Effect of conditioning electrical stimuli on temporalis electromyographic activity during sleep. J Oral Rehabil. 2008;35(3):171–183. doi: 10.1111/j.1365-2842.2007.01781.x. [DOI] [PubMed] [Google Scholar]
- 25.Watanabe A, Kanemura K, Tanabe N, et al. Effect of electromyogram biofeedback on daytime clenching behavior in subjects with masticatory muscle pain. J Prosthodont Res. 2011;55(2):75–81. doi: 10.1016/j.jpor.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 26.Kim JH, McAuliffe P, O'Connell B, et al. Development of wireless bruxism monitoring device based on pressure-sensitive polymer composite. Sensors and Actuators A: Physical. 2010;163(2):486–492. [Google Scholar]
- 27.Klasser GD, Greene CS, Lavigne GJ. Oral Appliances and the Management of Sleep Bruxism in Adults: A Century of Clinical Applications and Search for Mechanisms. Int J Prosthodont. 2010;23(5):453–462. [PubMed] [Google Scholar]
- 28.XiaoLong Wei, WeiPing Gu, ZhiYu Qian, et al. China. A biofeedback device for bruxism. 201120149478.2, January 4, 2012. [Google Scholar]
- 29.Doering S, Boeckmann JA, Hugger S, et al. Ambulatory polysomnography for the assessment of sleep bruxism. J Oral Rehabil. 2008;35(8):572–576. doi: 10.1111/j.1365-2842.2008.01902.x. [DOI] [PubMed] [Google Scholar]
- 30.Nishigawa K, Bando E, Nakano M. Quantitative study of bite force during sleep associated bruxism. J Oral Rehabil. 2001;28(5):485–491. doi: 10.1046/j.1365-2842.2001.00692.x. [DOI] [PubMed] [Google Scholar]
- 31.Buysse DJ, Reynolds CF, 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 32.Lavigne GJ, Kato T, Kolta A, et al. Neurobiological mechanisms involved in sleep bruxism. Crit Rev Oral Biol Med. 2003;14(1):30–46. doi: 10.1177/154411130301400104. [DOI] [PubMed] [Google Scholar]
- 33.Lobbezoo F, Naeije M. Bruxism is mainly regulated centrally, not peripherally. J Oral Rehabil. 2001;28(12):1085–1091. doi: 10.1046/j.1365-2842.2001.00839.x. [DOI] [PubMed] [Google Scholar]
- 34.Madani AS, Abdollahian E, Khiavi HA, et al. The efficacy of gabapentin versus stabilization splint in management of sleep bruxism. J Prosthodont. 2013;22(2):126–131. doi: 10.1111/j.1532-849X.2012.00914.x. [DOI] [PubMed] [Google Scholar]
- 35.Van der Zaag J, Lobbezoo F, Wicks DJ, et al. Controlled assessment of the efficacy of occlusal stabilization splints on sleep bruxism. J Orofac Pain. 2005;19(2):151–158. [PubMed] [Google Scholar]
- 36.Pidcock FS, Wise JM, Christensen JR. Treatment of Severe Post-Traumatic Bruxism With Botulinum Toxin-A: Case Report. J Oral Maxillofac Surg. 2002;60(1):115–117. doi: 10.1053/joms.2002.29127. [DOI] [PubMed] [Google Scholar]
- 37.Santamato A, Panza F, Di Venere D, et al. Effectiveness of botulinum toxin type A treatment of neck pain related to nocturnal bruxism: a case report. J Chiropr Med. 2010;9(3):132–137. doi: 10.1016/j.jcm.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee SJ, McCall WD, Jr, Kim YK, et al. Effect of Botulinum Toxin Injection on Nocturnal Bruxism. Am J Phys Med Rehabil. 2010;89(1):16–23. doi: 10.1097/PHM.0b013e3181bc0c78. [DOI] [PubMed] [Google Scholar]
- 39.Long H, Liao Z, Wang Y, et al. Efficacy of botulinum toxins on bruxism: an evidence-based review. Int Dent J. 2012;62(1):1–5. doi: 10.1111/j.1875-595X.2011.00085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jankovic J. Disease-oriented approach to botulinum toxin use. Toxicon. 2009;54(5):614–623. doi: 10.1016/j.toxicon.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 41.Watanabe T, Baba K, Yamagata k, et al. A vibratory stimulation-based inhibition system for noctural bruxism: a clinical report. J Prosthet Dent. 2001;85(3):233–235. doi: 10.1067/mpr.2001.114270. [DOI] [PubMed] [Google Scholar]
- 42.Nissani M. Can Taste Aversion Prevent Bruxism. Appl Psychophysiol Biofeedback. 2000;25(1):43–54. doi: 10.1023/a:1009585422533. [DOI] [PubMed] [Google Scholar]
- 43.Summer John D, Bodegom Erik, Lee Allen. Intra-oral jaw tracking device. U.S. Patent 5989023, November 23, 1999 [Google Scholar]
- 44.Foster PS. Use of the Calmset 3 biofeedback/relaxation system in the assessment and treatment of chronic nocturnal bruxism. Appl Psychophysiol Biofeedback. 2004;29(2):141–147. doi: 10.1023/b:apbi.0000026640.54839.83. [DOI] [PubMed] [Google Scholar]